Abstract
Deviated nasal septum (DNS) causes nasal obstruction, secretions, decreased sense of smell, bleeding, headache and snoring. This study aims to compare endoscopic-assisted septoplasty versus conventional septoplasty in terms of surgical outcome and intra- and post-operative complications. A prospective study was done on 50 patients aged between 18 and 41 years of which, 41 (82%) cases were males and 9 (18%) were females who had DNS based on clinical examination and diagnostic nasal endoscopy. Patients were randomized by simple randomization into two groups. Functional outcome was assessed using nasal surgical questionnaire (NSQ) prior to and after surgery for 3 months post-operatively and complications associated with the surgery were compared between two groups. In this study, most of the patients had anterior dislocations, present in 37 cases (74%). Improvement in pre- to post-operative visual analogue scale (VAS) for nasal obstruction was significantly better in endoscopic-assisted than conventional septoplasty (p < 0.001*). Pre-and post-operative differences in 4-point likert scale for other nasal symptoms like decreased sense of smell, snoring, secretions, headache and crusting were better in endoscopic-assisted septoplasty (p < 0.001*). Complications in endoscopic-assisted septoplasty were less common compared to conventional septoplasty (p = 0.05). In endoscopic-assisted septoplasty patients, pre-to post-operative NSQ (Nasal Surgical Questionnaire) VAS improvement for nasal obstruction, likert scale change from pre-to post-op were better and complications were lesser compared to conventional septoplasty. This suggests endoscopic-assisted septoplasty has better surgical outcomes and fewer complications and posterior deviations, spurs and inferior deviations can be corrected with ease and fewer complications.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Surgery on a deviated nasal septum has seen several modifications since its inception, starting from radical septal resection to mucosal preservation and subsequent preservation of the possible septal framework. Various techniques have been described for the correction of different types of septal deviations in the past. The concept of SMR was popularized and refined by Killian [1] and Freer [2] separately in the early twentieth century.
According to Brennan et al. [3] the ideal objective in septal surgery is permanent correction of deviation with avoidance of any complication. Four basic principles are consistent with this objective: good exposure; safe elevation of flaps; resection of only a limited, necessary amount of septum; and elimination of aetiological dynamic forces.
The traditional approach to septoplasty involves headlight illumination, visualization through a nasal speculum, and surgical instruments that are typically disparate from that used during standard endoscopic procedures. These circumstances can be suboptimal when treating a narrow nose, approaching posterior deviation and correction of subluxation of septum over maxillary crest. In addition, impaired visualization may predispose to nasal mucosal trauma.
Endoscopic septoplasty is an attractive alternative to traditional headlight septoplasty. Of these four principles described by Brennan et al. the first three are best achieved by an endoscopic approach to the septum. The current study was conducted to compare the outcomes of endoscopic-assisted and conventional septoplasty among patients with the help of Nasal surgical questionnaire (NSQ) to assess the functional outcomes and diagnostic nasal endoscopy to assess the post operative complications.
Materials and Methods
A prospective study was done in 50 patients presenting with symptomatic Deviated Nasal Septum to the department of ENT and Head and Neck surgery at S.Nijalingappa Medical College and Hanagal Sri Kumareshwar Hospital and Research Centre, Bagalkot from 1st January 2019 to 30th June 2020 (18 months).
Study Design
It is a Randomized control study.
Method of Randomization
Simple randomization done using computer generated random table into
-
Group 1: Patients undergoing conventional septoplasty
-
Group 2: Patients undergoing endoscopic-assisted septoplasty.
Sample Size
Sample size calculation was done using open epi software ver2.3.1
At 95% confidence interval
80% power of study
Sample size calculated using the formula=\(2\left( {{\text{Z}}\upalpha + {\text{Z}}\upbeta } \right)2{\overline{\text{p}}}\left( {1 - {\overline{\text{p}}}} \right)/{\text{d}}\)
With a drop-out rate of 10% to follow-up,
Total sample size: 50
25 in each group
Inclusion Criteria
-
1.
Age group of 18 to 60 years
-
2.
Patient willing to give informed consent
-
3.
Patients with deviated nasal septum and spurs established clinically and endoscopically
Exclusion Criteria
-
1.
Patient not willing to give informed consent
-
2.
Age < 18 years and > 60 yrs
-
3.
Patients with allergic sinusitis
-
4.
Pregnancy
-
5.
Anemia and malnutrition
-
6.
Malignancies
Patients diagnosed with deviated nasal septum on the basis of clinical features, clinical examination and diagnostic nasal endoscopy were put in either of the two groups i.e.group 1 (Patient’s undergoing conventional septoplasty) or group 2 (Patient’s undergoing endoscopic-assisted septoplasty) using computer generated simple random method.
A detailed explanation of the procedure and the purpose of the study was offered to each patient. The patients fulfilling the inclusion criteria were enrolled for the study after obtaining informed consent. Meticulous preoperative examination was done by anterior rhinoscopy, diagnostic nasal endoscopy for all patients to assess the type and severity of the type of septal deformity present; such as right deviation, left deviation, inferior deviaton, posterior deviation and spurs Pre-operative functional/symptom assessment was done using nasal surgical questionnaire and visual analogue scale and was given to all the patients involved in the study. X ray nose and PNS-water’s view were done for all patients involved in the study. CT scans of the paranasal sinuses were done only when chronic sinusitis was suspected. Preoperative routine investigations such as complete blood count, bleeding time, coagulation time, urine routine, random blood sugar, blood urea, serum creatinine, ECG, and chest X-ray were done for all patients. Intra-operative and immediate post-operative complications such as synechiae, external deformities, mucosal tear, septal perforation were compared between the two groups.
All patients were evaluated on 5th day, 15th day and 3rd month post-operatively, regarding any improvement and if yes the degree of improvement (complete, substancial, mild, no improvement, worse), whether posterior deviations, septal spurs, high septal deviations were corrected, also the accompanying symptoms as a headache, secretions, crusting, snoring, bleeding and decreased sense of smell, whether disappeared or still persistent using Nasal surgical questionnaire (NSQ) [4] and Visual analogue score (VAS).
The data collected was analyzed statistically by SPSS software version 22. Percentages & proportions for qualitative data, student's t test for quantitative data, chi-square test for qualitative data and for association. Mean and standard deviations were used. Other statistically appropriate parametric and non parametric tests were used wherever they were needed such as Mann–Whitney U test for independent variables and Friedman test for k independent variables were used.p < 0.05 was considered as statistically significant.
Assessment Tools
Following tools were used in the study.
-
1.
Pre and post-operative diagnostic nasal endoscopy (DNE) were done using 00 rigid nasal endoscope (4 mm) Karl Storz connected to a monitor and recorded using ScopyDoc endoscopic image management system.
-
2.
Intra-operative use of headlight fitted to fibreoptic light source (Quartz Halogen Cold light source 24 V 250 watts) in conventional septoplasty and in endoscopic-assisted septoplasty 00 rigid nasal endoscope (4 mm) Karl Storz Hopkins 7230AWA connected to a hp monitor and recorded and edited using ScopyDoc endoscopic image management system.
-
3.
Functional outcome was measured using nasal surgical questionnaire (NSQ) [4]: Visual analogue scale (VAS) was assessed for nasal obstruction from 0 to 100 for day, night and exercise and likert scale was assessed for other nasal symptoms.
-
4.
Post-operative complications was assessed after removing the anterior nasal pack on 2nd post-operative day by anterior rhinoscopy and DNE.
Results
Most of the patients were in the age group of 18–20 years (46%) and 21–30 years (36%) in the present study. In group 1, 52%(13) patients were in the age group of 18–20 years whereas in group 2, 40%(10) patients were in the age group of 18–20 yrs. Mean age of the study population was 24.52 ± 7.271 yrs. Youngest patient was 18 yrs and oldest was of 41 yrs in the study.
In this study 41 patients (82%) were males and 9 patients (18%) were females with a M:F ratio of 4.1:1.
Most common type of septal deformity was type 1 Baumann’s classification of deviated nasal septum in both group 1 with 10 cases (40%) and group 2 with 13 (52%) cases in the present study (Table 1).
On Pre-op diagnostic nasal endoscopy and computed tomography scans (if done) various anatomical variations of the septum were seen. Most common anatomical abnormality was anterior deviations/cartilaginous deviations in both group 1 (68% of cases) and group 2 (80% cases). Other anatomical abnormalities such as posterior/bony deviations, spurs/bony cartilaginous deviations/sharp bony deviations, inferior deviations/subluxation of maxillary crest and cartilage junction and caudal deviations were also observed (Table 2).
The nasal obstruction VAS scores were measured pre operatively and post operatively at day 15, 1 month and 3 months and a VAS score from 0–100 for day, night and exercise each was marked by the patient and recorded manually. Comparison of VAS scores for nasal obstruction was done and it was observed that the mean VAS score for nasal obstruction decreased significantly for both the groups. In Group 1 it reduced from 172.4 to 59.6 and 183.20 to 12 in group 2. The improvement in VAS score was statistically significant at post-operative 1 month and 3 months duration with p value of 0.003 and < 0.001 respectively, when compared between the two groups (Table 3; Fig. 1).
In group 1, the mean pre-op and post-op VAS scores for nasal obstruction was measured for day and night for both the groups. The mean pre-op VAS score for day was 72.8 and post operative VAS score at 15th day, 1 month and 3 months were 30.8, 30.4 and 28.4 respectively and mean pre-op VAS score for night was 76.0 and post-operative VAS score at 15th day, 1 month and 3 months was 35.6, 35.2 and 31.2 respectively. This shows significant improvement in both day and night VAS scores with p values of < 0.001 (Table 4).
In group 2, the mean pre-op VAS score for day was 76.8 and post operative VAS score at 15th day, 1 month and 3 months were 26.0, 20.8, 6 respectively. The mean pre-op VAS score for night was 82.8 and post operative VAS score at 15th day, 1 month and 3 months were 31.2, 22.4 and 6.4 respectively. This shows significant improvement in both day and night VAS scores with p values of < 0.001 (Table 5).
A retrospective scale of improvement in breathing with complete, substantial, mild, or no improvement or worsening of symptoms was given post operatively. The pre to post operative change in day for each level of perceived improvement in nasal obstruction was recorded which showed complete improvement in breathing in 3 cases (12%) in group 1 and 3 cases (12%) in group 2, substantial improvement in breathing in 15 cases (60%) in group 1 and 19 cases (76%) in group 2 and mild improvement in breathing in 7 cases (28%) and 3 cases (12%) in group 1 and 2 respectively at 15th day post-operatively. 5 (20%) patients had complete improvement and 19 (76%) patients had substantial improvement in group 2 at 1 month post-operatively. There was complete improvement in breathing in 15 (60%) cases in group 2, compared to 3 (12%) cases in group 1 at 3 months post operatively. At 1 month and 3 months postoperatvively results were similar to post op day 15 in group 1 (Table 6).
The pre to post operative change in night for each level of perceived improvement in nasal obstruction was recorded which showed substantial improvement in breathing in 17 cases (68%) in group 1 and 22 cases (88%) in group 2 and mild improvement in breathing in 8 cases (32%) and 2 cases (8%) in group 1 and 2 respectively at 15th post operative day. There was complete improvement in breathing in 15 (60%) cases in group 2 and no cases in group 1 had complete improvement in night VAS scores at 3 months post operatively (Table 7).
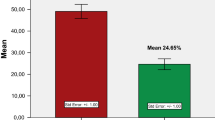
Mann–Whitney U test is applied in the Table 8 to compare between the two groups, which showed a statistical significance of p value 0.007 at post-op 1 month and < 0.001 at post-op 3 months in the total likert scale for other nasal symptoms such as decreased sense of smell, bleeding, snoring, secretions, headache and crusting (Fig. 2).
Most common intra operative complication in the present study was unilateral mucosal flap tear with 17 cases (68%) in group 1 and 8 cases (32%) in group 2. Intra operative mucosal flap tear was more common in group 1 than in group 2 which was statistically important with p value of 0.011. 2 cases in group 1 had intra-op septal perforation. Most common post-operative complication were early post-op bleeding and synechiae between the mucosal flap and turbinates. 15 cases in group 1 (60%) and 10 cases (40%) in group 2 had early post-operative bleeding and 16 cases (64%) in group 1 and 4 cases (16%) in group 2 had synechiae with a p value of 0.003 which was statistically significant between the two groups. 1 case in group 1 had post op external deformity in the form of supra tip depression (Table 9).
Discussion
Most of the patients were in the age group of 18–20 years (46%) and 21–30 years (36%) in the present study. Mean age of the study population was 24.52 ± 7.271 yrs. In group 1, 52%(13) patients were in the age group of 18–20 years whereas in group 2, 40%(10) patients were in the age group of 18–20 yrs. Youngest patient was 18 yrs and oldest was 41 yrs in the study. Similar to this study, in a study of 50 cases done by Sathyaki et al. [5] the age of the patients was varying between 10 and 60 years and in the group who underwent conventional septoplasty, the average age was 29.76 years (range was 10–50 years) and in the endoscopic septoplasty group, the average age was 27.88 years (range was 18–60 years) and the overall average was 28.82 years (Figs. 3, 4, 5).
In a study which was carried out on 100 patients by El Nasr et al. [6] fifty underwent endoscopic septoplasty (group A) while the other fifty underwent conventional septoplasty (group B). Their ages ranged between 16 to 34 (the mean age was 24.30 ± 9.59 years) and 19 to 38 (the mean was 25.70 ± 6.26 years) in group A and B, respectively, which is similar to the present study.
In this study 41 patients (82%) were males and 9 patients (18%) were females with a 4:1 ratio. 20 patients in group 1 and 21 patients in group 2 were males and 5 patients in group 1 and 4 patients in group 2 were females. This is in agreement with study done by Gulati et al. [7] in which there were 20 males (80%) and 5 (20%) females in each group.
Most common type of septal deformity was type 1 Baumann’s classification of deviated nasal septum in both group 1 with 10 cases (40%) and group 2 with 13 (52%) cases in the present study. It is in accordance with a study done by Eren et al. [8] which had the type 1 deformity as the most common type, with 22 cases out of 86 having the same.
Most common anatomical abnormality was anterior deviations/cartilaginous deviations in both group 1 (68% of cases) and group 2 (80% cases) on pre-op diagnostic nasal endoscopy and computed tomography scans in this study. This is in accordance with the study done by Kaushik et al. [9] where they observed that anterior deviations, 14 cases out of 30 in traditional septoplasty and 10 cases out of 30 in endoscopic septoplasty, were more common in both the endoscopic and conventional group than posterior deviations and spurs.
In a prospective study of 50 cases of deviated nasal septum between Oct. 2014 and March 2016, done by Chandra et al. [10] where patients were randomly divided equally in 2 groups for endoscopic (A) and conventional (B) septoplasty respectively. They observed that 48% patients had anterior deviation and spur was seen in 22% of patients which is similar to the findings in our study.
El Nasr et al. [7] have done a study on 100 patients in which 50 patients underwent conventional septoplasty and 50 underwent endoscopic septoplasty. Preoperative total mean NSQ VAS score for endoscopic septoplasty was 86.9 ± 6.7 and for conventional septoplasty was 83.12 ± 3.88 which reduced to 40.88 ± 14.18 in endoscopic septoplasty and 48.22 ± 15.10 in conventional septoplasty patients with p value of 0.001 in both the groups. In our study, the improvement in mean VAS score was statistically significant at post-operative 1 month and 3 months duration with p value of 0.003 and < 0.001 respectively, when compared between the two groups, suggesting better VAS score reduction achieved with endoscopic-assisted septoplasty compared to conventional septoplasty.
A retrospective scale of improvement in breathing with complete, substantial, mild, or no improvement or worsening of symptoms was given post operatively which showed better improvement in endoscopic-assisted group than conventional group. Similar to this scale Bayraktar et al. [11] have used a patient satisfaction scale from 1 to 5 in which 20 patients out of 51 (39.2%) had a score of 5 and 27 out 51 (52.9%) had a score of 4 in endoscopic-assisted septoplasty compared to just 5 patients out of 30 (16.7%) had a score of 5 in conventional septoplasty cases.
In a study done by Garzaro et al. [12] on 276 patients, NOSE score was used for subjective assessment and it showed statistical improvement in both groups: mean traditional septoplasty score decreased from 14.4 ± 2.37 to 5.2 ± 1.8 (p < 0.05), while in endoscopic septoplasty group it decreased from 14.7 ± 2.14 to 4.7 ± 1.7 (p < 0.05). However, they found no statistical difference between the two techniques at pre- and postoperative evaluations, concerning total nasal resistance and NOSE score.
El Nasr et al. [7] have done a study on 100 patients in which 50 patients underwent conventional septoplasty and 50 underwent endoscopic septoplasty. They observed that the likert scale for other nasal symptoms, had a significant improvement of the postoperative nasal discharge in both groups (p = 0.0001), while postoperative headache, snoring, hyposmia, and epistaxis showed insignificant improvement. In contrast, in our study there was a statistically significant change in scores for decreased sense of smell, snoring, secretions and crusting at post-operative period of 3 months with p value of 0.039, 0.020, 0.039 and 0.002 respectively between the two groups. There was a statistically significant change in scores for headache at 1 month and 3 months post operatively with p value of 0.017 and 0.002 respectively.
Most common intra operative complication in the present study was mucosal flap tear with 17 cases (68%) in group 1 and 8 cases (32%) in group 2 having the same. Most common post-operative complication were early post-op bleeding and synechiae between the mucosal flap and turbinates. 15 cases in group 1 (60%) and 10 cases (40%) in group 2 had early post-operative bleeding and 16 cases (64%) in group 1 and 4 cases (16%) in group 2 had synechiae.
When the two groups were compared there were lesser complications in group 2 than group 1 with respect to intra-op mucosal flap tear and post-op synechiae with a p value of 0.011 and 0.003 respectively which was statistically significant. Overall complications were more common in conventional septoplasty than endoscopic septoplasty with a significant difference (p value of 0.05 on applying paired t-test). Removal of posterior deviations, inferior deviations and spurs resulted in lesser intra-operative and post-operative complications in endoscopic-assisted septoplasty group than conventional group suggesting that endoscopic-assisted septoplasty results in lesser incidence of mucosal flap tear or perforation because it is easier to raise the mucoperichondrial flap without damaging it. It is partly due to better visualization that is offered by the endoscopic-assisted technique.
Similarly In a prospective observational study done by Garzaro et al. [12] on 276 consecutive patients affected by deviated nasal septum, septal tears/perforation were observed in 17 (11.56%) patients in traditional septoplasty and 7 (5.43%) patients in endoscopic septoplasty and synechiae were seen in 22 (14.96%) cases in traditional septoplasty and5 (3.88%) cases in endoscopic septoplasty and early post op bleeding in 10 (6.80%) cases in traditional septoplasty and 1 (0.78%) case in endoscopic septoplasty with statistical significance between the two groups with p value < 0.05.
In a randomized prospective study on 60 patients done by Elbanhawy et al. [13] in which 30 patients underwent conventional septoplasty and 30 patients underwent endoscopic septoplasty, most common complication was intraoperative flap tear, occurring in 5 (16.7%) patients undergoing endoscopic septoplasty compared to 10 (33.3%) patients undergoing conventional septoplasty.
In a cross-sectional comparative study done by Rajguru et al. [14] on 100 patients with 50 patients who underwent conventional septoplasty and 50 patients underwent endoscopic septoplasty, mucosal tear was seen in 9 (18%) patients in conventional septoplasty and 2 (4%) cases in endoscopic septoplasty which was the most common complication in their study. When compared between the two groups, there was statistically significant difference with p value of 0.026. Synechiae was seen in 10 (20%) cases and 1 (2%) case in conventional and endoscopic septoplasty with a p value of 0.0042 when compared.
Conclusion
-
1.
In this study it was seen that endoscopic-assisted procedure possesses the following advantages over conventional septoplasty such as minimal manipulation,minimal damage to the tissues,minimal removal of septum, hence precise reconstruction, stability of the septum is not compromised, mucosal tears are avoided, hence less chance of synechiae formation,easier to correct posterior deviation, inferior deviations and spurs.
-
2.
Functional outcome using nasal surgical questionnaire showed better outcomes in endoscopic-assisted septoplasty compared to conventional septoplasty.
-
3.
Intra and post-op complications were less common in endoscopic-assisted septoplasty compared to conventional septoplasty.
Limitations of the study
Due to short study period and small sample size, results of the study cannot be generalized. Large sample study and prolonged follow up is required for better scientific evidence from the study.
References
Killian G (1905) The submucous window resection of nasal septum. Ann Otol Rhinol Laryngol 14:363–393
Freer OT (1902) The correction of deflection of nasal septum with minimal traumatism. JAMA 38:636–642
Brennan LG (1996) Minimizing postoperative care and adhesions following endoscopic sinus surgery. Ear Nose Throat J 75(1):45–48
Haye R, Tarangen M, Shiryaeva O, Dosen LK. Evaluation of nasal surgical questionnaire for monitoring results of septoplasty. Int J Otolaryngol 2015:563639
Sathyaki DC, Geetha C, Munishwara GB, Mohan M, Manjunath K (2014) A comparative study of endoscopic septoplasty vs conventional septoplasty. Indian Otolaryngol HeadNeckSurg 66(2):155–161
El Nasr AA, Belih MAM (2018) Assessment of the nasal obstruction after endoscopic septoplasty compared with conventional technique by computed tomography and Nasal Surgical Questionnaire. Egypt J Otolaryngol 34:272–277
Gulati SP, Wadhera R, Ahuja N, Garg A, Ghai A (2009) Comparative evaluation of endoscopic with conventional septoplasty. Indian J Otolaryngol Head Neck Surg 61(1):27–29
Eren SB, Tugrul S, Dogan R, Ozucer B, Ozturan O (2014) Objective and subjective evaluation of operation success in patients with nasal septal deviation based on septum type. Am J Rhinol Allergy 28(4):e158–e162
Kaushik S, Vashistha S, Jain NK (2013) Endoscopic vs conventional septoplasty: a comparative study. Clin Rhinol Int J 6(2):84–87
Chandra S, Baisakhiya N (2017) A comparative study of endoscopic versus conventional septoplasty: an analysis of 50 cases. Int J Otorhinolaryngol Head Neck Surg 3(4):1046–1051
Bayraktar C, Doğan S (2016) The effectiveness of final intraoperative endoscopic control in conventional septoplasty. Eur Res J 2(3):177–181
Garzaro M, Dell’Era V, Riva G, Raimondo L, Pecorari G, Aluffi VP (2019) Endoscopic versus conventional septoplasty: objective/subjective data on 276 patients. Eur Arch Otorhinolaryngol 276(6):1707–1711
Elbanhawy OA, Khalil YA, Abdelshafy IA, Badr MM (2015) Endoscopic-aided septal surgery. Menoufia Med J 28:935–940
Rajguru R, Singh I, Galagali JR, Singh A (2017) Septoplasty techniques- conventional versus endoscopic: our experience. Int J Otorhinolaryngol Head Neck Surg 3:990–996
Funding
No funding sources.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None declared.
Ethical Clearance
Institutional ethical committee.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix
Appendix


Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ahmed, R., Hiremath, C.S., Khavasi, P. et al. Comparative Study of Surgical Outcome in Endoscopic-Assisted Versus Conventional Septoplasty Using Nasal Surgical Questionnaire (NSQ): A Randomized Control Trial. Indian J Otolaryngol Head Neck Surg 75, 3610–3620 (2023). https://doi.org/10.1007/s12070-023-04029-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04029-0