Abstract
To investigate the source of serum exosomal HOTAIR, to uncover the diagnostic and prognostic values of serum exosomal HOTAIR, and to discern the expression of serum exosomal HOTAIR between neoadjuvant chemotherapy and response to tamoxifen therapy. Samples were collected from the Third Affiliated Hospital of Kunming Medical University, Tumor Hospital of Yunnan. Exosomes were isolated from serum, cell culture medium and tumor tissues. We used transmission electron microscopy and western immunoblotting assay to characterize exosomes, and real-time PCR (qPCR) to assess HOTAIR expression. Neoadjuvant chemotherapy and tamoxifen therapy were carried out according to established guidelines. Breast cancer patients expressed higher serum exosomal HOTAIR than did healthy individuals (P < 0.001). Serum exosomal HOTAIR levels 3 months after surgery were markedly decreased compared with levels before surgery (P < 0.001), and the expression level of exosomal HOTAIR in cell culture medium increased with time in both breast cancer cell lines (72 h > 48 h > 24 h, 48 h vs 24 h [P < 0.05]; 72 h vs 24 h [P < 0.01]). Expression of serum exosomal HOTAIR in nude mice was notably greater than in the mock control group (P < 0.001). The results of the ROC analysis revealed an AUC for serum exosomal HOTAIR of 0.9178 with a 95% CI of 0.8407–1.017 (P < 0.01). The AUC for the CA15-3 cell line was 0.7378 (95% CI, 0.5585–0.9170; P = 0.03). High expression of exosomal HOTAIR led to a worse disease-free survival (P = 0.0481) and overall survival (P = 0.0463). In the high-expression chemotherapy group, six patients achieved a partial response (PR) and eight demonstrated stable disease (SD) and nine patients achieved PR and two SD in the low-expression group (P = 0.048). In the low-expression tamoxifen group, one patient had a recurrence of breast cancer and another 10 patients exhibited no recurrence, while six showed recurrence, and seven had none in the high-expression group (P = 0.035). We isolated exosomes successfully, and demonstrated that serum exosomal HOTAIR originated from primary breast cancer tissue. We conclude that serum exosomal HOTAIR exhibits the potential to be a diagnostic and prognostic biomarker. High expression of serum exosomal HOTAIR was also correlated with poor neoadjuvant chemotherapy and response to tamoxifen therapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
Breast cancer is the most common tumor found in women worldwide (DeSantis et al. 2017; Bray et al. 2018). Although comprehensive treatment for breast cancer includes surgery, chemotherapy, radiotherapy and hormone therapy, it still entails poor outcomes for advanced breast cancer patients (Bleyer and Welch 2012). Lack of efficient biomarkers to indicate prognosis and chemotherapy resistance are therefore two crucial factors that can lead to the progression of disease (Murtaza et al. 2013; Tang et al. 2017). Thus, it is incumbent upon us to discover appropriate diagnostic and prognostic biomarkers. One of these biomarkers may be found in the use of exosomes.
Exosomes are small membrane vesicles (30–150 nm) that originate from the endosomal membrane compartment (Regev-Rudzki et al. 2013; Wang et al. 2016), and cells can release exosomes that then persist in body fluids (Dear et al. 2013). Exosomes contain important biologically active species, including miRNA, lncRNA and circRNAs (Thoms et al. 2015). Investigators have recently demonstrated that exosomes not only play key roles in cell-cell communication, but also in the progression of tumorigenesis and tumor metastasis (Luga et al. 2012; Boelens et al. 2014). Although exosomes – especially lncRNA – also contribute significantly to tumor metastasis and chemotherapy resistance, they remain largely uncharacterized.
LncRNAs are a class of non-coding RNAs with biologic function, but which cannot be translated into protein (Lee 2012). HOTAIR is an lncRNA of 2.2 kb in length that is transcribed from the antisense strand of the HOXC gene cluster present in chromosome 12 (Rinn et al. 2007; Bhan and Mandal 2015). Increasing evidence indicates that expression of HOTAIR correlates with malignant tumors, including breast cancer (Gupta et al. 2010; Sørensen et al. 2013), ovarian cancer (Nakayama et al. 2013), hepatocellular carcinoma (Yang et al. 2011) and renal carcinoma (Wu et al. 2014). Recent studies have revealed that HOTAIR was expressed at a high level in breast cancer tissues compared with adjacent non-tumorous tissues (Gupta et al. 2010; Sørensen et al. 2013), and that overexpression of HOTAIR promoted breast cancer cell proliferation, invasion and migration (Stefani 2007; Chisholm et al. 2012).
Although much has been published on exosomes and HOTAIR, few publications mention the relationship between the two. Wang and his colleagues demonstrated that HOTAIR exists in serum exosomes, and serum exosomal HOTAIR has the potential of developing into a diagnostic and prognostic biomarker in laryngeal squamous cell carcinoma (Wang et al. 2014). Few studies have depicted the value and function of exosomal HOTAIR in breast cancer patients; however, it remains largely uninvestigated. In the present study, we uncovered the generation of HOTAIR in exosomes and evaluated the diagnostic and prognostic value of breast cancer exosomal HOTAIR. We additionally assessed the relationships among exosomal HOTAIR expression, neoadjuvant chemotherapy and response to tamoxifen therapy.
2 Materials and methods
2.1 Patients, serum and tissue sampling and follow-up
The protocols of the present study were approved by the Ethics Committees of the Third Affiliated Hospital of Kunming Medical University, Tumor Hospital of Yunnan. All research participants provided written informed consent prior to enrollment in our study, and these were stored in our hospital database. Serum samples were obtained from the Third Affiliated Hospital of Kunming Medical University, Tumor Hospital of Yunnan, with 15 breast cancer patients treated surgically and 15 healthy individuals enrolled as controls; 25 patients received neoadjuvant chemotherapy before surgery and another 25 patients received tamoxifen hormone treatment after surgery, all between July 2012 and December 2012. We simultaneously collected 20 breast cancer tissue samples and stored them at −80°C for further analysis. Our clinic visits consisted of follow-ups for all patients every 3 months for the first 2 years, every 6 months during the subsequent 3 years, and every year thereafter until either death occurred or when August of 2018 was reached. Blood samples from breast cancer patients were mixed with ethylenediaminetetraacetic acid and then centrifuged at 3000×g for 15 min at 4°C to collect supernatants. Supernatants were then stored at −80°C for further study. This same protocol was also followed to harvest and store cell culture medium supernatants.
2.2 Cell lines and culture
Human breast cancer cell lines (MDA-MB-231 and MCF-7) and a normal breast epithelial cell line (MCF-10A) were purchased from the Type Culture Collection of the Chinese Academy of Sciences (Shanghai, China). Culture medium contained RPMI-1640 (Corning, USA) and 10% fetal bovine serum (Corning, USA). Cell lines were cultured in a humidified atmosphere of 95% air and 5% CO2 at 37°C.
2.3 Isolation of exosomes
We used a 0.45-μm polyvinylidene fluoride (PVDF) filter (Millipore, Billerica, MA, USA) for serum and medium. ExoQuick solution (System Biosciences, Mountain View, CA, USA) was added and mixed with supernatant, and the mixture was stored at −4°C for 30 min. We then harvested exosomes by an ultracentrifugation at 1500×g for 30 min at 4°C.
2.4 Transmission electron microscopy
We used phosphate-buffered saline (PBS) (0.5 mg/mL) to dilute exosome samples, and a sequenced, glow-discharged copper grid was used to obtain exosomes. The exosomes were fully stained in an aqueous solution of phosphotungstic acid (2%) that we incubated for 1 min. We then wiped off excess buffer and finally stained the grid with 2% uranyl acetate at pH 7.0 for 40 s. The grid was sequenced and air dried at room temperature. Exosomes were examined under transmission electron microscopy (JEM-1-11 microscope, Japan) at 100 keV.
2.5 A xenograft model of human breast cancer
Cells (5 × 106 MDA-BC-231 or MCF-7) were washed with PBS and suspended in ice-cold membrane matrix (BD Matrigel). Cells were then injected into the subcutaneous layer of nude mice for experiments, or sham injection of normal saline was used for controls; we observed a temporal sequence of 4 weeks of feeding. Under anesthesia, blood from nude mice was collected by eyeball enucleation and samples were stored in procoagulant tubes.
2.6 Western blot analysis
We extracted total protein with RIPA buffer (BOSTER, Wuhan, China), and measured total protein concentration using a BCA protein assay kit (BOSTER, Wuhan, China). SDS-PAGE gels (10%) were used to separate 50 μg of protein, and we then transferred the protein onto PVDF membranes (Millipore). After blocking in Tris-buffered saline-Tween solution containing 5% non-fat milk for 1 h, we incubated the membranes overnight at 4°C with primary anti-CD63 antibody (1:1000 dilution; ab59479, Abcam, USA) and anti-Hsp70 antibody (1:1000 dilution; ab2787, Abcam, USA). Subsequently, the membranes were washed 3 times with TBST for 10 min and probed with goat anti-rabbit HRP secondary antibody (1:2000 dilution, ab6721, Abcam, USA) for 1 h at room temperature. We visualized signals with enhanced chemiluminescence solution (BOSTER, Wuhan, China) by exposure to film (Tang et al. 2017).
2.7 RNA extraction, RT-PCR and qPCR
Total RNA was extracted from samples and exosomes by using the MiniBEST Universal RNA Extraction Kit (Takara, Dalian, China) according to the manufacturer’s instructions. We measured total RNA concentration on the Peqlab NanoDrop and checked its quality by using RNA LabChips on an Agilent Bioanalyzer 2100 (Agilent Technologies). RNA with an integrity number greater than 6.5 was used for cDNA synthesis, and cDNAs were reverse transcribed using a PrimeScript™RT reagent kit (TaKaRa, Dalian, China). SYBR® Premix Ex Taq™ II (TaKaRa) was used to perform real-time PCR, and reactions were run in duplicate at 95°C for 30 s for 1 cycle, 95°C for 3 s and 60°C for 30 s for 40 cycles. Primers were designed as follows: HOTAIR forward primer, 5′-GGCGGATGCAAGTTAATAAAAC-3′; reverse primer, 5′-TACGCCTGAGTGTTCACGGAG-3′; and internal reference U6 primer, 5′-CAAATTCGTGAAGCGTTCCATAT-3′. Ct values of the samples were calculated, and the relative RNA levels were analyzed with the 2−ΔΔCt method (Tang et al. 2018).
2.8 Neoadjuvant chemotherapy treatment
Twenty-five patients received an anthracycline + taxane + cyclophosphamide regimen. Of these 25 patients, 14 underwent 2–4 cycles of a TAC regimen (docetaxel, 75 mg/m2 iv, on day 1; pirarubicin, 60 mg/m2 iv, on day 1; cyclophosphamide, 600 mg/m2 iv, on day 1; every 3 weeks). Eleven patients received 2–4 cycles of TEC regimen (docetaxel, 75 mg/m2 iv, on day 1; epirubicin, 100 mg/m2 iv, on day 1; cyclophosphamide, 600 mg/m2 iv, on day 1; every 3 weeks).
2.9 Tamoxifen treatment
All 25 patients received a dose of 20 mg of oral tamoxifen daily. Patients at high risk of cancer recurrence were given two options for suppression of ovarian function: leuprorelin at a dose of 3.75 mg subcutaneously every 28 days or bilateral oophorectomy.
2.10 Statistical analysis
Statistical analyses were performed using SPSS 22.0 (IBM Corp, NY, USA) and GraphPad Prism 6.0. Comparisons of continuous outcomes between groups were performed using a two-tailed, paired Student’s t-test. The log-rank test and Kaplan–Meier estimator method were used for survival analyses; and receiver operating characteristic (ROC) curves and AUC values were used to assess diagnostic accuracy by calculating sensitivities and specificities. The relationship between the expression of HOTAIR and neoadjuvant chemotherapy or response to tamoxifen therapy was evaluated with the χ2 test. P < 0.05 was considered to indicate a statistically significant difference. *P < 0.05, **P < 0.01, ***P < 0.001, relative to controls.
3 Results
3.1 Exosome characterization
We used transmission electron microscopy to distinguish the characteristics of exosomes (figure 1A), and detected expression of the characteristic exosomal protein markers CD63 and Hsp70 by western blot assays in serum exosomal (exo) and exosome-depleted supernatant (exo-d) samples (figure 1B).
3.2 Source of serum exosomal HOTAIR
We hypothesized that serum exosomal HOTAIR was generated from primary tumor tissue and released into blood, and designed individual experiments to explore this hypothesis. First, we compared the expression levels of serum exosomal HOTAIR between 15 breast cancer patients and 15 healthy individuals, and demonstrated that breast cancer patients expressed significantly higher serum exosomal HOTAIR than did the healthy controls (P < 0.001, figure 2A). Second, when we observed the former 15 patients continuously and collected their serum samples 3 months after surgery, their serum exosomal HOTAIR levels were markedly decreased compared with the expression levels before surgery (P < 0.001, figure 2B). In the third experiment, the exosomes in the supernatant of cell culture medium were collected, and we found that with time, the expression levels of exosomal HOTAIR in the medium increased in both breast cancer cell lines (72 h > 48 h > 24 h, 48 h vs 24 h, P < 0.05; 72 h vs 24 h, P < 0.01). However, this phenomenon was not observed in the normal breast epithelial cell line MCF-10A (figure 2C). In the fourth experiment we established a human-derived breast cancer xenograft model 4 weeks after injection, and observed that serum exosomal HOTAIR in nude mice was expressed at markedly higher levels than in the mock group (P < 0.001, figure 2D). Based on our four experiments, we recognized that serum exosomal HOTAIR originated from breast cancer primary tissue and was then released into the blood.
Origin of serum exosomal HOTAIR. (A) Serum exosomal HOATIR expression in breast cancer patients and healthy people. (B) Serum exosomal HOATIR expression in breast cancer patients before and after surgery. (C) Medium exosomal HOATIR expression in breast cancer cells and normal breast epithelial cells at different times. (D) Serum exosomal HOATIR expression in xenograft models.
3.3 Diagnostic and prognostic values of serum exosomal HOTAIR
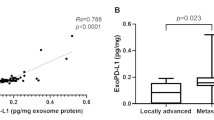
We performed ROC curve analyses to further elucidate potential diagnostic and prognostic values of serum exosomal HOTAIR. We collected CA15-3 values from 20 patients and also performed ROC curve analysis, and compared results with serum exosomal HOTAIR ROC curves. The AUC of the serum exosomal HOTAIR was 0.9178 (95% CI, 0.8407–1.017; P < 0.01), significantly greater than the AUC for CA15-3 (0.7378; 95% CI, 0.5585–0.9170; P = 0.03) (figure 3A and B).
We further investigated the prognosis for breast cancer patients using exosomal HOTAIR expression obtained directly from cancerous tissues, and separated the patients into high expression (++/+++) and low expression (+) according to the qPCR results. The clinicopathological characteristics for exosomal HOTAIR low- and high-expression subgroups are listed in table 1. The results of the survival analysis revealed that high expression of exosomal HOTAIR led to a worse disease-free survival (P = 0.0481) and overall survival (P = 0.0463) than low exosomal HOTAIR expression (figure 3C and D).
3.4 Correlation between serum exosomal HOTAIR expression and response to neoadjuvant chemotherapy
We focused on 25 patients who received neoadjuvant chemotherapy before surgery to investigate how HOTAIR expression would influence response to neoadjuvant chemotherapy. Of these 25 patients, 14 exhibited high expression and 11 exhibited low expression. In the high-expression group, six patients achieved PR and eight SD; however, in the low-expression group, nine patients showed PR and two SD (P = 0.048, table 2). Based on the chi-square test results we suggest that high expression of HOTAIR may lead to a poor response to neoadjuvant chemotherapy.
3.5 Relation between exosomal HOTAIR expression in serum and response to tamoxifen therapy
We included 25 patients who received tamoxifen hormone treatment in this study. In this patient cohort, 13 showed high HOTAIR expression and 12 manifested low expression. In the low-expression group, one patient had a recurrence of breast cancer while another 10 exhibited no recurrence. In the high-expression group, six showed a recurrence and seven did not (P = 0.035, table 3). These results suggested that high expression of HOTAIR could lead to a poor response to tamoxifen hormone therapy.
4 Discussion
In the present study, we separated exosomes from serum, culture medium and tumorous tissues. To the best of our knowledge, we are the first group to demonstrate that HOTAIR originates in serum exosomes. We are also the first to investigate the diagnostic and prognostic values of exosomal HOTAIR in serum, the correlation between serum exosomal HOTAIR expression and response to neoadjuvant chemotherapy, and the relationship between serum exosomal HOTAIR expression and response to tamoxifen therapy.
Research on exosomes is currently an exciting area (Hessvik and Llorente 2018; Hu et al. 2018; Morton et al. 2018), and evidence is accumulating that exosomes play important roles in cell-cell communication, tumorigenesis, tumor metastasis and the tumor microenvironment (Luga et al. 2012; Boelens et al. 2014; Hu et al. 2018). However, the molecular nature of exosomal contents remains largely unelucidated. Although Tan et al. (2018) revealed that exosomes contained important biologically active species such as miRNAs, lncRNAs and circRNAs; the source of these molecules remains arcane. Liu et al. (2016) found that the exosomal lncRNA CRNDE-h has a strong correlation with primary colorectal cancer. In the present study, we designed four experiments to investigate the generation of serum exosomal HOTAIR, and demonstrated after in vivo, in vitro and clinical research that serum exosomal HOTAIR is derived from primary breast cancer tissues and is packed into a membrane structure as exosomes for ultimate release into the bloodstream.
The function of serum exosomal lncRNAs such as HOTAIR still requires clarification. Song et al. (2015) illustrated that exosome-derived Hotair was a critical regulator and potent marker for rheumatoid arthritis, and Wang and colleagues demonstrated the potential for exosomal HOTAIR as a biomarker for prognosis and diagnosis in laryngeal squamous cell carcinoma patients (Wang et al. 2014). Investigators have also uncovered exosomal HOTAIR in bladder cancer, cervical cancer and gallbladder carcinoma, and showed that expression patterns differed between cancer patients and healthy individuals (Berrondo et al. 2016; Zhang et al. 2016; Tan et al. 2018). However, there is currently no extant report on serum exosomal HOTAIR expression in breast cancer patients. The present study is the first to reveal serum exosomal HOTAIR expression in breast cancer patients: we observed that serum exosomal HOTAIR was expressed at higher levels in breast cancer patients relative to healthy people, and that overexpression of serum exosomal HOTAIR correlated poorly with disease-free survival or overall survival. Our results thus showed that exosomal HOTAIR has the potential to be a prognostic and diagnostic biomarker for breast cancer patients.
The treatment of breast cancer requires complex and systematic treatment approaches (Fan et al. 2014; Storz-Pfennig and Wolf 2014), and neoadjuvant and adjuvant chemotherapies remarkably improve outcomes for breast cancer patients. A number of investigators have reported that high expression of HOTAIR may lead to chemotherapy resistance (Liu et al. 2013; Teschendorff et al. 2015; Wang et al. 2015; DeSantis et al. 2017; Li et al. 2017; Cheng et al. 2018), and the mechanisms underlying this phenomenon included HOTAIR downregulation of P21 expression (Liu et al. 2013) and activation of the NF/kB signaling pathway. However, there are no reports on how HOTAIR – particularly exosomal HOTAIR – expression influences the response to breast cancer chemotherapy. Our study is also the first to show that overexpression of exosomal HOTAIR was correlated with a poor PR response in breast cancer patients who received neoadjuvant chemotherapy treatment. Our results were similar to other studies, although there remained differences. Although current research in the literature focuses more on HOTAIR and platinum, our research focuses on the first-line chemotherapy strategy that uses the anthracene nucleus combined with taxane. We demonstrated that overexpression of exosomal HOTAIR correlated not only with platinum resistance, but also with a poor response to chemotherapy that entailed the anthracene nucleus combined with taxane. These results may in the future present a novel chemotherapeutic strategy for breast cancer patients.
Tamoxifen therapy is not only an important treatment as per the National Comprehensive Cancer Network (NCCN) guidelines, it provides a significant protective modality for breast cancer patients who are ER/PR positive (Osborne 1998; Francis et al. 2015). Xue et al. (2016) demonstrated that LncRNA HOTAIR enhanced ER signaling and conferred tamoxifen resistance in breast cancer patients, and this stimulated our interest in this field. Other than the report by Xue et al. there are no studies of how HOTAIR influences tamoxifen treatment. The present study was the first to reveal that a high expression of HOTAIR may lead to a poor response to tamoxifen hormone therapy, and our results were similar to those of Xue’s. However, our study was the first to focus on the relationship between exosomal HOTAIR and clinical tamoxifen treatment; and should provide a foundation for further clinical trials.
One drawback to our study is the overall small sample size, and we expect to increase our sample population in future studies to corroborate and further support our results.
In summary, our research suggested that exosomal HOTAIR plays a significant role in breast cancer. Serum exosomal HOTAIR is derived from primary breast cancer tissues and then released into blood. Serum exosomal HOTAIR appears to us to have the potential to be a prognostic and diagnostic biomarker for breast cancer patients. Overexpression of exosomal HOTAIR was correlated with poor PR rate for breast cancer patients receiving neoadjuvant chemotherapy. High expression of HOTAIR may also lead to a poor response to tamoxifen hormone therapy. However, due to the limitations of the current study, further investigations on the clinical or experimental use of exosomal HOTAIR are required to confirm these data.
References
Berrondo C, Flax J, Kucherov V, Siebert A, Osinski T, Rosenberg A, Fucile C, Richheimer S and Beckham CJ 2016 Expression of the long non-coding RNA HOTAIR correlates with disease progression in bladder cancer and is contained in bladder cancer patient urinary exosomes. PLoS ONE 11 e0147236
Bhan A and Mandal SS 2015 LncRNA HOTAIR: a master regulator of chromatin dynamics and cancer. Biochim. Biophys. Acta 1856 151–164
Bleyer A and Welch HG 2012 Effect of three decades of screening mammography on breast-cancer incidence. N. Engl. J. Med. 367 1998–2005
Boelens MC, Wu TJ, Nabet BY, Xu B, Qiu Y, Yoon T, Azzam DJ, Twyman-Saint VC, Wiemann BZ, Ishwaran H, Ter BPJ, Jonkers J, Slingerland J and Minn AJ 2014 Exosome transfer from stromal to breast cancer cells regulates therapy resistance pathways. Cell 159 499–513
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA and Jemal A 2018 Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 68 394–424
Cheng C, Qin Y, Zhi Q, Wang J and Qin C 2018 Knockdown of long non-coding RNA HOTAIR inhibits cisplatin resistance of gastric cancer cells through inhibiting the PI3 K/Akt and Wnt/β-catenin signaling pathways by up-regulating miR-34a. Int. J. Biol. Macromol. 107 2620–2629
Chisholm KM, Wan Y, Li R, Montgomery KD, Chang HY and West RB 2012 Detection of long non-coding RNA in archival tissue: Correlation with polycomb protein expression in primary and metastatic breast carcinoma. PLoS ONE 7 e47998
Dear JW, Street JM and Bailey MA 2013 Urinary exosomes: A reservoir for biomarker discovery and potential mediators of intrarenal signalling. Proteomics 13 1572–1580
DeSantis CE, Ma J, Goding SA, Newman LA and Jemal A 2017 Breast cancer statistics, 2017, racial disparity in mortality by state. CA Cancer J. Clin. 67 439–448
Fan L, Strasser-Weippl K, Li JJ, St LJ, Finkelstein DM, Yu KD, Chen WQ, Shao ZM and Goss PE 2014 Breast cancer in China. Lancet Oncol. 15 e279–e289
Francis PA, Regan MM, Fleming GF, Láng I, Ciruelos E, Bellet M, Bonnefoi HR, Climent MA, et al 2015 Adjuvant ovarian suppression in premenopausal breast cancer. N. Engl. J. Med. 372 436–446
Gupta RA, Shah N, Wang KC, Kim J, Horlings HM, Wong DJ, Tsai MC, Hung T, Argani P, Rinn JL, Wang Y, Brzoska P, Kong B, Li R, West RB, van de Vijver MJ, Sukumar S and Chang HY 2010 Long non-coding RNA HOTAIR reprograms chromatin state to promote cancer metastasis. Nature 464 1071–1076
Hessvik NP and Llorente A 2018 Current knowledge on exosome biogenesis and release. Cell. Mol. Life Sci. 75 193–208
Hu C, Chen M, Jiang R, Guo Y, Wu M and Zhang X 2018 Exosome-related tumor microenvironment. J. Cancer 9 3084–3092
Lee JT 2012 Epigenetic regulation by long noncoding RNAs. Science 338 1435–1439
Li P, Zhang X, Wang L, Du L, Yang Y, Liu T, Li C and Wang C 2017 lncRNA HOTAIR contributes to 5FU resistance through suppressing miR-218 and activating NF-κB/TS signaling in colorectal cancer. Mol. Ther. Nucleic Acids 8 356–369
Liu T, Zhang X, Gao S, Jing F, Yang Y, Du L, Zheng G, Li P, Li C and Wang C 2016 Exosomal long noncoding RNA CRNDE-h as a novel serum-based biomarker for diagnosis and prognosis of colorectal cancer. Oncotarget 7 85551–85563
Liu Z, Sun M, Lu K, Liu J, Zhang M, Wu W, De W, Wang Z and Wang R 2013 The long noncoding RNA HOTAIR contributes to cisplatin resistance of human lung adenocarcinoma cells via downregualtion of p21(WAF1/CIP1) expression. PLoS ONE 8 e77293
Luga V, Zhang L, Viloria-Petit AM, Ogunjimi AA, Inanlou MR, Chiu E, Buchanan M, Hosein AN, Basik M and Wrana JL 2012 Exosomes mediate stromal mobilization of autocrine Wnt-PCP signaling in breast cancer cell migration. Cell 151 1542–1556
Morton DJ, Kuiper EG, Jones SK, Leung SW, Corbett AH and Fasken MB 2018 The RNA exosome and RNA exosome-linked disease. RNA 24 127–142
Murtaza M, Dawson SJ, Tsui DW, Gale D, Forshew T, Piskorz AM, Parkinson C, Chin SF, et al 2013 Non-invasive analysis of acquired resistance to cancer therapy by sequencing of plasma DNA. Nature 497 108–112
Nakayama I, Shibazaki M, Yashima-Abo A, Miura F, Sugiyama T, Masuda T and Maesawa C 2013 Loss of HOXD10 expression induced by upregulation of miR-10b accelerates the migration and invasion activities of ovarian cancer cells. Int. J. Oncol. 43 63–71
Osborne CK 1998 Tamoxifen in the treatment of breast cancer. N. Engl. J. Med. 339 1609–1618
Regev-Rudzki N, Wilson DW, Carvalho TG, Sisquella X, Coleman BM, Rug M, Bursac D, Angrisano F, Gee M, Hill AF, Baum J and Cowman AF 2013 Cell-cell communication between malaria-infected red blood cells via exosome-like vesicles. Cell 153 1120–1133
Rinn JL, Kertesz M, Wang JK, Squazzo SL, Xu X, Brugmann SA, Goodnough LH, Helms JA, Farnham PJ, Segal E and Chang HY 2007 Functional demarcation of active and silent chromatin domains in human HOX loci by noncoding RNAs. Cell 129 1311–1323
Song J, Kim D, Han J, Kim Y, Lee M and Jin EJ 2015 PBMC and exosome-derived hotair is a critical regulator and potent marker for rheumatoid arthritis. Clin. Exp. Med. 15 121–126
Sørensen KP, Thomassen M, Tan Q, Bak M, Cold S, Burton M, Larsen MJ and Kruse TA 2013 Long non-coding RNA HOTAIR is an independent prognostic marker of metastasis in estrogen receptor-positive primary breast cancer. Breast Cancer Res. Treat. 142 529–536
Stefani M 2007 Generic cell dysfunction in neurodegenerative disorders: role of surfaces in early protein misfolding, aggregation, and aggregate cytotoxicity. Neuroscientist 13 519–531
Storz-Pfennig P and Wolf K 2014 Biomarkers in early breast cancer and beyond: who needs all those tests. Lancet Oncol. 15 919–920
Tan SK, Pastori C, Penas C, Komotar RJ, Ivan ME, Wahlestedt C and Ayad NG 2018 Serum long noncoding RNA HOTAIR as a novel diagnostic and prognostic biomarker in glioblastoma multiforme. Mol. Cancer 17 74
Tang S, Pan H, Wei W, Yang H, Liu J and Yang R 2017 GOLPH3: A novel biomarker that correlates with poor survival and resistance to chemotherapy in breast cancer. Oncotarget 8 105155–105169
Tang S, Yang R, Zhou X, Pan H and Liu J 2018 Expression of GOLPH3 in patients with non-small cell lung cancer and xenografts models. Oncol. Lett. 15 7555–7562
Teschendorff AE, Lee SH, Jones A, Fiegl H, Kalwa M, Wagner W, Chindera K, Evans I, et al 2015 HOTAIR and its surrogate DNA methylation signature indicate carboplatin resistance in ovarian cancer. Genome Med. 7 108
Thoms M, Thomson E, Baßler J, Gnädig M, Griesel S and Hurt E 2015 The exosome is recruited to RNA substrates through specific adaptor proteins. Cell 162 1029–1038
Wang J, Zhou Y, Lu J, Sun Y, Xiao H, Liu M and Tian L 2014 Combined detection of serum exosomal miR-21 and HOTAIR as diagnostic and prognostic biomarkers for laryngeal squamous cell carcinoma. Med. Oncol. 31 148
Wang Y, Wang H, Song T, Zou Y, Jiang J, Fang L and Li P 2015 HOTAIR is a potential target for the treatment of cisplatin-resistant ovarian cancer. Mol. Med. Rep. 12 2211–2216
Wang X, Xu C, Hua Y, Sun L, Cheng K, Jia Z, Han Y, Dong J, Cui Y and Yang Z 2016 Exosomes play an important role in the process of psoralen reverse multidrug resistance of breast cancer. J. Exp. Clin. Cancer Res. 35 186
Wu Y, Liu J, Zheng Y, You L, Kuang D and Liu T 2014 Suppressed expression of long non-coding RNA HOTAIR inhibits proliferation and tumourigenicity of renal carcinoma cells. Tumour Biol. 35 11887–11894
Xue X, Yang YA, Zhang A, Fong KW, Kim J, Song B, Li S, Zhao JC and Yu J 2016 LncRNA HOTAIR enhances ER signaling and confers tamoxifen resistance in breast cancer. Oncogene 35 2746–2755
Yang Z, Zhou L, Wu LM, Lai MC, Xie HY, Zhang F and Zheng SS 2011 Overexpression of long non-coding RNA HOTAIR predicts tumor recurrence in hepatocellular carcinoma patients following liver transplantation. Ann. Surg. Oncol. 18 1243–1250
Zhang J, Liu SC, Luo XH, Tao GX, Guan M, Yuan H and Hu DK 2016 Exosomal long noncoding RNAs are differentially expressed in the cervicovaginal lavage samples of cervical cancer patients. J. Clin. Lab. Anal. 30 1116–1121
Acknowledgements
This work was supported by the National Natural Science Foundation of China (Grant Nos. 81402306, 81760481 and 81360312).
Author information
Authors and Affiliations
Corresponding author
Additional information
Communicated by xxxxx.
Corresponding editor: Sorab Dalal
Rights and permissions
About this article
Cite this article
Tang, S., Zheng, K., Tang, Y. et al. Overexpression of serum exosomal HOTAIR is correlated with poor survival and poor response to chemotherapy in breast cancer patients. J Biosci 44, 37 (2019). https://doi.org/10.1007/s12038-019-9861-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12038-019-9861-y