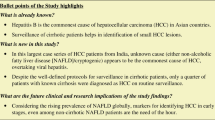
Abstract
Background
The incidence of hepatocellular carcinoma (HCC) has increased significantly in United States over the last few decades in parallel with the epidemic of nonalcoholic fatty liver disease (NAFLD). Limited data suggests that HCC could arise in steatotic liver without the presence of cirrhosis. The present study was conducted to characterize patients with NAFLD presenting with HCC in non-cirrhotic liver (NCL) compared to the NAFLD- HCC patients in association with cirrhotic liver (CL).
Methods
A retrospective analysis of all patients diagnosed with HCC and NAFLD diagnosis seen at our institution between 2003 and 2012 was done. The patients were characterized based on demographic and clinical variables as well as histological and tumor features. Comparisons between the NCL and CL groups were done using analysis of variance (ANOVA) or the non-parametric Kruskal–Wallis tests and Pearson's chi-square tests or Fisher's Exact tests as appropriate. P value of <0.05 was considered statistically significant.
Results
Thirty-six patients with NAFLD and HCC in NCL (HCC-NCL group) were identified and compared to 47 patients with NAFLD-HCC and Liver Cirrhosis (HCC-LC group). Liver fibrosis was not present in 55.9 % of patients in the HCC-NCL group (F0), stage 1 was present in 17.6 %, stage 2 in 8.8 % and stage 3 in 17.6 %. Lobular inflammation was present in 63.6 % of non-cirrhotic patients. Patients in the HCC-NCL were older (67.5 ± 12.3 vs. 62.7 ± 8.1 years), and less likely to be obese (52 % vs. 83 %) or have type 2 diabetes (38 % vs. 83 %), with p value <0.05 for all. More importantly, compared with the HCC-CL group, those in the HCC-NCL group were more likely to present with a single nodule (80.6 % vs. 52.2 %), larger nodule size (>5 cm) (77.8 % vs. 10.6 %), and receive hepatic resection as the modality of HCC treatment (66.7 % vs. 17 %); and were less likely to receive loco-regional therapy (22.3 % vs. 61.7 %) or orthotopic liver transplantation (OLT) (0 % vs. 72.3 %), with p value <0.001 for all. Furthermore, 86 % of patients without cirrhosis had HCC recurrence compared to only 14 % in patients with cirrhosis (p < 0.001). Unadjusted analysis indicates that non-cirrhotics had worse survival with mortality rate of 47 % vs. 28 % in CL group (p = 0.03); however this difference in survival between two groups was not significant after adjusting for age or OLT (p > 0.05).
Conclusion
Patients with HCC in the absence of liver cirrhosis are more likely to present at an older age with larger tumor and have higher rates of tumor recurrence. Studies to assess the cost-effectiveness of HCC surveillance in this group should be conducted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular carcinoma (HCC) is the fifth most common cancer worldwide with more than 500 thousand newly diagnosed cases each year [1, 2]. Moreover, HCC is the third leading cause of death from cancer overall with very rapid-growing cancer-related mortality rate in the USA in the last 10 years [3, 4]. Recently, the incidence of HCC has increased more than threefold in the USA [3], which coincided with the progressive prevalence of non-alcoholic fatty liver disease (NALFD) [5].
NAFLD is the hepatic manifestation of the metabolic syndrome and has emerged as the most common variant of chronic liver disease in the last decade [6]. NAFLD is expected to constitute the main reason for liver-related morbidity, mortality and liver transplantation in the upcoming years in the USA [5] because of the growing epidemics of diabetes and obesity. Population-based studies have revealed an estimated NAFLD prevalence of at least 30 % in the adult population with even higher rates among obese and type 2 diabetes patients (70–90 %) [7, 8]. Similarly, HCC has an established association with obesity and diabetes [9, 10]. Two meta-analyses have reported a relative increased risk of HCC in obese and diabetic patients of 1.89 and 2.31 fold, respectively [11, 12].
Although more than half of the HCC cases are attributed to virus- and alcohol-related cirrhosis, the definitive cause of HCC in 15–50 % of the cases remains unclear (cryptogenic hepatocellular carcinoma) and without well-known risk factors [13, 14]. It has been identified that non-alcoholic steatohepatitis (NASH), the aggressive form of NAFLD, accounts for a substantial portion (13–38 %) of these cryptogenic hepatocellular carcinoma cases [15, 16]. Moreover, NAFLD has been established as a risk factor for HCC in emergent data [17], with 2.6 % yearly cumulative incidence of HCC in patients with NASH cirrhosis [18].
Although HCC has been well reported to develop in cirrhotic livers secondary to NAFLD [19, 20], fatty liver without cirrhosis has also been recognized to play a significant role in the tumor genesis of HCC [14]. Few observations suggest an association between solely hepatic steatosis and HCC hypothesizing the potential carcinogenetic effect of hepatic steatosis in HCC development despite the absence of cirrhosis [21].
This correlation between HCC and non-cirrhotic chronic liver disease has been reported previously [22, 23], but scarcity of information and limited data are available on the characteristics and outcome of HCC arising in NAFLD-related liver disease in the absence of cirrhosis.
The present study was conducted to characterize patients with NAFLD presenting with HCC in non-cirrhotic liver (NCL) and compare them with patients with HCC in NAFLD-related cirrhotic liver (CL) as well as to identify demographic variables, risk factors, tumor features and survival differences between the two groups.
Materials and methods
A retrospective analysis was performed on all adults (age ≥18 years) diagnosed with HCC and NAFLD at Cleveland Clinic Foundation between 2003 and 2012.
The electronic medical records were reviewed thoroughly aiming to characterize the patients with HCC in NCL-NAFLD and compare them to HCC patients in CL based on demographic and clinical variables, histological features and tumor presentation. Liver cirrhosis was identified based on the histological presentation and/or radiological evidence of cirrhosis. NAFLD was defined according to the histological features of steatosis (with/without inflammation ± fibrosis), when available, cryptogenic cirrhosis in the presence of metabolic syndrome, or presence of fatty liver on imaging modalities without a history of significant alcohol intake or confounding liver diseases. Metabolic syndrome was defined in accordance with National Cholesterol Education Program Adult Treatment Plan III (ATP III) guidelines (the waist circumference trait was replaced by BMI > 28.2 kg/m2 for study purposes, which has been validated) [24].
The diagnosis of diabetes mellitus was made based on clinical notes, the use of insulin or oral hypoglycemic medication or HbA1C level ≥6.5.
Demographic data (age, sex and race) and medical history of hypertension, hyperlipidemia and diabetes with their corresponding therapy were obtained from medical records. Details of the metabolic traits and chemistry panel were evaluated at the time of HCC diagnosis—including levels of bilirubin, albumin, prothrombin time, alkaline phosphatase, gamma-glutamyl transferase, alanine aminotransferase, aspartate aminotransferase, creatinine, hemoglobin, platelet count, HbA1c, triglyceride, high-density lipoprotein, ferritin and alpha-fetoprotein (AFP) levels.
All our patients underwent either whole-liver resection than pathological study through the process of a liver transplant or, if a transplant was not applicable, at least two liver biopsies were done, one from the tumor and the other from the adjacent or normal liver tissue. The liver histological report was reviewed, and steatosis was graded similar to the NAFLD activity score (NAS) [25] as absent, mild, moderate or severe when it involved <5 % (0), 5–33 % (1), 33–66 % (2) or >66 % (3) of hepatocytes, respectively. Inflammation also was assessed and graded as none, mild, moderate or severe according to the report. Hepatic fibrosis (stage) was assigned according to the Ludwig-Batts scoring system with a scale of 0–4 (F0: absent; F1: portal fibrosis; F2: periportal fibrosis; F3: bridging fibrosis; F4: cirrhosis).
The diagnosis of HCC was based on radiological and/or histological evidence according to the American Association for the Study of Liver Diseases (AASLD) guidelines [26]. Tumor characteristics were obtained using pathological and radiological reports. These features include the size and number of HCC nodules, presence of lymph nodes and distant metastases as well as the degree of tumor differentiation.
Additionally, the treatment modality, survival rate and factors influencing the survival were analyzed based on retrospective review of the medical records. Follow-up time was defined as the time from HCC diagnosis to the last available follow-up visit. The length of survival was considered from the date of HCC diagnosis to the date of death or the date of last available follow-up visit.
Patients with confounding liver diseases were excluded from the study including: seropositive hepatitis B or C infection, hereditary hemochromatosis (by serum iron indices in all patients and genetic testing, if indicated); primary biliary cirrhosis (serum mitochondrial antibody and compatible histology); primary sclerosing cholangitis (by cholangiogram, if suspected); Wilson disease; autoimmune hepatitis (based on serum markers and histology); and alpha-1-antitrypsin deficiency (phenotypic analysis, AAT levels). Patients with “significant alcohol intake” were also excluded. According to the recent consensus meeting [27] conclusion for NASH clinical trials, significant alcohol consumption is defined as ongoing or recent alcohol consumption (over a 2-year period prior to baseline liver histology) >21 drinks on an average per week in males and >14 drinks in females.
Statistical analysis
Data are presented as mean ± standard deviation or median [25th, 75th percentiles] for continuous variables and N (%) for categorical factors. A univariable analysis was performed to assess differences between NAFLD patients with and without cirrhosis. Wilcoxon rank sum and t tests were used for continuous variables, and Pearson’s chi-square or Fisher’s exact tests were used for categorical factors.
Kaplan-Meier product limit estimates were used to assess patient survival, and a log-rank test was used to compare the groups. In addition, multivariable Cox regression analysis was performed. A p value < 0.05 was considered statistically significant. SAS version 9.4 (The SAS Institute, Cary, NC) was used to perform all analyses.
Results
Based on the selection criteria, a total of 83 patients were identified with HCC arising in the background of NAFLD. There were 36 patients with NAFLD and HCC in the NCL (HCC-NCL) group and 47 patients in the NAFLD-HCC and CL (HCC-CL) group. Average age at time of HCC diagnosis was 65 ± 10 years, and 65 % were male. Tables 1 and 2 present a summary of patient characteristics.
Demographical and clinical variables
The results of comparison between two groups (CL and NCL) were as follows:
Patients in the HCC-NCL group were older with a mean age of 67.5 ± 12.3 years vs. 62.7 ± 8.1 years for patients with HCC-CL, p value of 0.035 (Table 1). A significant difference was noticed according to the race. While the majority of patients were Caucasians in both groups, the only four African American subjects were seen exclusively in the NCL group.
In the HCC-NCL group, as expected, normal liver enzymes, higher albumin and hemoglobin levels as well as WBC and platelet counts and lower AST, total bilirubin, INR and RDW-CV values were noted. Patients in the HCC-NCL group were less likely to be obese (BMI >30) (52 vs. 83 % in HCC-CL, p value of 0.003). Correspondingly, metabolic syndrome was noticed more frequently among HCC-CL patients (93 vs. 67 %, p value of 0.003).
A significant difference between two groups was apparent with respect to diabetes mellitus. Patients in the NCL group were less likely to have type 2 diabetes (38 vs. 83 %, p value <0.001). There were no statistically significant differences between these two groups with regard to hypertension, hyperlipidemia, smoking or alcohol consumption, or median values of AFP (ng/ml) (14.2 vs. 6.2 in the CL group), alkaline phosphatase (U/l) (94 vs. 143) and ferritin (ng/ml) (157.6 vs. 229.6) at the time of diagnosis.
Characterization of histological features
Liver tissue for histological analysis was present in 79 patients (a specimen was obtained at the time of OLT in 34 patients, liver resection in 16 patients and liver biopsy in 29 patients). Four patients did not have liver tissue available. In patients with available liver tissue, liver fibrosis was not present in 55.9 % of patients in the HCC-NCL group (F0), stage 1 was present in 17.6 %, stage 2 in 8.8 % and stage 3 in 17.6 % (Fig. 1). Moreover, the majority of NCL patients (87.6 %) had only grade 1 steatosis (5–33 %), and lobular inflammation was present in 63.6 %. Importantly, compared to the HCC-CL group, subjects in the HCC-NCL group were more likely to present with a single nodule (80.6 vs. 52.2 %) and larger nodule size (>5 cm) (77.8 vs. 10.6 %), p value <0.05 for both. In addition, subjects without cirrhosis were less likely to have Mallory bodies found on biopsy (0 vs. 25.5 %).
HCC treatment and recurrence
Overall, patients in the NCL group were more likely to have hepatic resection (66.7 vs. 17 %) or palliative treatment (13.9 vs. 0 %) as the modality for HCC treatment, and they were less likely to receive locoregional (including chemoembolization and radiofrequency ablation) therapy (22.3 vs. 61.7 %) or liver transplant (0 vs. 72.3 %), p value <0.05 for all.
Recurrence information was only available for 58 subjects (21 NCL and 37 CL). Patients in the NCL group were more likely to have cancer recurrence (86 vs. 14 %), even if there were no significant differences observed with respect to tumor stage (presence of involved lymph nodes or distant metastases) or tumor differentiation at time of HCC diagnosis.
Survival analysis
Survival status was unknown for four subjects. Unadjusted analysis indicates that CL group subjects have better survival than those in the NCL group, probably because (as shown above) they were significantly younger and more likely to have OLT. Nevertheless, after adjusting for age, there is no evidence of a difference in 5-year survival rates between the two groups (Fig. 2 presents the Kaplan-Meier plot). Similarly, after adjusting for OLT, there is no evidence of a difference in survival rates between the two groups as well (data not shown). Multivariable Cox regression analysis showed no difference in mortality between the NCL and CL groups with a hazard ratio (95 % CI) of 1.5 (0.57, 4.0), p value of 0.4. The only variable that was associated with increased mortality in NAFLD patients with HCC with and without cirrhosis was age [for each 1-year increase in age, mortality increased by 10 %; hazard ratio (95 % CI) of 1.10 (1.03, 1.2), p value of 0.004].
Discussion
The salient findings observed in the present study include: (1) HCC can develop in NAFLD patients despite the absence of fibrosis (fibrosis was absent on biopsy in 55.9 % of NCL patients). (2) Obesity and diabetes background was not present in striking proportions of the NCL group. (3) HCC-NCL patients were more likely to present at an older age with larger tumors and have higher rates of tumor recurrence. (4) No survival difference was observed between the two groups after adjustment for age and OLT.
Of 83 NAFLD-HCC patients in our study, 36 (43 %) had no cirrhosis, which is similar to the prevalence of NAFLD-HCC individuals without evidence of cirrhosis in Ertle et al. [16] (41.7 %) and Duan et al. [28] (40 %). Patients with HCC in NCL presented at an older age (mean age of 67.5 ± 12.3 years) than patients with HCC in CL, and this finding has also been documented in a previous study [29].
It is not proven whether in these patients steatosis and/or inflammation is sufficient alone or whether fibrosis is needed to develop before HCC can arise. However, in our analysis liver fibrosis was not present in 55.9 % of patients in the HCC-NCL group. Moreover, there are multiple theories suggesting the potential strong role of steatosis and associated hormonal and inflammatory mechanisms in hepatocarcinogenesis of HCC development in non-cirrhotic NAFLD subjects [30, 31]. Therefore, further studies are needed to elucidate the clear mechanisms for HCC in non-cirrhotic fatty liver.
The cohort study of Alexander et al. [32] characterized the significant association between steatosis and/or steatohepatitis with HCC in 157 HCC patients in the background of histologically proven non-cirrhotic hepatic steatosis. The prevalence of both steatosis and NASH in non-cirrhotic HCC was reported as significant as 54 and 15 %, respectively [32]. Additionally, the previous study reported HCC being more prevalent in cases with higher grades of steatosis (88 % of patients with grade 3 steatosis had HCC), in contrast to our report, which showed the majority of HCC-NCL NAFLD patients (87.6 %) had only mild steatosis.
On the other hand, another important point in understanding the nature of NAFLD-related HCC is its relation to diabetes mellitus and metabolic syndrome. The data of a recent retrospective study by Ertle et al. [16] on patients with HCC revealed the patients with NAFLD/NASH-associated HCC exhibited a higher prevalence of metabolic features including DM and hyperlipidemia compared to people in non-NAFLD HCC patients. Nevertheless, in our analysis HCC-NCL patients were interestingly less likely to be obese (BMI >30) (52 vs. 83 % in CL group). Only 38 % had type 2 diabetes and 67.9 % had metabolic syndrome, whereas a significant proportion of patients with cirrhosis had metabolic syndrome (n = 44, 93 %). These findings are consistent with the few reported cases of HCC that occurred in non-cirrhotic fatty livers despite the absence of obesity, diabetes and other metabolic risk factor [16, 32]. All of these observations raised the assumption that NAFLD could be the primary risk factor for HCC rather than obesity or diabetes, taking into account that hepatic steatosis was also found to be present in 74 % of patients with diabetes [8]. Our data demonstrated that patients with NAFLD-associated HCC in the absence of cirrhosis were more likely to present with a single nodule (80.6 %) and larger nodule size (>5 cm) at time of HCC diagnosis, and this finding goes along with the reports of previous studies [29, 33, 34]. This finding was expected because the current AASLD guidelines do not support screening for HCC in non-cirrhotic patients with NAFLD, allowing the tumor to become larger before identification and potentially causing worse outcome.
The major strength of the analysis of this study is that this is the first study in the USA, to our knowledge, to directly describe the characteristics of patients with NAFLD-associated HCC without a cirrhosis background and perform a thorough comparison with HCC patients with NAFLD-related cirrhosis. However, the present study has some limitations due to the retrospective design and small number of patients, which might lead to insignificant findings in the statistical analyses.
In conclusion, HCC in non-cirrhotic patients has distinct features compared to HCC in CL; these patients present incidentally with larger tumor size and have higher rates of tumor recurrence, conferring an unfavorable prognosis. Given the lack of currently effective therapeutic and preventive measures for NCL-NAFLD patients, major challenges still face physicians in terms of management of this population. Therefore, targeting a novel specific risk factor profile that defines NAFLD patients without cirrhosis as at higher risk of developing HCC is necessary. Additionally, further studies to identify the epidemiological associations of HCC and NAFLD without cirrhosis and to assess the cost-effectiveness of HCC surveillance in this population group would be of interest and need to be conducted.
References
El-Serag HB, Rudolph KL. Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology. 2007;132(7):2557–2576
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90
Altekruse SF, McGlynn KA, Reichman ME. Hepatocellular carcinoma incidence, mortality, and survival trends in the United States from 1975 to 2005. J Clin Oncol. 2009;27(9):1485–1491
El-Serag HB. Hepatocellular carcinoma. New England J Med. 2011;365(12):1118–1127
Charlton MR, Burns JM, Pedersen RA, Watt KD, Heimbach JK, Dierkhising RA. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141(4):1249–1253
Fan JG, Zhu J, Li XJ, Chen L, Li L, Dai F, Li F, Chen SY. Prevalence of and risk factors for fatty liver in a general population of Shanghai, China. J Hepatology. 2005;43(3):508–514
Torres DM, Harrison SA. Diagnosis and therapy of nonalcoholic steatohepatitis. Gastroenterology. 2008;134(6):1682–1698
Williams CD, Stengel J, Asike MI, Torres DM, Shaw J, Contreras M, Landt CL, Harrison SA. Prevalence of nonalcoholic fatty liver disease and nonalcoholic steatohepatitis among a largely middle-aged population utilizing ultrasound and liver biopsy: a prospective study. Gastroenterology. 2011;140(1):124–131
Lawson DH, Gray JM, McKillop C, Clarke J, Lee FD, Patrick RS. Diabetes mellitus and primary hepatocellular carcinoma. Q J Med. 1986;61(234):945–955
Regimbeau JM, Colombat M, Mognol P, Durand F, Abdalla E, Degott C, Degos F, Farges O, Belghiti J. Obesity and diabetes as a risk factor for hepatocellular carcinoma. Liver Transpl. 2004;10(2 Suppl 1):S69–S73
Larsson SC, Wolk A. Overweight, obesity and risk of liver cancer: a meta-analysis of cohort studies. Br J Cancer. 2007;97(7):1005–1008
Wang P, Kang D, Cao W, Wang Y, Liu Z. Diabetes mellitus and risk of hepatocellular carcinoma: a systematic review and meta-analysis. Diabetes/Metab Res Rev. 2012;28(2):109–122
Page JM, Harrison SA. NASH and HCC. Clin Liver Dis. 2009;13(4):631–647
Starley BQ, Calcagno CJ, Harrison SA. Nonalcoholic fatty liver disease and hepatocellular carcinoma: a weighty connection. Hepatology. 2010;51(5):1820–1832
Sanyal A, Poklepovic A, Moyneur E, Barghout V. Population-based risk factors and resource utilization for HCC: US perspective. Curr Med Res Opin. 2010;26(9):2183–2191
Ertle J, Dechene A, Sowa JP, Penndorf V, Herzer K, Kaiser G, Schlaak JF, Gerken G, Syn WK, Canbay A. Non-alcoholic fatty liver disease progresses to hepatocellular carcinoma in the absence of apparent cirrhosis. Int J Cancer. 2011;128(10):2436–2443
Hashimoto E, Yatsuji S, Tobari M, Taniai M, Torii N, Tokushige K, Shiratori K. Hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. J Gastroenterol. 2009;44(Suppl 19):89–95
Ascha MS, Hanouneh IA, Lopez R, Tamimi TA, Feldstein AF, Zein NN. The incidence and risk factors of hepatocellular carcinoma in patients with nonalcoholic steatohepatitis. Hepatology. 2010;51(6):1972–1978
Adams LA, Lymp JF, Sauver JS, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology. 2005;129(1):113–121
White DL, Kanwal F, El-Serag HB. Association between nonalcoholic fatty liver disease and risk for hepatocellular cancer, based on systematic review. Clin Gastroenterol Hepatol. 2012;10(12):1342–1359
Torres DM, Harrison SA. Nonalcoholic steatohepatitis and noncirrhotic hepatocellular carcinoma: fertile soil. Semin Liver Dis. 2012;32(1):30–38
Dupont-Bierre E, Compagnon P, Raoul JL, Fayet G, de Lajarte-Thirouard AS, Boudjema K. Resection of hepatocellular carcinoma in noncirrhotic liver: analysis of risk factors for survival. J Am Coll Surg. 2005;201(5):663–670
Lang H, Sotiropoulos GC, Brokalaki EI, Schmitz KJ, Bertona C, Meyer G, Frilling A, Paul A, Malago M, Broelsch CE. Survival and recurrence rates after resection for hepatocellular carcinoma in noncirrhotic livers. J Am Coll Surg. 2007;205(1):27–36
Lean ME, Han TS, Morrison CE. Waist circumference as a measure for indicating need for weight management. BMJ. 1995;311(6998):158–161
Kleiner DE, Brunt EM, Van Natta M, Behling C, Contos MJ, Cummings OW, Ferrell LD, Liu YC, Torbenson MS, Unalp-Arida A, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41(6):1313–1321
Bruix J, Sherman M, American association for the study of liver D. Management of hepatocellular carcinoma: an update. Hepatology. 2011;53(3):1020–1022
Sanyal AJ, Brunt EM, Kleiner DE, Kowdley KV, Chalasani N, Lavine JE, Ratziu V, McCullough A. Endpoints and clinical trial design for nonalcoholic steatohepatitis. Hepatology. 2011;54(1):344–353
Duan XY, Qiao L, Fan JG. Clinical features of nonalcoholic fatty liver disease-associated hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2012;11(1):18–27
Schutte K, Schulz C, Poranzke J, Antweiler K, Bornschein J, Bretschneider T, Arend J, Ricke J, Malfertheiner P. Characterization and prognosis of patients with hepatocellular carcinoma (HCC) in the non-cirrhotic liver. BMC gastroenterol. 2014;14:117
Hu W, Feng Z, Eveleigh J, Iyer G, Pan J, Amin S, Chung FL, Tang MS. The major lipid peroxidation product, trans-4-hydroxy-2-nonenal, preferentially forms DNA adducts at codon 249 of human p53 gene, a unique mutational hotspot in hepatocellular carcinoma. Carcinogenesis. 2002;23(11):1781–1789
Hashimoto E, Tokushige K. Hepatocellular carcinoma in non-alcoholic steatohepatitis: growing evidence of an epidemic? Hepatol Res. 2012;42(1):1–14
Alexander J, Torbenson M, Wu TT, Yeh MM. Non-alcoholic fatty liver disease contributes to hepatocarcinogenesis in non-cirrhotic liver: a clinical and pathological study. J Gastroenterol Hepatol. 2013;28(5):848–854
Alkofer B, Lepennec V, Chiche L. Hepatocellular cancer in the non-cirrhotic liver. J Visc Surg. 2011;148(1):3–11
Leung C, Yeoh SW, Patrick D, Ket S, Marion K, Gow P, Angus PW. Characteristics of hepatocellular carcinoma in cirrhotic and non-cirrhotic non-alcoholic fatty liver disease. World J Gastroenterol. 2015;21(4):1189–1196
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Bashar Mohamad, Vaishal Shah, Mykola Onyshchenko, Mohammed Elshamy, Federico Aucejo, Rocio Lopez, Ibrahim A. Hanouneh, Razan Alhaddad, Naim Alkhouri declare that they have no conflict of interest.
Informed consent
Informed consent was obtained from the patients before any procedure or therapy was applied.
Compliance with ethical standards
All procedures followed were in accordance with the ethical standards of the responsible committees on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Financial support
Supported by the ACG Junior Faculty Development Award to Naim Alkhouri.
Rights and permissions
About this article
Cite this article
Mohamad, B., Shah, V., Onyshchenko, M. et al. Characterization of hepatocellular carcinoma (HCC) in non-alcoholic fatty liver disease (NAFLD) patients without cirrhosis. Hepatol Int 10, 632–639 (2016). https://doi.org/10.1007/s12072-015-9679-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-015-9679-0