Abstract
Background
Hepatic encephalopathy (HE) is associated with poor prognosis in cirrhosis. Gut-derived nitrogenous substances play a role in pathogenesis of HE. The present study was conducted to assess small intestinal bacterial overgrowth (SIBO) and prolonged orocecal transit time (OCTT) in cirrhosis and low-grade HE.
Methods
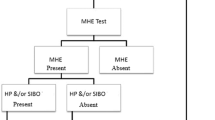
In cross-sectional prospective study, 75 patients were divided into 3 groups: group 1 (no HE, n = 31), group 2 (minimal HE, n = 29), and group 3 (early/grade 1 HE, n = 15). Minimal HE (MHE) was diagnosed when psychometric hepatic encephalopathy score (PHES) was ≤5. Early HE was diagnosed, according to West Haven criteria. All patients underwent glucose hydrogen breath test (GHBT) for SIBO and lactulose hydrogen breath test (LHBT) for OCTT.
Results
A total of 29 patients (38.67 %) had MHE and 15 (20 %) had early HE. Prevalence of MHE in Child–Turcotte–Pugh (CTP) class A, B, and C was 33.3, 38.71, and 45 %, respectively, while SIBO was detected in 26 (34.67 %). Prevalence of SIBO was 12.5 % in CTP class A, 41.94 % in CTP class B, and 50 % in CTP class C. Five (16.13 %) patients in no HE group had SIBO as compared to 14 (48.28 %) in MHE group and 7 (46.67 %) in early HE group (p = 0.018). OCTT was 111.13 ± 13.95 min in patients with no HE as compared to 137.59 ± 14.80 min in patients with MHE and 150 ± 15.12 min in patients with early HE (p < 0.001). OCTT was significantly prolonged in patients with SIBO (145 ± 17.49 min) than in those without SIBO (120.71 ± 18.3 min) (p < 0.001).
Conclusion
SIBO and delayed OCTT are more common with MHE and early HE in patients with cirrhosis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatic encephalopathy (HE) is defined as metabolically induced, potentially reversible, functional disturbance of the brain [1]. Depending on the stage of illness, neuropsychiatric impairment associated with HE ranges from mild alteration of cognition and consciousness to deep coma [1]. Minimal HE (MHE), the mildest form of HE, is characterized by subtle motor and cognitive deficits and impairs health-related quality of life [2]. HE is a common complication in patients with cirrhosis and its development associated with poor prognosis and economic burden to society [3, 4].
Gut-derived nitrogenous substances are universally acknowledged to play a major role in the pathogenesis of HE [5, 6]. Patients with liver cirrhosis have been found to have substantial derangements in the gut microecology, with significant fecal overgrowth of potentially pathogenic Escherichia coli and Staphylococcal species [7]. Small intestinal bacterial overgrowth (SIBO) in cirrhotic patients is common and is associated with systemic endotoxemia, even in the absence of overt infection [8]. SIBO and delayed orocecal transit time (OCTT) have been found to be associated with HE in patients with cirrhosis [9, 10].
Modulation of gut flora with probiotics may be an option for treating patients with cirrhosis and have been found to decrease endotoxin level and improve HE [7, 11]. We performed glucose hydrogen breath test (GHBT) and lactulose hydrogen breath test (LHBT) with the hypothesis that SIBO might be associated with prolonged OCTT and the presence of low-grade HE in patients with cirrhosis of liver.
Methods
In this cross-sectional prospective study, 140 consecutive patients with cirrhosis attending Gastroenterology Outpatient Department of Govind Ballabh Pant Hospital, Delhi, were screened. An informed written consent was taken from every patient before enrolment. The study was approved by the Institutional Ethical Committee. The guidelines laid down by the Indian Council of Medical Research (1994) and the Helsinki Declaration (modified 1989) were adhered to in all patients in the study. Cirrhosis was diagnosed based on the clinical features, laboratory tests, endoscopic evidence of portal hypertension, radiologic evidence, and liver histology, if available. Exclusion criteria included patients on lactulose or l-ornithine l-aspartate therapy; patients who had previous episode of HE; patients with history of recent alcohol intake (in past 6 months); patients who had recent infection or antibiotic use (in past 6 weeks); patients on prophylaxis for spontaneous bacterial peritonitis; patients with recent gastrointestinal bleeding (past 3 months); those who had hepatocellular carcinoma; previous transjugular intrahepatic portosystemic shunt; patients who used drugs, which may affect gastrointestinal motility (β blockers, anti-cholinergic drugs, etc.); patients who used psychotropic drugs, which may affect psychometric tests; any neurologic disease, such as Alzheimer’s disease, Parkinson’s disease, and non-hepatic metabolic encephalopathy; and patients who had significant heart, respiratory, or renal failure. A complete clinical assessment was done to exclude the presence of any illness, which could cause or affect the neurological status. Salt restriction and diuretics were advised for control of ascites. Laboratory investigations included a complete hemogram, serum electrolytes, renal and liver function tests, and complete coagulation profile, viral markers, autoimmune markers, serum ceruloplasmin, and 24 h urinary copper. Slit lamp examination for Kayser–Fleischer (KF) ring was done when indicated. Upper gastrointestinal endoscopy was performed in all patients for the presence of esophageal or gastric varices and portal hypertensive gastropathy. Severity of liver disease was determined by Child–Turcotte–Pugh (CTP) class and model for end-stage liver disease (MELD) scores. Grading of HE was done according to West Haven criteria [1]. Psychometric tests include number connection test (NCT)-A, NCT-B, serial dotting test, digit symbol test, and the line tracing test. NCT was replaced with figure connection test (FCT), as many patients were not familiar with English alphabets and could not perform NCT. FCT is similar to the NCT, except that the numbers are replaced by figures (motifs) [12]. Each test was expressed as Z score, indicating the difference (in standard deviation) between the observed and expected scores for given age and education, based on controls. Negative value indicated poor performance. Psychometric HE score (PHES) was calculated as follows: the results with Z score ± 1 scored 0 points, those with −1 and −2 scored −1, those between −2 and −3 scored −2 points, and those with score less than −3 scored −3. Results better than +1 Z score scored +1 point. The individual test scores were summarized to a sum-score of PHES. Score ≤5 was considered abnormal and diagnostic of MHE [12]. Critical flicker frequency (CFF) was measured by HEPAtonorm analyzer in quiet, semi-darkened room. Patients were first instructed and trained about the procedure. Flicker frequencies were measured 8 times and mean value was calculated. CFF threshold was measured by intrafoveal stimulation with a luminous diode. Decreasing the frequency of the light pulse from 60 Hz downward, the CFF threshold was determined as the frequency when the impression of fused light turned to a flickering one. CFF was considered abnormal when it was <38 Hz [13, 14].
Glucose hydrogen breath test
SIBO was diagnosed by measuring the early appearance of hydrogen following the administration of 100 g glucose [15]. The subjects were asked to avoid slowly absorbed carbohydrates (bread, potato, and corn) and fiber for 3 days prior to the test evening to avoid delayed excretion of hydrogen in the breath. They were also advised to avoid cigarette smoking or physical exercise for 2 h before and during the test, which might cause hyperventilation and consequent changes in breath hydrogen content. They were also advised to brush their teeth and rinse mouth with chlorhexidine mouth wash before the test. Following a 12-h fast, a basal sample of end expiratory breath was collected before the test meal. Patients with high basal breath hydrogen level were rescheduled after ensuring all above precautions. The test consisted of the administration of a 100 g dose of glucose dissolved in 200 ml of water. Breath samples were measured by SC Microlyzer instrument (Quintron Instrument, Milwaukee, WI, USA) for hydrogen every 15 min for a 3 h period. Results were expressed as parts per million (ppm); a persistent increase in breath hydrogen of at least 12 ppm above the baseline value (2 consecutive readings) within the 3 h period was considered indicative of SIBO.
Orocecal transit time
LHBT was performed on the day following GHBT, to measure OCTT. A basal sample of end expiratory breath was collected before the test meal after a 12-h fast. A 15-ml dose of lactulose syrup containing 10 g of lactulose was used as the test dose [16]. Breath samples were measured at 15 min intervals (beginning 30 min after the dose of lactulose) for the first 2 h and at 20 min intervals for next 2 h. OCTT was calculated as the time when an increase of at least 15 ppm of hydrogen above the baseline was documented in two consecutive readings (SC Microlyzer, Quintron Instrument, Milwaukee, WI, USA).
Statistical analysis
Chi-square test was used to assess the difference between categorical variables. Analysis of variance (one way ANOVA) and unpaired t test were applied to analyze the difference between continuous variables. A p value of <0.05 was considered statistically significant. Correlation between PHES and CFF with OCTT was done with Pearson correlation coefficient. Statistical analysis was performed with SPSS software version 15.0 (SPSS Inc., Chicago, IL, USA) and Primer of Statistics software.
Results
Of the 140 patients with cirrhosis screened, 75 patients (age 42.49 ± 9.65 years; M:F 55:20) who met the inclusion criteria were included in the study. Up to 65 patients were excluded due to one or more exclusion criteria such as lactulose or LOLA therapy (n = 21), recent infection or antibiotic use (n = 10), recent alcohol intake (n = 11), hepatocellular carcinoma (n = 2), β blocker (n = 15), and other systemic illness (n = 6) (Fig. 1). Etiology of liver cirrhosis was alcohol in 40 patients (53.33 %), hepatitis B in 14 patients (18.67 %), hepatitis C in 6 patients (8 %), and other causes in 15 patients (20 %) (including autoimmune hepatitis 2; primary biliary cirrhosis 1, cryptogenic cirrhosis 12 patients). A total of 24 patients (32 %) were in CTP class A, 31 (41.33 %) were in CTP class B, and 20 (26.67 %) were in CTP class C (Table 1).
Among 75 patients, 29 (38.67 %) had MHE and 15 (20 %) had early HE (grade 1 HE). Prevalence of MHE in CTP class A, B and C was 33.33, 38.71, and 45 %, respectively. About 31 patients (41.33 %) had no MHE or early HE.
CFF values were significantly lower in patients with MHE (29.97 ± 4.32 vs. 48.74 ± 4.93, p < 0.001) and early HE (25.17 ± 5.15 vs. 48.74 ± 4.93, p < 0.001) as compared to patients without HE. However, there was no significant difference between patients with MHE and early HE (29.97 ± 4.32 vs. 25.17 ± 5.15, p = NS).
Of the 75 patients with cirrhosis, SIBO was detected in 26 patients (34.67 %). Prevalence of SIBO was 12.5 % in patients with CTP class A, 41.94 % in CTP class B, and 50 % in CTP class C (Table 2). SIBO was detected in 5 patients (16.13 %) without HE as compared to 14 patients (48.28%) in MHE group and 7 patients (46.67 %) in early HE group (p = 0.018).
OCTT was 111.13 ± 13.95 min in patients who had no HE as compared to 137.59 ± 14.80 min in patients with MHE and 150 ± 15.12 min in patients with early HE (p < 0.001). OCTT was 118.75 ± 20.62 min in CTP class A, 132.23 ± 19.80 min in CTP class B, and 143.81 ± 17.52 min in CTP class C (p < 0.001, Table 2).
OCTT was significantly prolonged in patients who had SIBO (145 ± 17.49 min) than in those who did not have SIBO (120.71 ± 18.30 min) (p < 0.001). OCTT was inversely correlated with CFF (r = −0.684, p < 0.001) and PHES (r = −0.691, p < 0.001).
Discussion
We have shown that patients with MHE and early HE have higher prevalence of SIBO and prolonged OCTT as compared to patients without HE. Our study demonstrated high prevalence of SIBO (34.67 %) in patients with cirrhosis. The prevalence of SIBO in cirrhotic patients in the previous studies ranged between 24 and 64 % [8, 9, 17, 18]. This difference may be due to difference in patient profile and diagnostic methodology. Higher prevalence of SIBO has been reported with increasing severity of liver cirrhosis and presence of ascites [19, 20]. However, recent study by Lakshmi et al. [17] reported no association between severity of liver dysfunction and SIBO. We found significantly higher prevalence of SIBO in CTP class B (41.94 %) and CTP class C (50 %) as compared to CTP class A (12.5 %) cirrhosis.
In our study group, 38.67 % patients had MHE and 20 % had early HE. SIBO was more prevalent in patients with MHE and early HE. This finding was similar to that reported in previous studies [7, 9]. Gupta et al. [9] in their study demonstrated that the only factor associated with MHE was SIBO. Patients with SIBO had prolonged OCTT as compared to patients without SIBO. However, study design did not permit to evaluate cause and effect relationship between these entities. SIBO in cirrhotic patients can be associated with several factors other than the degree of derangement of liver function and portal hypertension. Intestinal peristalsis, gastric acid, and mucosal immunity act together to prevent SIBO in normal subjects. Studies using 24 h pH-metry have shown reduced gastric acid in cirrhotic patients, which is aggravated by indiscriminate use of proton pump inhibitor [21]. Moreover, mucosal immune defense mechanisms, which promote colonization of pathogenic organisms, are deranged in patients with cirrhosis [22].
Various studies have shown increased gastrointestinal transit time in patients with liver cirrhosis [23–25]. We also found that OCTT was more prolonged in patients with MHE and early HE. We found inverse correlation of PHES and CFF with OCTT. Also, patients in CTP classes B and C had more delayed OCTT as compared to CTP class A. The exact etiology for delayed intestinal transit in patients with liver cirrhosis is largely unknown. It is also not clear whether delayed OCTT leads to SIBO or SIBO is responsible for delayed OCTT. Various mechanisms, such as presence of autonomic neuropathy, metabolic derangements due to portosystemic shunting, and SIBO, have been proposed for slow gastrointestinal transit in cirrhosis [23–25]. Thuluvath and Triger [25] have shown that the presence of autonomic neuropathy was an independent predictor of delayed OCTT in patients with cirrhosis. Metabolic derangements in cirrhotic patients as a consequence of portosystemic venous shunting secondary to portal hypertension may be responsible for delayed OCTT [23]. SIBO may alter gastrointestinal transit by effect of endotoxin on local neuronal circuit. Antibiotic therapy has been shown to improve the OCTT in patients with liver cirrhosis, which makes it likely that bacterial overgrowth alters the small intestinal motility [23].
Results of the present study may have therapeutic implications. Abnormal intestinal motility may play an important role in increasing the growth of pathogenic bacteria and increased absorption of gut toxins. Ammonia, mercaptans, phenols, short- and medium-chain fatty acids, and benzodiazepine-like compounds have all been found to be elevated in cirrhotic patients with HE. Recent observations in patients with liver disease suggested that inflammatory response is also important in the pathogenesis of HE [5]. Manipulation of gut flora by prebiotics, probiotics, synbiotics, prokinetics, or antibiotics may be useful in the prevention and treatment of HE. Probiotics exhibit efficacy in the treatment of HE by decreasing total ammonia in the portal blood by decreasing bacterial urease activity, decreasing ammonia absorption by decreasing pH, improving nutritional status of gut epithelium and decreasing intestinal permeability and competitive inhibition against pathogenic bacteria, and by decreasing inflammation and oxidative stress in the hepatocyte leading to increased hepatic clearance of ammonia and other toxins [26]. Liu et al. [7] first reported significant reduction in blood ammonia levels, reversal of MHE, CTP class improvement in 50 % patients, and a significant reduction in endotoxemia with synbiotic treatment. Bajaj et al. [27] showed that treatment of MHE with probiotic yogurt in patients with non-alcoholic cirrhosis was associated with reversal of MHE in 71 % of patients. Prokinetics, such as cisapride, has been shown to decrease OCTT and reduce SIBO in cirrhotic patients, suggesting the potential role of prokinetics in treatment of MHE and early HE [28].
Limitations of our study include small sample size and lack of measurement of serum level of endotoxins, cytokines, and intestinal permeability.
We conclude that SIBO and delayed OCTT are more common in patients with cirrhosis with MHE and early HE. Further, randomized control trial is warranted to study the role of alteration of gut flora (with antibiotics, prebiotics, or probiotics) and gastrointestinal transit (with prokinetic agents) for reversibility of MHE or early HE in patients with liver cirrhosis.
References
Ferenci P, Lockwood A, Mullen K et al. Hepatic encephalopathy—definition, nomenclature, diagnosis and quantification: final report of the working party at the 11th world congress of gastroenterology, Vienna 1998. Hepatology 2002;35:716–721
Dhiman RK, Saraswat VA, Sharma BK et al. Minimal hepatic encephalopathy: consensus statement of a working party of the Indian National Association for study of the liver. J Gastroenterol Hepatol 2010;25(6):1029–1041
Bustamante J, Rimola A, Ventura PJ et al. Prognostic significance of hepatic encephalopathy in patients with cirrhosis. J Hepatol 1999;30:890–895
Poordad FF. The burden of hepatic encephalopathy. Aliment Pharmacol Ther 2007;25(Suppl 1):3–9
Butterworth RF. Hepatic encephalopathy: a central neuroinflammatory disorder? Hepatology 2011;53(4):1372–1376
Butterworth RF. Pathogenesis and treatment of portal-systemic encephalopathy: an update. Dig Dis Sci 1992;37:321–327
Liu Q, Duan ZP, Ha DK et al. Symbiotic modulation of gut flora: effect on MHE in patients with cirrhosis. Hepatology 2004;39:1441–1449
Bauer TM, Schwacha H, Steinbrückner et al. Small intestinal bacterial overgrowth in human cirrhosis is associated with systemic endotoxemia. Am J Gastroenterol 2002;97(9):2364–2370
Gupta A, Dhiman RK, Kumari S et al. Role of small intestinal bacterial overgrowth and delayed gastrointestinal transit time in cirrhotic patients with minimal hepatic encephalopathy. J Hepatol 2010;53(5):849–855
Nagasako CK, de Oliveira Figueiredo MJ, de Souza Almeida JR et al. Investigation of autonomic function and orocecal transit time in patients with nonalcoholic cirrhosis and the potential influence of these factors on disease outcome. J Clin Gastroenterol 2009;43(9):884–889
Mittal VV, Sharma BC, Sharma P et al. A randomized controlled trial comparing lactulose, probiotics, and l-ornithine l-aspartate in treatment of minimal hepatic encephalopathy. Eur J Gastroenterol Hepatol 2011;23(8):725–732
Dhiman RK, Kurmi R, Thumburu KK et al. Diagnostic and prognostic significance of minimal hepatic encephalopathy in patients with cirrhosis of liver. Dig Dis Sci 2010;55:2381–2390
Kircheis G, Wettstein M, Timmermann L et al. Critical flicker frequency for quantification of low-grade hepatic encephalopathy. Hepatology 2002;35:357–366
Romero-Gómez M, Córdoba J, Jover R et al. Value of critical flicker frequency in patients with minimal hepatic encephalopathy. Hepatology 2007;45(4):879–885
Kerlin P, Wong L. Breath hydrogen testing in bacterial overgrowth of small intestine. Gastroenterology 1988;95:982–988
Sarno S, Erasmas LP, Haslbeck M et al. Orocaecal transit, bacterial overgrowth and hydrogen production in diabetes mellitus. Ital J Gastroenterol 1993;25:490–496
Lakshmi CP, Ghoshal UC, Kumar S et al. Frequency and factors associated with small intestinal bacterial overgrowth in patients with cirrhosis of the liver and extra hepatic portal venous obstruction. Dig Dis Sci 2010;55:1142–1148
Gunnarsdottir SA, Sadik R, Shev S et al. Small intestinal motility disturbances and bacterial overgrowth in patients with liver cirrhosis and portal hypertension. Am J Gastroenterol 2003;98:1362–1370
Pande C, Kumar A, Sarin SK. Small-intestinal bacterial overgrowth in cirrhosis is related to the severity of liver disease. Aliment Pharmacol Ther 2009;29:1273–1281
Casafont Morencos F, de las Heras Castaño G, Martín Ramos L et al. Small bowel bacterial overgrowth in patients with alcoholic cirrhosis. Dig Dis Sci 1996;41:552–556
Savarino V, Mela GS, Zentilin P et al. Evaluation of 24-hour gastric acidity in patients with hepatic cirrhosis. Hepatology 1996;25(2):152–157
Rimola A, Soto R, Bory F et al. Reticuloendothelial system phagocytic activity in cirrhosis and its relation to bacterial infections and prognosis. Hepatology 1984;4(1):53–58
Van Thiel DH, Fagiuoli S, Wright HI et al. Gastrointestinal transit in cirrhotic patients: effect of hepatic encephalopathy and its treatment. Hepatology 1994;19:67–71
Fleckenstein JF, Frank S, Thuluvath PJ. Presence of autonomic neuropathy is a poor prognostic indicator in patients with advanced liver disease. Hepatology 1996;23:471–475
Thuluvath PJ, Triger DR. Autonomic neuropathy and chronic liver disease. Q J Med 1989;72:737–747
Shukla S, Shukla A, Mehboob S et al. Meta-analysis: the effects of gut flora modulation using prebiotics, probiotics and synbiotics on minimal hepatic encephalopathy. Aliment Pharmacol Ther 2011;33(6):662–671
Bajaj JS, Saeian K, Christensen KM et al. Probiotic yogurt for the treatment of minimal hepatic encephalopathy. Am J Gastroenterol 2008;103:1707–1715
Madrid AM, Hurtado C, Venegas M et al. Long-term treatment with cisapride and antibiotics in liver cirrhosis: effect on small intestinal motility, bacterial overgrowth, and liver function. Am J Gastroenterol 2001;96:1251–1255
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lunia, M.K., Sharma, B.C. & Sachdeva, S. Small intestinal bacterial overgrowth and delayed orocecal transit time in patients with cirrhosis and low-grade hepatic encephalopathy. Hepatol Int 7, 268–273 (2013). https://doi.org/10.1007/s12072-012-9360-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-012-9360-9