Abstract
Retrospective study of the prelingual cochlear implantation programme under government scheme done at medical college hospital in central India. Forty-two prelingually deaf children screened and sent for cochlear implantation at our centre From March 2015 to Feb 2018 were reviewed with respect to their age, sex, preimplantation hearing aid use, surgical technique for cochlear implantation, type of FDA (USA) approved cochlear implant, post operative speech therapy and its outcome with respect to categories of auditory perception and speech intelligibility scoring were compared for children younger than 4 years and older than 4 years. For outcome measurement non parametric statistical method was used for any significance between the two groups. There was a wide range of children implanted ranging from 2 to 7 years. Both varia and mastoidectomy and posterior tympanotomy method of cochlear implantations were done with good rate complete insertion and electrode activation. There was no significant difference between the two group with regard to CAP and SIR outcomes after 1 year. In order to get better outcomes with respect to the speech language development, there is need to strengthen the early identification and cochlear implantation before 4 years of age in government approved schemes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multi channel cochlear implant was approved for marketing for children in the year 1990 by the FDA [1]. Since 2000 after FDA’S approval many children above 12 months have been implanted. In India, cochlear implant is done as a measure to treat deaf children screened under the national programme for prevention and control deafness and is implemented by many medical centres. Prelingually deaf children have got neural plasticity to develop auditory verbal communication [2]. Neuroplasticity is ability of the brain to adapt in response to incoming sensory input in early life and in part this is due to major increase in synaptogenesis [3]. Hence it is ideal to implant the prelingually deaf is within 3–4 years of age [4]. Also in our country there is considerable delay in diagnosis of deafness after birth and hence most of prelingually deaf children are older than 4 years of age. However, cochlear implant can be done at any age with some auditory benefit with questionable communication language development [4]. Here we are reviewing 42 prelingually deaf children implanted with FDA (USA) approved implants for its benefits with respect to this critical age for implantation. Auditory verbal therapy and monitoring with categories of auditory perception(CAP) scores for receptive language and speech lintelligebility rating for (SIR) strategies have been thought to be good for the prelingually deaf children [5].
Materials and Methods
We retrospectively reviewed the 42 prelingually deaf children approved for cochlear implant under state government cochlear implant programme from March 2015 to February 2018. There were 28 male and 14 female children. The age of the children varied from 2 to 7 years. We divide the group into two groups with group A with children of 4 years and less than 4 years and group B with children of more than 4 years of age. In both groups all the screened children were profoundly deaf. This was diagnosed by ABR and ASSR preoperatively and all children were given sufficient amount of hearing aid trial with no benefit before deciding for the cochlear implantation.
All children under went thorough paediatric and psychological evaluation for the growth and development physically and mentally and screened for any associated co-morbities and handicaps.
All children received meningococcal and pneumococcal vaccination well in advance before cochlear implant as per centre for disease control (CDC) and prevention updated guidelines. Thorough ENT examination was done to rule out any co morbidities of upper respiratory tract. High resolution temporal bone CT scan and MRI was studied before surgical procedure for anticipating any abnormalities with regard to development of cochlea turns, abnormal cochlear aqueduct, rotation of cochlear axis with regard to parasaggital plane, vestibular aqueduct, internal auditory meatus and cochlear nerve. Parent counselling with regard to the realistic expectations from the cochlear implant and also for regular follow up for speech therapy following operation was done by the resident audiologist and speech therapist of our centre.
A written informed consent of the parents of the children were taken before surgical procedure after thorough counselling once again. 20 of the children were operated with varia technique and 22 of the children were operated with post auricular incision and posterior tympanotomy approach. 30 children received cochlear nuceus device CI24RE (straight) with CP802 processor and 12 children received advanced bionics HR 90K Advantage HiFocus 1J device with Naida CI Q 30 processor. All the implants were inserted into the cochlea using cochleostomy approach. Intra operative impedance and neural response telemetry and neural response imaging was done and check X-ray was taken to reassure the position of the implant. All the patients withstood the procedure well and discharged after 5 days, stitch removal was done on 10th post operative day and implants were switched on 4th post operative week.
Postoperatively, all the patients received speech therapy regularly. Children were called for AVT twice in a week for 12 months at our centre. And they were assessed using 7 categories of auditory perception (CAP) protocol at 12 months for the sound perception and speech intelligibility rating scale (SIR) for measuring the intelligibility of speech and the quality, which might be recognisable by the listener.
Results
Youngest child to be implanted 2 year. Oldest child to be implanted 7 years. None of the patients had residual hearing. One patient had hydrocephalus and cardiac anomaly which were treated first before cochlear implant. One patient had rotated cochlea. Two patients had enlarged cochlear aqueduct All the patients had impedance within normal range upon insertion in the cochlea. Number of active electrodes at the time of insertion was 922 (99.35%) and at the time switch on it was 926 (99.78%). The stimulation strategies for cochlear device was ACE Stimulation strategy for the advanced bionics was HiRes Optima S.
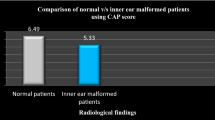
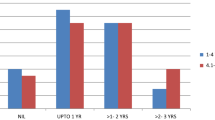
Both CAP and SIR scores for both groups are as shown in the table. After 1 year mean cap score was above 4 for both group A and group B (Table 1) and SIR were above 3 for both groups (Table 2). Both scores were compared with respect to significant difference using Mann–Whitney rank sum test as shown in the graph. There was no statistical significance between both groups with respect to CAP score and the SIR rating (Figs. 1, 2).
Discussion
Cochlear implant is being done in prelingually deaf children since 1990 [1]. Earlier the age of the implant better the verbal language development. The ideal age for cochlear implant before 3rd or 4th year after birth so that spoken language development is within 1 year of chronological age of the child [6]. The main advantage of the early implant is the neural plasticity. In our series, we had youngest being 2 years and oldest to be implanted is 7 years with many children over 3 years of age.
Important investigations before cochlear implant surgery are CT scan for detecting any bony anomalies and MRI to detect any nerve anomaly and soft tissue within cochlea. Important with regard to surgery are the abnormal cochlear aqueduct which is in continuity with the scala tympani and pose as gusher during surgery and the vestibular aqueduct which is in continuity with the endolymph and may or may not have oozers from cochleostomy [7].
In our series we encountered two cases of enlarged cochlear aqueduct and presented as gushers during surgery and were controlled intraoperatively using additional fascia for closing the cochleostomy and complete electrode insertion was possible.
Rotation of the cochlea is rotation of axis is the cochlear axis rotation either ventrally or dorsally from normal range of towards medial side. It is measured by more obtuse angle formed by the line passing through the basal turn of the cochlea with regard to the parasaggital plane. Ideally it is around 55-degree [8]. In these cases insertion becomes difficult through the cochleostomy due to different orientation of the round window. We encountered one such case and it was managed successfully by changing the insertion vector more along medially and upwards.
Mastoidectomy and posterior technique and alternative non mastoidectomy techniques are used for cochlear implantation with equal complication rates [9]. In our series half of the children underwent cochlear implantation by mastoidectomy and posterior tympanotomy and half of the children underwent cochlear implantation by non mastoidectomy varia technique.
Both cochlear and advanced bionics implant electrodes programmes have in built measurement methods to detect the impedance or the resistance between them and the spiral ganglion cells and immediately tell the validity or difficulty in stimulation before electrodes are stimulated. Higher impedance is attributed to the greater inflammatory tissue between the electrode and spiral ganglion [10]. In order to avoid it cortisol injection and antibiotics are injected. And also in case of return of the normal impedence measurement after some period might be due to air bubbles which have been displaced and now electrode is against least resistance pathway for current stimulation. In our series we found out that those electrodes which were shown to be open circuit with high impedance returned to normal impedance after some period.
Stimulation strategy is basically spectral resolution tool which stimulates the spiral ganglion cells and tries to simulate normal hearing as much as possible. But majority of the technologies have focussed perception of sound in quiet environment. All technologies with this regard focus on the number of channels needed to simulate speech spectrum, number of electrodes needed to simulate these channels and temporal stimulation sequence of these electrodes. Advanced combinational encoder (ACE) strategy is used by nucleus straight implant and Hi Res Optima S is the strategy used by the advanced bionics with virtualisation of channels so that inter channel spaces are also used for spectral resolution [11]. All of these help in detecting threshold current for hearing, comfortable current level for stimulation, known as MAPPING [12, 13].
One of the goals of auditory verbal therapy (AVT) is make a child to acquire a spoken language to develop communication skills sufficiently in order to function independently at normal day do day environments. In our country, there are constraints for accessing these services due to proximity of services, expenses involved, and due to lack of AVT therapist. However, in our centre we have AVT therapy facility for this and also parents are trained sufficiently to teach the child at home environment. It will effectively reduce the gap between the chronological age and age of language development. This auditory language stimulation during critical 2–3 years of life is good for acquisition communication skills through spoken language. Categories of auditory perception (CAP) are reliable and valid tool to continuously assess these children [14, 15]. Here we have used 7 point subjective scales for individual children. At the same time speech intelligibility score is also noted for the development of oral language skills. All the assessments were done by the single AVT specialist. Earlier it has been shown that without speech therapy and only environmental sounds are sufficient for good perception and speech skills children implanted at earlier ages of less than 18 months [16]. But, in children who are implanted after 2 years of age show only 20–30% attainment of normal CAP score [17]. So, in our series there was no difference in attainment of CAP scores between children implanted less than 4 years and more than 4 years. Also, youngest implanted child was also above 2 years. In our series all the patients were from poor socioeconomic background with considerable delay in diagnosis of the deafness before implantation. Hence, the basic screening in general population needs to be strengthened to encourage the early identification and implantation.
SIR grading was also showed considerable improvement with 1 year AVT with mean scores above 3 which is comparable with other studies [18].
References
Clark GM (2015) The multi-channel cochlear implant: multi-disciplinary development of electrical stimulation of the cochlea and the resulting clinical benefit. Hear Res 322:4–13. https://doi.org/10.1016/j.heares.2014.08.002
Sharma A, Campbell J (2011) A sensitive period for cochlear implantation in deaf children. J Maternal Fetal Neonatal Med 24(01):151–153
Huttenlocher PR, Dhabolkar AS (1997) Regional differences in synaptogenesis in human cerebral cortex. J Comp Neurol 387:167–178
Sharma A, Nash AA, Dorman M (2009) Cortical development, plasticity and re- organisation in children with cochlear implant. J Commun Disord 42(4):272–279
Gilmour L (2010) The inter rater reliability of categories of auditory performance- II. University of Southampton, Southampton
Nicholas JG, Geers AE (2007) Will they catch up? The role of age at cochlear implantation in the spoken language development of children with severe profound hearing loss. J Speech Lang Hear Res 50(4):1048–1062
Vassolare TMF, da Fountoura G, Bergonse R et al (2008) Cochlear implant and large vestibular aqueduct syndrome in children. Br J Otorhinolaryngol 74(2):260–264
Mikhail S, Mandour MF et al (2018) Lateral rotation of basal turn of cochlea with its impact on cochlear implant feasibility. Med J Cairo Univ 86(1):383–387
El-Anwar MW, El Assar AS, Foad YA (2016) Non-mastoidectomy cochlear implant: a literature review. Int Arch Otorhinolaryngol 20:180–184
Tykocinkski M, Cohen LT et al (2005) Measurement and analysis of access resistance and polarisation impedance in cochlear implant recipients. Otol Neurootol 26(5):948–956
Charles TM, Choi, Yi-Hsuan L (2012) A review of stimulating strategies for cochlear implants. Cochlear implants research updates. In: Dr. Cila Umat (Ed), ISBN: 978-953-51-0582-4 InTech. http://www.intechopen.com/books/cochlear-implant-research-updates/stimulating-strategies-for-cochlearimplants
Gonzalez RIB, Castillo SC, Lee GR (2017) Fitting parameters for cochlear implant. Bol Med Hosp Infant Mex 74(1):65–69
Raghunandan S, Ravikumar A, Kameshwaran M et al (2015) Electrophysiological correlates of behavioural comfort levels in cochlear implantees: a prospective study. Indian J Otolaryngol Head Neck Surg 67(3):210–222
Archbold S, Lutmann ME, Marshall DH (1995) Categories of auditory performance. Ann Otol Rhinol Laryngol Suppl 166:312–314
Archbold S, Lutmann ME, Nikolopoulos T (1998) Categories of auditory performance: inter user reliabilility. Br J Audiol 32(1):7–12
Zhou H, Chen Z, Shi H et al (2013) Categories of auditory performance and speech intelligibility ratings of early implanted children without speech training. PLoS ONE 8(1):e53852
Govearts PJ et al (2002) Outcomes of cochlear implantation at different ages from 0 to 6 years. Otol Neurootol 23:885–890
Kos M-I, Deriaz M et al (2009) What can be expected from a late cochlear implantation? Int J Pediatr Otorhinolaryngol 73:189–193
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that no conflict of interest.
Rights and permissions
About this article
Cite this article
Kulkarni, V., Raghuwanshi, S., Kumar, A. et al. Cochlear Implant in Prelingually Deaf Children: Our Experience. Indian J Otolaryngol Head Neck Surg 70, 544–548 (2018). https://doi.org/10.1007/s12070-018-1435-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-018-1435-z