Abstract
Purpose
This study aimed to evaluate the efficacy and safety of entecavir, lamivudine and telbivudine for treating patients with HBV-ACLF and to validate the Tongji prognostic predictor model (TPPM) in these patients.
Methods
In this retrospective study, we enrolled 283 patients with HBV-ACLF (100 treated with entecavir, 98 treated with lamivudine and 85 treated with telbivudine). There were no significant differences in baseline clinical and virological characteristics among patients treated with entecavir, telbivudine or lamivudine.
Results
There were no significant differences in the 4- and 12-week survival rates of entecavir-, telbivudine- and lamivudine-treated patients (79.00, 81.18 and 86.73 %, respectively, at 4 weeks; 67.00, 65.88 and 73.47 %, respectively, at 12 weeks). Patients in all three groups achieved an improvement in the model for end-stage liver disease (MELD) score. Using the Hosmer-Lemeshow test, the validation of the TPPM score for HBV-ACLF demonstrated a good degree of fit with disease prognosis. Based on this unique group of patients, the TPPM score with an AUC of 0.787 was superior to the MELD score, which had an AUC of 0.736 in the prediction of 12-week mortality. The TPPM had an AUC of 0.733, and the MELD score had an AUC of 0.672 in the prediction of 4-week mortality. Using a cutoff value of 0.22 for 12-week mortality prediction by the TPPM, the positive predictive value was 49.66 %, with a negative predictive value of 89.55 %.
Conclusion
Treatment with nucleoside analogs including entecavir, lamivudine and telbivudine prevented disease progression and increased the survival of patients with HBV-ACLF. Validation of the established TPPM scoring system in this study confirmed its superior predictive value for HBV-ACLF patients when compared with the MELD system.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV) infection is a major public health problem, especially in Asia, and the World Health Organization (WHO) reported approximately 350–400 million cases of chronic HBV infection worldwide [1, 2]. In most Asian countries, chronic hepatitis B infection constitutes almost 70 % of the underlying liver disease in acute-on-chronic liver failure (ACLF). Other morbidities included alcoholic cirrhosis, autoimmune liver disease and genetic metabolic disease. However, in China, HBV-related ACLF accounts for more than 80 % of all ACLF cases. Complications such as spontaneous bacterial peritonitis (SBP, 25 %), hepatorenal syndrome (HRS, 12 %), hepatic encephalopathy (HE, >20 %), upper gastrointestinal bleeding, pneumonia and urinary tract infections are common in ACLF patients and could increase mortality to approximately 80 % in the absence of liver transplantation [3–6]. Although a number of factors play a role in the etiology and progression of HBV-ACLF, the syndrome is not well understood. There is currently no effective therapeutic modality for patients with HBV-ACLF other than liver transplantation [6, 7]. Most HBV-ACLF patients receive symptomatic and supportive treatment, artificial liver support systems, preventive treatment for complications, antiviral treatment, immunomodulatory regimens and correction of coagulation disorders [3, 8, 9]. There has been a recent focus on antiviral therapy to treat HBV-ACLF [10, 11]. Based on Asian-Pacific Association for the Study of the Liver (APASL) consensus, nucleoside analogs such as entecavir, telbivudine and lamivudine have been recommended since 2009 as antiviral therapy for HBV-ACLF [12].
The challenge of finding liver donors makes the prediction of prognosis very important during the management of HBV-ACLF. Studies showed that HBV-ACLF patients treated with nucleoside analogs (NAs) had a better prognosis compared to the non-NA-treated group, and antiviral therapy was an independent beneficial factor of survival [13–15]. However, these studies failed to systematically compare the efficacy of antiviral agents and to indicate the optimal choice of nucleoside analog for HBV-ACLF patients. We conducted this retrospective study to assess the clinical efficacy of therapeutic NAs in HBV-ACLF patients. We enrolled three groups of HBV-ACLF patients who were treated for 12 weeks with entecavir, telbivudine or lamivudine, respectively. Response to treatment was evaluated based on clinical features and laboratory tests as well as imaging examinations. We also compared survival rates of the three groups.
The MELD score has been widely applied in liver transplantation based on its simplicity, accuracy and subjectivity of use in daily clinical practice. However, it is not clear whether the MELD score is related to the prognosis of patients with HBV-ACLF, and there is an urgent need to improve the predictive accuracy of the scoring model in HBV-ACLF. We previously demonstrated the value of using the TPPM scoring system to predict the prognosis of patients with HBV-ACLF [9]. The present study was conducted to validate our earlier data.
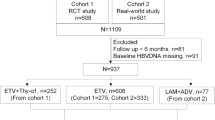
Patients and methods
Patients
In this retrospective study, we enrolled 283 patients with HBV-ACLF who were hospitalized at the Infectious Disease Department of Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, between 2007 and 2011. We analyzed the clinical manifestations and laboratory tests of all 283 patients (253 males and 30 females). Patients were divided into three groups: the entecavir group had 100 patients, the telbivudine group had 85 patients, and the lamivudine group had 98 patients. All patients were NA-treatment naive. We set the endpoint of observation as 12 weeks after initiation of NAs treatment, since a number of patients primarily treated with entecavir would choose another nucleoside analog at 12 weeks because of the high expense of entecavir.
All patients received standard medical treatment as well as one of the oral nucleoside analogs (ETV, LAM or LdT). The standard medications included but were not limited to vitamin K1 (10 mg Qd), compound glycyrrhizin injection (160 mg Qd), hepatocyte growth-promoting factors (pHGF, 120 μg Qd), transmetil (1gQd) and artificial liver support system (ALSS) with indications. The timing for NA treatment was within 3 days of the patients’ hospital administration with an HBV DNA positivity assay. A selection of NAs was decided after an extensive discussion between clinicians and patients based upon patients’ insurance condition and willingness. ALSS is a plasma exchange system used to obtain more time for hepatocytes to regenerate. Those patients with TBil > 171 μmol/l were recommended to receive plasma exchange (2,000 ml once a week) using Plasauto IQ (Asahi Medical Co., Ltd., Tokyo, Japan). The proportions of patients who received plasma exchanges were comparable among the three groups. No significant differences in the total number of plasma exchanges were observed among the three groups, which demonstrated the minimal influence of plasma exchange on the clinical outcome. Coagulation factors were supplemented with fresh plasma and cryoprecitation, which were regularly supplied via intravenous drip. Hospitalized patients were closely monitored during treatment for clinical manifestations of disease. Grade of hepatic encephalopathy, impaired coagulation [international normalized ratio (INR) and prothrombin time], and serum liver enzyme and bilirubin levels were measured every week for the first month and monthly thereafter. Telephone follow-up calls after patients left the hospital helped to confirm the continuation of nucleoside analogs and to record specific survival times.
Diagnosis criteria of HBV-ACLF
Patients who met the diagnostic criteria and without exclusion criteria were admitted to the study. HBV-ACLF diagnosis was based on both the local and Asian-Pacific criteria. HBV-ACLF diagnostic criteria from the recommendations of the APASL [12] included jaundice and coagulopathy, complicated within 4 weeks by ascites and/or encephalopathy, in a patient with previously diagnosed or undiagnosed chronic liver disease. The presence of jaundice [serum bilirubin >5 mg/dl (85 μmol/l)] and coagulopathy (INR >1.5 or prothrombin activity <40 %) is a mandatory criterion. Ascites and/or encephalopathy were determined by experienced physicians. Based on the Chinese criteria, HBV-ACLF was defined as chronic decompensated liver disease, serious debilitation and dysfunction of the alimentary tract, with TBil >171 μmol/l or an increase of TBil >17.1 μmol/l/day, and PTA <40 % [16]. HBsAg positivity for at least 6 months, serum bilirubin ≥5/dl (85 μmol/l) and INR ≥1.5 were additional criteria, consistent with the APASL recommendations. At baseline, there were no significant differences for the proportions of patients with cirrhosis among the three groups, 27.55 % (27/98) in LVD, 31.76 % (27/85) in LdT and 28 % (28/100) in ETV-treated groups, respectively. Biochemical tests including alanine aminotransferase (ALT) or aspartate aminotransferase (AST), total bilirubin (TBIL), albumin levels (ALB), serum creatine (sCR), blood urea nitrogen (BUN), and INR as well as routine blood sugar and electrolyte panels were performed by standard laboratory procedures. All study patients were negative for IgM anti-HAV, IgM anti-HEV and anti-HCV. HBV DNA was detected and quantitated by polymerase chain reaction (PCR), with a detection range of 5.0E2–1.0E8 IU/ml. Complications such as ascites, pulmonary infection, SBP, GI bleeding, HRS and/or HE, which often increase the hospitalization course and mortality in HBV-ACLF patients, were diagnosed by experienced clinicians.
Exclusion criteria Patients with HCV/HIV infection or autoimmune hepatitis, CHB patients who had received anti-HBV therapy with other NAs or interferon within the past 6 months, and patients with hepatocellular carcinoma, liver transplantation, serious cardiovascular and/or respiratory disease and other severe illnesses with high risk of short-term mortality were all excluded.
There was no significant difference in the clinical (age, sex, MELD score and pretreatment liver function) or virological characteristics (HBV-DNA level) between groups. Baseline characteristics of patients are shown in Table 1.
Laboratory tests
Standard ELISA assays (Kehua Biological Corp., Shanghai, China) were used to analyze HBsAg, HBsAb, HBeAg, HBeAb, HBcAb, IgM anti-hepatitis A virus (HAV) antibody and anti-hepatitis C virus (HCV) antibody levels according to the manufacturer’s instructions. HBV DNA was measured with a Fluocycle real-time polymerase chain reaction (PCR) system (Kehua Biological Corp., Shanghai, China).
The TPPM and MELD score
In our previous study, the Tongji prognostic predictor model (TPPM) [11] was calculated as:
The MELD score calculated from three objective variables (total bilirubin, serum creatine and INR) has been validated as a predictor of survival and disease severity for allocation of donor livers. In this study, the MELD score was analyzed as an independent variable [17, 18].
Unit conversion: TBil 1 mg/dl = 17.1 μmol/l; Cr 1 mg/dl = 88.4 μmol/l.
Statistical analysis
Data collection and analysis were undertaken in compliance with the regulations of the Tongji Hospital Medical Records Room and with the approval and supervision of the Tongji Hospital Research Institutional Review Board.
Statistical analyses were performed with Statistical Product and Service Solutions (SPSS) release 17.0 for Windows (SPSS, Inc., Chicago, IL).
Quantitative data were expressed as mean ± standard deviation (SD). One-way analysis of variance (ANOVA), t-test or the nonparametric Mann-Whitney U test was used to analyze data. Chi-square test or Fisher’s exact test was performed for comparison of qualitative data. A p value < 0.05 was considered to indicate statistical significance.
The accuracy of the TPPM and MELD scores in estimating the prognosis of patients was compared by ROC statistical analysis. The validity of the models was measured by means of the concordance (c) statistics (equivalent to the area under the ROC curve). The ROC area under the curve was compared by the DeLong’s test. Correlation between the scores was measured with Spearman’s rank-sum correlation test.
Results
HBV-ACLF patients treated with entecavir, telbivudine and lamivudine had similar survival curves
The mortality of HBV-ACLF patients at 4 weeks was 21.00 % for the ETV group, 18.82 % for the LdT group and 13.27 % for the LVD group; mortality at 8 weeks was 31.00 % for the ETV group, 34.12 % for the LdT group and 25.51 % for the LVD group; mortality at the end of 12 weeks was 33.00 % for the ETV group, 34.12 % for the LdT group and 26.53 % for the LVD group, respectively. Although LVD-treated patients showed a slightly lower mortality, there were no statistically significant differences in survival curves among the three groups at any of the time points after initiation of anti-viral therapy (p = 0.48, Fig. 1).
Patients treated with entecavir, telbivudine and lamivudine had similar improvements in serum biochemistry biomarkers
Results of laboratory tests were compared to evaluate the efficacy of the three agents at different time points. An analysis was done on ALT, AST, TBIL, BUN and Cr levels in the three groups at each time point and compared different time points in each group. There were no significant differences except for a slightly higher Cr level in ETV-treated patients at the third week of treatment (Fig. 2). After 2 weeks of anti-viral therapy, Cr levels were 0.86 ± 0.52 mg/dl in the ETV group (n = 89), 0.67 ± 0.78 mg/dl in the LdT group (n = 74) and 0.69 ± 0.21 mg/dl in the LVD group (n = 89) (p < 0.05). However, this difference disappeared at the fourth week of treatment.
Entecavir, telbivudine and lamivudine improved MELD scores in HBV-ACLF patients
A declining trend in MELD scores was observed in the three groups of HBV-ACLF patients with progressing time points. The ETV-treated group showed a declining trend from baseline (19.39 ± 5.08) to the third week (18.86 ± 7.11) and then to the fourth week (18.89 ± 7.09); the LVD-treated group showed a decline from baseline (20.00 ± 4.78) to the third week (16.93 ± 6.28) and then to the fourth week (15.13 ± 5.46), and the LdT-treated group showed a decline from baseline (19.82 ± 5.36) to the third week (16.81 ± 6.33) and to the fourth week (16.15 ± 7.34). There was a statistically significant difference in MELD scores (p < 0.05) in the LdT- and LVD-treated survivors after 2 weeks of anti-viral therapy, while there was no significant difference in MELD scores in the ETV-treated group at the different time points (Fig. 3). Additionally, there was no statistical difference in MELD scores among the groups at any of the time points. The declining trend of MELD scores in the LdT and LVD groups could be a predicator of benign outcome. Although mortality in the LVD group was initially similar to those of the LdT and ETV groups, it was lower than in the ETV and LdT groups after the third week, possibly because of the continuous decline in MELD scores (Fig. 1). Interestingly, the ETV group and LdT groups had a similar mortality, despite the difference in MELD scores.
HBV-ACLF patients with cirrhosis had a higher incidence of complications
HBV-ACLF patients usually suffer from a number of complications. In our study there was no statistical difference in the occurrence of complications among the three groups (Table 2).
HBV-ACLF patients with cirrhosis had a significantly higher risk of complications compared to those without cirrhosis (p < 0.05). These complications mainly included ascites, spontaneous bacterial peritonitis, hepatorenal syndrome and gastrointestinal bleeding (Table 3). However, patients with or without cirrhosis achieved a similar mortality (p = 0.887).
Validation of the TPPM
The MELD score consists of three objective parameters, TBIL, Cr and INR, which indicate the severity of the liver condition. The TPPM system is a novel model that calculates the TBIL, INR, number of complications and HBV copy number. This model pays close attention to multiorgan disorders and takes the pathogen (HBV) into account. In order to validate the efficacy of TPPM in the prediction of short-term mortality, we compared the TPPM and MELD (Fig. 4). A 4-week mortality prediction in HBV-ACLF patients showed that the AUCs (areas under curve) of TPPM and MELD were 0.733 and 0.670 (Z = 1.58, p = 0.11), respectively (Fig. 4A). A 12-week mortality prediction showed that the AUCs of TPPM and MELD were 0.786 and 0.738 (Z = 1.55, p = 0.12), respectively (Fig. 4B). The TPPM, which takes into account the HBV copy number, was more accurate in predicting outcomes of HBV-ACLF patients compared to the MELD score, which was consistent with the results obtained by Ma et al. [9]. Using a cutoff of 0.22 for the 12-week mortality prediction by the TPPM, sensitivity was 84.09 %, specificity was 61.54 %, positive predictive value was 49.66 %, and negative predictive value was 89.55 %. Using a cutoff of 0.27 for the 4-week mortality prediction by the TPPM, the sensitivity was 78 %, specificity was 54.94 %, positive predictive value was 27.83 %, and negative predictive value was 92.09 %.
Prediction of 4-week (A, Z = 1.58, p = 0.11) and 12-week (B, Z = 1.55, p = 0.12) survival in HBV-related ACLF patients using the MELD and TPPM. AUCs of the TPPM were 0.733 and 0.786, respectively, in the prediction of 4- and 12-week mortality compared to the MELD score, which had AUCs of 0.670 and 0.738, respectively
Discussion
HBV-ACLF is a specific clinical syndrome with a high mortality rate. An overactive immune response initiated by HBV, especially the CTL reaction to infected hepatocytes, plays a key role in the pathogenesis of HBV-ACLF and is necessary for HBV clearance; it causes significant necrosis and apoptosis of hepatocytes [19–22]. Antiviral therapy has been shown to effectively inhibit active HBV replication and improve hepatic function and short-term outcomes of HBV-ACLF [9, 12, 13, 15, 23], suggesting that patients with HBV-ACLF could benefit from earlier antiviral treatment with NAs.
It was previously demonstrated that entecavir treatment prevented disease progression and increased the survival of patients with HBV-ACLF. Entecavir efficiently inhibited HBV replication and subsequently might modulate the expanded host immune response against HBV-infected hepatocytes [1, 24–28]. Thus, early initiation of antiviral therapy has the advantage of rapidly controlling HBV replication and alleviating immune damage to hepatocytes. Survival in patients receiving standard internal medication plus additional entecavir treatment was significantly higher than in patients receiving standard internal medications without an NA [9]. In this study, we showed the efficacy of ETV, LdT and LVD in HBV-ACLF patients. Our data showed no significant difference in short-term survival of HBV-ACLF patients treated with ETV, LdT or LVD. We evaluated the effect of antiviral therapy on MELD scores. After 2 weeks of NA treatment, LdT and LVD survivors had a significant decrease in MELD scores, although this was not seen in ETV-treated patients. The specific mechanism underlying this difference among the NAs remains unclear. Since lactic acidosis in entecavir-treated patients has only been reported recently [29], lactate levels were not regularly checked in our study, and none of the patients had reduction of the entecavir dose. In our study, we showed that ETV, LdT and LVD were well tolerated by HBV-ACLF patients and that antiviral treatment prevented disease progression. Entecavir treatment has previously been reported to be associated with increased short-term mortality in patients with severe acute exacerbation of chronic hepatitis B but achieves better virological response in the long run [30]. Long-term suppression of HBV has been shown to improve liver biochemical and histological characteristics [20, 21, 31, 32]. It is interesting to note that discontinuation of NAs resulted in fatalities due to a rebound of HBV and exacerbation of CHB [23, 33].
Complications associated with HBV-ACLF include infection (SBP, pulmonary infection, urinary infection or biliary infection), hepatorenal syndrome, hepatic encephalopathy and upper gastrointestinal hemorrhage, which all increase the risk of mortality [5, 34–37]. We showed no significant difference in the total occurrence of complications among the three NA-treated groups. Interestingly, we found a significantly higher incidence of complications with inclusion of ascites, SBP, HRS and GI bleeding among HBV-ACLF patients with cirrhosis, possibly due to portal hypertension. However, it was previously shown that there was no significant difference in mortality between HBV-ACLF patients with and without cirrhosis [38]. This could be attributed to intensive internal treatment to prevent short-term mortality of patients with HBV-ACLF.
Studies showed that TBIL, Cr and INR levels are associated with mortality and patients with high MELD scores are more likely to have a worse outcome [17, 39]. Ma et al. [9] collected clinical data from 248 HBV-related ACLF patients to establish a novel model (Tongji prognostic predictor model, TPPM), which predicted the prognosis of HBV-ACLF patients. The TPPM was shown to be superior to the MELD. The exclusion of the HBV etiology was a possible reason for the MELD to be less applicable to these specific patients. We compared TPPM and MELD scores in the 283 NA-treated patients and showed that TPPM had a higher discriminative power with a larger AUC compared to MELD in the prediction of 4- or 12-week survival. It is important to note that HBV infection triggers an immune attack on hepatocytes and then cascades to a systematic response, resulting in complications. Our data suggest that TPPM scores, which are calculated taking into account the HBV copy number, are superior to the MELD system in predicting outcomes of HBV-related ACLF patients. The TPPM had a higher NPV compared to the MELD score, suggesting this model is more specific and accurate to predict survival for this unique group of patients with ACLF induced by HBV. It also strongly suggests that timely administration of NAs and standard medications are important treatment strategies, which facilitate over 60 % of the patients avoiding liver transplantation in our clinical settings. One limitation of this study is that it is a single-center retrospective cohort study of acute-on-chronic liver failure. The general applicability of the TPPM system needs to be confirmed further by prospective evaluation of HBV-related liver diseases.
In conclusion, nucleoside analogs including entecavir, lamivudine and telbivudine treatment prevented disease progression and increased the short-term survival of patients with HBV-ACLF. Validation of the established TPPM scoring system in this study confirmed its superior predictive value for HBV-ACLF patients when compared with MELD.
References
Lai CL, Yuen MF. The natural history and treatment of chronic hepatitis B: a critical evaluation of standard treatment criteria and end points. Ann Intern Med 2007;147:58–61
Liaw YF. Hepatitis B virus replication and liver disease progression: the impact of antiviral therapy. Antivir Ther 2006;11:669–679
Laleman W, Verbeke L, Meersseman P, Wauters J, van Pelt J, Cassiman D, et al. Acute-on-chronic liver failure: current concepts on definition, pathogenesis, clinical manifestations and potential therapeutic interventions. Expert Rev Gastroenterol Hepatol 2011;5:523–537 quiz 537
Jalan R, Williams R. Acute-on-chronic liver failure: pathophysiological basis of therapeutic options. Blood Purif 2002;20:252–261
Graziadei IW. The clinical challenges of acute on chronic liver failure. Liver Int 2011;31(Suppl 3):24–26
Wong GL, Wong VW, Choi PC, Chan AW, Chim AM, Yiu KK, et al. Increased liver stiffness measurement by transient elastography in severe acute exacerbation of chronic hepatitis B. J Gastroenterol Hepatol 2009;24:1002–1007
Olson JC, Kamath PS. Acute-on-chronic liver failure: concept, natural history, and prognosis. Curr Opin Crit Care 2011;17:165–169
Jindal A, Kumar M, Sarin SK. Management of acute hepatitis B and reactivation of hepatitis B. Liver Int 2013;33(Suppl 1):164–175
Ma K, Guo W, Han M, Chen G, Chen T, Wu Z, et al. Entecavir treatment prevents disease progression in hepatitis B virus-related acute-on-chronic liver failure: establishment of a novel logistical regression model. Hepatol Int 2012;6:735–743
Garg H, Sarin SK, Kumar M, Garg V, Sharma BC, Kumar A. Tenofovir improves the outcome in patients with spontaneous reactivation of hepatitis B presenting as acute-on-chronic liver failure. Hepatology 2011;53:774–780
Seto WK, Lai CL, Yuen MF. Acute-on-chronic liver failure in chronic hepatitis B. J Gastroenterol Hepatol 2012;27:662–669
Sarin SK, Kumar A, Almeida JA, Chawla YK, Fan ST, Garg H, et al. Acute-on-chronic liver failure: consensus recommendations of the Asian Pacific Association for the study of the liver (APASL). Hepatol Int 2009;3:269–282
Chen T, He Y, Liu X, Yan Z, Wang K, Liu H, et al. Nucleoside analogues improve the short-term and long-term prognosis of patients with hepatitis B virus-related acute-on-chronic liver failure. Clin Exp Med 2012;12:159–164
Cui YL, Yan F, Wang YB, Song XQ, Liu L, Lei XZ, et al. Nucleoside analogue can improve the long-term prognosis of patients with hepatitis B virus infection-associated acute on chronic liver failure. Dig Dis Sci 2010;55:2373–2380
Sun LJ, Yu JW, Zhao YH, Kang P, Li SC. Influential factors of prognosis in lamivudine treatment for patients with acute-on-chronic hepatitis B liver failure. J Gastroenterol Hepatol 2010;25:583–590
Liver Failure and Artificial Liver Group CSoID, Chinese Medical Association, Severe Liver Diseases and Artificial Liver Group, Chinese Society of Hepatology. Diagnostic and treatment guidelines for liver failure. Chin J Hepatol 2006;14:643–646
Freeman RB Jr. Model for end-stage liver disease (MELD) for liver allocation: a 5-year score card. Hepatology 2008;47:1052–1057
Mao W, Ye B, Lin S, Fu Y, Chen Y. Prediction value of model for end-stage liver disease scoring system on prognosis in the acute on chronic liver failure patients with plasma exchange treatment. ASAIO J 2010;56:475–478
Fattovich G. Natural history and prognosis of hepatitis B. Semin Liver Dis 2003;23:47–58
Lok AS, McMahon BJ. Chronic hepatitis B. Hepatology 2007;45:507–539
Hoofnagle JH, Doo E, Liang TJ, Fleischer R, Lok AS. Management of hepatitis B: summary of a clinical research workshop. Hepatology. 2007;45:1056–75
Lee WM. Hepatitis B virus infection. N Engl J Med 1997;337:1733–1745
Wang J, Wang M, Huang Y. Acute liver failure resulting from discontinuation of nucleoside analogues in chronic hepatitis B patients: a report of two cases. Scand J Infect Dis 2013;45:158–160
Zheng Y, Huang Z, Chen X, Tian Y, Tang J, Zhang Y, et al. Effects of telbivudine treatment on the circulating CD4(+) T-cell subpopulations in chronic hepatitis B patients. Mediators Inflamm 2012;2012:789859
Zhao S, Tang L, Fan X, Chen L, Zhou R, Dai X. Comparison of the efficacy of lamivudine and telbivudine in the treatment of chronic hepatitis B: a systematic review. Virol J 2010;7:211
Hadziyannis SJ, Vassilopoulos D. Telbivudine in the treatment of chronic hepatitis B. Expert Rev Gastroenterol Hepatol 2008;2:13–22
Matthews SJ. Entecavir for the treatment of chronic hepatitis B virus infection. Clin Ther 2006;28:184–203
Yao G, Chen C, Lu W, Ren H, Tan D, Wang Y, et al. Virologic, serologic, and biochemical outcomes through 2 years of treatment with entecavir and lamivudine in nucleoside-naive Chinese patients with chronic hepatitis B: a randomized, multicenter study. Hepatol Int 2008;2:486–493
Lange CM, Bojunga J, Hofmann WP, Wunder K, Mihm U, Zeuzem S, et al. Severe lactic acidosis during treatment of chronic hepatitis B with entecavir in patients with impaired liver function. Hepatology 2009;50:2001–2006
Wong VW, Wong GL, Yiu KK, Chim AM, Chu SH, Chan HY, et al. Entecavir treatment in patients with severe acute exacerbation of chronic hepatitis B. J Hepatol 2011;54:236–242
Lai CL, Yuen MF. Chronic hepatitis B—new goals, new treatment. N Engl J Med 2008;359:2488–2491
Dienstag JL, Wei LJ, Xu D, Kreter B. Cross-study analysis of the relative efficacies of oral antiviral therapies for chronic hepatitis B infection in nucleoside-naive patients. Clin Drug Investig 2007;27:35–49
Lim SG, Wai CT, Rajnakova A, Kajiji T, Guan R. Fatal hepatitis B reactivation following discontinuation of nucleoside analogues for chronic hepatitis B. Gut 2002;51:597–599
Marsden PA, Ning Q, Fung LS, Luo X, Chen Y, Mendicino M, et al. The Fgl2/fibroleukin prothrombinase contributes to immunologically mediated thrombosis in experimental and human viral hepatitis. J Clin Invest 2003;112:58–66
Zhu CL, Yan WM, Zhu F, Zhu YF, Xi D, Tian DY, et al. Fibrinogen-like protein 2 fibroleukin expression and its correlation with disease progression in murine hepatitis virus type 3-induced fulminant hepatitis and in patients with severe viral hepatitis B. World J Gastroenterol 2005;11:6936–6940
Zou Y, Chen T, Han M, Wang H, Yan W, Song G, et al. Increased killing of liver NK cells by Fas/Fas ligand and NKG2D/NKG2D ligand contributes to hepatocyte necrosis in virus-induced liver failure. J Immunol 2010;184:466–475
Kumar A, Mishra SR, Sharma P, Sharma BC, Sarin SK. Clinical, laboratory, and hemodynamic parameters in portal hypertensive gastropathy: a study of 254 cirrhotics. J Clin Gastroenterol 2010;44:294–300
Yang WB, Chen EQ, Bi HX, Bai L, Chen XB, Feng P, et al. Different models in predicting the short-term prognosis of patients with hepatitis B virus-related acute-on-chronic liver failure. Ann Hepatol 2012;11:311–319
Lv XH, Liu HB, Wang Y, Wang BY, Song M, Sun MJ. Validation of model for end-stage liver disease score to serum sodium ratio index as a prognostic predictor in patients with cirrhosis. J Gastroenterol Hepatol 2009;24:1547–1553
Acknowledgements
Supported by research grants from the National Natural Science Foundation of China (NSFC81030007/NSFC81171558), Innovation Team Development Plan of the Ministry of Education (IRT1131).
Compliance with ethical requirements and Conflict of interest
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for inclusion in the study. Junshuai Wang, Ke Ma, Meifang Han, Wei Guo, Jiaquan Huang, Daofeng Yang, Xiping Zhao, Jiangxin Song, Deying Tian, Junying Qi, Yuancheng Huang and Qin Ning declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Junshuai Wang and Ke Ma have contributed equally to this study.
Rights and permissions
About this article
Cite this article
Wang, J., Ma, K., Han, M. et al. Nucleoside analogs prevent disease progression in HBV-related acute-on-chronic liver failure: validation of the TPPM model. Hepatol Int 8, 64–71 (2014). https://doi.org/10.1007/s12072-013-9485-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-013-9485-5