Abstract
To address the relationship between hepatitis B virus (HBV) endemicity and HBV-related liver diseases in Mexico. Research literature reporting on HBsAg and antibody to hepatitis B core antigen (anti-HBc) prevalence in Mexican study groups were searched in NLM Gateway, PubMed, IMBIOMED, and others. Weighted mean prevalence (WMP) was calculated from the results of each study group. A total of 50 studies were analyzed. Three nationwide surveys revealed an HBsAg seroprevalence of less than 0.3%. Horizontal transmission of HBV infection occurred mainly by sexual activity and exposure to both contaminated surgical equipment and body fluids. High-risk groups exposed to these factors included healthcare workers, pregnant women, female sex workers, hemodialysis patients, and emergency department attendees with an HBsAg WMP ranging from 1.05% (95% confidence interval [CI], 0.68–1.43) to 14.3% (95% CI, 9.5–19.1). A higher prevalence of anti-HBc in adults than those younger than 20 years was associated with the main risk factors. Anti-HBc WMP ranged from 3.13% (95% CI, 3.01–3.24) in blood donors to 27.7% (95% CI, 21.6–33.9) in hemodialysis patients. A heterogeneous distribution of HBV infection was detected, mainly in native Mexican groups with a high anti-HBc WMP of 42.0% (95% CI, 39.5–44.3) but with a low HBsAg WMP of 2.9% (95% CI 2.08–3.75). Estimations of the Mexican population growth rate and main risk factors suggest that HBsAg seroprevalence has remained steady since 1974. A low HBsAg prevalence is related to the low incidence of HBV-related liver cirrhosis and hepatocellular carcinoma (HCC) previously reported in Mexico.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatitis B virus (HBV) infection is a health problem worldwide, with approximately 400 million chronically infected people. The endemicity of a given population is determined by the presence of HBsAg in serum and is classified as low, intermediate, and high endemicity according to the percentage of infection (2%, 2–7.9%, and ≥8%, respectively) [1–5]. However, there is limited information about the epidemiology of HBV infection in many countries of low endemicity.
Asia is a region of high endemicity [1–5] for HBV infection, whereas in America, low or intermediate endemicity is prevalent [6–8]. However, several studies have revealed the existence of high endemic areas, especially within the indigenous populations throughout the continent [9–11]. Another difference between both continents besides the genetic background of the population is the HBV genome variability and geographical distribution. Genotypes B and C predominate in Asia, whereas genotypes F and H predominate in Latin American [9–13]. Genotype H has been detected mainly in Mexico [14, 15] and is scarce in some countries of Central America and abroad [16, 17]. In contrast, genotype F appears to be predominating in most countries of Central and South America [18–20].
The association between a specific HBV genotype and native population has led to the analysis and follow-up of the transmission routes between regions, especially in this present era of global mobility, since HBV infection acquisition from one region to another has been recently reported [21].
On the other hand, further evidence revealed that HBV genotype might also be associated to the natural course of infection and response to antiviral treatment [22–24]. This association has been documented mostly from countries of high endemicity and creates the necessity in those countries with low endemicity to further investigate this association, since different treatment and prevention strategies could be required for disease control.
Furthermore, the natural course of HBV infection and complications of the disease are mainly referred from countries with high endemicity of HBV infection and specific genotypes, and such evidence is generally extended to other countries, such as Latin America, and particularly to Mexico [6, 25, 26]. However, HBV genotype H is predominant in Mexico unlike the rest of the American countries and the world. This raises the question about the number of acutely or chronically HBV-infected people in the country, the main risk factors involved in infection transmission, and the prevalence of HBV-related liver diseases and complications. To answer this question, it will be also important to understand why hepatocellular carcinoma (HCC) is rare in Mexico [27, 28] considering the fact that the main causes of liver cirrhosis are alcohol, followed by hepatitis C virus (HCV) infection, and, only in 5.2% of the cases, HBV [29]. Although obesity along its associated metabolic complications is currently a main health problem in Mexico [30], the burden of their pathophysiological states in the development of liver disease is relatively unknown.
By performing a systematic review and meta-analysis of the research literature on HBV infection, the aim of this study was to estimate the HBsAg and antibody to hepatitis B core antigen (anti-HBc) seroprevalence to analyze the course of HBV infection from 1987 to 2007 and to identify the main risk factors involved and further understand the association of HBV with HCC in Mexico.
Material and methods
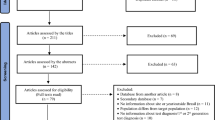
Main search strategy
This study was conducted following the general methodology recommended for systematic reviews [31, 32]. The main research questions formulated to guide the study search were as follows: (1) “Is Mexico a low endemicity region for HBV infection?”; (2) “Have there been changes in the HBsAg seroprevalence from 1974 to 2007?”; (3) “Which are the main risk factors involved in HBV transmission?” and (4) “Is there an association between low prevalence of HBV infection and HCC?”
The initial approach was to electronically search for both English and Spanish publications concerning the epidemiology of HBV infection in Mexico. For English and/or Spanish language studies, the databases NLM Gateway, MEDLINE, PubMed, Artemisa, Medigrafic, IMBIOMED, and Lilacs were searched by using the following terms: “HBV,” both spelt out and abbreviated, “hepatitis B prevalence,” “epidemiology,” “risk factors,” and “HBsAg” combined with “HBV infection” and “Mexico.” As for search terms in Spanish, “VHB,” “hepatitis B” (and) “prevalencia,” “infección de la hepatitis B en Mexico,” alone and/or combined with “HBsAg,” “epidemiologia,” and “factores de riesgo” were used.
All articles were reviewed and their corresponding reference lists were revised to identify additional material that had not been initially detected, and then were later either retrieved by a new electronic search or searched manually. The period for this review was set from January 1985 up to August 2007 and also the first epidemiological study dated 1974 was considered as a reference point [33].
Eligibility criteria
First-round review criteria for the selection of full-text publications included sufficient and explicit data on the year of publication, time period, selection of study group, location of study, number of subjects studied, and number of subjects positive to HBsAg, anti-HBc, or stated crude prevalence. Information related to risk factors was also extracted.
Differences in the sensibility of the HBsAg detection assay reported in each study were examined. Our strategy was to enlist each study by the year of performance, assay used, and test generation. Only those studies that tested HBV serological markers with assays that had third-generation sensitivity were included for meta-analysis. Among the different study group categories, the three main HBsAg detection assays identified were from Abbott Laboratories (Abbott Park, IL), Auszyme Monoclonal, IMx HBsAg (V2), and AxSYM HBsAg (V2). During the time period of this review, at least 90% of the studies were performed with Auszyme Monoclonal or IMx HBsAg (V2), followed by AxSYM HBsAg. Furthermore, this preliminary analysis also revealed that a second-generation assay, counterelectrophoresis (CEP), was used in a general population study performed in 1974 and thus was not included for the next stage of meta-analysis.
In studies performed in pregnant women, three different assays were detected, Auszyme Monoclonal (Abbott Laboratories), Hepanostika HBsAg Uni-form II (Organon Tecnika, B.V., The Netherlands, currently distributed by BioMerieux, France), and Monolisa HBsAg Plus (Bio-Rad Laboratories, Marnes-la-Coquette, France). In this case, studies were not included in meta-analysis.
As for meeting eligibility criteria for the abstracts that appeared during the strategy search, these were included if the same eligibility criteria were completed and excluded if data were found published as full-text publications. Direct searches were performed within specific Web sites of several national associations of medical specialists related to HBV infection to retrieve online abstracts covering all meetings enlisted.
Data extraction, synthesis, and meta-analysis
Extracted data were synthesized in tables and figures by different criteria to analyze the information and answer research questions. Data grouped by crude prevalence followed the categories established by the World Health Organization criteria of endemicity [2] according to HBsAg prevalence, that is, low prevalence (<2%), intermediate prevalence (2–7.9%), and high prevalence (≥8%).
High-risk groups were defined according to the standard criteria of high-exposed individuals to HBV infection, such as female sex workers, healthcare workers, and hemodialyzed and institutionalized patients. The number of studies was superior to the number of publications, since in some cases, more than one population group was reported in a single article.
From the data of primary studies, 95% confidence intervals (CIs) for crude seroprevalence of each study report and different estimates on the overall seroprevalence in Mexico were calculated as previously described [34]. Briefly, the pooled prevalence (PP) was calculated as follows: PP = ∑n i /N, where n i = number of seroreactive cases in each study and N = total number of individuals. The mean prevalence (MP) was estimated as follows: MP = ∑prev i /S, where prev i = prevalence in each study and S = number of studies. We also calculated the weighted mean prevalence (WMP) to restrict the bias that may impose the heterogeneous nature of the reports. It was calculated as follows: WMP = ∑(ωI·prev i )/∑ωI, where ωI = 1[prev i (1 − prev i /N i ] and N i = total number of subjects studied. Here, WMP is regarded as the most accurate method to estimate prevalence of HBV infection after considering several reports. This method has proven to be reliable when combining a number of studies with inherent heterogeneity in sample size and effects. All estimates on seroprevalence are expressed as proportions and the respective 95% CI. Chi-square statistics were used to test differences in prevalence estimates between studies.
Results
General scope of publications on HBV infection prevalence
The epidemiological evidence of HBV infection prevalence in Mexico was documented by 1 of 2 serological markers, HBsAg or anti-HBc; however, in some cases, they were not simultaneously used in the same study. A total of 50 studies collected from 47 publications for this systematic review were considered eligible for meta-analysis. The main study groups were blood donors (n = 25), followed by female sex workers or men with high-risk behavior (n = 8), healthcare workers, and students (n = 6), and to a lesser extent, patients with liver diseases (n = 4), native communities (n = 3), and hemodialysis patients (n = 2), as well as psychiatric patients and emergency department attendees (1 of each). The studies performed in general population (n = 3) and pregnant women (n = 9), not included in the meta-analysis, were examined separately for comparative purposes only.
Prevalence of HBV infection by HBsAg marker
Nationwide survey studies
Each nationwide survey was performed by different institutions, first in 1974 and later in 1997 and 2000, in which none had consecutive follow-ups [7, 33, 35] (Table 1). Three types of assays were conducted with different levels of sensitivity. The earliest study from 1974 used a CEP-based assay, whereas the following studies used third-generation assays, such as Auszyme Monoclonal and AxSYM HBsAg (V2). However, all three studies revealed a low HBV seroprevalence of less than 0.3%.
Blood donors
In total, 21 publications [36–56] were concerning HBsAg seroprevalence in blood donor banks that involved 1,130,485 people from 10 states and Mexico City (Table 2). The crude seroprevalence reported in each study ranged from 0.073 to 1.22%. When the results from blood donors were analyzed separately by using assays as mentioned in the “Material and methods” section, no significant differences were detected among Auszyme Monoclonal, IMx HBsAg (V2), and AxSYM HBsAg (Abbott Laboratories) (data not shown). Thus, the overall estimated MP, PP, and WMP were 0.42% (95% CI, 0.29–0.56), 0.27% (95% CI, 0.26–0.28%), and 0.61% (95% CI, 0.59–0.62), respectively.
Geographical distribution of HBV infection in Mexico
These results are in agreement with other studies conducted in Mexican blood banks [57], which revealed differences in the geographical distribution of HBsAg seroprevalence in blood donors among the states within the country (p < 0.05). Figure 1 denotes the Mexican states where the individual HBsAg seroprevalence was higher than the WMP HBsAg seroprevalence estimated for this group (≥0.6%, Table 2). Populations with a higher prevalence were located in Mexico City and surrounding states, as well as located in the northern and southern borders of the country where nonpermanent migration is common. It was interesting to note that these localities are also within or near regions where the main native Mexican groups live.
Pregnant women
Nine studies of HBV prevalence in pregnant women [58–61] involved 19,246 persons, in which four studies were carried out in Mexico City and five in other states. Three HBsAg detection assays were identified with different sensitivities. Significant changes in the prevalence of HBsAg in pregnant women were observed when studies were compared with Monolisa HBsAg Plus that had been recently introduced into the country. This variability in prevalence may be caused by differences in assay sensitivity and the natural variability of HBV genotype among Mexicans. Table 3 depicts studies performed in pregnant women in which both HBsAg and anti-HBc were tested in some cases.
On the other hand, HBsAg prevalence was either absent or low in infants born to HBsAg-positive mothers [58, 60], suggesting that vertical HBV transmission is not the main cause of infection.
High-risk groups
The estimates of HBsAg seroprevalence of blood donors compared with high-risk groups including healthcare workers [62–67], females sex workers [68–75], patients with liver diseases [29, 40, 76, 77], hemodialysis patients [78, 79], emergency department attendees [80], and psychiatric patients [81] are depicted in Table 2. The estimates from the native Mexican population [82–84] are also included in this group based on an HBsAg seroprevalence higher than the general population and blood donors.
Prevalence of HBV infection by anti-HBc marker
Anti-HBc determination was performed only in 23 of the 50 publications reviewed in this study in which HBsAg was also tested (Table 4). As could be expected, anti-HBc seroprevalence increased proportionally as HBsAg seroprevalence increased. However, despite the high anti-HBc seroprevalence in native Mexican groups, HBsAg prevalence was low or intermediate (Fig. 2).
Main risk factors for HBV infection in Mexican population
Risk factors determined by univariate or multivariate analysis and associated to anti-HBc prevalence by odds ratio (OR) were reported in general population [35], pregnant women [61], healthcare workers [66], and female sex workers [73]. The main risk factors were (i) age at first sexual intercourse above 25 years in general population and in pregnant women, with a reported OR of 3.24 (95% CI, 1.44–7.28) and 5.1 (95% CI, 1.4–19.1), respectively; and (ii) age above 33 years in female sex workers with an OR of 5.4 (2.2–13.0). Marital status denoted an OR of 1.92 (95% CI, 1.0–3.6) in single or divorced pregnant women and 7.4 (95% CI, 3.9–14.2) in widows from studies in general population. Other important risk factors related to HBV transmission were blood transfusion, residence in cities with high migration rates or near the northern or southern borders, and within the rural areas with low economic status. In these particular conditions, an OR of 4.8 (95% CI, 2.1–11.3) was reported in female sex workers with antecedents of blood transfusion and an OR of 3.2 (95% CI, 1.57–6.51) in pregnant women living in cities with high migration rates. In general population, an OR of 2.8 (95% CI, 1.4–4.4) and 1.1 (95% CI, 0.8–1.6) was reported in individuals living on the border or within the rural areas, respectively. Four or more sexual partners, promiscuity, tattooing, and antecedents of surgery were risk factors detected with a high frequency; however, ORs were neither estimated nor reported.
Age-related incidence, prevalence of HBV infection, and HCC
To have a wider scope regarding HBV infection in Mexico, data related to the annual and age-related incidence rates of acute HBV infection reported by the Mexican Health Secretariat were analyzed. An incidence of 0.83 new cases per year per 100,000 inhabitants was reported in the year 2000 [85, 86]. However, further investigations have revealed that such low incidence of HBV infection has remained less than 1% from 1990 to date. Also, in the population older than 20 years, the incidence rate was 3.5 times higher than in those younger than 20 years throughout this same time period [85].
The age-related prevalence of HBV infection by anti-HBc marker is depicted in Fig. 3. The higher increase of HBsAg prevalence in adults than in the younger population is confirmed by studies that reported the anti-HBc prevalence at different ages. In two different studies from native Mexican groups and two from the general population, an important increase in the prevalence of anti-HBc marker around the age of 15, when sexual activity initiates, and older ages was observed. Similar results were obtained in the first epidemiological study performed in 1974 [33].
From 1992 to 2002, the Mexican Health Secretariat registered an average of 13,688 new cases of cirrhosis per year [103], whereas in a national multicenter study, HBV infection accounted for 5.2% of all cases of liver cirrhosis [29]. Such low prevalence of HBV infection is associated with a very low incidence of HCC in Mexico City [27] and the west of the country [28], which are the main population regions.
Causes of steady HBV infection in the last 30 years
Two main factors presumably involved in the prevalence of HBV infection in Mexico is horizontal transmission as reported in young and adult Mexican populations and the fact that a low HBsAg seroprevalence has remained steady from 1974 to date. To explain this state, governmental official data [87] and estimations reported elsewhere [88] were obtained for population size and the number of people both younger than and older than 20 years was determined. Figure 4 provides a comparison of the Mexican population growth rate from 1790 to 2008 and the distribution percentage of the population both younger than and older than 20 years. The years when blood bank regulations were introduced to control HBV infection in Mexico are indicated. A switch in the age distribution in the population both younger than and older than 20 years was observed between 1950 and 1990. Therefore, if sexual activity is the main risk factor in the transmission of HBV infection, this figure appears to explain why the HBsAg seroprevalence has not changed since 1974 in spite of the introduction of sanitary regulations in 1987.
Discussion
To address the questions, whether Mexico is a low endemic region for HBV infection and whether changes in the HBsAg seroprevalence have occurred from 1974 to 2007, we found a limitation not only in the number of studies performed to date but also in the methodology used in each case. The immunological tests for the detection of HBsAg serological tests have evolved since the decade of the 1970s from low specificity and sensitivity to the identification of escape mutants in specific populations as reported recently [89–93].
The first large epidemiological study performed in Mexico in 1974 by Landa [33] used a CEP-based assay, which was later considered as a second-generation methodology for the detection of HBsAg. This immunological method was characterized because of its capacity to identify two of three panels used at that time by the Food and Drug Administration, Bureau of Biologics Reference Panel [94]. However, by comparing the second- and third-generation methods, the CEP assay was shown to have 0.9% of false positives against 12.1% of false negatives [89]. Based on this information, it could be deduced that the 0.29% seroprevalence obtained at that time, even with an increase of 10% in HBV seropositives, would remain as a population of low HBV endemicity.
The epidemiological studies performed in 1997 and 2000 also showed HBsAg seroprevalence below 0.3% by using third-generation tests. Besides the methodological differences, further limitations were noticed. In the first epidemiological study, actually the largest performed to date with 19,000 people sampled, the main limitation of this study was that the population studied was younger than 50 years [33]. In the second study analyzed in 1996 [7], there was no follow-up to compare data with the former study and information for population older than 40 years was lacking. The third study appeared to be complementary to the second one, since it was performed almost at the same time and included groups with persons older than 40 years but not younger than 21 years [35].
From 1987 to 1995, Auszyme Monoclonal was the main immunological test used in blood banks throughout the country. However, the analysis of the data that used this immunological test and comparison with those performed years latter, whether IMx or AxSYM, did not show statistical significant differences (data not shown). Therefore, considering that data from blood donors are obtained only from adult population, then, at least from 1987 to date, HBsAg prevalence has also been low in this group although higher than in general population. These data are in agreement with a recent study that showed no changes in the prevalence of HBV, HCV, and HIV in national blood banks from 1999 to 2003 [57].
On the other hand, those studies performed in pregnant woman were not included in the meta-analysis either because of differences in the immunological test or because of large variability in results obtained in each study. If these results are considered as valid, then they may indicate an important variability in sensitivity and specificity of all the immunological test used to date, considering that they have been designed mainly for genotypes A and/or D [90, 92, 95–98] whereas in Mexico and Latin America, genotypes H and F predominate, both with a higher genetic variability than any of the other genotypes reported [13].
Then, if this were the case, discrepant results such as those reported in native Mexican with a high prevalence of anti-HBc but a low prevalence of HBsAg could be explained because of variability in results of the immunological test that was used. This is an area that deserves further investigation. However, data obtained to date indicate that in most of the Mexican populations, a low HBsAg seroprevalence is predominant, although an underestimation could be latent. Thus, even if more sensitive and specific immunological tests were used, it would be difficult in such populations to shift HBsAg seroprevalence from low to high endemicity.
There is limited information about the distribution of HBV infection throughout the country; however, since 1974, different studies [33, 50, 57, 82] have shown heterogeneity in HBsAg seroprevalence, which appears to be due to the native Mexican populations. More than 60 native groups with a population of more than 10 millions could have HBsAg seroprevalence ranging from intermediate to high endemicity if studies are extended and confirmed in these populations.
In 2000, the Mexican population was 97.5 million, of which 56.4% were adults [87, 88]. Therefore, if HBsAg WMP from blood banks (0.61%) is considered, then we would expect that at least 300,000 adults were HBV infected at that time. The first study preformed in 1974 by Landa [33] showed that in Mexico City more than 6% of the population studied at that time have had HBV infection. Two latter studies performed in general population indicated that 1.4 and 3.3% were anti-HBc positive, respectively, suggesting at least 2.4 million people have been infected with HBV until the year 2000.
Sexual transmission was considered as an important risk factor based on the association of the number of persons that have had the infection during the age of sexual activity and the increasing number of older infected people as confirmed by subsequent studies [7, 33, 35]. For example, in a study performed recently [35], it is emphasized that a 1:200 ratio for people between the ages of 20 and 30 years have had the infection whereas the number of persons infected increases to a 1:10 ratio in those older than 50 years. The present data analysis confirms that horizontal transmission predominates in Mexico as reported in other areas of low HBV endemicity [3].
Although vertical transmission is also observed, it is not the main route of transmission as corroborated by the low or very low HBsAg seroprevalence in children younger than 10 years [99, 100]. However, besides the sexual transmission of HBV infection in the adult population, the fact that those older than 50 years are infected in a higher proportion may be due to the fact that before the 1960s in most of the Mexican villages, it was common to use a single syringe for several patients.
Therefore, the epidemiological studies performed to date indicate that the main risk factors involved in HBV transmission in Mexico are sexual activity and the exposure to contaminated body fluids and contaminated surgical equipment. People living in low social status areas have a further risk of infection with contaminated body fluids owing to the lack or deficiency of sanitized procedures. The predominance of these risk factors besides the late introduction of blood bank regulations [101], such as prohibition of blood commercialization in 1987, the mandatory detection of HCV and HBV serological markers in 1993, and the application of the HBV vaccine in 1999 in newborns [102], appears to explain why the prevalence of HBV infection remains steady in Mexico since 1974.
The same risk factors appear to explain the high prevalence of HBsAg and anti-HBc in specific population groups such as female sexual workers, as well as those who have frequent contact with contaminated surgical equipment and biological fluids, such as healthcare workers, hemodialysis patients, and emergency department attendees. Both risk factors may also prevail simultaneously in the same group and in other groups such as prison inmates and psychiatric patients.
Although blood transfusion has also been a common antecedent in HBV-infected patients, in this present analysis, it was not the main risk factor as in HCV infection [34]. Unlike other countries, intravenous drug abuse is not common among drug addicts in Mexico, instead marijuana, inhalants, and recently, an increase in cocaine abuse are prevalent [103]. These data indicate that the frequency of risk factors among countries is variable and therefore raises the necessity to recognize them individually to establish specific strategies of HBV infection control in each country.
In spite of the fact that Mexico and other countries have a low endemicity for HBV, infected individuals can continue transmitting HBV infection. This generates the need of additional specific strategies along with blood bank regulations, such as vaccination programs in young and adult populations to avoid HBV transmission by sexual relationships, better compliance to sanitary procedures, and more effective sterilization methods in hospitals and healthcare workers’ offices, including dentists. The use of highly sensitive tests for HBV detection, such as nucleic acid testing (NAT), is also warranted. HBV vaccine, which was enforced in newborn vaccination programs in 2000, will have an important effect against the acquisition of HBV infection in the next generation within 20 or 30 years if HBV genome variability due to genotype or escape vaccine mutants does not interfere.
The natural course of HBV infection has been described in international reports on the basis of clinical observations from patients primarily from high endemic areas. Such information has been mistakenly extrapolated to predict the course of disease or its complications for patients in other countries, as in the case of the Latin American studies [6, 7]. The fact that in Mexico, HBV genotype H is predominant [14, 15] and that the HBsAg seroprevalence is low or very low in spite of the high frequency of anti-HBc in some of the studies groups may be indicative of that the natural course of liver diseases may be different from that reported in Asia and even South America where HBV genotype F predominates. Another possibility is that the diagnosis of liver disease caused by HBV infection is omitted and therefore remains underestimated mainly because NAT is not commonly performed in the country and the prevalence of occult hepatitis B in patients with liver cirrhosis is unknown to date.
On the other hand, the overall average of prevalence of cirrhosis per year reported by the Mexican Health Secretariat [85] and the low prevalence of HBV infection appear to be associated with the low incidence of HCC reported to date [27, 28]. These data are conciliatory with estimates made from the total Mexican population and the lowest percentage of HBsAg-positive patients (1%) who will present with chronic hepatitis per year (n = 3,000) and cirrhosis (20%; n = 600), and for patients with cirrhosis, only 18–30 cases would be expected (3–5%) to develop HCC per year. On the basis of these estimates, then only 0.2% of HBsAg-positive patients will develop liver cirrhosis and 0.01% HCC, data that are similar to those reported earlier [28]. These data reveal that Mexico could have the lowest incidence of HCC per 100,000 per year (0.01–0.02%) than among North America (1.8–2.0%), Europe (1.5–3.4%), South America (3.8–4.7%), and very distant Asian countries such as Japan where the incidence of HCC is estimated to be 20 per 100,000 per year [104, 105].
In Japan, HBV genotypes B and C are predominant and the reported prevalence of both HCV and HBV is 1.5% [105]. However, in the former, 80% of infected individuals become chronic carriers, whereas in the latter, only 20% develop chronic hepatitis and cirrhosis [105]. In contrast, in Mexico, a lower HBV and HCV prevalence [34] and the predominance of HBV genotype H [14, 15] may indicate that viral genotypes play an important role in the development and course of liver diseases. Therefore, further investigations regarding the variability of HBV genotype H compared with other genotypes and the genetic characteristics of the human population, as well as environmental factors, will be necessary in the future.
Abbreviations
- anti-HBc:
-
Antibody to hepatitis B core antigen
- CEP:
-
Counterelectrophoresis
- HBsAg:
-
Hepatitis B virus surface antigen
- HBV:
-
Hepatitis B virus
- HCC:
-
Hepatocellular carcinoma
- HCV:
-
Hepatitis C virus
- HIV:
-
Human immunodeficiency virus
- MP:
-
Mean prevalence
- NAT:
-
Nucleic acid testing
- PP:
-
Pooled prevalence
- WMP:
-
Weighted mean prevalence
References
Mast EE, Alter MJ, Margolis HS. Strategies to prevent and control hepatitis B and C virus infections: a global perspective. Vaccine 1999;17:1730–1733. doi:10.1016/S0264-410X(98)00415-0
World Health Organization. Department of Communicable Disease Surveillance and Response 2002, Hepatitis B [cited December 2007]. Available from: http://www.who.int/emc
Lavanchy D. Hepatitis B virus epidemiology, disease burden, treatment, and current and emerging prevention and control measures. J Viral Hepat 2004;11:97–107. doi:10.1046/j.1365-2893.2003.00487.x
Hou J, Liu Z, Gu F. Epidemiology and prevention of hepatitis B virus infection. Int J Med Sci 2005;2(1):50–57
Gish RG, Gadano AC. Chronic hepatitis B: current epidemiology in the Americas and implications for management. J Viral Hepat 2006;13(12):787–798. doi:10.1111/j.1365-2893.2006.00787.x
Fay OH. Hepatitis B in Latin America: epidemiological patterns and eradication strategy. The Latin American Regional Study Group. Vaccine 1990;8(Suppl):S100–S106
Silveira TR, da Fonseca JC, Rivera L, Fay OH, Tapia R, Santos JI, et al. Hepatitis B seroprevalence in Latin America. Rev Panam Salud Pública/Pan. Am J Public Health 1999;6(6):378–383
Ramiro Cruz J, Perez-Rosales MD. Availability, safety, and quality of blood for transfusion in the Americas. Rev Panam Salud Pública 2003;13(2–3):103–110
Campos RH, Mbayed VA, Pineiro Y, Leone FG. Molecular epidemiology of hepatitis B virus in Latin America. J Clin Virol 2005;34(Suppl 2):S8–S13. doi:10.1016/S1386-6532(05)80028-9
Ponce JG, Cadenas LF, Garcia F, Leon G, Blitz-Dorfman L, Monsalve F, et al. Alta prevalencia de marcadores de hepatitis B y C en una comunidad de indigentes en Caracas Venezuela. Invest Clin 1994;35(3):123–129
Echevarria JM, Leon P. Epidemiology of viruses causing chronic hepatitis among populations from the Amazon Basin and related ecosystems. Cad Saude Publica 2003;19(6):1583–1591. doi:10.1590/S0102-311X2003000600003
Miyakawa Y, Mizokami M. Classifying hepatitis B virus genotypes. Intervirology 2003;46(6):329–338. doi:10.1159/000074988
Norder H, Louroucé AM, Coursaget P, Echevarria JM, Lee SD, Mushahwar JK, et al. Genetic diversity of hepatitis B virus strains derived worldwide: genotypes, subgenotypes and HBsAg subtypes. Intervirology 2004;47(6):289–309. doi:10.1159/000080872
Sanchez LV, Maldonado M, Bastidas-Ramirez BE, Norder H, Panduro A. Genotypes and S-gene variability of Mexican hepatitis B virus strains. J Med Virol 2002;68(1):24–32. doi:10.1002/jmv.10166
Sanchez LV, Tanaka Y, Maldonado M, Mizokami M, Panduro A. Difference of hepatitis B virus genotype distribution in two groups of Mexican patients with different risk factors. Intervirology 2007;50(1):9–15. doi:10.1159/000096307
Arauz-Ruiz P, Norder H, Robertson BH, Magnius LO. Genotype H: a new Amerindian genotype of hepatitis B virus revealed in Central America. J Gen Virol 2002;83:2059–2073
Nakajima A, Usui M, Huy TT, Hlaing NKT, Masaki N, Sata T, et al. Full-length sequence of hepatitis B virus belonging to genotype H identified in a Japanese patient with chronic hepatitis. Jpn J Infect Dis 2005;58:244–246
Mbayed VA, Barbini L, Lopez JL, Campos RH. Phylogenetic analysis of the hepatitis B virus (HBV) genotype F including Argentine isolates. Arch Virol 2001;146(9):1803–1810. doi:10.1007/s007050170066
Norder H, Arauz-Ruiz P, Blitz L, Pujol FH, Echevarria JM, Magnius LO. The T (1858) variant predisposing to the precore stop mutation correlates with one or two major genotype F hepatitis B virus clades. J Gen Virol 2003;84(Pt 8):2083–2087. doi:10.1099/vir.0.19034-0
Huy TT, Ushijima H, Sata T, Abe K. Genomic characterization of HBV genotype F in Bolivia: genotype F subgenotypes correlate with geographic distribution and T (1858) variant. Arch Virol 2006;151(3):589–597. doi:10.1007/s00705-005-0671-1
Khan A, Tanaka Y, Saito H, Ebinuma H, Sekiguchi H, Iwama H, et al. Transmission of hepatitis B virus (HBV) genotypes among Japanese immigrants and natives in Bolivia. Virus Res 2008;132(1–2):174–180
Kao JH, Chen PJ, Lai MY, Chen DJ. Hepatitis B genotypes correlate with clinical outcomes in patients with chronic hepatitis B. Gastroenterology 2000;118:554–559. doi:10.1016/S0016-5085(00)70261-7
Kao JM. Hepatitis B viral genotypes: clinical relevance and molecular characteristics. J Gastroenterol Hepatol 2002;17(6):643–650. doi:10.1046/j.1440-1746.2002.02737.x
Tanaka Y, Mizokami M. Genetic diversity of hepatitis B virus as an important factor associated with differences in clinical outcomes. J Infect Dis 2007;195(1):1–4. doi:10.1086/509898
Ganem D, Prince AM. Hepatitis B virus infection—natural history and clinical consequences. N Engl J Med 2004;350(11):1118–1129. doi:10.1056/NEJMra031087
Pan CQ, Zhang JX. Natural history and clinical consequences of hepatitis B virus infection. Int J Med Sci 2005;2(1):36–40
Cortes-Espinoza T, Mondragón-Sanchez R, Hurtado-Andrade H, Sanchez-Cisneros R. Hepatocellular carcinoma and hepatic cirrhosis in Mexico: a 25 year necroscopy review. Hepatogastroenterology 1997;44(17):1401–1403
Vivas Arceo C, Bastidas Ramírez BE, Panduro A. Hepatocellular carcinoma is rarely present in Western Mexico. Hepatol Res 1999;16(1):26–35. doi:10.1016/S1386-6346(99)00035-2
Méndez-Sánchez N, Aguilar-Ramírez JR, Reyes A, Dehesa M, Juárez A, Castañeda B, et al. Etiology of liver cirrhosis in Mexico. Ann Hepatol 2004;3(1):30–33
Olaiz-Fernández G, Rivera-Dommarco J, Shamah-Levy T, Rojas R, Villalpando-Hernandez S, Hernández-Avila M, et al. Encuesta Nacional de Salud y Nutricion 2006. Cuernavaca Morelos (Mexico): Instituto Nacional de Salud Pública; 2006. p. 1–132 [cited December 2007]. Available from: http://www.insp.mx/ensanut/ensanut2006.pdf
Green S. Systematic reviews and meta-analysis. Singapore Med J 2005;46(6):270–274
Clarke M. Systematic reviews and the Cochrane Collaboration [cited November 2007]. Available from: http://www.cochrane.org/docs/whycc.htm
Landa L. Seroepidemiología de la hepatitis B. Gac Med Mex 1976;111(2):108–114
Chiquete E, Panduro A. Low prevalence of anti-hepatitis C virus antibodies in Mexico: a systematic review. Intervirology 2007;50:1–8. doi:10.1159/000096306
Valdespino JL, Conde-González CJ, Olaiz-Fernandez G, Palma O, Sepúlveda J. Prevalence of hepatitis B infection and carrier status among adults in Mexico. Salud Publica Mex 2007;49(Suppl 3):S404–S411
Marín LA, Luis LA, Ortega RM, López PS, Montiel MG. Marcadores serológicos indirectos (ALAT y anti-HBc) para hepatitis noA noB en donadores de sangre de la ciudad de Puebla. In Mem XXXI Jornada Agrup Mex Estudio Hematol; Oct 1990; Monterrey, Nuevo León, Mexico
Álvarez Muñoz MT, Bustamante Calvillo ME, Guiscafre Gallardo JP, Muñoz O. Hepatitis B y Delta: prevalencia de marcadores seroepidemiológicos en donadores de sangre voluntarios y su grupo familiar. Gac Med Mex 1991;127(5):399–404
Rivas Velazco R, Palomares BR, Gómez E, Moreno G, Martínez I, Badillo H. Enfermedades transmisibles en donadores de sangre en la zona oriente de la ciudad de México. In Mem XXXII Jornada Agrup Mex Estudio Hematol Oct 1991; Xalapa, Veracruz, Mexico
Rivas R, Gómez Martínez E, Martínez Pérez I, López Flores H, Fernández Jiménez A, Palomares B. Comportamiento de la seroprevalencia de enfermedades transmisibles en donadores de la zona oriente del Valle de México. In Mem XXXIV Jornada Agrup Mex Estudio Hematol Junio 1993; Guadalajara, Jalisco, Mexico
Souto Meiriño CA, Simón Domínguez J, Pulido Priego MA, Hernández Pérez A, García Hernández IC, Río Chiriboga CA. Prevalencia de marcadores para hepatitis A, B y C en un hospital de México. Salud Publica Mex 1994;36(3):257–262
Rivas Llamas R. Seroprevalencia y tendencia de la infección por VIH, VHB, VHC en donadores de sangre en la ciudad de Culiacán. Rev Med IMSS Mex 1996;34(6):487–493
Romero D, Villanueva M, Guzmán E, Bravo A. Prevalencia de anticuerpos contra hepatitis C en una población de disponentes familiares en la ciudad de México. In Mem XXXVIII Jornada Agrup Mex Estudio Hematol Mayo, 1997, León, Guanajuato, Mexico
Ayala Gaytan JJ, Guerra Avalos FJ, Mora Brondo P, Casillas Romo A. Prevalencia de marcadores virales para hepatitis B, C y Virus de la Inmunodeficiencia Humana en donadores de sangre voluntarios en el Noroeste de México. Rev Gastroenterol Mex 1997;62(4):250–253
Pita-Ramírez L, Torres-Ortiz GE. Prevalencia de anticuerpos virales y reaginas luéticas en donadores de sangre de un hospital. Rev Invest Clin 1997;49:475–480
Romero Martínez E. Selección de donadores sanguíneos: identificación de anti-HBc para evitar hepatitis postransfusional. Rev Med IMSS Mex 1998;36(4):327–332
Ramírez-Barragan J, Muñoz-Valle JF, Navarro-Hernández RE. Frecuencia de anticuerpos contra el HIV, HCV y HBsAg en donadores familiares en el Hospital del Carmen de la ciudad de Guadalajara, Jalisco. Rev Mex Patol Clin 1999;46(4):243–248
Méndez-Sánchez N, Baptista González H, Sánchez Gómez RH, Bordes Aznar J, Uribe Esquivel M. Prevalencia de hepatitis B y C en donadores de sangre en un hospital de tercer nivel de la ciudad de México. Salud Publica Mex 1999;41:475–478
Tristan Rojas CM, Nájera Tobias E, Cázares Taméz R, Flores Aréchiga A. Estudio comparativo de la seroprevalencia observada en diferentes bancos de sangre de la Republica Mexicana. XXVIII Congreso de Patología Clínica. Rev Mex Patol Clin 1999;46(1):34–35
Carreto-Velez MA, Carrada-Bravo T, Martínez-Magdaleno A. Seroprevalencia de VHB, VHC y VIH de donadores de sangre en Irapuato, México. Salud Publica Mex 2002;45(Suppl 5):S690–S693
Flores-Padilla L, Trejo-Franco J, Becerril-Brito J. Prevalencia de seromarcadores de hepatitis B y C en donadores del IMSS, Cd. Juarez, Chihuahua. XXVII Congreso Anual de la Asociación Mexicana de Infectologia y Microbiologia Clínica, A.C. 2002;22(3):106
Monteon VM, Reyes-Lopez PA, Sosa-Palacio A, Leon-Tello G, Martinez-Murguia J, Sosa-Jurado F. Heterogeneous distribution of the prevalence of anti-Trypsanosoma cruzi antibodies among blood donors in the State of Puebla, Mexico. Salud Publica Mex 2005;47(2):116–125. doi:10.1590/S0036-36342005000200005
Rivera-Lopez MRF, Zavala-Méndez C, Arenas-Esqueda A. Prevalencia de seropositividad para VIH, hepatitis B y C en donadores de sangre. Gac Med Mex 2004;140(6):657–660
Chiquete E, Sanchez LV, Becerra G, Quintero A, Maldonado M, Panduro A. Performance of the serologic and molecular screening of blood donations for the hepatitis B and C viruses in a Mexican Transfusion Center. Ann Hepatol 2005;4(4):275–278
García-Montalvo BM. Seropositividad de VIH, VHB, VHC y Treponema pallidum en donadores de sangre en el Sureste de Mexico. Rev Invest Clin 2006;58(6):567–572
Pita-Ramírez L, Rodríguez-Mejorada M. Comparación de dos poblaciones de sangre de la ciudad de Morelia. XLVII Congreso Nacional de Hematologia: Medicina Transfusional. Revista de Hematología 2006;7 (Suppl 1):S73
Cacique-Almazán J, Pérez-Martínez E, Gómez-Bravo A, Ángeles-Chimal JS. XLVII Congreso Nacional de Hematología: Medicina Transfusional. Rev Hematol 2006;7(Suppl 1):S71
Vázquez-Flores JA, Valiente-Banuet L, Marín y López RA, Sanchez-Guerrero SA. La seguridad de las reservas sanguíneas en la Republica Mexicana durante los años 1999 a 2003. Rev Invest Clin 2006;58(2):101–108
Álvarez Muñoz MT, Vázquez Rosales JG, Bustamante Calvillo ME, del Rey Pineda G, Arredondo García JL. Prevalencia de marcadores serológicos para los virus B y C de la hepatitis en una cohorte de mujeres embarazadas del Valle de México. Bol Med Hosp Infant Mex 1995;52(3):143–147
Ortiz Ibarra F, Figueroa Damian R, Lara Sánchez J, Arredondo García JL, Ahued Ahued JR. Prevalencia de marcadores serológicos de los virus de la hepatitis A, B, C y D en embarazadas. Salud Publica Mex 1996;38:317–322
Hernández Arriaga JL, Ramírez Crespo A, a Gómez M, Castellanos Martínez J. Marcadores serológicos de hepatitis B en la etapa perinatal. Bol Med Hosp Infant Mex 2000;57(12):682–685
Vazquez Martínez JL, Coreño Juárez MO, Montaño Estrada LF, Attlan M, Gómez Dantés H. Seroprevalencia de hepatitis B en mujeres embarazadas en México. Salud Publica Mex 2003;45(3):165–170
Kerschenobich D, Hurtado R, Collawin C, Bobadilla J, Cabrera G, Borovoy J, et al. Seroprevalencia de marcadores virales de hepatitis B en profesionales de la salud. Estudio multicéntrico en México. Rev Invest Clin 1990;42(4):251–256
Navarrete-Navarro S, Alvarez-Muñoz MA, Bustamante C, Vallejo Aguilar OJ, Muñoz O, Santos-Preciado JI, et al. Protección contra hepatitis B en trabajadores de salud con vacuna de DNA recombinante. Bol Med Hosp Infant Mex 1992;49(11):739–742
Flores Calderón J, Álvarez Muñoz MT, Bustamante Calvillo ME, Vázquez Rosales G, Reyes Morales H. Prevalencia de marcadores serológicos para el virus de la hepatitis B en personal de un hospital pediátrico. Bol Med Hosp Infant Mex 1994;51:99–104
Villasis-Keever MA, Peña LA, Miranda Novales G, Alvarez Muñoz MT, Damasio Santana RA, López Fuentes G, et al. Prevalence of serological markers against measles, varicella, hepatitis B, hepatitis C, and human immunodeficiency virus among medical residents in Mexico. Prev Med 2001;32(5):424–428. doi:10.1006/pmed.2001.0825
Méndez-Sánchez N, Motola-Kuba D, Zamora-Valdés D, Sánchez-Lara K, Ponciano-Rodríguez G, Uribe-Ramos MH, et al. Risk factors and prevalence of hepatitis virus B and C serum markers among nurses at a tertiary-care hospital in Mexico City, Mexico: a descriptive study. Ann Hepatol 2006;5(4):276–280
Flores Castañeda MS, García Méndez BL, Tijerina Menchaca R. Seropositividad de la infección por HCV y VHB en estudiantes universitarios del Estado de Nuevo León, México. Rev Gastroenterol Mex 1996;61(4):327–331
Hyams KC, Escamilla J, Lozada Romero R, Macareno Alvarado E, Bonilla Giraldo N, Papadimos TJ, et al. Hepatitis B infection in a non-drug abusing prostitute population in Mexico. Scand J Infect Dis 1990;22(5):527–531. doi:10.3109/00365549009027091
Valdespino Gómez JL, García García ML, del Río Chiriboga C, Loo Méndez E, López Sotelo A. Las enfermedades de transmisión sexual y la epidemia de VIH/SIDA. Salud Publica Mex 1995;37(6):549–555
Uribe-Salas F, Hernández-Giron C, Conde-González C, Cruz-Valdez A, Juárez-Figueroa L, Hernández-Avila M. Characteristics related to STD/HIV in men working in bars with prostitutes in Mexico City. Salud Publica Mex 1995;37:385–393
Juárez-Figueroa LA, Uribe-Salas FJ, Conde-González CJ, Hernández-Avila M, Hernández-Nevarez P, Uribe-Zúñiga P, et al. Hepatitis B markers in men seeking human immunodeficiency virus antibody testing in Mexico City. Sex Transm Dis 1997;24(4):211–217
Hernández-Girón C, Uribe-Salas F, Conde-González C, Cruz-Valdez A, Juárez-Figueroa L, Uribe-Zúñiga P, et al. Seroprevalencias a diversos virus y características sociodemográficas en mujeres que buscan detectarse VIH. Rev Invest Clin 1997;49:5–13
Juárez-Figueroa L, Uribe-Salas F, Conde-González C, Hernández-Ávila M, Olamendi-Portugal M, Uribe-Zúñiga P, et al. Low prevalence of hepatitis B among Mexican female sex workers. Sex Transm Infect 1998;74:448–450
Uribe-Salas F, Hernández-Avila , Juárez-Figueroa L, Conde-González CJ, Uribe-Zuñiga P. Risk factors for herpes simplex virus type 2 infection among female commercial sex workers in Mexico City. Int J STD AIDS 1999;10(2):105–111. doi:10.1258/0956462991913727
Uribe-Salas F, Conde-González CJ, Juárez-Figueroa L, Hernández-Castellanos A. Sociodemographic dynamics and sexually transmitted infections in female sex workers at the Mexican-Guatemalan border. Sex Transm Dis 2003;30(3):266–271. doi:10.1097/00007435-200303000-00018
Tamez Treviño E, Tijerina Menchaca R, Bosques Padilla F, Rangel Orozco R, Isibasi A, Flores Castañeda MS. Frecuencia de la infección con VHC, VHB o VIH no diagnosticada en pacientes hepatópatas. Med Universitaria 2002;4(16):148–152
Campollo O, Valencia-Salinas JJ, Berumen-Arellano A, Pérez-Aranda MA, Panduro-Cerda A, Segura-Ortega J. Características epidemiológicas de la cirrosis hepática en el Hospital Civil de Guadalajara. Salud Publica Mex 1997;39:195–200. doi:10.1590/S0036-36341997000300004
Porras Nuñez LO, Balderas Ávila R, Lejia Guzman M, Mattar Olivo C. Core M marcador útil de hepatitis B en pacientes de hemodiálisis. Rev Mex Patol Clin 2002;49(3):148–152
Treviño Hernández R, Pérez Ramírez JL, Cruz Valdez J, Ramírez B, et al. Prevalencia de hepatitis C y B en pacientes con insuficiencia renal crónica en programa de hemodiálisis en el Hospital Universitario y Centro Renal de Monterrey. Med Universitaria 2003;5(21):228–232
Kato-Maeda M, Ponce-de-Leon S, Sifuentes-Osoirnio J, Rangel-Frausto MS, Calva-Mercado J, Infante-Surez L, et al. Bloodborne viral infections in patients attending an emergency room in Mexico City: estimate of seroconversion probability in healthcare workers alter an occupational exposure. Infect Control Hosp Epidemiol 2000;21(9):600–602. doi:10.1086/501811
Alvarado-Esquivel C, Arreola-Valenzuela MA, Mercado-Suarez F, Espinoza-Andrade F. Hepatitis B virus infection among inpatients of a psychiatric hospital of Mexico. Clin Pract Epidemol Ment Health 2005;1:10. doi:10.1186/1745-0179-1-10
Alvarez Muñoz MT, Bustamante Calvillo MA, Martínez García MC, Moreno Altamirano L, Guiscafre-Gallardo H, Guiscafre JP, et al. Seroepidemiology of the hepatitis B and delta in the southeast of Chiapas, Mexico. Arch Invest Med (Mex) 1989;20(2):189–195
Cisneros-Castolo M, Hernández-Ruiz L, Ibarra-Robles IE, Fernández-Gárate IH, Escobedo-de la Peña J. Prevalence of hepatitis B virus infection and related risk factors in a rural community of Mexico. Am J Trop Med Hyg 2001;65(6):759–763
Roman S, Panduro A, Maldonado M, Sanchez C, Quezada D, Martinez E, et al. High prevalence of occult hepatitis B infection among different Mexican ethnic groups. Liver Int 2006;26(Suppl 1):S51
Secretaria de Salud. México, Sistema Único de Vigilancia Epidemiológica. Dirección General de Epidemiología. Anuario de Morbilidad 1984–2006 [cited December 2007]. Available from: http://www.dgepi.salud.gob.mx/anuario/mdex.html
Secretaria de Salud. México, Sistema Nacional de Información en Salud, Reporte de Mortalidad 2000–2005 [cited December 2007]. Available from: http://sinais.salud.gob.mx/mortalidad
Instituto Nacional de Estadisticas. Geografia e Informatica (INEGI). Censo General de Población y Vivienda 2000 (data on CD-ROM). Aguascalientes (Mexico): INEGI; 2001
Celis A, Gaxiola-Robles R, Sevilla-Godinez E, Orozco-Valerio MJ, Armas J. Tendencia de la mortalidad por picaduras de alacran en Mexico, 1979–2003. Rev Panam Salud Publica 2007;21(6):373–380. doi:10.1590/S1020-49892007000500005
Taylor RN, Fulford KM. Results of the Center for Disease Control Proficiency Testing Program for the detection of hepatitis B surface antigen. J Clin Microbiol 1976;4(1):32–39
Weber B, Bayer A, Kirch P, Schlüter V, Schlieper D, Melchior W. Improved detection of hepatitis B virus surface antigen by a new rapid automated assay. J Clin Microbiol 1999;37(8):2639–2647
Diepersloot RJ, van Zantvliet-van Oostrom Y, Gleaves CA. Comparison of a chemiluminescent immunoassay with two microparticle enzyme immunoassays for detection of hepatitis B virus surface antigen. Clin Diagn Lab Immunol 2000;7(6):865–866. doi:10.1128/CDLI.7.6.865-866.2000
Gerlich WH. Diagnostic problems caused by HBsAg mutants—a consensus report of an expert meeting. Intervirology 2004;47(6):310–313. doi:10.1159/000080873
Ly TD, Servant-Delmas A, Bagot S, Gonzalo S, Férey MP, Ebel A, et al. Sensitivities of four new commercial hepatitis B virus surface antigen (HBsAg) assays in detection of HBsAg mutant forms. J Clin Microbiol 2006;44(7):2321–2326. doi:10.1128/JCM.00121-06
Food and Drug Administration. Test for hepatitis B surface antigen. Fed Regist 1975;40:P29706–P29712
Principles in evaluation of HBsAg test kits: appropriate use of 2nd WHO International Standard (IS) and Reference Panel for HBsAg. Geneva: World Health Organization; Nov 2004 [cited September 15, 2008]. Available from: http://www.who.int/entity/bloodproducts/publications/en/HBsAg_application_ECBS_2004pdf
Mizuochi T, Okada Y, Umemori K, Mizusawa S, Sato S, Yamaguchi K. Reactivity of genotypically distinct hepatitis B virus surface antigens in 10 commercial diagnostic kits available in Japan. Jpn J Infect Dis 2005;58(2):83–87
van Roosmalen MH, de Jong JJ, Haenen W, Jacobs T, Couwenberg F, Ahlers-de Boer GJ, et al. A new HBsAg screening assay designed for sensitive detection of HBsAg subtypes and variants. Intervirology 2006;49(3):127–132. doi:10.1159/000089373
Togashi H, Hashimoto C, Yokozawa J, Suzuki A, Sugahara K, Saito T, et al. What can be revealed by extending the sensitivity of HBsAg detection to below the present limit? J Hepatol 2008;49(1):17–24. doi:10.1016/j.jhep.2008.03.019
Baptista González HA, Kourchenko Raab H, Rosenfeld Mann F, Rizo Almenara S, Peñuela Olaya MA. Estudio de infecciones virales en el lactante menor transfundido en la etapa neonatal. Bol Med Hosp Infant Mex 1998;55(7):386–392
Cervantes Bustamante R, Ramírez Mayans J, Zarate Mondragón F, Mata Rivera N, Munguia Venegas P, Mason Cordero T, et al. Marcadores serológicos para el virus de Hepatitis B en un grupo de niños mexicanos. Acta Pediatr Mex 2002;23(6):352–354
Norma Oficial Mexicana NOM. 003/SSA2/1993. Normas y Técnicas para la Disposición de Sangre Humana y sus Componentes con Fines Terapéuticos. Diario Oficial de la Federación del 18 de Julio del 1994 [cited November 2007]. Available from: http://www.salud.gob.mx/unidades/cdi/nom/003ssa23.html
Norma Oficial Mexicana. NOM-031-SSA2-1999, para la atencion a la salud del niňo. Diario Oficial de Federacion del 9 de junio del 2000 [cited November 2007]. Available from: http://www.salud.gob.mx/unidades/cdi/nom/031ssa29.html
CONADICT. Statistics on Drug Abuse Patterns, Mexico 2001 [cited January 2008]. Available from: http://www.conadic.gob.mx/pre/ena2002.html
Simonetti RG, Camma C, Fiorello F, Politi F, D’amico G, Pagliaro L. Hepatocellular carcinoma. A worldwide problem and the major risk factors. Dig Dis Sci 1991;36:962–972. doi:10.1007/BF01297149
Tanaka Y, Kurbanov F, Mano S, Orito E, Vargas V, Esteban JI, et al. Molecular tracing of the global hepatitis C virus epidemic predicts regional patterns of hepatocellular carcinoma. Gastroenterology 2006;130(3):703–714. doi:10.1053/j.gastro.2006.01.032
Acknowledgment
This work was supported by a grant (Salud-Conacyt-2004-01-025) to A.P. from the National Council of Science and Technology (CONACYT, Mexico).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roman, S., Panduro, A., Aguilar-Gutierrez, Y. et al. A low steady HBsAg seroprevalence is associated with a low incidence of HBV-related liver cirrhosis and hepatocellular carcinoma in Mexico: a systematic review. Hepatol Int 3, 343–355 (2009). https://doi.org/10.1007/s12072-008-9115-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12072-008-9115-9