Abstract
Lymphoepithelial carcinoma (LEC) of salivary glands is a rare malignant salivary gland tumour and demonstrates genetic and regional distribution. It commonly occurs in major salivary gland especially parotid gland. We report a case of LEC of submandibular gland occurring in a 70 year-old lady.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lymphoepithelial carcinoma (LEC) of salivary glands is a rare malignant salivary gland tumour accounted for 0.4 % of salivary gland tumour [1]. LEC demonstrates regional and racial predisposition and it’s associated with infection of Epstein–Barr virus [2]. Its incidence in Eskimos, Greenlandic Inuit, southern coastal region of China and Japanese were relatively higher than the other population [1]. We report a case of LEC of submandibular gland occurring in a 70 year-old Chinese lady.
Case Report
A 70 year-old Chinese lady presented with right submandibular swelling for 1 month duration. The swelling was painless and not associated with fever or upper respiratory tract infection symptoms. There was no loss of appetite or weight. On examination, patient was well and comfortable. Neck examination showed right submandibular mass measuring 2 cm × 2 cm, firm, non-tender and not inflamed. No other neck masses palpable. Nasopharyngolaryngoscopy examination revealed normal findings. Fine needle aspiration cytology of the mass showed malignant cells, consistent with carcinoma. Contrast enhanced computed tomography showed ill-defined homogenously enhancing lobulated lesion measuring 1.8 × 1.9 × 2.3 cm seen within the right submandibular gland, with attenuation value of 130 HU and absence of calcification or fat component and no evidence of neck nodes enlargement. Patient then underwent right submandibulectomy. Histopathological examination of the right submandibular gland confirmed diagnosis of LEC with clear surgical margin. One year follow up post-operatively patient remain asymptomatic.
Discussion
Malaysia is consisted with multiple ethnicities, mainly Malay, Chinese and Indian ethnic and our country also not included in endemic population of LEC of salivary glands. Its rarity worldwide and in our population, making the diagnosis and management of LEC of salivary glands challenging.
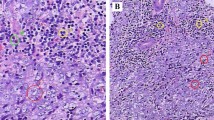
The majority of LEC arise in major salivary glands, with the parotid being most commonly affected (~80 % of cases) [1, 3]. Most cases had unilateral episodes and manifested as slow-growing painless mass which can be associated with facial paralysis, or enlarged cervical lymph node [1]. In this case, patient presented with unilateral submandibular gland enlargement without cervical lymph node involvement, mimicking benign condition. Fine needle aspiration cytology of our patient only showed single lying and sheets of malignant cells exhibiting pleomorphic and vesicular nuclei with prominent large nucleoli in which consistent with carcinoma. Histopathological examination of the submandibular gland post submandibulectomy showed malignant cells rich with lymphoid stroma which is composed of reactive lymphoid cells with lymphoid follicles exhibiting prominent germinal centers (Figs. 1, 2, 3). Typically, histology of LEC consists of differently sized infiltrative-growth neoplastic epithelium and varying amount of lymphoid interstitial.
While clinical presentation may look like a benign lesion, imaging was a useful tool in showing malignant changes of the gland. The preoperative imaging has an important role in surgical planning [1]. A study concluded that typical CT finding of LEC was speculative but it can be decided by the sites of the lesion, morphology and density, pattern of enhancement, margin of nodule, peripheral infiltration and prognosis [1]. Preoperative CT scan was done in this case to look at the nature and extension of the submandibular gland malignancy and to rule out cervical nodes involvement.
In terms of management, it involves submandibulectomy with or without neck dissection or postoperative radiation. Radiotherapy has an adjuvant role following definitive surgery for large tumors, high grade tumors, closed/incomplete excisions, and perineural or vascular invasion [4]. If the accuracy of preoperative or intraoperative grade diagnosis of salivary gland tumour is low, elective neck dissection has been recommended for all the salivary gland cancer patients [4]. For our patient, submandibulectomy was done without neck dissection in view of absence evidence of cervical nodes involvement by clinical examination and CT scan. Adjuvant radiotherapy was not administered to our patient after discussion with the oncology expert in view of her frailty and age with evidence of clear surgical margin histologically. The patient was counseled and advised that a close surveillance and postoperative monitoring will be essential. In conclusion, we have a 70 year-old lady with LEC of submandibular gland treated with submandibulectomy without neck dissection and no adjuvant radiotherapy, who is still alive and no locoregional recurrence after 1 year. Standard management of salivary gland LEC is total excision with adjuvant radiotherapy for better locoregional control [5]. Based on this case, submandibulectomy alone with clear surgical margin can produce a good outcome and should be considered as a method of treatment especially in elderly and frail patient. However, continuation of surveillance monitoring for at least 5 years is still mandatory.
References
Guobin Z, Juan T, Yuping P, Qixin Z, Chungen W (2014) CT features and pathologic characteristics of lymphoepithelial carcinoma of salivary glands. Int J Clin Exp Pathol 7(3):1004–1011
Schneider M, Rizzardi C (2008) Lymphoepithelial carcinoma of the parotid glands and its relationship with benign lymphoepithelial lesions. Arch Pathol Lab Med 132:278–282
Ming Z, Shuang JL, Jinhua F, Hanjiang W, Yijun G (2015) Primary lymphoepithelial carcinoma of the intraoral minor salivary gland: a case report. Oncol Lett 9:790–792
Wang YL, Zhu YX, Chen TZ, Wang Y, Sun GH, Zhang L, Huang CP, Wang ZY, Shen Q, Li DS, Wu Y, Ji HQ (2012) Clinicopathologic study of 1176 salivary gland tumors in a Chinese population: experience of one cancer center 1997–2007. Acta Otolaryngol 132:879–886
Lee CJ, Rayleigh CPY (2007) Lymphoepithelioma-like carcinoma of the submandibular gland: a case report. Tzu Chi Med J 19:40–42
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None of the authors has any conflict of interest, financial or otherwise.
Ethical Approval
This article does not contain any studies with human participants performed by any of the authors.
Rights and permissions
About this article
Cite this article
Sairin, M.E., Yahya, N., Kuan, C.Y. et al. Management of a Rare Lymphoepithelial Carcinoma of the Submandibular Gland in Elderly. Indian J Otolaryngol Head Neck Surg 71 (Suppl 1), 18–20 (2019). https://doi.org/10.1007/s12070-015-0940-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-015-0940-6