Abstract
Introduction
Bone marrow-derived cells (BMCs) include stem cells capable of self-renewal and differentiation into a variety of cell types. Administration of granulocyte colony-stimulating factor (G-CSF) induces the circulation of BMCs in the peripheral blood. A phase II prospective trial was carried out for evaluation of BMC mobilization induced by multiple courses of G-CSF in cirrhotic patients.
Patients and methods
Fifteen patients with advanced liver cirrhosis (Child-Pugh score ≥6 points) were enrolled and treated with a 3-day G-CSF course, administered at 3-month intervals for a total of four courses. BMC mobilization was assessed by evaluating CD34+ve cells using flow cytometry. Expressions of multiple hepatic and stem markers were assessed on mobilized CD34+ve cells. Feasibility and safety were explored; clinical and adverse events were compared to those of a control group. Telomere length was monitored to rule out early cell aging caused by G-CSF.
Results
A significant increase in G-CSF-induced circulating CD34+ve cells was consistently observed, although a progressive reduction of peak values was documented from cycle I to IV (p < 0.005). Mobilized CD34+ve cells expressed both stem and multiple hepatocyte markers, including mRNA of albumin and CYP2B6 (cytochrome P2 B6). Treatment was well tolerated, with no severe adverse events and no significant telomere length shortening following G-CSF. The procedure was safe. Overall, ten patients had either improved or had stable liver function tests (such as the Child-Pugh score), whereas five worsened and died from liver-related causes.
Conclusion
This study demonstrates that G-CSF can be safely administrated up to four times over a 1-year period in decompensated cirrhotic patients. The repeated BMC mobilization favors the circulation of stem cells coexpressing hepatic markers and mRNA of liver-related genes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several studies have documented the regenerative potential of human stem cells for the repair of damaged tissues. Bone marrow has been considered the most accessible source for the acquisition of adequate amounts of functionally active stem cells. Indeed, bone marrow-derived cells (BMCs) include multipotent stem cells capable of self-renewal and differentiation into a variety of adult cell types including hepatocytes. A number of reports have demonstrated that BM stem cells can be converted into hepatocyte-like cells in vitro and, in response to acute or chronic liver damage, can spontaneously populate the liver and contribute to hepatic regeneration [1–4]. However, the rate of BM stem cells capable of lodging in the liver, leading to possible regeneration of hepatic tissue, is ultimately very low [5]. After mobilization into the peripheral blood (PB), BM-derived CD34+ve cells coexpressing immature stem cell markers such as CD133 and CD117 (c-Kit) might home to the liver and may contribute to liver regeneration. A non-invasive and effective approach for obtaining large numbers of circulating BMCs is their mobilization by cytokines [6, 7]. Granulocyte colony-stimulating factor (G-CSF) is the most widely used cytokine for BMC mobilization purposes because of its high tolerability. Some reports have already shown the feasibility and potent BMC mobilization capacity of G-CSF in cirrhotic patients [8, 9]. Moreover, G-CSF treatment led to improved survival with signs of histological liver regeneration in animal models [10, 11]. More recently, the clinical benefit of G-CSF has been reported in patients with acute liver injury [12]. Mobilized CD34+ve cells can be easily collected in large amounts and re-infused as autologous cells through the hepatic vessels. Enhanced hepatic regeneration with signs of clinical improvement has been reported using this approach, confirming the potential for liver regeneration of mobilized BMCs [8, 13].
Several aspects regarding the possible use of G-CSF in patients with cirrhosis require further investigation including the degree of mobilization of immature cells after multiple courses, the possible expression of hepatic markers by mobilized cells and potential effects on liver function. This study is a phase II prospective trial carried out to evaluate the feasibility and safety of multiple procedures of BMC mobilization in patients with cirrhosis and signs of liver decompensation, and to characterize the liver signature of mobilized cells.
Patients and methods
Study patients and control group
Fifteen patients with advanced liver cirrhosis (Child-Pugh score ≥6 and MELD score ≥10) referred to our Hepatological Unit were enrolled and followed in a phase II prospective trial on the safety and feasibility of multiple courses of G-CSF, administered for 3 consecutive days. Eligibility and exclusion criteria are listed in the Supporting Information section: link-1. Patients with hepatocellular carcinoma and active alcohol abuse were excluded; alcohol intake had to be interrupted at least 12 months prior to enrollment and abstinence maintained during the entire follow-up study.
Adverse and clinical events occurring throughout the study in G-CSF treated patients were compared with those of a control group of 15 patients selected with the same inclusion/exclusion criteria, link-1, and matched to the study patients for the Child-Pugh score (±1), MELD score (±4), sex and age (±5 years). The control group was managed and monitored during the same time period and in the same way as the treated patients. The main clinical features of the patients entering the study protocol and of the control group are summarized in Table 1.
Experimental protocol
The protocol consisted of G-CSF (Myelostim®, Italfarmaco, Milan, Italy), given subcutaneously at a dose of 5 μg/kg every 12 h for 3 consecutive days. This is the standard protocol employed for BMC mobilization in healthy volunteer donors for hematopoietic stem cell transplantation and has already been utilized in previous mobilization protocols for patients with advanced liver failure [9, 12, 14]. G-CSF administration was repeated every 3 months for a total of four courses, in line with a recent report of multiple courses of G-CSF in patients with amyotrophic lateral sclerosis [15]. Subsequent to the entire treatment program, all patients were followed up for 12 months. The protocol was approved by the Regional Ethics Committee (Eudract no. 2008-003701-14), and the study was carried out according to the 1975 Declaration of Helsinki. All patients gave formal written informed consent before entering the study protocol.
Assessment of BMC mobilization
The degree of BMC mobilization was assessed by evaluating the number of circulating CD34+ve cells using flow cytometry, as described [9]. Circulating myeloid progenitor (CFU-GM) levels were determined using the clonogenic assay at baseline and following G-CSF administration, as described [18].
Immunophenotypic characterization of circulating CD34+ve cells
Two-color flow cytometry was used to characterize mobilized CD34+ve cells. Cells were double stained using anti-CD34-FITC or anti-CD34-PE (BD Biosciences, San Josè, CA) monoclonal antibodies in combination with one of the following monoclonal antibodies: anti-CD133-PE (marker of liver progenitor cells; Miltenyi Biotech, GmbH, Germany), anti-CD90-PE (Thy1; (BD Biosciences, Pharmigen, San Diego, CA), anti-CD184-FITC [CXCR4, stromal cell derived factor-1 (SDF-1) receptor; Medical and Biological Laboratories, Japan], anti-CD117-PE [c-KIT, stem cell factor (SCF) receptor, (BD Biosciences], and anti-cMET [hepatocyte growth factor (HGF) receptor; BD Biosciences]. A minimum of 150,000 cells per sample were acquired and analyzed using a FACSCalibur Flow Cytofluorimeter from BD using the Cell Quest PRO Software.
Plasma concentration of hematopoietic cytokines and hepatocyte growth factor
SDF-1 (stromal derived factor-1), SCF (stem cell factor) and HGF (hepatocyte growth factor) were measured at baseline and on day 4 following G-CSF administration using quantitative sandwich enzyme immunoassay kits (R&D Systems, Minneapolis, MN, USA) according to the manufacturer’s instructions.
Reverse-transcription polymerase chain reaction (RT-PCR) for mRNAs
Mobilized CD34+ve cells were evaluated for their possible content of hepatocyte-related mRNA. Details of the cell purification procedure are reported in the supporting information section: link-2.
Total RNA was extracted from purified CD34+ve cells using the RNeasy Plus Mini kit (Qiagen, Germany). The QuantiTect Primer Assay (Qiagen, Germany) was used for amplification of mRNA liver-specific markers, namely ALB_1 (albumin 1), AFP_1 (alpha-feto protein 1), HNF4A-1 (hepatocyte nuclear factor 4A) and CYP2B6_2 (cytochrome P2 B6). Details of the assay are reported in the supporting information section: link-3.
Detection of HCV RNA in mobilized CD34+ve cells
Total RNA extracted from immuno-purified CD34+ve cells collected from nine patients was available for HCV-RNA detection. Details are reported in the supporting information section: link-4.
Safety and clinical evaluation
To evaluate possible early and late side effects, clinical examination and biochemical data (including blood count, transaminases, glucose, albumin, bilirubin, prothrombine time, alfa-fetoprotein, serum creatinine, gamma-glutamyl transpeptidase, pseudocholinesterase) were recorded prior to treatment (at baseline), daily during G-CSF administration, monthly during the intermediate periods between G-CSF administration and 3 monthly for 12 months thereafter. The total study time was 21 months. Abdominal ultrasound (US) scans and portal US Doppler imaging were performed daily from day 0 to day 4 and every 3 months thereafter in order to evaluate changes in spleen diameter, portal flow and possible appearance of focal lesions. The Child-Pugh (CP) score, MELD scores and liver function tests were assessed in the study group at baseline and during treatment up to the final follow-up. Results were compared with analogous assessments performed in control patients during the observation period. In all patients, cirrhosis complications were treated with standard therapies, and infusion of albumin was performed following local guidelines (serum albumin <2 g/l with edema/ascites nonresponsive to diuretics or paracentesis >4l).
A breath test with [14C]-labeled aminopyrine was used as a non-invasive measure of cytochrome P-450 metabolic activity in liver function tests. Following ingestion of [14C]-aminopyrine, breath 14CO2 data were analyzed from patients with hepatic disease before and after treatment with G-CSF. Tests were based on 2 h sampling of breath 14CO2 produced by demethylation of [14C]-labeled aminopyrine to analyze the hepatic microsomal enzyme function.
Telomere evaluation
In order to rule out possible early aging of hematopoietic cells due to proliferative stress induced by repeated exposure to G-CSF, telomere length (TL) was determined by Southern blot analysis, as described [16]. The assay was performed on PB cells following each mobilization course. Results of TL from treated patients were compared to the known TL of age-matched normal subjects [17].
Statistical analysis
Categorical data were presented as absolute values and percentages, whereas continuous data were provided as median and range or mean and standard deviation (SD) as appropriate. Student’s t test was used for statistical comparison of quantitative and continuous data, whereas the Mann-Whitney U test was performed for categorical small sample size data. The Cox regression model was used to investigate the effect of various variables on survival time. A p-value <0.05 was regarded as statistically significant. Analyses were performed using a statistical software package (StatsDirect version 2.7.8) and GraphPad InStat 3, version 3.06 (GraphPad Software, Inc.).
Results
Assessment of BMC mobilization
Following G-CSF stimulation, a significant (p < 0.005) increase in circulating CD34+ve cells was observed in the peripheral blood of all patients, as shown in Fig. 1. The rate of CD34+ve cell mobilization varied remarkably between patients, ranging from 1.73 to 37.32 CD34+ve cells/μl at peak detection. The highest values of circulating CD34+ve cells were obtained during the first mobilization cycle, with a decreasing trend in the peak values from cycle I to IV (p < 0.005). Taking all courses into consideration, the rate of BMC mobilization was significantly lower (median peak value: 12.54/μl CD34+ve cells, range 3.4–37.3/μl) when compared with mobilization results from healthy stem cell donors stimulated with G-CSF observed at our Bone Marrow Transplantation Unit (median peak value: 36.89/μl CD34+ve cells, range 2.6–130.06/μl, p < 0.05). The peak value of mobilized CD34+ve cells was inversely proportional to spleen diameter (p = 0.046), but was unaffected by other demographic (age, sex, BMI, liver disease etiology), clinical and laboratory parameters. Four patients had progressive liver failure and died before concluding the study protocol; they showed similar values of mobilized CD34+ve cells compared to patients with better clinical basal conditions or to those that completed the protocol (median: 9.02 cells/μl, range 1.83–37.32 vs. 8.78 cells/μl, range 1.73–15.72), (p > 0.05).
The number of CD34+ve cells was also evaluated in the peritoneal ascites of three patients on the peak day of mobilization. Results demonstrated similar or even higher values of CD34+ve cells in the abdominal liquid compared to CD34+ve cells in the peripheral blood.
In order to further characterize BMC mobilization, the amount of circulating CFU-GM was evaluated during G-CSF treatment by means of an in vitro clonogenic assay. A significant increase in CFU-GM was recorded on day 4 of the treatment (774 CFU-GM/ml, range 68–4592) compared to basal pre-treatment values (35 CFU-GM/ml, range 5–528) (p < 0.001). Again, each G-CSF course led to a subsequent increase in CFU-GM, with a slight but not significant reduction in CFU-GM peak values at the fourth mobilization course.
Immunophenotypic characterization of circulating CD34+ve cells
The expression of early stem cell and epithelial markers by circulating CD34+ve cells is reported in Table 2. Immunophenotypic characterization was carried out prior to treatment and daily thereafter during G-CSF administration. All evaluated markers were expressed by circulating CD34+ve cells at basal conditions. No relevant differences in the percentage of CD34+ve cells coexpressing CD90 and CD117 markers were detected following G-CSF stimulation, while a significant increase in CD133/CD34+ve cells (p = 0.0015) and a significant reduction in CD184+ve and hepatocyte growth-factor receptor (c-Met) +ve/CD34+ve cells (p < 0.0001) were observed.
Expression of liver-related genes and HCV RNA in circulating CD34+ve cells
The expression of hepatocyte-specific mRNA was assessed in purified CD34+ve cells obtained from PB during mobilization. The expression of ALB and CYP2B6 mRNA was detectable in mobilized CD34+ve cells in 91 and 82 % of cases, respectively, while AFP and HNF4A-1 only in 1 % of cases. Similar results were observed in mobilized CD34+ve cells from healthy volunteer donors (data not shown).
The availability of purified CD34+ve cells enabled the investigation of the presence of HCV RNA in BMCs obtained from nine treated patients (4 HCV-related cirrhosis and 5 no-viral cirrhosis patients, used as controls). Using the RT-PCR assay, HCV RNA was detected in CD34+ve cells derived from all four HCV-related cirrhosis patients.
Plasma concentrations of hematopoietic cytokines and hepatocyte growth factor
Cytokine levels (SCF and SDF-1) and HGF were available at baseline and at peak day (day 4) after G-CSF administration in 12 treated patients and were compared with those of 6 healthy volunteers. SCF, SDF-1 and HGF values were significantly higher (p < 0.005) in cirrhotic patients compared to healthy subjects. Cytokine and HGF levels were elevated at both baseline and peak mobilization levels, without significant changes crosswise G-CSF administration, as shown in Fig. 2.
Safety assessment of repeated G-CSF administration
Overall, treatment was well tolerated, with no notable severe adverse events, the only major complaint being manageable bone pain in four patients. No significant modifications in liver enzymes or ultrasound and Doppler hepatic features were registered during the treatment period. As expected, white blood cells (WBC) significantly increased at each G-CSF course, with peak values between day 3 and 4 (p < 0.05) with a rapid return to pre-treatment values within a few days after G-CSF discontinuation. A minor reduction in platelets and a decrease in fasting morning glucose levels with no diet change were also observed. Two patients with mild chronic kidney disease showed a marked though transient increase in blood creatinine levels up to 3–4 mg/dl during cycles I and II; in both cases, kidney function was rapidly restored, and creatinine levels returned to basal values following adequate hydration and diuretic withdrawal. An increase in longitudinal diameter of the spleen was observed at the mobilization peak (median: 168 mm, range 126–210 mm) compared to pre-treatment diameters (median: 157 mm, range 125–170 mm) (p < 0.05). Spleen diameters returned to pre-treatment values at the end of each G-CSF treatment course in all patients. No significant adverse events were recorded in the post-treatment follow-up; no patient developed hepatocellular carcinoma, and alpha-feto protein levels remained stable.
In order to rule out possible telomere loss as a consequence of accelerated cell proliferation induced by G-CSF exposure, TL was evaluated in PB cells at each G-CSF course. No significant TL shortening was documented from cycles I to IV (Fig. 3). Our cirrhotic patients showed a progressive shortening of telomere terminal sequences related to aging similar to the trend observed in healthy subjects with a shortening rate of about 50 bp per year.
Exploratory clinical evaluations
Following the IV mobilization course, all treated patients were followed up for an additional 12 months. Liver-related complications throughout the study period did not differ in type or frequency in the G-CSF-treated patients compared to untreated patients (Table 3).
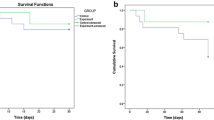
Eleven patients completed all four G-CSF courses and four died within the treatment period at 1,2, 8 and 8 months, respectively. Between study patients, at the end of the follow-up period, five patients (2 HCV, 1 NASH and 2 alcohol-related cirrhosis) showed an improvement in liver function tests (reduction of ≥2 points of CP score), and five (1 HCV, 1 HBV, 1 NASH and 2 alcohol-related cirrhosis) had stable values (change of ≤1 point in CP score), whereas the remaining five patients (1 HCV and 4 alcohol-related cirrhosis) (33 %) worsened and died during the treatment period or the further follow-up (1 patient). Overall, in treated patients a significant improvement in the Child-Pugh score (p < 0.05) was registered from baseline and crosswise G-CSF administration to the end of follow-up, whereas the MELD score did not change significantly. Details of the Child-Pugh and MELD scores changes during the study period are summarized in Fig. 4 and Table 4 in the Supporting Information section. Risk of mortality correlated with pre-treatment serum creatinine values (p = 0.01), whereas there was no association with other laboratory parameters. The survival rate during 21 months of follow-up was not different between treated and control patients. It should be noted that comorbidities, ischemic heart disease, insulin-dependent diabetes and chronic kidney disease stage >1 (GFR <89 ml/min/1.73 m2) affected the five patients who died during treatment or during follow-up (at months 1, 2, 8, 8 and 15, respectively) and contributed to the worst prognosis of these patients.
The aminopyrine breath test was carried out prior to and following treatment in nine patients; the c-aminopyrine peak and the dosing after 2 h showed an improvement in liver metabolism in four patients and remained unchanged in five, with results correlating with CP score improvement or stabilization.
Liver function tests did not show significant variations in the 15 control patients from baseline to the end of follow-up as detailed in Fig. 4. The Child-Pugh score improved in one patient (7 %) (decrease of <2 points in CP score), was stable in six (40 %) (±1 point in CP score) and worsened in eight; six of them died during the follow-up period (at months 1, 1, 2, 6, 16, 18, respectively). Two control patients developed hepatocellular carcinoma at 6 and 12 months after enrollment, respectively. Liver-related complications throughout the study period are reported in Table 3.
Discussion
This prospective trial reports the results of multiple BM stem cell mobilizations induced by repeated G-CSF courses in patients with advanced liver cirrhosis. The data demonstrate that G-CSF can be repeatedly and safely administrated over 1 year to cirrhotic patients without relevant side effects.
The study suggests that no adverse events could be attributed to the mobilization procedure. However, there are limiting factors for drawing conclusive clinical outcomes due to the low number of treated patients and to the unrandomized selection of control patients in this phase II trial study.
The extent of multiple BMC mobilization in cirrhotic patients was consistent, but remained significantly lower compared to that recorded in healthy donors [18, 19]. These results may be attributed to multiple causes, such as a long history of liver disease [20], coexisting chronic cardiopulmonary and kidney diseases, and spleen enlargement [21]. In our patients the peak values of CD34+ve cell mobilization were inversely proportional to the spleen diameter. Although mobilization is reported to be correlated to younger age [22], no relationship between the amount of CD34+ cell mobilization and age was reveled in this study, as reported [23]. Of interest, the peak values of circulating CD34+ve cells showed a decreasing trend from cycle I to cycle IV, in agreement with hematological studies showing that consecutive courses of chemotherapy and G-CSF treatment at short intervals can impair progenitor mobilization in peripheral blood [24, 25]. However, in response to G-CSF, despite these features, all cirrhotic patients were able to mobilize varying amounts of immature cells with functional properties tested in vitro with clonogenic assays similar to those from healthy donors.
This study also aimed to characterize the immunophenotypic features of the mobilized cells to describe their eventual potential contribution to liver regeneration. The concept that G-CSF promotes mobilization of immature cells that may lodge in the liver and differentiate into the hepatocyte lineage [26] is supported, in this study, by the finding that mobilized stem cells may also express surface markers and genes associated with liver differentiation. Mobilized cells showed the variable coexpression of several surface markers, including CD133, CD184 and c-Met (hepatocyte growth-factor receptor). Tissue-specific surface markers have been reported in cirrhotic patients as well as in patients with coronary artery disease and in amyotrophic lateral sclerosis (ALS) patients [27]. The increased CD133 expression is noteworthy because of the capacity of CD133+ve cells to differentiate in vitro into cells with hepatocyte-like features. A notable mobilization of CD133+ve expressing cells has been observed in healthy human liver donors after partial hepatectomy [28]. Moreover, purified CD34+ve cells obtained after G-CSF treatment express, in varying proportions, the early hepatocyte markers AFP and HNF4A-1 and the liver-specific genes, ALB and CYP2B6. Unfortunately, these cells, mobilized from hepatitis C patients, also contained HCV RNA, possibly limiting their specific therapeutic use.
Homing of circulating BMCs is a critical issue for the potential use of mobilized stem cells for regenerative purposes. Receptors for the cytokines SCF, HGF and SDF-1 are present on mobilized CD34+ve cells, as also previously demonstrated [9, 29]. The values of circulating SCF, HGF and SDF-1 were significantly higher in our cirrhotic patients than in healthy controls; also high levels of these cytokines have been documented in murine models of liver injury and regeneration in patients with liver cirrhosis of different etiologies [27–29]. SCF and its receptor, c-Kit, are involved in cell differentiation and hepatic chemotaxis [30], and HGF is involved in progenitor cell recruitment to the liver through an SCF-mediated mechanism. G-CSF administration is able to upregulate SDF-1 expression in an injured liver, determining an increasing concentration of SDF-1 from the BM to the injured liver via the peripheral blood [31]. It could be speculated that the chemoattractive effect of this gradient toward the liver may explain the reduction in CD34+ve cells coexpressing CD184 and c-Met surface antigens in the peripheral blood of our patients following G-CSF treatment.
In summary, a novel schedule of multiple courses of G-CSF treatment has been developed for cirrhotic patients and found to be safe and feasible. Repeated hematopoietic activation does not modify the degree of cell aging and cellular senescence of peripheral blood cells after the 1-year treatment, as measured by telomere length following each G-CSF cycle.
Consistent mobilization of immature CD34+ve cells from BM to peripheral blood was observed in all patients. The mobilization process was characterized by the increased circulation of liver-committed stem cells that could be suitable for organ regeneration approaches. During multiple G-CSF courses, some clinical benefit may be registered but not clearly demonstrated. Treated patients showed improvement in the Child-Pugh score during treatment persisting in the follow-up, but no improvement in the Meld score. Randomized studies on adequate numbers of patients appear to be necessary in order to establish the clinical usefulness of the mobilization procedure.
Abbreviations
- BMC:
-
Bone marrow-derived cells
- G-CSF:
-
Granulocyte colony-stimulating factor
- TL:
-
Telomere length
- PB:
-
Peripheral blood
- BM:
-
Bone marrow
- MELD:
-
Model for end-stage liver disease
- CFU-GM:
-
Colony-forming unit-granulocyte–macrophage
- SDF-1:
-
Stromal derived factor-1
- SCF:
-
Stem cell factor
- HGF:
-
Hepatocyte growth factor
- ALB_1:
-
Albumin 1
- AFP-1:
-
Alpha-feto protein 1
- HNF4A-1:
-
Hepatocyte nuclear factor 4A
- CYP2B6_2:
-
Cytochrome P2 B6
- RT-PCR:
-
Real time polymerase chain reaction
- US:
-
Ultrasound
- CP:
-
Child-Pugh
- SD:
-
Standard deviation
- WBC:
-
White blood cells
- c-Met:
-
Hepatocyte growth-factor receptor
References
Schwartz RE, Reyes M, Koodie L, Jiang Y, Blackstad M, Lund T, et al. Multipotent adult progenitor cells from bone marrow differentiate into functional hepatocyte-like cells. J Clin Invest 2002;109:1291–1302
Haga J, Wakabayashi G, Shimazu M, Tanabe M, Takahara T, Azuma T, et al. In vivo visualization and portally repeated transplantation of bone marrow cells in rats with liver damage. Stem Cells Dev 2007;16:319–328
Ng IO, Chan KL, Shek WH, Lee JM, Fong DY, Lo CM, et al. High frequency of chimerism in transplanted livers. Hepatology 2003;38:989–998
Gaia S, Cappia S, Smedile A, Bacillo E, Gaia E, Gubetta L, et al. Epithelial microchimerism: consistent finding in human liver transplants. J Gastroenterol Hepatol 2006;21:1801–1806
Herencia C, Rodriguez-Ariza A, Canalejo A, Naranjo A, Briceno FJ, Lopez-Cillero P, et al. Differential bone marrow hematopoietic stem cells mobilization in hepatectomized patients. J Gastrointest Surg 2011;15:1459–1467
Tarella C, Ferrero D, Bregni M, Siena S, Gallo E, Pileri A, et al. Peripheral blood expansion of early progenitor cells after high-dose cyclophosphamide and rhGM-CSF. Eur J Cancer 1991;27:22–27
Levesque JP, Winkler IG. Mobilization of hematopoietic stem cells: state of the art. Curr Opin Organ Transpl 2008;13:53–58
Spahr L, Lambert JF, Rubbia-Brandt L, Chalandon Y, Frossard JL, Giostra E, et al. Granulocyte-colony stimulating factor induces proliferation of hepatic progenitors in alcoholic steatohepatitis: a randomized trial. Hepatology 2008;48:221–229
Gaia S, Smedile A, Omede P, Olivero A, Sanavio F, Balzola F, et al. Feasibility and safety of G-CSF administration to induce bone marrow-derived cells mobilization in patients with end stage liver disease. J Hepatol 2006;45:13–19
Jin SZ, Meng XW, Sun X, Han MZ, Liu BR, Wang XH, et al. Granulocyte colony-stimulating factor enhances bone marrow mononuclear cell homing to the liver in a mouse model of acute hepatic injury. Dig Dis Sci 2010;55:2805–13
Li N, Zhang L, Fang B. Human CD34+ cells mobilized by granulocyte colony-stimulating factor ameliorate radiation-induced liver damage in mice. Stem Cell Res Ther 2010;1:22. doi:10.1186/scrt22.
Garg V, Garg H, Khan A, Trehanpati N, Kumar A, Sharma BC, et al. Granulocyte colony-stimulating factor mobilizes CD34(+) cells and improves survival of patients with acute-on-chronic liver failure. Gastroenterology 2012;142(505–512):e501
Dar A, Goichberg P, Shinder V, Kalinkovich A, Kollet O, Netzer N, et al. Chemokine receptor CXCR4-dependent internalization and resecretion of functional chemokine SDF-1 by bone marrow endothelial and stromal cells. Nat Immunol 2005;6:1038–1046.
Corradini P, Tarella C, Olivieri A, Gianni AM, Voena C, Zallio F, et al. Reduced-intensity conditioning followed by allografting of hematopoietic cells can produce clinical and molecular remissions in patients with poor-risk hematologic malignancies. Blood 2002;99:75–82
Tarella C, Rutella S, Gualandi F, Melazzini M, Scime R, Petrini M, et al. Consistent bone marrow-derived cell mobilization following repeated short courses of granulocyte-colony-stimulating factor in patients with amyotrophic lateral sclerosis: results from a multicenter prospective trial. Cytotherapy 2010;12:50–59
Ruella M, Rocci A, Ricca I, Carniti C, Bodoni CL, Ladetto M, et al. Comparative assessment of telomere length before and after hematopoietic SCT: role of grafted cells in determining post-transplant telomere status. Bone Marrow Transpl 2010;45:505–512
Rocci A, Ricca I, Dellacasa C, Longoni P, Compagno M, Francese R, et al. Long-term lymphoma survivors following high-dose chemotherapy and autograft: evidence of permanent telomere shortening in myeloid cells, associated with marked reduction of bone marrow hematopoietic stem cell reservoir. Exp Hematol 2007;35:673–681
Gianni AM, Siena S, Bregni M, Tarella C, Stern AC, Pileri A, et al. Granulocyte-macrophage colony-stimulating factor to harvest circulating haemopoietic stem cells for autotransplantation. Lancet 1989;2:580–585
Couto BG, Goldenberg RC, da Fonseca LM, Thomas J, Gutfilen B, Resende CM, et al. Bone marrow mononuclear cell therapy for patients with cirrhosis: a phase 1 study. Liver Int 2011;31:391–400
Lorenzini S, Isidori A, Catani L, Gramenzi A, Talarico S, Bonifazi F, et al. Stem cell mobilization and collection in patients with liver cirrhosis. Aliment Pharmacol Ther 2008;27(10):932–939
Panasiuk A, Kemona A. Bone marrow failure and hematological abnormalities in alcoholic liver cirrhosis. Rocz Akad Med Bialymst 2001;46:100–105
Pozotrigo M, Adel N, Landau H, Lesokhin A, Lendvai N, Chung DJ, et al. Factors impacting stem cell mobilization failure rate and efficiency in multiple myeloma in the era of novel therapies: experience at Memorial Sloan Kettering Cancer Center. Bone Marrow Transpl 2013;. doi:10.1038/bmt.2012.281.
Chow S, Lazo-Langner A, Ormond G, Howson-Jan K, Xenocostas A. Predictors of unsuccessful mobilization with granulocyte colony-stimulating factor alone in patients undergoing autologous hematopoietic stem cell transplantation. J Clin Apher 2013;. doi:10.1002/jca.21252.
Akard LP, Wiemann M, Thompson JM, Swinney M, Lynn K, Hanks S, Jansen J. Impaired stem cell collection by consecutive courses of high-dose mobilizing chemotherapy using cyclophosphamide, etoposide, and G-CSF. J Hematother 1996;5:271–277
Tarella C, Caracciolo D, Gavarotti P, Bondesan P, Cherasco C, Omede P, Bregni M, et al. Circulating progenitors following high-dose sequential (HDS) chemotherapy with G-CSF: short intervals between drug courses severely impair progenitor mobilization. Bone Marrow Transpl 1995;16:223–238
Wan Z, You S, Rong Y, Zhu B, Zhang A, Zang H, Xiao L, et al. CD34+ hematopoietic stem cells mobilization, paralleled with multiple cytokines elevated in patients with HBV-related acute-on-chronic liver failure. Dig Dis Sci 2013;58:448–457
Gehling UM, Willems M, Schlagner K, Benndorf RA, Dandri M, Petersen J, et al. Mobilization of hematopoietic progenitor cells in patients with liver cirrhosis. World J Gastroenterol 2010;16:217–224
Zocco MA, Piscaglia AC, Giuliante F, Arena V, Novi M, Rinninella E, Tortora A, et al. CD133+ stem cell mobilization after partial hepatectomy depends on resection extent and underlying disease. Dig Liver Dis 2010;43:147–154
Swenson ES, Kuwahara R, Krause DS, Theise ND. Physiological variations of stem cell factor and stromal-derived factor-1 in murine models of liver injury and regeneration. Liver Int 2008;28:308–318
Hu B, Colletti LM. Stem cell factor and c-kit are involved in hepatic recovery after acetaminophen-induced liver injury in mice. Am J Physiol Gastrointest Liver Physiol 2008;295:G45–G53
Lei Y, Liu Z, Han Q, Kang W, Zhang L, Lou S. G-CSF enhanced SDF-1 gradient between bone marrow and liver associated with mobilization of peripheral blood CD34+ cells in rats with acute liver failure. Dig Dis Sci 2009;55:285–291
Acknowledgement
This work was supported in part by grants from the Ministero Italiano Università e Ricerca (MIUR) (PRIN 2006 and Ricerca locale), Rome, Italy; Regione Piemonte (Ricerca Sanitaria Finalizzata and Ricerca Scientifica Applicata), Torino, Italy. G-CSF Lenograstim (rHu G-CSF) (Myelostim®, Italfarmaco) was kindly provided by Azienda Ospedaliero—Universitaria Città della Salute e della Scienza di Torino (ex San Giovanni Battista of Torino). Study sponsors approved the design and protocol but had no involvement in the study design, data collection, analysis and interpretation, or in the writing of the report or the decision to submit the paper for publication.
Conflict of interest
Silvia Gaia, Antonella Olivero, Antonina Smedile, Marco Ruella, Maria Lorena Abate, Maurizio Fadda, Emanuela Rolle, Paola Omedè, Paola Bondesan, Roberto Passera, Alessandra Risso, Manuela Aragno, Alfredo Marzano, Alessia Ciancio, Mario Rizzetto and Corrado Tarella declare that they have no conflict of interest.
Compliance with Ethical Requirements
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5). Informed consent was obtained from all patients for being included in the study. No identifying information about patients is included in the article.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gaia, S., Olivero, A., Smedile, A. et al. Multiple courses of G-CSF in patients with decompensated cirrhosis: consistent mobilization of immature cells expressing hepatocyte markers and exploratory clinical evaluation. Hepatol Int 7, 1075–1083 (2013). https://doi.org/10.1007/s12072-013-9473-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-013-9473-9