Abstract
Background and aim
Reduction of platelet count is often observed in chronic hepatitis B (CHB) patients with significant liver fibrosis. In this cohort study, we investigated whether platelets’ increase after entecavir (ETV) therapy was associated with the improvement of liver fibrosis.
Methods
We collected the data of a cohort 82 CHB patients with paired liver biopsies before and after 78-week ETV therapy, and assessed the platelets’ change following the treatment and further investigated the associated clinical factors with platelets’ change.
Results
Platelet count increased after treatment, which occurred mainly in patients with low baseline level of platelet count (< 200 × 109/L) or with significant fibrosis (Ishak ≥ 3). Regression analysis showed that baseline platelet count was the main factor associated with post-treatment increase of platelets (β = − 0.215, p = 0.015). In patients with significant fibrosis, correlation and linear regression analysis revealed that post-treatment platelets’ increase was correlated with improvement of liver fibrosis assessed by reduction of quantitative collagen percentage area (r = 0.392, p = 0.006) (β = 2.449, p = 0.035), but no correlation between changes in platelet counts and Ishak fibrosis score. Receiver operating curve analysis showed an increase of 12.5 × 109/L in platelet count could identify improvement of liver fibrosis (AUC = 0.70).
Conclusion
Platelets’ increase after ETV therapy was associated to the improvement of liver fibrosis with reduction of collagen percentage area in CHB patients with significant fibrosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Antiviral therapy has been the vital treatment in patients with chronic hepatitis B (CHB) [1,2,3], and it can significantly improve the outcome of patients. It has been proved that liver fibrosis can be regressed after antiviral therapy, even in cirrhosis patients [4, 5]. Paired biopsies of pre- and post-treatment are still the gold standard of evaluating liver fibrosis change. The non-invasive assessment is needed, which will be useful to dynamically evaluate the fibrosis change after treatment and improve compliance.
Thrombocytopenia is strongly associated with severe fibrosis in patients with chronic liver diseases; therefore platelet count is often used in diagnostic algorithms to noninvasively identify the presence of significant fibrosis [6, 7]. The relationship between post-treatment change of platelet count and liver fibrosis is still unclear. Previous studies on chronic hepatitis C (CHC) revealed that platelets’ increase after sustained virological response was correlated with the improvement of hepatic fibrosis [8,9,10].
Although it had been reported that the platelets increased after nucleoside treatment in CHB patients [11], there has been no study to determine whether post-treatment platelets’ increase had relationship with fibrosis improvement. Besides, previous studies used semi-quantitative Ishak staging system to evaluate the change of liver fibrosis, which might cause bias.
In this study, we evaluated the change of platelet counts after ETV (entecavir) treatment and investigated the factors associated with platelets’ change, with focus on whether the post-treatment increase of platelet counts was related with improvement of liver fibrosis evaluated by quantitative collagen percentage area (CPA) assessment before and after treatment.
Patients and methods
Patients
All participating patients were from the “Regression Study” (ClinicalTrials.gov: NCT01938781, NCT01938820). Inclusion criteria included: male or female aged 18–65 years; HBsAg positive for at least 6 months before treatment; HBV-DNA load of more than 20,000 IU/mL in the HBeAg-positive patients before treatment or 2000 IU/mL in the HBeAg-negative patients; with paired liver biopsy before and after 78-week ETV therapy. Exclusion criteria were as follows: co-infection with hepatitis C or human immuno-deficiency virus; the presence of chronic liver disease caused by other etiologies; decompensated cirrhosis; alpha-fetoprotein > 100 ng/mL; Cr > 1.5 times than the upper limit of normal; malignant tumors; severe diseases of heart, lung, kidney, brain, blood system or other organs; pregnant or lactating female.
All patients received ETV therapy after initial evaluation of the liver fibrosis by liver biopsy, and the second liver biopsy was conducted after 78 weeks treatments to evaluate fibrosis change.
Collection of clinical data
Demographic data were collected at baseline (week 0), and clinical tests were performed at baseline and at every 26 weeks intervals including blood cell counts, HBV-DNA level, serological markers of HBV, liver functional tests, AFP, and liver ultrasonography. HBV serological markers and serum HBV-DNA level were measured centrally using Abbott Architect i2000 (ABBOTT, Wiesbaden, Germany) and Roche COBAS®TaqMan® HBV Test, respectively.
Histological evaluation
Liver tissues were formalin fixed, paraffin embedded and sectioned at local centers according to standard techniques. The tissue sections were stained centrally with hematoxylin and eosin, reticulin and Masson trichrome. The stained sections were then independently evaluated by two experienced pathologists. Necroinflammation was assessed by the modified histology activity index (HAI) grading system (a scale of 0–18) and fibrosis was staged by the Ishak fibrosis scoring system (a scale of 0–6) [12].
Measurement of CPA
Measurement of CPA was performed by second-harmonic generation (SHG)/two-photon excitation fluorescence (TPEF) microscope (Genesis200TM, HistoIndex Pte. Ltd, Singapore) [13, 14]. SHG microscope was used to visualize collagen and TPEF was to identify cell structures. The CPA was measured by the area percentage of TPEF signals normalizing the SHG signals (Supplementary Fig. 1).
Definition of liver fibrosis improvement
The improvement of liver fibrosis was evaluated by CPA reduction. We defined the fibrosis improvement with a 2.0 CPA reduction after treatment. The receiver operating characteristic curve (ROC) analysis showed that a 2.0 post-treatment reduction of CPA identified the standard with the area under curve (AUC) of 0.68, (Supplementary Fig. 2). The standard was at least 1-point decrease in Ishak score, or was “Predominately Regressive” by “P-I-R classification” when Ishak score was same before and after treatment [15].
Statistical analysis
Characteristics on pre- and post-treatment were compared using student’s paired t test for normally distributed continuous variables, the Mann–Whitney test for non-normally distributed variables and the Chi-square test for categorical variables. Repeated measurement analysis was used to assess the platelets’ change following treatment. Linear regression analysis was performed to determine the clinical factors associated with the platelets’ change.
Correlations between platelets’ increase and reduction of CPA and Ishak score were performed using the Spearman’s rank test. For assessing the performance of platelets’ increase and increase rate to identify liver fibrosis improvement, the receiver operating characteristic (ROC) curve analysis was carried out to determine the area under the curve (AUC) values. A p value of less than 0.05 was considered statistically significant. Statistical analyses were performed using SPSS version 20.0 (IBM, Chicago, IL).
Results
Characteristics of the study population
This study enrolled 90 patients receiving ETV treatment. Finally, 82 patients with eligible paired biopsy were included in the final analysis. Most of the patients were male (77%) with a mean age of 41 years. Before treatment, 74% of them were HBeAg-positive with elevated serum ALT and mean HBV-DNA level of 6.30 log IU/mL. After 78 weeks of ETV therapy, HBV-DNA was undetectable (< 20 IU/mL) in 79% patients. Laboratory tests and histology of liver tissue improved, platelets increased from 155 ± 53 × 109/L to 182 ± 52 × 109/L and CPA decreased (Table 1). Liver fibrosis improved after treatment. Ishak scores decreased in 46% patients (Supplementary Fig. 3) and median of CPA measurement also decreased from 4.95 to 2.43 (p < 0.01). Among significant fibrosis and cirrhosis patients with unchanged post-treatment Ishak score, 78% of them had fibrosis regression according to “P-I-R criterion” (Supplementary Table).
Factors associated with post-treatment platelets’ increase
Table 2 showed the linear regression analysis about the factors associated with post-treatment platelets’ increase. In the univariate analysis, the factors contributing to platelets’ increase included worse baseline liver function tests, change of these tests after treatment, pre-treatment inflammatory score and baseline platelet counts. In the multivariate analysis, the baseline level of platelet counts was the only factor related with the post-treatment increase of platelets (β = − 0.215, p = 0.015) (Table 2). Platelets’ increase was mainly observed in patients with low platelet counts at baseline.
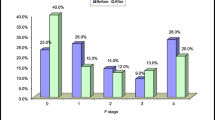
Impact of baseline platelet counts and fibrosis stage on platelets’ increase
Repeated measurement analysis showed that patients with low baseline platelet counts (< 200 × 109/L) or with significant fibrosis (Ishak ≥ 3) had significant platelets’ increase after treatment. The mean of platelet counts increased from 135 × 109/L at baseline to 167 × 109/L at week 78 in patients with low baseline platelets, from 158 × 109/L to 188 × 109/L in patients with Ishak3/4, and from 131 × 109/L to 158 × 109/L in cirrhosis patients (Ishak5/6). There was no difference in platelet counts between pre- and post-treatment among patients with high baseline platelets or mild fibrosis (Table 3).
Factors associated with platelets’ increase in patients with significant fibrosis
In 53 patients with baseline platelet counts less than 200 × 109/L and Ishak score ≥ 3, the mean platelet counts increased from baseline 130 × 109/L to 163 × 109/L after 78-week treatment. The correlation analysis revealed that there was a positive correlation between post-treatment platelets’ increase and CPA reduction in patients with significant fibrosis (r = 0.392, p = 0.006), and no correlation between platelets’ increase and Ishak score change (Fig. 1). The multivariate linear regression analysis showed that the only factor associated with platelets’ increase were post-treatment CPA reduction (β = 2.449, p = 0.035) (Table 4). There was no correlation between post-treatment change of Ishak score and platelets’ increase either univariate or multivariate analysis.
Performance of platelets’ increase to identify fibrosis improvement
ROC analysis showed that platelets’ increase and increase rate could identify fibrosis improvement which defined as at least 2.0 reduce in CPA. A post-treatment 12.5 × 109/L increase in platelet counts distinguished fibrosis improvement with 89% sensitivity, 46% specificity, and an AUC of 0.70 (95% CI 0.54–0.82). It was similar to 9% increase rate of platelet count to identify fibrosis improvement (sensitivity: 86%, specificity: 50%, and AUC: 0.68) (Fig. 2).
Discussion
In this cohort study, we found that the platelets increased after ETV therapy in CHB patients, especially in those patients with low pre-treatment platelet counts and significant fibrosis. Among patients with significant fibrosis, platelets’ increase after treatment was correlated with improvement of liver fibrosis measured by CPA reduction.
Our results were in line with previous studies of CHC patients receiving antiviral therapy. In a study including CHC patients mostly with mild fibrosis, the mean level of platelet counts was similar between pre- and post-treatment (232 × 109/L vs. 235 × 109/L) [16]. In contrast, the platelet counts after treatment were significantly increased compared with pre-treatment level in studies which included patients mostly with significant fibrosis [17, 18].
We found that post-treatment platelets’ increase had a positive correlation with fibrosis improvement in patients with significant fibrosis, and the fibrosis improvement should be evaluated by CPA. There was no correlation when fibrosis change was measured by Ishak score. Similarly, Kim et al. also found that improvement in non-invasive measurements of liver fibrosis was not associated with liver fibrosis change assessed by Ishak staging in CHB patients [11]. The reason might be that the semi-quantitative Ishak scoring system was not sensitive enough to evaluate the post-treatment change of liver fibrosis. The quantitative CPA was suitable in assessing the subtle change of liver fibrosis. Some studies had confirmed that CPA can be used to effectively monitor the liver fibrosis change in CHC patients [19, 20]. The results of our study suggested that post-treatment change of platelets counts might be useful tool to evaluate the subtle fibrosis change measured by CPA.
One limitation of this cohort study was that most of patients were followed only for 78 weeks. Fortunately, patients in the cohort will be followed successively for another 5 years, and then we can verity the results in longer follow-up interval. The cohort of present study was not large-scale. Hopefully, the strict inclusion and exclusion criteria could minimize the confounding factors.
In conclusion, ETV therapy can increase platelet counts of CHB patients with significant liver fibrosis, and this platelets’ increase had positive correlation with fibrosis improvement that need be evaluated by CPA.
Abbreviations
- ALT:
-
Alanine aminotransferase
- AST:
-
Aspartate aminotransferase
- AUC:
-
Area under the curve
- CHB:
-
Chronic hepatitis B
- CHC:
-
Chronic hepatitis C
- CI:
-
Confidence interval
- CPA:
-
Collagen proportionate area
- ETV:
-
Entecavir
- SHG:
-
Second-harmonic generation
- TPEF:
-
Two-photon excitation fluorescence
- ROC:
-
Receiver operating curve
References
World Health Organization. Guidelines for the Prevention, Care and Treatment of Persons with Chronic Hepatitis B Infection. Geneva. 2015.
American Association for the Study of Liver Diseases. AASLD guidelines for treatment of chronic hepatitis B. Hepatology. 2016;63:261–83.
Association for the study of the liver. EASL clinical practice guidelines: management of chronic hepatitis B virus infection. J Hepatol. 2012;57:167–85.
Marcellin P, Gane E, Buti M, et al. Regression of cirrhosis during treatment with tenofovir disoproxil fumarate for chronic hepatitis B: a 5-year open-label follow-up study. Lancet. 2013;381:468–75.
Liaw YF. Reversal of cirrhosis: an achievable goal of hepatitis B antiviral therapy. J Hepatol. 2013;59:880–1.
European Association for Study of Liver. EASL-ALEH clinical practice guidelines. Non-invasive tests for evaluation of liver disease severity and prognosis. J Hepatol. 2015;63:237–64.
American Association for the study of liver diseases. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management. Hepatology. 2017;65:310–35.
Coverdale SA, Samarasinghe DA, Lin R, et al. Changes in antipyrine clearance and platelet count, but not conventional liver tests, correlate with fibrotic change in chronic hepatitis C: value for predicting fibrotic progression. Am J Gastroenterol. 2003;98:1384–90.
Taniguchi H, Iwasaki Y, Fujiwara A, et al. Long-term monitoring of platelet count, as a non-invasive marker of hepatic fibrosis progression and/or regression in patients with chronic hepatitis C after interferon therapy. J Gastroenterol Hepatol. 2006;21:281–7.
Meer AJ, Maan R, Veldt BJ, et al. Improvement of platelets after SVR among patients with chronic HCV infection and advanced hepatic fibrosis. J Gastroenterol Hepatol. 2016;31:1168–76.
Kim WR, Berg T, Asselah T, et al. Evaluation of APRI and FIB-4 scoring systems for non-invasive assessment of hepatic fibrosis in chronic hepatitis B patients. J Hepatol. 2016;64:773–80.
Ishak K, Baptista A, Bianchi L, et al. Histological grading and staging of chronic hepatitis. J Hepatol. 1995;22:696–9.
Xu S, Wang Y, Tai DC, et al. qFibrosis: a fully-quantitative innovative method incorporating histological features to facilitate accurate fibrosis scoring in animal model and chronic hepatitis B patients. J Hepatol. 2014;61:260–9.
Tai DC, Tan N, Xu S, et al. Fibro-C-Index: comprehensive, morphology-based quantification of liver fibrosis using second harmonic generation and two-photon microscopy. J Biomed Opt. 2009;14:044013.
Sun Y, Zhou J, Wang L, et al. New classification of liver biopsy assessment for fibrosis in chronic hepatitis B patients before and after treatment. Hepatology. 2017;65:1438–50.
George SL, Bacon BR, Brunt EM, et al. Clinical, virologic, histologic, and biochemical outcomes after successful HCV therapy: a 5-year follow-up of 150 patients. Hepatology. 2009;49:729–38.
Koh C, Heller T, Haynes-Williams V, et al. Long-term outcome of chronic hepatitis C after sustained virological response to interferon based therapy. Aliment Pharmacol Ther. 2013;37:887–94.
Morgan TR, Ghany MG, Kim HY, et al. Outcome of sustained virological responders with histologically advanced chronic hepatitis C. Hepatology. 2010;52:833–44.
Caballero T, Pérez-Milena A, Masseroli M, et al. Liver fibrosis assessment with semiquantitative indexes and image analysis quantification in sustained-responder and non-responder interferon-treated patients with chronic hepatitis C. J Hepatol. 2001;34:740–7.
Goodman ZD, Becker RL Jr, Pockros PJ, Afdhal NH. Progression of fibrosis in advanced chronic hepatitis C: evaluation by morphometric image analysis. Hepatology. 2007;45:886–94.
Acknowledgements
The authors are thankful to the staff of participating institutions.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Lin Wang, Bingqiong Wang, Hong You, Xiaoning Wu, Jialing Zhou, Xiaojuan Ou, and Jidong Jia do not have anything to disclose regarding potential conflicts of interest.
Ethical approval
The study was conducted in accordance with the ethical guidelines of the 1975 Declaration of Helsinki (2008 revision), and the protocol of study was approved by the Ethics Committee of Beijing Friendship Hospital. Our study had been registered in the ClinicalTrials.gov (NCT01938781 and NCT01938820).
Financial support
This study was supported by the grant of National Science and Technology Major Project (2013ZX10002004) and Key Project from Beijing Municipal Science and Technology Commission (D121100003912003).
Informed consent
The written informed consent was obtained from every patient prior to initiating any study procedures.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Wang, L., Wang, B., You, H. et al. Platelets’ increase is associated with improvement of liver fibrosis in entecavir-treated chronic hepatitis B patients with significant liver fibrosis. Hepatol Int 12, 237–243 (2018). https://doi.org/10.1007/s12072-018-9864-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-018-9864-z