Abstract
The evolution of expanded endoscopic skull base surgery has enabled development of minimally invasive approaches for resection of large skull base tumors with the nasoseptal flap proving to be an indispensable tool in skull base reconstruction. We here present our experience of sphenoid mucocele development after skull base reconstruction with the nasoseptal flap along with a comprehensive review of the limited literature on the same. With the expanding scope of endoscopic skull base surgery, the nasoseptal flap is increasingly being used for reconstruction. Despite adherence to standard recommendations and use of meticulous technique during flap placement, the potential risk of mucocele formation under the flap should always be borne in mind. In our experience, displacement of the flap pedicle could lead to ostial obstruction and mucocele formation. Hence, in addition to meticulous technique, a close follow up of such patients via nasal endoscopy or imaging is important to further our knowledge and understanding of the long-term effects and complications of this flap.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The evolution of expanded endoscopic skull base surgery has enabled development of minimally invasive approaches for resection of large skull base tumors. The nasoseptal flap has proved to be an indispensable tool in skull base reconstruction. This versatile vascularized pedicled flap significantly reduces the rate of post-operative CSF leaks and thus is the standard of care in repair of skull base defects [1,2,3]. The nasoseptal flap however is associated with the potential risk of development of mucocele in the late post-operative period [4, 5]. Entrapment of mucosa, meatal adhesions, and improper flap placement are a few etiological factors implicated in formation of mucocele after skull base surgeries [6, 7]. Several guidelines have been put forth in an attempt to minimize the development of mucocele under nasoseptal flaps, particularly in the sphenoid sinus. We here present our experience of sphenoid mucocele development after skull base reconstruction with the nasoseptal flap along with a comprehensive review of literature on the same.
Our Experience
A 48 year old male was referred to our institution with CSF leak from the right side that developed after endoscopic sinus surgery that was performed 8 months back for chronic rhinosinusitis with bilateral nasal polyposis. On nasal examination, clear fluid discharge was observed from the right nostril in addition to post-operative changes with mucosal adhesions. CT and MRI imaging of paranasal sinuses demonstrated a skull base defect in the posterior foveal region on the right side.
Endoscopic closure of CSF leak was performed. Polypoidal mucosa in the ethmoidal gallery on the right side was debrided. The frontal sinus was identified and frontal recess widened. The defect was identified in the right posterior fovea just lateral to the attachment of middle turbinate just posterior to the course of anterior ethmoidal artery. A wide sphenoidotomy was performed by drilling the neo-osteogenic bone surrounding the sphenoid ostium.
The pseudoencephalocele was identified and bipolarized (Fig. 1). All margins of the defect were delineated. The remnant middle turbinate was excised. Mucosa was removed from the anterior fovea, posterior fovea and sphenoid sinus. Mucosa near the margins and middle turbinate was removed using coblation. The dura was raised from superior surface of the bone to create space for underlay. The defect was approximately 2 cm × 1.5 cm in size. Tensor fascia lata was used for underlay and nasoseptal flap was placed (Fig. 2). The flap was then coated with a layer of fibrin sealant (Tisseel; Baxter Healthcare corporation, Deerfield, IL) and supported by several pieces of absorbable gelatin sponge and merocele nasal tampon (Medtronic Xomed, Jacksonville, FL).
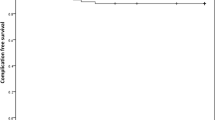
Patient had an unremarkable post-operative course and subsequent postoperative follow up showed adequate mucosalization as observed by nasal endoscopy. Five months post operatively patient developed complaints of headache and sensation of heaviness despite healthy appearing nasal endoscopy with the septal flap adherent to the sphenoid wall and skull base. An MRI imaging revealed a well-defined T1/T2 hyperintense cystic lesion of size 35 × 27 mm in the sphenoid sinus suggestive of sphenoid mucocele (Fig. 3).
Patient was planned for endoscopic trans-nasal exploration and marsuplization of mucocele. Intraoperatively, occlusion of the right sphenoid sinus ostium was observed by the displaced pedicle of the nasoseptal flap along with neo-osteogenesis in left sphenoid ostium as a sequela of Functional Endoscopic Sinus Surgery (FESS) (Fig. 4). The mucosa over the anterior wall of the sphenoid was debrided and mucocele was marsupialized. Erosion of the sella causing exposure of the dura was noted (Fig. 5). The patient was asymptomatic and endoscopic examination showed complete healing of the mucosa inside the sphenoid sinus for a period of 7 months.
Discussion and Critical Review
Mucocele is defined as benign cystic collection of mucus within paranasal sinuses with bony destruction caused by distension. The frontal and ethmoidal sinuses are more commonly involved. Mucocele of the sphenoid sinus is observed in 1–8% of cases [8,9,10]. Diverse theories have been proposed to elucidate the mechanism of mucocele formation. Etiological factors implicated include chronic rhinosinusitis, cystic degeneration of nasal polyps and inflammatory obstruction of mucous drainage. Mucoceles may also arise secondary to entrapment of mucosa after trauma, surgery (e.g. trans-sphenoidal hypophysectomy) or due to obstruction sinus outflow caused by fibrosis or adhesions in the post-operative period [6, 7, 9, 11,12,13]. Radiotherapy to the head and neck is associated with development of sphenoid sinus mucocele as a late complication caused by scarring and stenosis of the ostium [14]. Lund et al. [15] suggested that release of proinflammatory cytokines from the mucocele wall leads to osteoclastic bone resorption and destruction of adjacent tissue [15, 16].
In the past, mucocele formation after skull base surgery was reported predominantly in pediatric age group and with use of free mucosal grafts from middle or inferior turbinate for defect reconstruction [17]. This was attributed to incomplete removal of frontal sinus mucosa and obstruction of the frontonasal outflow particularly in anterior defects. Intracranial mucocele formation caused by mucosal entrapment and abnormal proliferation of traumatized sequestered mucosa has also been reported with the use of free mucosal patch grafts [6, 7]. Post-operative mucocele formation after trans-sphenoidal pituitary surgery has been reported in a number of cases, wherein mucosal scarring, stenosis or synechiae formation lead to obstruction of the sphenoid sinus ostium [18,19,20].
The Hadad–Bassagasteguy flap, a pedicled vascular flap has, since its description in 2006, become the workhorse in reconstruction of large skull base defects [2, 21,22,23,24,25,26,27,28,29,30,31]. Although the harvest and inset of this flap is relatively safe, it carries a potential risk of mucocele formation that may be caused by inadvertent mucosal overlap, mucosal entrapping, and sinus ostium obstruction. In view of this, extirpation of sphenoid sinus mucosa prior to flap placement was recommended by the originators of the flap [21].
The first report of mucocele formation with the use of nasoseptal flap for skull base reconstruction was published by Bleier et al. [4] in 2011. The study reviewed 28 cases that used unilateral or bilateral nasoseptal flaps for skull base reconstruction with mucosal denudation being performed solely around the defect site. They reported a 3.6% (1 case) mucocele rate. This was attributed to the inadvertent flap inset over a concavity with circumferential injury that led to complete obstruction of the lateral sellar recess. Partial mucosal denudation solely at cranial base defect was carried out in an attempt to avoid adjacent neurovascular injury, prolonged post- operative crusting, and increased scarring.
Conversely, Vaezeafshar et al. [5] reported a sphenoid mucocele 4 months after repair of a skull base defect using nasoseptal flap. The complication developed despite extirpation of mucosa over the sphenoid sinus and clival recess prior to flap placement. Demucosalization of the area of skull base along the course of the pedicle in addition to mucosal stripping at the primary defect site is advocated by some authors. This prevents trapping of mucosa under the course of the nasoseptal flap and helps achieve a 0% mucocele rate as demonstrated by Husain et al. [32]. No mucocele formation was observed by Nyquist et al. [33] in their review of five patients who underwent skull base reconstruction using bilateral nasoseptal flaps. They advocated complete removal of sphenoid sinus mucosa, a wide lateral sphenoidotomy to help the flap adhere to the bony walls of the sphenoid and meticulous technique to avoid overlap of the flaps in case of bilateral flap reconstruction. A 2% risk of postoperative mucocele formation reported by McCoul et al. [34] was ascribed to incomplete removal of sphenoid sinus mucosa with persistent secretion of mucus beneath the flap.
A retrospective analysis by Soudry et al. [35] on the use of nasoseptal flap, demonstrated only a single case of sphenoid mucocele (0.8%). Additional steps undertaken by the authors during flap inset included removal of bony septations in the vicinity of the defect and circumferential stripping of mucosa around the defect to aid direct contact of the flap with bone. Care was taken to prevent torsion of the pedicle and flap misorientation. Dolci et al. [36] reported 0% mucocele rate in a mean follow-up period of 12.2 months and strongly encouraged a complete removal of all mucosa and bony septae within sphenoid sinus along with mucosal denudation at the defect site prior to flap inset. Furthermore, creating a wide sphenoidotomy was also recommended to avoid obstruction of ventilation. A systematic review on complications of nasoseptal flap reconstruction by Lavigne et al. [37] concluded that mucocele formation in the sphenoid sinus does not appear to be a complication of the neoseptal flap; rather it arises from incomplete removal of sinus mucosa on the recipient bed.
Clinical presentation of sphenoid mucocele may be variable with headache being the most common symptom [38, 39]. Progressive enlargement with osteoclastic bone resorption leads to erosion of the walls of the sphenoid, causing compression of adjacent neurovascular structures. The compression of optic nerve, III, IV, VI cranial nerves lying within the cavernous sinus can result in visual disturbance or III, IV, VI cranial nerve palsies [39,40,41]. Endocrine disorders and hypopituitarism have also been reported in association with sphenoid mucoceles [42].
Surgery is considered the mainstay of treatment of sphenoid mucocele [43]. Endoscopic trans-nasal sphenoidotomy with wide removal of anterior and inferior sphenoid wall is considered the gold standard approach, offering excellent visualization of the sphenoid sinus intra-operatively and facilitates adequate drainage in the post-operative period thus minimizing recurrence [44,45,46].
Our patient presented with an iatrogenic posterior foveal defect with CSF rhinorrhoea on the right-side following FESS performed for the management of chronic sinusitis with nasal polyposis. Nasoseptal flap was harvested on the right side and employed for reconstruction of the skull base defect. A wide sphenoidotomy was performed on the right and sinus mucosa stripped. The sphenoid ostium on the left though narrow, appeared to be patent and hence was not manipulated with.
The formation of sphenoid mucocele 5 months post operatively in this patient could be attributed to displacement of the nasoseptal flap pedicle causing occlusion of the right sphenoid ostium and neo-osteogenesis causing obstruction of the sinus drainage on the left side.
A recent study by Benkhatar et al. [47] also observed an increased risk of post-operative mucocele in patients with a high preoperative Lund-Mackay score (> 19). Thus, post-operative ostial narrowing leading to mucocele formation may occur in patients showing a strong tendency to cicatrization, adhesions and bone hyperplasia [39]. These finer aspects need to be considered during surgical planning and undertaking appropriate steps prior to reconstruction of skull base defects will help avoid complications.
This comprehensive review of the existing literature on mucocele formation after nasoseptal flap reconstruction of skull base defects helps establish that despite meticulous technique the possibility of mucocele formation in late post-operative period cannot be overlooked. However, prevention is facilitated by judicious removal of mucosa around the defect site and complete removal of mucosa from the sphenoid sinus to ensure adherence of the flap to the bone. A bilateral wide sphenoidotomy that aids in maintaining adequate sinus ventilation is advisable especially in patients with history of prior FESS surgery or those undergoing revision surgery with postoperative adhesions or fibrotic changes. Furthermore, as observed in this case report, displacement of the flap pedicle is another potential hazard that can result in sphenoid sinus ostium obstruction and development of post-operative mucocele. Hence, it is essential to also create a predetermined path for the pedicel of the nasoseptal flap that does not obstruct any sinus ostia along its course.
Further, larger studies elucidating the extent of mucosal denudation to be performed along the skull base and pedicle are necessary as mucosal preservation during flap inset avoids extensive tissue scarring and as shown by Bleier et al is associated with only a 3.6% risk of mucocele formation [4].
Conclusion
With substantial advancements ensuing in the field of skull base surgery, the nasoseptal flap has become an invaluable tool to surgeons faced with the arduous task of repairing large skull base defects with minimal failure rates. Adherence to standard recommendations and use of meticulous technique during flap placement, avoiding ostial obstruction along its course is imperative in reducing post-operative complications. However, the potential risk of mucocele formation under the flap despite surgical proficiency should always be borne in mind. Hence a close follow up of patients undergoing skull base reconstruction via nasal endoscopy or imaging is advisable.
References
Zanation AM, Carrau RL, Snyderman CH et al (2009) Nasoseptal flap reconstruction of high flow intraoperative cerebral spinal fluid leaks during endoscopic skull base surgery. Am J Rhinol Allergy 23:518–521
Shah RN, Surowitz JB, Patel MR et al (2009) Endoscopic pedicled nasoseptal flap reconstruction for pediatric skull base defects. Laryngoscope 119:1067–1075
Caicedo-Granados E, Carrau R, Snyderman CH et al (2010) Reverse rotation flap for reconstruction of donor site after vascular pedicled nasoseptal flap in skull base surgery. Laryngoscope 120:1550
Bleier BS, Wang EW, Vandergrift WA II, Schlosser RJ (2011) Mucocele rate after endoscopic skull base reconstruction using vascularized pedicled flaps. Am J Rhinol Allergy 25:186–187
Vaezeafshar R, Hwang PH, Harsh G, Turner JH (2012) Mucocele formation under pedicled nasoseptal flap. Am J Otolaryngol 33:634–636
Eloy JA, Fatterpekar GM, Bederson JB, Shohet MR (2007) Intracranial mucocele: an unusual complication of cerebrospinal fluid leakage repair with middle turbinate mucosal graft. Otolaryngol Head Neck Surg 137:350–352
Wang L, Kim J, Heilman CB (1999) Intracranial mucocele as a complication of endoscopic repair of cerebrospinal fluid rhinorrhea: case report. Neurosurgery 45:1243–1245
Kosling S, Hinter M, Brandt S, Schulz T, Bloching M (2004) Mucoceles of the sphenoid sinus. Eur J Radiol 51:1–5
Hantzakos AG, Dowley AL, Yung MW (2003) Sphenoid sinus mucocele: late complication of sphenoidotomy. J Laryngol Otol 117:561–563
Delfini R, Missori P, Iannetti G, Ciappetta P, Cantore G (1993) Mucoceles of the paranasal sinuses with intracranial and intraorbital extension: report of 28 cases. Neurosurgery 32:901–906
Kim YS, Kim K, Lee JG et al (2011) Paranasal sinus mucoceles with ophthalmologic manifestations: a 17-year review of 96 cases. Am J Rhinol Allergy 25:272–275
Daniilidis J, Nikolaou A, Kondopoulos V (1993) An unusual case of sphenoid sinus mucocele with severe intracranial extension. Rhinology 31:135–137
Rombaux P, Bertrand B, Eloy P et al (2000) Endoscopic endonasal surgery for paranasal sinus mucoceles. Acta Otorhinolaryngol Belg 54:115–122
Rejab E, Said H, Saim L, Thim L (1991) Sphenoid sinus mucocele: a possible late com- plication of radiotherapy to the head and neck. J Laryngol Otol 105:959–960
Lund VJ, Henderson B, Song Y (1993) Involvement of cytokines and vascular adhesion receptors in the pathology of fronto-ethmoidal mucocoeles. Acta Otolaryngol 113:540–546
Herman P, Lot G, Guichard JP et al (1998) Mucocele of the sphenoid sinus: a late complication of transsphenoidal pituitary surgery. Ann Otol Rhinol Laryngol 107:765–768
Di Rocco F, Couloigner V, Dastoli P et al (2010) Treatment of anterior skull base defects by a transnasal endoscopic approach in children. J Neurosurg Pediatr 6:459–463
Giordano M, Gerganov VM, Draf W et al (2012) Sphenoid sinus pyocele after transsphenoidal approach for pituitary adenoma. Pituitary 15:188–192
Lu YJ, Chang CN, Pai PC et al (2009) Isolated sphenoid sinusitis or mucocele: a potential complication of endonasal transsphenoidal surgery. J Neurooncol 91:63–67
Kessler L, Legaludec V, Dietemann JL et al (1999) Sphenoidal sinus mucocele after transsphenoidal surgery for acromegaly. Neurosurg Rev 22:222–225
Hadad G, Bassagasteguy L, Carrau RL et al (2006) A novel reconstructive technique after endoscopic expanded endonasal approaches: vascular pedicle nasoseptal flap. Laryngoscope 116:1882–1886
Eloy JA, Kalyoussef E, Choudhry OJ et al (2012) Salvage endoscopic nasoseptal flap repair of persistent cerebrospinal fluid leak after open skull base surgery. Am J Otolaryngol 33:735–740
Eloy JA, Patel SK, Shukla PA et al (2013) Triple-layer reconstruction technique for large cribriform defects after endoscopic endonasal resection of anterior skull base tumors. Int Forum Allergy Rhinol 3:204–211
Kassam AB, Thomas A, Carrau RL et al (2008) Endoscopic reconstruction of the cranial base using a pedicled nasoseptal flap. Neurosurgery 63:ONS44–ONS52
Snyderman CH, Kassam AB, Carrau R, Mintz A (2007) Endoscopic reconstruction of cranial base defects following endonasal skull base surgery. Skull Base 17:73–78
Liu JK, Schmidt RF, Choudhry OJ et al (2012) Surgical nuances for nasoseptal flap reconstruction of cranial base defects with high-flow cerebrospinal fluid leaks after endoscopic skull base surgery. Neurosurg Focus 32:E7
Schmidt RF, Choudhry OJ, Raviv J et al (2012) Surgical nuances for the endoscopic endonasal transpterygoid approach to lateral sphenoid sinus encephaloceles. Neurosurg Focus 32:E5
Eloy JA, Choudhry OJ, Friedel ME et al (2012) Endoscopic nasoseptal flap repair of skull base defects: is addition of a dural sealant necessary? Otolaryngol Head Neck Surg 147:161–166
Eloy JA, Choudhry OJ, Shukla PA et al (2012) Nasoseptal flap repair after endoscopic transsellar versus expanded endonasal approaches: is there an increased risk of postoperative cerebrospinal fluid leak? Laryngoscope 122:1219–1225
Eloy JA, Kuperan AB, Choudhry OJ et al (2012) Efficacy of the pedicled nasoseptal flap without cerebrospinal fluid (CSF) diversion for repair of skull base defects: incidence of postoperative CSF leaks. Int Forum Allergy Rhinol 2:397–401
Eloy JA, Choudhry OJ, Christiano LD et al (2013) Double flap technique for reconstruction of anterior skull base defects after craniofacial tumor resection: technical note. Int Forum Allergy Rhinol 3(5):425–430. https://doi.org/10.1002/alr.21092
Husain Q, Sanghvi S, Kovalerchik O, Shukla PA, Choudhry OJ, Liu JK et al (2013) Assessment of mucocele formation after endoscopic nasoseptal flap reconstruction of skull base defects. Allergy Rhinol 4:e27–e31
Nyquist GG, Anand VK, Singh A, Schwartz TH (2010) Janus flap: bilateral nasoseptal flaps for anterior skull base reconstruction. Otolaryngol Head Neck Surg 142:327–331
McCoul ED, Anand VK, Singh A, Nyquist GG, Schaberg MR, Schwartz TH (2014) Long-term effectiveness of a reconstructive protocol using the nasoseptal flap after endoscopic skull base surgery. World Neurosurg 81(1):136–143. https://doi.org/10.1016/j.wneu.2012.08.011
Soudry E, Psaltis AJ, Lee KH, Vaezafshar R, Nayak JV, Hwang PH (2015) Complications associated with the pedicled nasoseptal flap for skull base reconstruction. Laryngoscope 125(01):80–85
Dolci RL, Miyake MM, Tateno DA, Cancado NA, Campos CA, Santos AR et al (2017) Postoperative otorhinolaryngologic complications in transnasal endoscopic surgery to access the skull base. Braz J Otorhinolaryngol 83:349–355
Lavigne P, Faden LD, Wang E, Snyderman HC (2018) Complications of nasoseptal flap reconstruction: a systematic review. J Neurol Surg Part B Skull Base 79:S291–S299. https://doi.org/10.1055/s-0038-1668158
Friedman A, Batra PS, Fakhri S et al (2005) Isolated sphenoid sinus disease: etiology and management. Otolaryngol Head Neck Surg 133(544–50):2
Moriyama H, Hesaka H, Tachibana T et al (1992) Mucoceles of ethmoid and sphenoid sinus with visual disturbance. Arch Otolaryngol Head Neck Surg 118:142–146
Lee LA, Huang CC, Lee TJ (2004) Prolonged visual disturbance secondary to isolated sphenoid sinus disease. Laryngoscope 114:9
Sethi DS, Lau DP, Chan C (1997) Sphenoid sinus mucocoele presenting with isolated oculomotor nerve palsy. J Laryngol Otol 111:471–473
Hejazi N, Witzmann A, Hassler W (2001) Occular manifestations of sphenoid mucoceles: clinical features and neurosurgical management of three cases and a review of the literature. Surg Neurol 56:338–343
Kennedy DW, Josephson JS, Zinreich SJ et al (1989) Endoscopic sinus surgery for mucoceles: a viable alternative. Laryngoscope 99:885–895
Giovannetti F, Filiaci F, Ramieri V et al (2008) Isolated sphenoid sinus mucocele, etiology and management. J Craniofac Surg 19:1381–1384
Har-El G (2001) Endoscopic management of 108 sinus mucoceles. Laryngoscope 111:2131–2134
Lund VJ (1998) Endoscopic management of paranasal sinus mucoceles. J Laryngol Otol 112:36–40
Benkhatar H, Khettab I, Sultanik P, Laccourreye O, Bonfils P (2018) Mucocele development after endoscopic sinus surgery for nasal polyposis: a long-term analysis. Ear Nose Throat J 97(9):284–294
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Janakiram, T.N., Karunasagar, A. Sphenoid Mucocele: A Complication of Skull Base Reconstruction with Nasoseptal Flap—A Critical Review and Our Experience. Indian J Otolaryngol Head Neck Surg 71 (Suppl 3), 2151–2156 (2019). https://doi.org/10.1007/s12070-019-01713-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-019-01713-y