Abstract
It has recently been accepted that long-term high-fat diet (HFD) intake is a significant possible cause for prediabetes and cognitive and brain dysfunction through the disruption of brain mitochondrial function and dynamic balance. Although modulation of mitochondrial dynamics by inhibiting fission and promoting fusion has been shown to reduce the morbidity and mortality associated with a variety of chronic diseases, the impact of either pharmacological inhibition of mitochondrial fission (Mdivi-1) or stimulation of fusion (M1) on brain function in HFD-induced prediabetic models has never been studied. Thirty-two male Wistar rats were separated into 2 groups and fed either a normal diet (ND, n = 8) or HFD (n = 24) for 14 weeks. At week 12, HFD-fed rats were divided into 3 subgroups (n = 8/subgroup) and given an intraperitoneal injection of either saline, Mdivi-1 (1.2 mg/kg/day), or M1 (2 mg/kg/day) for 2 weeks. Cognitive function and metabolic parameters were determined toward the end of the protocol. The rats then were euthanized, and the brain was immediately removed in order to evaluate brain mitochondrial function and mitochondrial dynamics. HFD-fed rats experienced prediabetes, evidenced by elevated plasma insulin and the HOMA index, impaired mitochondrial function in the brain, altered dynamic regulation, and cognitive impairment were also found. Mdivi-1 and M1 treatment exerted neuroprotection to a similar extent by improving metabolic parameters, balancing mitochondrial dynamics, and reducing mitochondrial dysfunction, resulting in a gradual increase in cognitive function. Therefore, pharmacological targeting of mitochondrial fission and fusion protected the brain against chronic HFD-induced prediabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past decade, the incidence of obesity and the associated burden of diseases have increased markedly throughout the world [1, 2]. It is well accepted that exposure to a chronic high-fat diet (HFD) induces obesity-related insulin resistance and increases circulating insulin levels, decreasing insulin sensitivity and progression to type 2 diabetes [3]. Supporting data from clinical and animal researches revealed that obesity-related insulin resistance or prediabetes is associated with an elevated risk of numerous chronic illnesses, notably neurodegeneration and cognitive deficit [4,5,6,7]. Similarly, our previous reports described a link between a decline in cognitive function and the prediabetic condition in 12-week HFD-fed rats [8,9,10,11]. The underlying mechanisms associated with prediabetes-induced neurodegeneration have been attributed to neuroinflammation, oxidative stress, programmed apoptosis, mitochondrial dysfunction, and changes in mitochondrial dynamics [11,12,13].
Mitochondria are dynamically active organelles governed primarily by fusion and fission events. The balance between fusion and fission is essential for the regulation of energy metabolism through mitochondrial quality control mechanisms [14, 15]. The proteins mitofusin (Mfn) 1, 2 and Optic atrophy type 1 (Opa1) primarily control mitochondrial fusion, which acts to repair damaged mitochondria while also increasing energy production according to metabolic requirements [16,17,18]. Meanwhile, fission is governed by the dynamin-related protein 1 (Drp1) occurring when mitochondria are injured or exposed to intense degrees of oxidative responses [16,17,18]. As shown previously, mitochondria play important roles in the pathogenesis of various HFD-induced neurodegenerative disorders [8,9,10,11]. Changes in mitochondrial function promote oxidative stress, which results in higher fatty acid synthesis and increased lipid deposition, both of which are linked to insulin resistance [19]. Increased mitochondrial fission, in particular, has been attributed to obesity and the resulting insulin resistance in a variety of tissues. Increased mitochondrial fission in the brain due to elevated phosphorylated Drp1 at serine 616 (p-Drp1ser616) could induce neuronal death and synaptic dysfunction [20]. It has also been shown that HFD-activated p-Drp1ser616 aggravated amyloid plaque aggregation and neurofibrillary tangles in Alzheimer’s disease (AD) [21]. In contrast, a decrease in mitochondrial fusion proteins (Mfn1/2) has been shown to worsen the severity of neurodegenerative diseases [22]. Therefore, targeting mitochondrial dynamics by suppressing mitochondrial fission and enhancing fusion could be beneficial for patients with either prediabetes or diabetes who suffer from neurodegenerative disorders.
Fortunately, pharmacological modulation of mitochondrial dynamics has been shown to exert positive impact on multiple brain disorders [23,24,25,26,27]. Mitochondrial division inhibitor 1 (Mdivi-1) is an effective inhibitor of mitochondrial division that has been reported to inhibit Drp1-dependent mitochondrial fission and Bax-dependent cytochrome c release during programmed apoptosis [28]. Administration of Mdivi-1 at 1.2 mg/kg alleviated neuronal apoptosis in animal models of brain ischemia [29, 30]. Similarly, upregulation of Mfn2 protein expression by a mitochondrial fusion promoter (M1) at 2 mg/kg effectively mitigated brain mitochondrial dysfunction, blood brain barrier (BBB) breakdown, reduced apoptosis, macrophage infiltration, and Alzheimer’s disease-related proteins in rats with cardiac I/R injury [26]. In addition, our previous study demonstrated that either 1.2 mg/kg Mdivi-1 or 2 mg/kg M1 treatment for 14 days improves cardiometabolic profiles in pre-diabetic models [10]. Despite those previous reports, the effects of both Mdivi-1 and M1 on cognitive and brain mitochondrial function in pre-diabetic rats have never been examined. We hypothesized that Mdivi-1 and M1 provide neuroprotection in pre-diabetic rats by enhancing mitochondrial function and restoring the levels of mitochondrial dynamic proteins, leading to improve cognitive performance.
Material and Methods
Animal Preparation and Ethical Approval
All rat studies followed NIH standards (Guide for the care and use of laboratory animals) and were carried out in accordance with the protocol authorized by the Faculty of Medicine, Chiang Mai University, Thailand (Ethical approval number: 34/2561). Male Wistar rats (n = 32, ~ 220 g, ~ 7 weeks old) were obtained from the National Laboratory Animal Center, Mahidol University, Bangkok, Thailand. This model of male Wistar rat has been used in our previous studies [31, 32]. All rats were fed standard rat chow with water ad libitum and kept at 25 °C, in a 12-h light/12-h dark cycle for 1 week.
Experimental Design
After acclimatization, rats were randomly assigned to one of two dietary groups: a normal diet (ND, comprising 19.77% energy from fat, n = 8) and a high-fat diet (HFD, comprising 59.28% calories from fat, n = 24) [12]. Twelve weeks after being fed on the same diet, rats in the HFD groups were divided into three subgroups to receive one of three interventions for 2 weeks: (1) vehicle (0.1% DMSO, i.p.), (2) mitochondrial fission inhibitor or Mdivi-1 (1.2 mg/kg/day, i.p.), and (3) mitochondrial fusion promoter or M1 (2 mg/kg/day, i.p.). Throughout the study, the body weight and dietary intake of all rats were recorded. Blood samples were taken from the tail vein at the beginning and end of the 2-week experimental period to determine metabolic parameters. An oral glucose tolerance test (OGTT), an open field test (OFT), and a novel object location (NOL) were performed. The rats were then sedated by intramuscular injections of zoletil (50 mg/kg, Vibbac Laboratories, Carros, France) and xylazine (0.15 mg/kg, Laboratorios Calier, S.A., Barcelona, Spain), and the brain was immediately removed for mitochondrial function and biochemical investigations. The experimental protocol is shown in Fig. 1.
Diagram of the experimental protocol. BW: body weight; DMSO: dimethyl sulfoxide; HDL: high-density lipoprotein; HFD: high-fat-diet fed rats; HFV: high-fat-diet fed rats with vehicle treatment; HFM1: high-fat-diet fed rats with M1 treatment; HFMdivi1: high-fat-diet fed rats with Mdivi-1 treatment; LDL: low-density lipoprotein; ND: normal-diet fed rats; NDV: normal-diet fed rats with vehicle treatment; OGTT: oral glucose tolerance test; TC: total cholesterol; TG: triglycerides
Determination of Metabolic Parameters
Using commercial colorimetric assays, fasting plasma glucose, total cholesterol (TC), triglyceride (TG) (Erba Diagnostics, Mannheim, Germany), and HDL levels (BioVision, Inc.) were determined. LDL levels were determined using the Friedewald formula. A sandwich ELISA kit was used to measure plasma insulin levels (Millipore, MI, USA). HOMA of insulin resistance was calculated using fasting plasma insulin and fasting plasma glucose concentrations from total area under the curve to determine the degree of insulin resistance (AUCg) [32].
Cognitive Function Test
OFT
Open field test (OFT) was conducted to examine general locomotor activity in rats as described previously [33]. The apparatus in this method is a circular-based box that is opened from above (70 cm of the base, 50 cm of height). Each animal was placed in the box and given 10 min to explore. The animals were taken out after 10 min of exploration. SMART 3.0 software was used to calculate total distance (cm), mean speed without resting (cm/s), and time spent in the center (s) (Panlab, Harvard Apparatus, Barcelona, Spain).
NOL
The novel object location (NOL) test is a learning and memory test that is dependent on the hippocampus. NOL test was performed in a black plastic box, a circular-based box opened from above (70 cm of diameter, 50 cm of height). The field base was paved by a black feature board (80 × 80 cm2). For visual clues on the arena’s walls, black and white strip lines were placed on the wall of the circular-based box. Two small metal cylinders (6.5 cm in diameter, 10 cm in height) were used. The task procedure consists of two phases: familiarization and NOL test. The familiarization phase was performed on the second day of behavioral testing. A single animal was placed in the box containing two similar objects, and rats were explored for 10 min, and the time of exploration was calculated as a percent exploration. On the third day, rats were again placed into the box containing two familiar objects, in which one object was placed at a new location. The test was performed for 10 min. A video was recorded using a recording camera above the box throughout each phase for off-line examination. The percentage exploration time and percentage preference index were calculated from the following formula: % index preference = [(time on object with new location)/(time on object 1 + time on object with new location)] × 100 [34].
Brain Mitochondrial Function Study
As previously described, brain mitochondria were collected using a differential centrifuge technique [35]. Following the removal of the brain, it was placed in a 5-mL ice-cold MSE solution (225 mmol/L mannitol, 75 mmol/L sucrose, 1 mmol/L EGTA, 5 mmol/L HEPES, and 1 mg/mL BSA, pH 7.4) to rapidly wash out the blood. The brain was then homogenized using a homogenizer at 600 rpm in a 10-mL ice-cold MSE solution containing 0.05% proteinase (Sigma-Aldrich). After centrifuging the homogenate at 2,000 g for 4 min, the supernatant was collected. The supernatant was then centrifuged for 9 min at 12,000 g. The mitochondrial pellets were collected and resuspended in 4 mL of ice-cold MSE-digitonin solution (0.02% digitonin in MSE solution). The solution was centrifuged at 12,000 g for an additional 11 min. Subsequently, the mitochondrial pellet was collected and resuspended in a respiration buffer with 150 mmol/L KCl, 5 mmol/L HEPES, 5 mmol/L K2HPO40.3H2O, 5 mmol/L l-glutamate, and 5 mmol/L pyruvate sodium salt. The mitochondrial protein was identified using the bicinchoninic acid assay. Isolated brain mitochondria at 0.4 mg/mL concentration were utilized to examine mitochondrial parameters, including ROS levels, membrane potential changes, and swelling in the brain mitochondria.
The fluorescence intensity of dichlorofluorescein (DCF) was used to evaluate the amount of ROS in the brain mitochondria. The red-to-green fluorescence intensity ratio of tetraethylbenzimidazolylcarbocyanine iodide (JC1) was used to measure brain mitochondrial membrane potential changes. The absorbance of mitochondrial protein in a respiration buffer was used to evaluate brain mitochondrial swelling. A fluorescent/absorbance microplate reader was used for all measurements (BioTek). A transmission electron microscope was used to capture images of brain mitochondria (TEM; JEM-1200 EX II, JEOL Ltd., Japan).
Determination of Protein Expressions by Western Blotting
The levels of expression of the mitochondrial fission proteins (p-Drp1ser616 and Drp1), mitochondrial fusion proteins (Mfn2 and Opa1), apoptotic proteins (Bax, Bcl2, Caspase3, and Cleaved caspase3), blood–brain barrier (BBB) protein (Claudin5), and neurodegenerative proteins (p-Tau, Tau, Amyloid-beta precursor protein (APP), amyloid-beta (Aβ)) were determined by Western blot analysis. In brief, the cortex and hippocampus were lysed with extraction buffer. The cortex lysate (1.8–2.7 mg/mL) or hippocampal lysate (0.9 mg/mL) was used to analyze the mitochondrial dynamic proteins. Gel electrophoresis on 10% polyacrylamide gel was used to separate the tissue lysate, which was then transferred onto nitrocellulose membranes. Immunoblots were blocked in Tris-buffer saline (pH 7.4) containing 0.1% Tween 20 for 1 h with 5% skim milk powder or BSA. Then, the membranes were probed with anti-Drp1, anti-p-Drp1ser616, anti-Mfn2, anti-Bax, anti-Bcl2, anti-Caspase3, anti-Cleaved caspase3, anti-Claudin5, anti-p-Tau, anti-Tau, anti-APP, anti-Aβ, and anti-β-Actin (Cell Signaling Technology, Danvers, MA, USA) for 12 h. Horseradish peroxidase conjugated with anti-rabbit IgG was used to identify bound antibodies. To identify peroxidase reaction products, enhanced chemiluminescence (ECL) detection reagents were used [34].
Statistical analysis
The data were presented as mean SEM. A one-way ANOVA was used to compare variables, followed by an LSD post-hoc test. P < 0.05 was regarded statistically significant.
The LSD was used as a post hoc test following the ANOVA to identify whether the mean variations were statistically significant from the others. The LSD was also chosen for multiple comparisons of data with the same characteristics [36]. In this study, we compared the effects of different treatments in this study for a total of 5 groups of analysis, and our data have the same characteristics with minor variations. Thus, our statistician recommended the LSD as a suitable test for our data. ANOVA was used for statistical analysis, and all results were corrected for multiple comparisons using the LSD test.
Results
Mdivi-1 and M1 Treatment Improved Metabolic Parameters in Pre-diabetic Rats
Body weight, visceral fat, plasma levels of insulin, glucose, TC, and LDL, as well as AUCg and HOMA index, of HFD-fed rats were substantially higher than those of ND-fed rats after 14 weeks of HFD intake (Table 1). However, in comparison to the ND-fed rats, the HFD-fed rats had lower HDL levels. No difference in food intake, plasma glucose, and TG levels among all groups was observed. These data showed that long-term HFD intake resulted in the prediabetic condition.
After the 2-week intervention, there were marked decreases in plasma cholesterol and LDL levels in the HFD-fed rats being given Mdivi1 and M1 treatment when compared with vehicle-treated HFD-fed rats (HFV) (Table 1). Interestingly, the degree of insulin sensitivity was also improved in the Mdivi1 and M1 treated HFD-fed rats as indicated by decreasing plasma insulin, AUCg, and HOMA index, when compared to HFV rats.
Mdivi-1 and M1 Treatment Reduced Cognitive Impairment, Alzheimer’s and BBB Protein Expressions in Pre-diabetic Rats
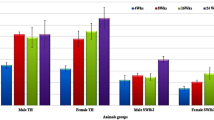
After ingestion of HFD for 14 weeks, the anxiety-related and exploratory behaviors were tested using OFT. The result showed that the total travel distance, mean speed without resting, and time spent in the center were not different among all groups, suggesting that locomotor activity and the anxiety-related and exploratory behaviors were intact in all rats and were not differences among groups (Fig. 2a-c). Next, the hippocampal-dependent learning and memory behavior were also tested using the NOL task (Fig. 2d-f). The results showed that the percentage of preference index of two objects during the familiarization phase was no different between groups (Fig. 2e). On the other hand, the preference (%) of two objects during the testing phase was markedly decreased in HFV rats, when compared to vehicle-treated ND-fed rats (NDV), indicating a decline in cognitive function of HFD-fed rats (Fig. 2f). Two weeks after interventions, the Mdivi1-and M1-treated HFD-fed rats displayed an increase in preference index (%) in comparison with the HFV rats (Fig. 2f).
The effects of Mdivi-1 and M1 treatment on anxiety-related and exploratory behaviors as well as cognitive function in pre-diabetic rats. a Total distance of OFT; b mean speed without resting of OFT; c time spent in the center of OFT; d NOL protocol; e % preference index during familiarization period; f % preference index during test period. Values are mean ± SEM. N = 8/group. *P < 0.05 vs NDV and †P < 0.05 vs HFV. HFV: high-fat-diet fed rats with vehicle treatment; HFM1: high-fat-diet fed rats with M1 treatment; HFMdivi1: high-fat-diet fed rats with Mdivi-1 treatment; NDV: normal-diet fed rats with vehicle treatment
In addition, long-term exposure to HFD consumption resulted in an increased Aβ/APP ratio in the cerebral tissue, indicating the development of Alzheimer’s like pathologies (Fig. 3a). Similarly, Tau hyperphosphorylation (increase p-Tau/Tau ratio) was also observed in HFV rats, compared with NDV rats (Fig. 3b). Both Mdivi-1 and M1 treatments in HFD-fed rats resulted in significantly reduced Aβ aggregation (Aβ/APP ratio) and Tau hyperphosphorylation (p-Tau/Tau ratio) back to the same levels of NDV rats (Fig. 3a and b).
The effects of Mdivi-1 and M1 treatment on Alzheimer’s and blood–brain barrier protein expression in pre-diabetic rats. a Aβ/APP ratio; b p-Tau/Tau ratio; c Claudin5/β-Actin ratio. Values are mean ± SEM. n = 8/group. *P < 0.05 vs NDV and †P < 0.05 vs HFV. Aβ: amyloid beta; APP: amyloid precursor protein; HFV: high-fat-diet fed rats with vehicle treatment; HFM1: high-fat-diet fed rats with M1 treatment; HFMdivi1: high-fat-diet fed rats with Mdivi-1 treatment; NDV: normal-diet fed rats with vehicle treatment
In relation to the expression of BBB protein, the results showed that the expression of claudin5 protein was markedly decreased in HFV rats when compared with NDV rats (Fig. 3c). Mdivi-1 and M1 treatment in HFD-fed rats effectively restored this level of protein expression to the same level of NDV rats (Fig. 3c).
Mdivi-1 and M1 Treatment Mitigated Brain Mitochondrial Dysfunction in Pre-diabetic Rats
Brain mitochondrial function was evaluated in this study by detecting ROS generation in mitochondria, membrane potential changes, and swelling. When compared to the NDV rats, the HFV rats showed a substantial increase in mitochondrial ROS levels, membrane potential depolarization, and swelling (Fig. 4a–c). Mdivi-1 or M1 had a similar efficacy in HFD-fed rats in attenuating brain mitochondrial dysfunction through reducing ROS production, depolarization of mitochondrial membranes, and swelling, compared with the HFV rats (Fig. 4a–c).
The effects of Mdivi-1 and M1 treatment on brain mitochondrial function in pre-diabetic rats. a Mitochondrial ROS production; b mitochondrial membrane potential changes; c mitochondrial swelling; d TEM representative images of brain mitochondria. Values are mean ± SEM. n = 8/group. *P < 0.05 vs NDV and †P < 0.05 vs HFV. HFV: high-fat-diet fed rats with vehicle treatment; HFM1: high-fat-diet fed rats with M1 treatment; HFMdivi1: high-fat-diet fed rats with Mdivi-1 treatment; NDV: normal-diet fed rats with vehicle treatment; ROS: reactive oxygen species
When compared to the NDV rats, the representative TEM images of brain mitochondria revealed that the mitochondrion in the HFV group showed signs of unfolding cristae and swelling (Fig. 4d). Whereas, HFD-fed rats treated with Mdivi-1 or M1 had reduced mitochondrial swelling, as seen by more prominent cristae in the mitochondria (Fig. 4d).
Mdivi-1 and M1 Treatment Reduced Brain Mitochondrial Dynamic Imbalance in Pre-diabetic Rats
Regarding the mitochondrial fission proteins, HFV rats had a significantly increased p-Drp1ser616/total Drp1 ratio, compared to NDV rats, indicating that the mitochondrial fission process was dominant after 14 weeks of HFD consumption (Fig. 5a). HFD-fed rats treated with either Mdivi-1 or M1 has a clearly decreased ratio of p-Drp1ser616/total Drp1, when compared with HFV rats (Fig. 5a). Mdivi-1 showed greater efficacy in reducing p-Drp1ser616/total Drp1 level than M1 treatment in HFD-fed rats (Fig. 5a).
The effects of Mdivi-1 and M1 treatment on brain mitochondrial dynamics in pre-diabetic rats. a p-Drp1ser616/Drp1 ratio; b Mfn2/β-Actin ratio; c Opa1/β-Actin ratio. Values are mean ± SEM. n = 8/group. *P < 0.05 vs NDV and †P < 0.05 vs HFV. Drp1: dynamin-related protein-1; p-Drp1ser616: phosphorylation of dynamin-related protein-1 at serine 616; HFV: high-fat-diet fed rats with vehicle treatment; HFM1: high-fat-diet fed rats with M1 treatment; HFMdivi1: high-fat-diet fed rats with Mdivi-1 treatment; Mfn2: mitofusin 2; NDV: normal-diet fed rats with vehicle treatment; Opa1: optic atrophy type 1
In addition to mitochondrial fission, the expression of mitochondrial fusion proteins (Mfn2 and Opa1) was investigated. In HFD-fed rats, HFV rats showed a significant decreased Mfn2 level, compared to NDV rats (Fig. 5b). After treatment with Mdivi-1 and M1, the expression of Mfn2 level was significantly increased, when compared to the HFV group (Fig. 5b). However, there was no difference in the expression of Opa1 among all groups (Fig. 5c).
Mdivi-1 and M1 Treatment Decreased Brain Programmed Apoptosis in Pre-diabetic Rats
Bax, Bcl2, and cleaved caspase3 expression was used as a marker of brain apoptosis. Our findings revealed that the ratios of Bax/Bcl2 and cleaved caspase3/caspase3 were substantially higher in the HFV rats compared to those of NDV rats (Fig. 6a, b). When compared to the HFV group, HFD-fed rats treated with Mdivi-1 and M1 had significantly reduced expression of those apoptotic proteins (Fig. 6a, b).
The effects of Mdivi-1 and M1 treatment on brain apoptosis in pre-diabetic rats. a Bax/Bcl2 ratio; b cleaved caspase3/Caspase3 ratio. Values are mean ± SEM. n = 8/group. *P < 0.05 vs NDV and †P < 0.05 vs HFV. Bax: Bcl2 associated X; Bcl2; B-cell lymphoma 2; HFV: high-fat-diet fed rats with vehicle treatment; HFM1: high-fat-diet fed rats with M1 treatment; HFMdivi1: high-fat-diet fed rats with Mdivi-1 treatment; NDV: normal-diet fed rats with vehicle treatment
Discussion
The major findings of this study are as follows: (1) Long-term HFD intake resulted in prediabetes with brain impairment. These adverse effects were due to metabolic disturbance leading to BBB breakdown, the impairment of brain mitochondrial function, brain mitochondrial dynamic dysregulation, increased expression of AD-related proteins, brain apoptosis, finally resulting in cognitive impairment. (2) Inhibition of mitochondrial fission using Mdivi-1 and promotion of fusion using M1 improved systemic metabolic parameters and cognitive function by attenuating insulin resistance, decreasing brain mitochondrial dysfunction and dynamic alteration, reducing expression of AD and BBB-related proteins, neuronal cell death, and in particular improving cognitive function.
Prediabetes induced by long-term HFD consumption is characterized by increases in visceral fat accumulation, body weight, dyslipidemia, and hyperinsulinemia with euglycemia. All of these pathological conditions can lead to the development of type 2 diabetes mellitus [4,5,6]. Numerous preliminary studies carried out by our team have demonstrated that chronic HFD consumption leads to the development of the prediabetic condition with brain disorders and cognitive decline through the modulation of mitochondrial function [34, 37,38,39,40]. Prolonged excessive fat deposition causes a rise in plasma free fatty acids (FFAs) and lipid buildup, resulting in long-chain acetyl coenzyme A (Acetyl-CoA) formation, followed by ceramide and diacylglycerol (DAG) aggregation. Rising ceramide and DAG levels have been shown to cause severe mitochondrial dysfunction by increasing mitochondrial β-oxidation and disrupting mitochondrial dynamic processes by boosting fission while impairing fusion [41,42,43,44]. It has been demonstrated that brain mitochondrial dysfunction occurs in cases of HFD consumption, the genetically induced pre-diabetic condition, and cases of diabetes, as evidenced by an increase in mitochondrial ROS production, changes in mitochondrial membrane potential, and swollen mitochondria with unfolded cristae in mitochondria [34, 37,38,39,40]. In this study, we have found that after 14 weeks on a high fat diet, all the rats developed brain mitochondrial dysfunction as evidenced by increasing ROS production, membrane depolarization, and swelling. In the brain, the mitochondrial caveat is the very simple approach used to isolate brain mitochondria via differential centrifugation, as it limits the ability to know the source of the mitochondria, and nothing was employed to release synaptosomal mitochondria. In this study, however, isolated brain mitochondria from a whole brain were used to determine brain mitochondrial function. Therefore, targeting synaptosomal mitochondria might be better for future studies. In addition to brain mitochondrial dysfunction, the pre-diabetic rats also exhibited an increase in mitochondrial fission in the brain as indicated by high expression of activated Drp1 level. Previous studies found that Drp1, Aβ, and phosphorylated tau had a gradually increasing association with prediabetes, which exacerbated Drp1 activity and resulted in severe fragmentation of the mitochondria [45, 46]. Likewise, the accumulation of Aβ and hyperphosphorylated tau in the brain is attributed to greater oxidative stress, decreased ATP synthesis and potential of the mitochondrial membrane, disrupted mitochondrial calcium control, increased mitochondrial apoptotic factor secretion, and upregulated mitochondrial fission [47, 48]. Although excessive mitochondrial fission-induced fragmentation is a significant early event in the development of AD after extended exposure to HFD intake, blocking excessive Drp1-mediated mitochondrial fission may be an effective treatment route for HFD-induced prediabetes and AD. Interestingly, Baek SH and colleagues (2017) demonstrated that Drp1 inhibition reduces mitochondrial fragmentation, mitochondrial membrane potential loss, ROS generation, ATP decrease, Aβ deposition, and synaptic depression, resulting in enhanced learning and memory in the brain of an Alzheimer’s disease model [49]. In this study, we also found that inhibition of Drp1 using Mdivi-1 exerted neuroprotective effects via attenuation of brain mitochondrial dysfunction and reduction in excessive mitochondrial fission and fragmentation-mediated brain impairments, resulting in improved cognitive function and AD-like pathology in HFD-induced prediabetes. As a result, Drp1 may be crucial in Aβ-mediated and AD-related neuropathology, as well as cognitive impairment in HFD-induced prediabetes.
In addition to the changes in fission, a reduction in brain mitochondrial fusion was observed in our prediabetic models via the downregulation of Mfn2 protein. Reduced mitochondrial fusion and Mfn2 levels in adipocytes have been linked to increased fat accumulation [50]. In accordance with this, the knocking down of Mfn2 in adipocytes in adult mice resulted in systemic metabolic disorders comparable to the high fat diet [50]. Mfn2 knockout in adipocytes, on the other hand, reduced cell size but increased fat storage, indicating that Mfn2 may play a role in regulating adipocyte proliferation. Several investigations have consistently identified decreased expression of major GTPases (e.g., Mfn2) involved in mitochondrial fusion in the brains of Alzheimer’s disease patients, suggesting that mitochondrial fragmentation occurs in vulnerable neurons in the Alzheimer’s brain, largely attributable to defective mitochondrial fusion [45, 51,52,53]. In this study, we have reported for the first time regarding an intervention with M1 to promote mitochondrial fusion. M1 effectively rescued mitochondrial fragmentation via the enhancement of Mfn2 expression, leading to improvement in mitochondrial function and overall cognitive outcomes. However, we did not find any differences in Opa1 expression between all groups. This could be due to the degree of development of brain impairment consequential to long-term HFD consumption or insufficient dosage of the M1 treatment; thus, future study is needed to test these hypotheses. Regarding the mitochondria in specific brain cell populations, Pysh JJ (1972) discovered persistent changes in mitochondrial structure, size, and concentration among several neuronal and neuroglial cells [54]. A systematic qualitative and quantitative electron microscopic comparison of mitochondrial structure and content in neurons and neuroglia from different regions of the central nervous system revealed that the crystal volume fraction of mitochondria (crystal packing density) was highest in choroid, intermediate in neurons, and lowest in astrocytes and oligodendrocytes, implying that oxidative enzyme concentrations may differ significantly between these three mitochondrial types. The mitochondrial crystal is dense aggregations of macromolecular protein units which either form a periodic inner substructure or have a geometric shape, or both inside the mitochondria [55]. Mitochondrial crystalline inclusions are frequently found in mitochondrial myopathies, such as cancer or ischemia [56]. It has been shown that protein crystals function as storage structures in highly metabolic active tissues or conditions of reduced metabolism and starvation [55]. Moreover, differences in mitochondrial crystal packing density, which can be distinguished by shape, size, and pattern, are associated with variations in mitochondrial volume fractions of cells and should indicate significant diversity in oxidative metabolism capability across the diverse neurons and neuroglia of the central nervous system [54]. It is proposed that variations in mitochondrial volume fractions of cells, together with differences in mitochondrial crystal packing density, should indicate significant diversity in oxidative metabolism capability across the diverse neurons and neuroglia of the central nervous system. However, future studies are needed to investigate the specific brain cell populations regarding the modulations in mitochondrial size (a proxy for mitochondrial dynamics) at the cellular level.
According to cell-type-specific profiling of brain mitochondria, Fecher et al. (2019) demonstrated that mitochondria’s cell-type-specific molecular diversity not only supports homeostatic demands by conserving fundamental functions in cells with varying geometries, but also provides mitochondria with specific properties that contribute to a specific cell type’s different function in the healthy brain and selective vulnerability during disease [57]. Proteomic studies assume that astrocytic mitochondria metabolize long-chain fatty acids more efficiently than neuronal mitochondria among the three major cerebellar cell types (Purkinje cells, granule cells, and astrocytes), implying differences in beta-oxidation, calcium buffering, and endoplasmic reticulum-mitochondria interaction [57]. Therefore, future studies targeting the effects of mitochondrial dynamic modulators on cell-type-specific profiling of brain mitochondria, particularly mitochondria in astrocytes, are needed.
Several investigations have found that brain apoptosis occurs in conjunction with prolonged HFD-induced mitochondrial dysfunction in the brain, leading to neurodegenerative diseases [38, 40]. The essential components are divided into two protein families: caspase enzymes and the Bcl-2 family [58]. Caspase enzymes function in a cascade, caspase3 being the most significant member of this family, playing an essential role in the death of neurons in the central nervous system after HFD feeding. The Bcl-2 family is a group of cytoplasmic proteins that control apoptosis. There are two main groups of this family of proteins, Bcl-2 (inhibit apoptosis) and Bax (activate apoptosis) [38, 59]. Activation of Bax along with decreased Bcl-2 expression was observed in brain tissue from rats with the pre-diabetic condition and could promote brain apoptosis through the triggering of the caspase cascades (i.e., cleaved caspase3) [38, 59]. As a result, apoptotic-mediated neuronal death has been identified as one underlying mechanism for cognitive impairment and other neurodegenerative diseases [60]. Fortunately, we found that Mdivi-1 and M1 treatment successfully prevented brain apoptosis subsequent to HFD-induced prediabetes.
Additionally, although the protective effects of Mdivi-1 and M1 on the expression levels of Aβ peptides for plaques and tau for tangles, markers of Alzheimer’s disease, support the link between HFD and brain pathologies, additional research into AD behavioral signs should be studied and discussed to determine the functional outcomes following intervention. In this study, the OFT was performed to determine exploratory behavior in response to anxiety-provoking conditions for all rats before cognitive testing, since stressful experiences have a powerful impact on cognitive function and can lead to both short- and long-term behavioral alterations [61]. The OFT results, including the total travel distance, mean speed without resting, and time spent in the center, confirmed that all animals were not associated with the aggravation of stress in response to anxiety-provoking conditions, suggesting that the beneficial effects of both Mdivi-1 and M1 could directly rescue cognitive impairment without affecting anxiety-related and exploratory behaviors in HFD-induced prediabetic models. However, the present study has the limitation that for a neuro focused report, the lack of any histology limits interpretation of the results as it is unclear what changed the behaviors. Therefore, the role of mitochondrial dynamic modulators on brain histology needs to be elucidated in a future study.
The NOL is a widely applicable test that assesses hippocampal-dependent spatial memory, which is an essential structure for memory formation in both humans and rodents [62]. The hippocampus is essential for declarative memory, which involves relational representations, but not for procedural memory, dependent on the brain’s motor centers [62]. Since the hippocampal memory function is so acutely sensitive to disruption, it has been the focus of research in a wide variety of fields of neuroscience [63]. Hippocampal impairment is related to several adverse issues ranging from prolonged stress and aging to seizures and stroke [64,65,66]. Moreover, HFD-induced obesity has previously been shown to decline cognitive function via impairing the NOL parameters [35, 67]. Numerous interventions, on the other hand, such as pharmacological strategies promote hippocampal function [35, 67]. In this study, we found that pharmacological inhibition of mitochondrial fission (Mdivi-1) or promotion of fusion (M1) effectively restored NOL-related hippocampal function in obese rats, thus rebalancing mitochondrial dynamics could be a putative strategy for neuroprotection against obesity. As a result, hippocampus memory testing using NOL may provide insight on the cellular and molecular mechanisms of memory and also the influence of various environmental modifications on hippocampal function.
Only “NOL” which tightly depends on adult hippocampal neurogenesis [62, 68] was used as cognitive test in our study. Other cognitive tests such as novel object recognition (NOR) should be used to confirm the cognitive impairment of this model. It has been shown that the NOR was used to evaluate non-spatial learning of object identity, which relies on multiple brain regions [62]. However, this study aimed to determine the effects of mitochondrial dynamic modulators on hippocampus-dependent cognitive function in obese rats. Therefore, we have performed only the NOL test, which was commonly used in several previous studies [35, 67] and has been primarily developed for the evaluation of spatial learning, which relies heavily on hippocampal activity [62]. Since the NOL results were only reported in this study, determination of non-hippocampus-dependent as the object recognition test is still further required to reveal the function and relative health of specific brain regions involved in memory.
Although Mdivi-1 and M1 at the doses of 1.2 and 2 mg/kg, respectively, have been noted as cardioprotective pharmacological modulators of mitochondrial dynamics against cardiac complications in HFD-induced prediabetes [10], their protective roles in the brain are still unknown. In this study, we demonstrated that Mdivi-1 at 1.2 mg/kg effectively protected the brain injury induced by long-term HFD consumption. However, there are some studies that reported the side effects of Mdivi-1 in various pathological conditions that need to be mentioned. Mdivi-1 has been shown to increase toxic effects in a mouse model of Parkinson’s disease [69]. Moreover, Mdivi-1 treatment altered the expression of oxidative phosphorylation (OXPHOS) complex proteins and altered the expression of mitochondrial serine/proteases, resulting in increased superoxide production [70]. Impaired autophagy flux was also observed following Mdivi-1 treatment in cardiomyocytes, suggesting that Mdivi-1 mediated inhibition of macro-autophagy. Additional effects of Mdivi-1 have been reported to reversibly inhibit mitochondrial Complex I-dependent O2 consumption and reverse electron transfer-mediated ROS production at concentrations used to target mitochondrial fission. Remarkably, Mdivi-1-induced respiratory impairment occurs without mitochondrial elongation and is not replicated by Drp1 deletion, implying that Mdivi-1 is not a specific Drp1 inhibitor [69]. In addition to Mdivi-1, Hydrazone M1 or mitochondrial fusion promoter-M1 is the most active cell-permeable phenylhydrazone compound that effectively decreased the mitochondrial fragmentation [71]. M1 was also identified as the most active compound in rescuing fusion in Mfn1 or Mfn2 knockout mouse embryonic fibroblasts (MEFs). In addition, M1 treatment exerted neuroprotective benefits against cardiac I/R injury via restoring Mfn2 protein, reducing brain mitochondrial dysfunction, BBB breakdown, macrophage infiltration, apoptosis, and Alzheimer-related proteins [26]. However, references to brain mitochondrial functions are still lacking, and proof of effects of M1 treatment on brain mitochondrial morphology in this context should be provided. Therefore, future studies are needed to investigate the pharmacological properties and long-term efficacies of both drugs.
Conclusion
Our findings demonstrated that prolonged HFD consumption led to the development of prediabetes and a decrease in brain mitochondrial function and mitochondrial dynamic imbalance, leading to brain apoptosis and cognitive decline. Modulation of mitochondrial dynamics with either a fission inhibitor (Mdivi-1) or a fusion promoter (M1) exerted similar neuroprotective effects against HFD-induced prediabetes via improving metabolic parameters, balancing mitochondrial dynamics, and reducing mitochondrial dysfunction, resulting in a gradual increase in cognitive function. These findings indicate real possibilities for novel therapeutic strategies for diabetes-associated cognitive impairment.
Data Availability
Not applicable.
Code Availability
Not applicable.
References
Malik VS, Willet WC, Hu FB (2020) Nearly a decade on — trends, risk factors and policy implications in global obesity. Nat Rev Endocrinol 16(11):615–616. https://doi.org/10.1038/s41574-020-00411-y
Haththotuwa RN, Wijeyaratne CN, Senarath U (2020) Chapter 1 - worldwide epidemic of obesity. In: Mahmood TA, Arulkumaran S, Chervenak FA (eds) Obesity and Obstetrics (Second Edition). Elsevier, pp 3–8.:https://doi.org/10.1016/B978-0-12-817921-5.00001-1
Riccardi G, Giacco R, Rivellese AA (2004) Dietary fat, insulin sensitivity and the metabolic syndrome. Clin Nutr 23(4):447–456. https://doi.org/10.1016/j.clnu.2004.02.006
Apaijai N, Pintana H, Chattipakorn SC, Chattipakorn N (2012) Cardioprotective effects of metformin and vildagliptin in adult rats with insulin resistance induced by a high-fat diet. Endocrinology 153(8):3878–3885. https://doi.org/10.1210/en.2012-1262
Pipatpiboon N, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2012) PPARgamma agonist improves neuronal insulin receptor function in hippocampus and brain mitochondria function in rats with insulin resistance induced by long term high-fat diets. Endocrinology 153 (1):329-338.:https://doi.org/10.1210/en.2011-1502
Pratchayasakul W, Kerdphoo S, Petsophonsakul P, Pongchaidecha A, Chattipakorn N, Chattipakorn SC (2011) Effects of high-fat diet on insulin receptor function in rat hippocampus and the level of neuronal corticosterone. Life Sci 88 (13–14):619–627.:https://doi.org/10.1016/j.lfs.2011.02.003
Petersen KF, Befroy D, Dufour S, Dziura J, Ariyan C, Rothman DL, DiPietro L, Cline GW, Shulman GI (2003) Mitochondrial dysfunction in the elderly: possible role in insulin resistance. Science 300(5622):1140–1142. https://doi.org/10.1126/science.1082889
Maneechote C, Palee S, Kerdphoo S, Jaiwongkam T, Chattipakorn SC, Chattipakorn N (2021) Modulating mitochondrial dynamics attenuates cardiac ischemia-reperfusion injury in prediabetic rats. Acta Pharmacol Sin.:https://doi.org/10.1038/s41401-021-00626-3
Maneechote C, Palee S, Kerdphoo S, Jaiwongkam T, Chattipakorn SC, Chattipakorn N (2020) Pharmacological inhibition of mitochondrial fission attenuates cardiac ischemia-reperfusion injury in pre-diabetic rats. Biochem Pharmacol 182:114295.:https://doi.org/10.1016/j.bcp.2020.114295
Maneechote C, Palee S, Apaijai N, Kerdphoo S, Jaiwongkam T, Chattipakorn SC, Chattipakorn N (2019) Mitochondrial dynamic modulation exerts cardiometabolic protection in obese insulin-resistant rats. Clin Sci (Lond) 133(24):2431–2447. https://doi.org/10.1042/cs20190960
Chunchai T, Keawtep P, Arinno A, Saiyasit N, Prus D, Apaijai N, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2019) N-acetyl cysteine, inulin and the two as a combined therapy ameliorate cognitive decline in testosterone-deprived rats. Aging 11(11):3445–3462. https://doi.org/10.18632/aging.101989
Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2011) Effects of estrogen in preventing neuronal insulin resistance in hippocampus of obese rats are different between genders. Life Sci 89 (19–20):702–707.:https://doi.org/10.1016/j.lfs.2011.08.011
Pintana H, Pratchayasakul W, Sa-nguanmoo P, Pongkan W, Tawinvisan R, Chattipakorn N, Chattipakorn SC (2016) Testosterone deprivation has neither additive nor synergistic effects with obesity on the cognitive impairment in orchiectomized and/or obese male rats. Metabolism 65(2):54–67. https://doi.org/10.1016/j.metabol.2015.10.015
Suen DF, Norris KL, Youle RJ (2008) Mitochondrial dynamics and apoptosis. Genes Dev 22(12):1577–1590. https://doi.org/10.1101/gad.1658508
Chan DC (2006) Mitochondrial fusion and fission in mammals. Annu Rev Cell Dev Biol 22:79–99. https://doi.org/10.1146/annurev.cellbio.22.010305.104638
Leduc-Gaudet J-P, Reynaud O, Chabot F, Mercier J, Andrich DE, St-Pierre DH, Gouspillou G (2018) The impact of a short-term high-fat diet on mitochondrial respiration, reactive oxygen species production, and dynamics in oxidative and glycolytic skeletal muscles of young rats. Physiol Rep 6 (4):e13548.:https://doi.org/10.14814/phy2.13548
Ong SB, Kalkhoran SB, Hernandez-Resendiz S, Samangouei P, Ong SG, Hausenloy DJ (2017) Mitochondrial-shaping proteins in cardiac health and disease - the long and the short of it! Cardiovasc Drugs Ther 31(1):87–107. https://doi.org/10.1007/s10557-016-6710-1
Scott I, Youle RJ (2010) Mitochondrial fission and fusion. Essays Biochem 47:85–98. https://doi.org/10.1042/bse0470085
Gao AW, Cantó C, Houtkooper RH (2014) Mitochondrial response to nutrient availability and its role in metabolic disease. EMBO Mol Med 6(5):580–589. https://doi.org/10.1002/emmm.201303782
Flippo KH, Strack S (2017) Mitochondrial dynamics in neuronal injury, development and plasticity. J Cell Sci 130(4):671–681. https://doi.org/10.1242/jcs.171017
Rigotto G, Basso E (2019) Mitochondrial dysfunctions: a thread sewing together Alzheimer's disease, diabetes, and obesity. Oxid Med Cell Longev 2019:7210892.:https://doi.org/10.1155/2019/7210892
Khan MSH, Hegde V (2020) Obesity and diabetes mediated chronic inflammation: a potential biomarker in Alzheimer’s disease. J Pers Med 10(2):42. https://doi.org/10.3390/jpm10020042
Zhang X, Huang W, Shao Q, Yang Y, Xu Z, Chen J, Zhang X, Ge X (2020) Drp1, a potential therapeutic target for Parkinson's disease, is involved in olfactory bulb pathological alteration in the rotenone-induced rat model. Toxicol Lett 325:1-13.:https://doi.org/10.1016/j.toxlet.2020.02.009
Zhang Y, Rui T, Luo C, Li Q (2021) Mdivi-1 alleviates brain damage and synaptic dysfunction after intracerebral hemorrhage in mice. Exp Brain Res.:https://doi.org/10.1007/s00221-021-06089-6
Mishra A, Singh S, Tiwari V, Bano S, Shukla S (2020) Dopamine D1 receptor agonism induces dynamin related protein-1 inhibition to improve mitochondrial biogenesis and dopaminergic neurogenesis in rat model of Parkinson's disease. Behav Brain Res 378:112304.:https://doi.org/10.1016/j.bbr.2019.112304
Surinkaew P, Apaijai N, Sawaddiruk P, Jaiwongkam T, Kerdphoo S, Chattipakorn N, Chattipakorn SC (2020) Mitochondrial fusion promoter alleviates brain damage in rats with cardiac ischemia/reperfusion injury. J Alzheimers Dis 77(3):993–1003. https://doi.org/10.3233/jad-200495
Ruiz A, Alberdi E, Matute C (2018) Mitochondrial division inhibitor 1 (mdivi-1) protects neurons against excitotoxicity through the modulation of mitochondrial function and intracellulAr Ca2+ signaling. Front Mol Neurosci 11 (3).:https://doi.org/10.3389/fnmol.2018.00003
Cassidy-Stone A, Chipuk JE, Ingerman E, Song C, Yoo C, Kuwana T, Kurth MJ, Shaw JT et al (2008) Chemical inhibition of the mitochondrial division dynamin reveals its role in Bax/Bak-dependent mitochondrial outer membrane permeabilization. Dev Cell 14(2):193–204. https://doi.org/10.1016/j.devcel.2007.11.019
Zhang N, Wang S, Li Y, Che L, Zhao Q (2013) A selective inhibitor of Drp1, mdivi-1, acts against cerebral ischemia/reperfusion injury via an anti-apoptotic pathway in rats. Neurosci Lett 535(104):109. https://doi.org/10.1016/j.neulet.2012.12.049
Li Y, Wang P, Wei J, Fan R, Zuo Y, Shi M, Wu H, Zhou M et al (2015) Inhibition of Drp1 by Mdivi-1 attenuates cerebral ischemic injury via inhibition of the mitochondria-dependent apoptotic pathway after cardiac arrest. Neuroscience 311(67):74. https://doi.org/10.1016/j.neuroscience.2015.10.020
Apaiajai N, Chunchai T, Jaiwongkam T, Kerdphoo S, Chattipakorn SC, Chattipakorn N (2018) Testosterone deprivation aggravates left-ventricular dysfunction in male obese insulin-resistant rats via impairing cardiac mitochondrial function and dynamics proteins. Gerontol 64(4):333–343. https://doi.org/10.1159/000487188
Tunapong W, Apaijai N, Yasom S, Tanajak P, Wanchai K, Chunchai T, Kerdphoo S, Eaimworawuthikul S et al (2017) Chronic treatment with prebiotics, probiotics and synbiotics attenuated cardiac dysfunction by improving cardiac mitochondrial dysfunction in male obese insulin-resistant rats. Eur J Nutr.:https://doi.org/10.1007/s00394-017-1482-3
Shwe T, Bo-Htay C, Ongnok B, Chunchai T, Jaiwongkam T, Kerdphoo S, Kumfu S, Pratchayasakul W et al (2021) Hyperbaric oxygen therapy restores cognitive function and hippocampal pathologies in both aging and aging-obese rats. Mech Ageing Dev 195:111465.:https://doi.org/10.1016/j.mad.2021.111465
Jinawong K, Apaijai N, Wongsuchai S, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2020) Necrostatin-1 mitigates cognitive dysfunction in prediabetic rats with no alteration in insulin sensitivity. Diabetes 69(7):1411. https://doi.org/10.2337/db19-1128
Jinawong K, Apaijai N, Wongsuchai S, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2020) Necrostatin-1 mitigates cognitive dysfunction in prediabetic rats with no alteration in insulin sensitivity. Diabetes 69(7):1411–1423. https://doi.org/10.2337/db19-1128
Clewer AG, Scarisbrick DH (2001) practical statistics and experimental design for plant and crop science. In, 2001
Saiyasit N, Chunchai T, Prus D, Suparan K, Pittayapong P, Apaijai N, Pratchayasakul W, Sripetchwandee J et al (2020) Gut dysbiosis develops before metabolic disturbance and cognitive decline in high-fat diet-induced obese condition. Nutrition 69:110576.:https://doi.org/10.1016/j.nut.2019.110576
Sa-Nguanmoo P, Tanajak P, Kerdphoo S, Jaiwongkam T, Pratchayasakul W, Chattipakorn N, Chattipakorn SC (2017) SGLT2-inhibitor and DPP-4 inhibitor improve brain function via attenuating mitochondrial dysfunction, insulin resistance, inflammation, and apoptosis in HFD-induced obese rats. Toxicol Appl Pharmacol 333(43):50. https://doi.org/10.1016/j.taap.2017.08.005
Chunchai T, Thunapong W, Yasom S, Wanchai K, Eaimworawuthikul S, Metzler G, Lungkaphin A, Pongchaidecha A et al (2018) Decreased microglial activation through gut-brain axis by prebiotics, probiotics, or synbiotics effectively restored cognitive function in obese-insulin resistant rats. J Neuroinflammation 15(1):11. https://doi.org/10.1186/s12974-018-1055-2
Pratchayasakul W, Thongnak LO, Chattipakorn K, Lungaphin A, Pongchaidecha A, Satjaritanun P, Jaiwongkam T, Kerdphoo S et al (2018) Atorvastatin and insulin equally mitigate brain pathology in diabetic rats. Toxicol Appl Pharmacol 342(79):85. https://doi.org/10.1016/j.taap.2018.01.021
Putti R, Sica R, Migliaccio V, Lionetti L (2015) Diet impact on mitochondrial bioenergetics and dynamics. Front Physiol 6:109. https://doi.org/10.3389/fphys.2015.00109
Jheng HF, Tsai PJ, Guo SM, Kuo LH, Chang CS, Su IJ, Chang CR, Tsai YS (2012) Mitochondrial fission contributes to mitochondrial dysfunction and insulin resistance in skeletal muscle. Mol Cell Biol 32(2):309–319. https://doi.org/10.1128/MCB.05603-11
Sartorius T, Peter A, Schulz N, Drescher A, Bergheim I, Machann J, Schick F, Siegel-Axel D et al (2014) Cinnamon extract improves insulin sensitivity in the brain and lowers liver fat in mouse models of obesity. PLoS One 9 (3):e92358.:https://doi.org/10.1371/journal.pone.0092358
Tong M, de la Monte SM (2009) Mechanisms of ceramide-mediated neurodegeneration. J Alzheimers Dis 16(4):705–714. https://doi.org/10.3233/jad-2009-0983
Manczak M, Calkins MJ, Reddy PH (2011) Impaired mitochondrial dynamics and abnormal interaction of amyloid beta with mitochondrial protein Drp1 in neurons from patients with Alzheimer’s disease: implications for neuronal damage. Hum Mol Genet 20(13):2495–2509. https://doi.org/10.1093/hmg/ddr139
Manczak M, Reddy PH (2012) Abnormal interaction between the mitochondrial fission protein Drp1 and hyperphosphorylated tau in Alzheimer’s disease neurons: implications for mitochondrial dysfunction and neuronal damage. Hum Mol Genet 21(11):2538–2547. https://doi.org/10.1093/hmg/dds072
Yao J, Du H, Yan S, Fang F, Wang C, Lue LF, Guo L, Chen D et al (2011) Inhibition of amyloid-beta (Abeta) peptide-binding alcohol dehydrogenase-Abeta interaction reduces Abeta accumulation and improves mitochondrial function in a mouse model of Alzheimer’s disease. J Neurosci 31(6):2313–2320. https://doi.org/10.1523/jneurosci.4717-10.2011
Cha MY, Han SH, Son SM, Hong HS, Choi YJ, Byun J, Mook-Jung I (2012) Mitochondria-specific accumulation of amyloid β induces mitochondrial dysfunction leading to apoptotic cell death. PLoS One 7 (4):e34929.:https://doi.org/10.1371/journal.pone.0034929
Baek SH, Park SJ, Jeong JI, Kim SH, Han J, Kyung JW, Baik SH, Choi Y et al (2017) Inhibition of Drp1 ameliorates synaptic depression, Aβ deposition, and cognitive impairment in an Alzheimer’s disease model. J Neurosci 37(20):5099–5110. https://doi.org/10.1523/jneurosci.2385-16.2017
Mancini G, Pirruccio K, Yang X, Blüher M, Rodeheffer M, Horvath TL (2019) Mitofusin 2 in mature adipocytes controls adiposity and body weight. Cell Rep 26 (11):2849–2858.e2844.:https://doi.org/10.1016/j.celrep.2019.02.039
Calkins MJ, Manczak M, Mao P, Shirendeb U, Reddy PH (2011) Impaired mitochondrial biogenesis, defective axonal transport of mitochondria, abnormal mitochondrial dynamics and synaptic degeneration in a mouse model of Alzheimer’s disease. Hum Mol Genet 20(23):4515–4529. https://doi.org/10.1093/hmg/ddr381
Wang X, Su B, Lee HG, Li X, Perry G, Smith MA, Zhu X (2009) Impaired balance of mitochondrial fission and fusion in Alzheimer’s disease. J Neurosci 29(28):9090–9103. https://doi.org/10.1523/jneurosci.1357-09.2009
Jiang S, Nandy P, Wang W, Ma X, Hsia J, Wang C, Wang Z, Niu M et al (2018) Mfn2 ablation causes an oxidative stress response and eventual neuronal death in the hippocampus and cortex. Mol Neurodegener 13(1):5. https://doi.org/10.1186/s13024-018-0238-8
Pysh JJ, Khan T (1972) Variations in mitochondrial structure and content of neurons and neuroglia in rat brain: an electron microscopic study. Brain Res 36(1):1–18. https://doi.org/10.1016/0006-8993(72)90762-7
Nürnberger S, Rentenberger C, Thiel K, Schädl B, Grunwald I, Ponomarev I, Marlovits S, Meyer C et al (2017) Giant crystals inside mitochondria of equine chondrocytes. Histochem Cell Biol 147(5):635–649. https://doi.org/10.1007/s00418-016-1516-6
Farrants GW, Hovmöller S, Stadhouders AM (1988) Two types of mitochondrial crystals in diseased human skeletal muscle fibers. Muscle Nerve 11(1):45–55. https://doi.org/10.1002/mus.880110109
Fecher C, Trovò L, Müller SA, Snaidero N, Wettmarshausen J, Heink S, Ortiz O, Wagner I et al (2019) Cell-type-specific profiling of brain mitochondria reveals functional and molecular diversity. Nat Neurosci 22(10):1731–1742. https://doi.org/10.1038/s41593-019-0479-z
Sripetchwandee J, Chattipakorn N, Chattipakorn SC (2018) Links between obesity-induced brain insulin resistance, brain mitochondrial dysfunction, and dementia. Front Endocrinol (Lausanne) 9:496.:https://doi.org/10.3389/fendo.2018.00496
Nuzzo D, Picone P, Baldassano S, Caruana L, Messina E, Marino Gammazza A, Cappello F, Mulè F et al (2015) Insulin resistance as common molecular denominator linking obesity to Alzheimer’s disease. Curr Alzheimer Res 12(8):723–735. https://doi.org/10.2174/1567205012666150710115506
Ghavami S, Shojaei S, Yeganeh B, Ande SR, Jangamreddy JR, Mehrpour M, Christoffersson J, Chaabane W et al (2014) Autophagy and apoptosis dysfunction in neurodegenerative disorders. Prog Neurobiol 112:24-49.:https://doi.org/10.1016/j.pneurobio.2013.10.004
Sturman O, Germain PL, Bohacek J (2018) Exploratory rearing: a context- and stress-sensitive behavior recorded in the open-field test. Stress 21(5):443–452. https://doi.org/10.1080/10253890.2018.1438405
Denninger JK, Smith BM, Kirby ED (2018) Novel object recognition and object location behavioral testing in mice on a budget. J Vis Exp (141).:https://doi.org/10.3791/58593
Bartsch T, Wulff P (2015) The hippocampus in aging and disease: from plasticity to vulnerability. Neuroscience 309(1):16. https://doi.org/10.1016/j.neuroscience.2015.07.084
Smith BM, Yao X, Chen KS, Kirby ED (2018) A larger social network enhances novel object location memory and reduces hippocampal microgliosis in aged mice. Front Aging Neurosci 10:142. https://doi.org/10.3389/fnagi.2018.00142
Garthe A, Roeder I, Kempermann G (2016) Mice in an enriched environment learn more flexibly because of adult hippocampal neurogenesis. Hippocampus 26(2):261–271. https://doi.org/10.1002/hipo.22520
Chieffi S, Messina G, Villano I, Messina A, Esposito M, Monda V, Valenzano A, Moscatelli F et al (2017) Exercise influence on hippocampal function: possible involvement of orexin-A. Front Physiol 8:85.:https://doi.org/10.3389/fphys.2017.00085
Saiyasit N, Chunchai T, Apaijai N, Pratchayasakul W, Sripetchwandee J, Chattipakorn N, Chattipakorn SC (2020) Chronic high-fat diet consumption induces an alteration in plasma/brain neurotensin signaling, metabolic disturbance, systemic inflammation/oxidative stress, brain apoptosis, and dendritic spine loss. Neuropeptides 82:102047.:https://doi.org/10.1016/j.npep.2020.102047
Cruz-Sanchez A, Dematagoda S, Ahmed R, Mohanathaas S, Odenwald N, Arruda-Carvalho M (2020) Developmental onset distinguishes three types of spontaneous recognition memory in mice. Sci Rep 10(1):10612. https://doi.org/10.1038/s41598-020-67619-w
Bordt EA, Clerc P, Roelofs BA, Saladino AJ, Tretter L, Adam-Vizi V, Cherok E, Khalil A et al (2017) The putative Drp1 inhibitor mdivi-1 is a reversible mitochondrial complex I inhibitor that modulates reactive oxygen species. Dev Cell 40 (6):583–594.e586.:https://doi.org/10.1016/j.devcel.2017.02.020
Aishwarya R, Alam S, Abdullah CS, Morshed M, Nitu SS, Panchatcharam M, Miriyala S, Kevil CG, Bhuiyan MS (2020) Pleiotropic effects of mdivi-1 in altering mitochondrial dynamics, respiration, and autophagy in cardiomyocytes. Redox Biol 36:101660.:https://doi.org/10.1016/j.redox.2020.101660
Wang D, Wang J, Bonamy GM, Meeusen S, Brusch RG, Turk C, Yang P, Schultz PG (2012) A small molecule promotes mitochondrial fusion in mammalian cells. Angew Chem Int Ed Engl 51(37):9302–9305. https://doi.org/10.1002/anie.201204589
Acknowledgements
We wish to thank Siripong Palee, Thidarat Jaiwongkam, and Sasiwan Kerdphoo for their laboratory assistance.
Funding
This work was supported by the Senior Research Scholar Grant from the National Research Council of Thailand (S.C.C.), the NSTDA Research Chair grant from the National Science and Technology Development Agency Thailand (N.C.), the Chiang Mai University Center of Excellence Award (N.C.), the National Research Council of Thailand, Fundamental Fund 2022, Chiang Mai University (C.M.), and the National Research Council of Thailand (C.M.).
Author information
Authors and Affiliations
Contributions
C.M. performed the experiments, analyzed the data, and wrote the manuscript. T.C., N.A. performed the experiments. N.C. designed the study, contributed to the discussion, and edited the manuscript. S.C.C. designed the study, analyzed the data, contributed to the discussion, and edited and finalized the manuscript.
Corresponding author
Ethics declarations
Ethics Approval
The protocols were approved by the Institutional Animal Care and Use Committee of the Faculty of Medicine, Chiang Mai University, Thailand (Permit No. 34/2561) and were performed at the Cardiac Electrophysiology Research and Training Center, Faculty of Medicine, Chiang Mai University, Chiang Mai, Thailand.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Maneechote, C., Chunchai, T., Apaijai, N. et al. Pharmacological Targeting of Mitochondrial Fission and Fusion Alleviates Cognitive Impairment and Brain Pathologies in Pre-diabetic Rats. Mol Neurobiol 59, 3690–3702 (2022). https://doi.org/10.1007/s12035-022-02813-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-022-02813-7