Abstract
Osteosarcoma is a mesenchymal malignant tumour of long bones; it is the second most common malignancy of bone after multiple myeloma but it rarely affects jaw, accounting only for 4–8% of all osteosarcomas (Baumhoer et al. in Oral Oncol 50(2):147–153, 2014). The rare occurrence of tumour makes it challenging to diagnose either by radiographic or histopathologic examination. Here we presented a rare case of chondroblastic variant of osteosarcoma of body of mandible in a 54 year old female.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteosarcoma (OS) is a mesenchymal malignant tumour of long bones, it is the second most common malignancy of bone after multiple myeloma but it rarely affect jaw bones accounting only for 4–8% of all osteosarcomas [1]. In mandible, the posterior ramus is common site while in the maxilla, alveolar ridge, palate and sinus areas are the sites of occurrence [2]. Pattern of expression in osteosarcoma of long bones is much different than in the jaw bones, presenting usually in older population. The different sites of OS in maxillo-mandibular region results in difficulty of resection and reconstruction compared to the long bones. We presented a rare case of jaw bone tumour with its unusual occurrence in the region of body of mandible showing its utter demonstration both by radiology and histology at an early stage of the disease which in itself is an inimitable coincidence as percentage of false negative results is much higher on incisional biopsy of these lesions.
Case Report
A 54 year old female presented to the department of oral and maxillofacial surgery with the chief complaint of swelling over the left side of the lower jaw since one and half month. Patient was asymptomatic 2 months before, then she started experiencing pain and swelling in the same region, for which she underwent extraction of tooth in that region at a private dental clinic. After extraction of tooth, the swelling progressively increased in size but without any pain. On extra-oral palpation swelling was hard and non tender measuring 3 × 3 cm. There was no pain or paresthesia. Submandibular lymph nodes were palpable and tender; one in number and firm in consistency. On intraoral examination, overlying mucosa was slightly oedematous and inflamed with central ulcerations extending from distal aspect of 1st premolar to mesial aspect of 1st molar (Fig. 1). On palpation lingual cortical plate expansion was also noted. Differential diagnosis included, fibrous dysplasia, osteosarcoma and carcinoma.
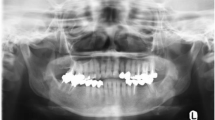
An orthopantomogram (OPG) showed radiopaque mass measuring about 3x3 cm in left body of mandible showing classical sun burst appearance (Fig. 2). 3D MDCT scan showed large bony mass lesion involving left body of the mandible measuring 41.8 mm × 25.4 mm with osteoid bone matrix and adjacent periosteal reaction (Fig. 3). Axial view CT scan confirmed the clinical finding of lingual cortical expansion (Fig. 4). Clinical and radiographic features were strongly suggestive of osteosarcoma of body of mandible. Routine haematological investigations were done. An open biopsy was performed with direct incision over the bone in the representative region; adequate size of bone tissue was removed using straight hand piece and copious saline irrigation. Continuous oozing was observed from the lesion obscuring the field. Incisional biopsy was also obtained from overlying soft tissues. Haemostasis was achieved by using local haemostatic measures. Samples were sent for histopathological examination which on H and E stained section showed osteoid material with atypical osteocytes, at focal areas chondroblastic tissues with atypical cells were evident while few sections showed cellular areas blending into malignant osteoid tissues confirming the diagnosis of OS of body of mandible (Fig. 5). The soft tissue biopsy was inconclusive. Patient was then referred to oncology department for further management. There she underwent hemi-mandibulectomy with disarticulation followed by free fibula microvascular reconstruction and followed by adjuvant chemotherapy. Final diagnosis of osteosarcoma of body of mandible with a skip metastastatic lesion in mandibular condyle was confirmed from histopathology reports.
Discussion
Osteosarcoma is the most common malignant bone tumour with rare occurrence in jaw bones accounting for 4–8 percent [1]. It constitutes 20% of all sarcomas and only 5% of all osteogenic sarcomas occurring in head and neck region. The rare occurrence of tumour makes it challenging to diagnose either by radiographic or histopathologic examination. History of fibrous dysplasia, paget’s disease, previous irradiation in head and neck region, osteomyelitis, trauma and osteochondromatosis are considered to be risk factors for OS [3]. There was no such history of bony pathology in our case, hence the etiology was obscure. OS has slightly high predilection for males compared to females with the ratio of 1.4:1 and it is usually seen in third to fourth decades of life [4] and ramus of mandible is most common site of occurrence. We have proffered a sixth decade female patient with OS in the body of mandible which is supremely rare. Swelling is the most common presenting feature of osteosarcoma where as pain, paresthesia and ulcerations remains tangential [5]. It is deceitful to come to the provisional diagnosis of osteosarcoma based on the clinical findings.
Radiological feature is of utmost importance as it acts as guide for the pathologist to correlate with clinic-pathological findings. Radiographic attributes include widening of periodontal ligament space along with the enfeeblement of lamina dura around a jaw tumour [6, 7]. However our patient had previous history of extraction of tooth in the same region, so the latter finding was truant. Radiographic appearance is based on the histological changes present in particular stage of osteosarcoma. It may display either bone formation (osteogenic), bone destruction (osteolytic) or a combination of both. Our patient’s OPG showed diffuse radiopacity in left body of mandible similar to that of classic “sun burst” appearance of osteosarcoma indicating malignant changes in the process of osteoid formation. Though OPG acts as a chaperon in the differential diagnosis, it has its own pitfalls such as image distortion and magnification. CT scan or MRI scan can be used as an advanced diagnostic tool to conclude on a more definitive diagnosis. The CT scan of our patient clearly delineated periosteal reaction with bony expansile lesion and osteoid bone matrix showing strong proclivity towards OS.
Altuwairagi et al. [8] stated that the chances of false negative biopsy in cases of OS varied from 17 to 25% which made the diagnosis and management challenging associated with precarious radiological features. However in this report we have presented OS both by histology and radiology without any uncertainty which makes this case interesting and unique in terms of coincidence of early presentation of patient and surgeon’s ability to identify the representative area from the bony lesion at the time of incisional biopsy. Histologically OS can be classified into 3 variants i.e. osteoblastic, chondroblastic and fibroblastic depending upon type of cellular component present. Daffner et al. classified presentation of OS into either multicentric (1–2%) or skip metastatic lesion (10%). Multicentric lesions can present as a synchronous lesion or a metachronous lesion. We had a chondroblastic variant with a skip lesion in the region of mandibular condyle [10]. The American Joint Committee Classification system is based on the histologic grade, tumor size and presence of metastases. Table 1 summarises AJCC classification system [11].
Radical surgical excision is the preferred management in OS with more than 5 year of overall survival. Role of chemotherapy in OS remains insignificant mainly in jaw bone tumour. Table 2 summarises various treatment protocol for OS. Rosen’s protocol in the management of OS involves use of chemotherapy followed by surgery and again use of chemotherapy [12]. One limitation for advocating Rosen’s protocol which is also known as sandwich technique is limitations regarding accurate diagnosis of this condition [11]. Metastasis in OS occurs approximately 2 years after diagnosis [9]. Our case was treated by combination approach in which surgical excision was performed followed by adjuvant chemotherapy as it had a skip lesion in the condyle. Marx et al. [13] suggested that treatment failures in case of OS are due to local recurrence followed by distant metastasis in lung, brain and Skeleton.
Conclusion
Unique muddle in osteosarcoma is its diagnosis and management. As the incidence of OS of mandible is very low, this report desires to pivot on two foremost purposes; firstly the early presentation of the patient to the surgeon irrespective of any swelling in maxillo-mandibular region and the ingenuity of surgeon while performing bone biopsy followed by radical excision of tumour after confirmed diagnosis.
References
Baumhoer D, Brunner P, Eppenberger-Castori S, Smida J, Nathrath M, Jundt G (2014) Osteosarcomas of the jaws differ from their peripheral counterparts and require a distinct treatment approach. Experiences from the DOESAK Registry. Oral Oncol 50(2):147–153
Bojan A, Christy W, Chanmougananda S, Ashokan K (2012) Osteosarcoma of mandible: a case report and review of literature. J Clin Diagn Res 6:753–757
Khorate MM, Goel S, Singh MP, Ahmed J (2010) Osteosarcoma of the mandible: a case report and review of the literature. J Cancer Sci Ther 2:122–125
Wang S, Shi H, Yu Q (2012) Osteosarcoma of the jaws: demographic and CT imaging features. Dentomaxillofac Radiol 41:37–42
Jasnau S, Meyer U, Potratz J, Jundt G, Kevric M, Joos UK et al (2008) Cooperative Osteosarcoma Study Group COSS: craniofacial osteosarcoma. Experience of the cooperative German-Austrian-Swiss osteosarcoma study group. Oral Oncol 44(3):286–294
Ogunlewe MO, Ajayi OF, Adeyemo WL, Ladeinde AL, James O (2006) Osteogenic sarcoma of the jaw bones: a single institutional experience over a 21-year period. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 101(1):76–81
Nakayama E, Sugiura K, Ishibashi H, Oobu K, Kobayashi I, Yoshiura K (2005) The clinical and diagnostic imaging findings of osteosarcoma of the jaw. Dentomaxillofac Radiol 34(3):182–188
Altuwairgi O, Papageorge MB, Karp DD (1996) Maxillary chondroblastic sarcoma: presentation of two cases and a literature review. J Oral Maxillofac Surg 54(11):1357–1364
Daffner RH, Fox KR, Galey K (2002) Fibroblastic osteosarcoma of the mandible. Skeletal Radiol 31:107–111
Thiele OC, Freier K, Bacon C, Egerer G, Hofele CM (2008) Interdisciplinary combined treatment of craniofacial osteosarcoma with neoadjuvant and adjuvant chemotherapy and excision of the tumour: a retrospective study. Br J Oral Maxillofac Surg 46:533–536
Amin MB, Edge S, Greene F, Byrd DR, Brookland RK et al (eds) (2016) AJCC cancer staging manual, 8th edn. Springer, New York
Rosen G, Caparros B, Huvos AG, Kosloff C, Nirenberg A, Cacavio A et al (1982) Preoperative chemotherapy for osteogenic sarcoma: selection of postoperative adjuvant chemotherapy based on the response of the primary tumor to preoperative chemotherapy. Cancer 49(6):1221–1230
Marx RE, Stern D (2012) Oral and maxillofacial pathology a rationale for diagnosis and treatment. Quintessence Pub. Co., Hanover Park
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Authors declare no conflict of interest.
Ethical Approval
This paper was exempted from ethical approval.
Informed Consent
Written informed consent was on obtained from patient.
Rights and permissions
About this article
Cite this article
Wagh, A., Kokane, G., Jendi, S. et al. Early Diagnosis: A Seeming Misfortune for Osteosarcoma of Mandible—Rare Case Report. Indian J Otolaryngol Head Neck Surg 71 (Suppl 1), 748–751 (2019). https://doi.org/10.1007/s12070-018-1534-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-018-1534-x