Abstract
The standard pharmacological treatment of the major depressive disorder (MDD) is still grounded in a monoaminergic approach. Consequently, antidepressant treatments pursue to heighten serotonergic and noradrenergic neurotransmissions. Thus, the aim of this study was to assess the impact of exposure to a well-characterized animal model, the chronic mild stress (CMS) on serotonin (5-HT) and noradrenaline (NE) levels, and reuptake transporters and receptors in the frontal cortex (FC) of CMS-exposed rats. Moreover, considering the diverse pharmacological profiles of existing antidepressants and the large number of patients not responding to treatments, we have investigated whether generally utilized antidepressants can modulate their expression. Male Wistar rats were exposed to CMS and some of them treated with desipramine, escitalopram, or duloxetine. Possible changes in the described monoaminergic neurotransmission elements were evaluated. CMS induced differences in the expression of reuptake transporters and receptors involved in the monoaminergic neurotransmission pointing towards the weakening of their signaling. CMS antidepressant-treated rats showed an improvement of the monoaminergic tone, being desipramine and duloxetine more influential than escitalopram over noradrenergic elements and having the three antidepressant-tested effects on serotonergic transmission. In summary, there are molecular alterations on the monoaminergic neurotransmission in FC induced by CMS exposure. Besides, antidepressant treatments modulate the elements of these neurotransmission systems differentially.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Major depressive disorder (MDD) affects over 322 million people worldwide being one of the leading causes of disability with enormous personal, medical, and economic costs [1]. However, the etiology and pathophysiology of this disease are still unknown, although different hypotheses (not exclusive but complementary) have been proposed, trying to shed light on its mechanisms [2].
Near one-third of patients with MDD are treatment-resistant to the available drugs, whose majority is still based on the classic monoaminergic hypothesis. Consequently, current treatments try to enhance serotonergic and noradrenergic neurotransmission through actions on degradation enzymes (monoamine oxidase inhibitors—MAOIs), reuptake transporters (tricyclic antidepressants—TCAs—and selective reuptake inhibitors), receptors (multi-receptor agonists or antagonists), or on these last two elements simultaneously (serotonin partial agonist reuptake inhibitors—SPARIs) [3].
Serotonin (5-HT) is one traditional therapeutic target of study in MDD. Nevertheless, there is still controversy on the detailed implications of this complex receptor system and how to overcome the technical difficulties of drug development due to the heterogeneous distribution and functionalities of the different 5-HT receptor types. To date, seven families and 14 5-HT receptors have been described with different expression and functional implications depending on their cerebral location, molecular features, second messengers, and affinity for their ligands among other factors (Barnes et al., IUPHAR database). Within them, the 5-HT1/2/7 families have arisen as the most connected with depressive-like behavior and antidepressant effect [4].
Norepinephrine (NE) is other neurotransmitter classically involved in the development of depressive-like behaviors. There are α- and β-adrenoceptors and up to nine subtypes with different implications and affinities for their ligands [5]. Given their widely spread location throughout the central nervous system (CNS), including the frontal cortex (FC), it has been shown that noradrenergic signaling participates in many different processes, some of them intimately bounded to depression (e.g., stress and immune responses, memory consolidation, plasticity, and sleep regulation) [6].
New drugs designed for the treatment of depression aim to modulate serotonergic and noradrenergic transmissions acting on highly specific targets. Studies about the actual decrease on the monoamine metabolites in biological fluids and the CNS in mental diseases convey the idea that antidepressants might improve the monoaminergic transmission modifying the expression of monoamine receptors and reuptake transporters [7]. This can contribute to the fine regulation needed for their efficacy due to the serious side effects arising when monoamine signaling is deficient or overstimulated [8].
Antidepressants (ADs) might modulate other biological systems worth to study; antioxidant [9], anti-inflammatory [10], epigenetic [11], neurotrophic [12], and mitochondrial [13] actions have been already described for ADs [14].
There is a profuse volume of published studies dealing with serotonin and norepinephrine neurotransmissions and their modulation by ADs. Nevertheless, these investigations focus on some particular elements of these signaling systems and, given the cross-regulation among all of them, these previous approaches would be partially explaining some of the conflicting results obtained.
The first aim of this study was to evaluate the impact of exposure to a well-characterized multidimensional animal model, the chronic mild stress (CMS) on 5-HT and NE levels, as well as the expression of their respective reuptake transporters and receptors in the FC of rats. Besides, available antidepressants have heterogeneous pharmacological profiles and there is an important number of patients not responding to classical treatments. Thus, new molecular insights in the activity of classic ADs over the monoaminergic neurotransmission are essential to improve ADs design and make it more accurate, powerful, and with a better tolerance profile. Hence, the second aim of this study was to examine whether commonly used antidepressants can modulate the expression of the monoaminergic elements explored in the FC.
Materials and Methods
Animals
Male outbred Wistar Hannover rats (HsdRccHan:Wist, from Envigo, Spain) initially weighing 200–225 g were housed one per cage. Animals were maintained under standard conditions of temperature and humidity and in a 12-h light/dark cycle (lights on at 08:00 h) with free access to food and water. Rats were handled daily for the change of cage and bedding for 14 days before the beginning of the stress protocol. All experimental procedures adhered to the guidelines of the Animal Welfare Committee of the Universidad Complutense (PROEX421/15) following European legislation (2010/63/EU) and they were carried out in the Animal Facility CAI-UCM. Animal studies are reported in compliance with the ARRIVE guidelines and all efforts were made to minimize animal suffering and to reduce the number of animals used.
Experimental Groups
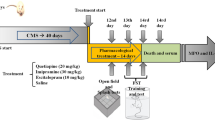
Animals which were randomly assigned to the following groups (n = 6–8 in each group) were used: (1) a control (animals were handled for few seconds once at 10:00 h) group (CT); (2) a control group with intraperitoneal injection (i.p.) of sterile saline (used as vehicle) injected daily for 7 days (CT+Veh); (3) a chronic mild stress (CMS) group; and (4) a CMS injected (i.p.) with vehicle (CMS+Veh) group (days 14–21).
For experiments involving the i.p. injection of ADs (from day 14 to day 21), three additional experimental groups were employed: (5) a CMS group injected with desipramine (CMS+Desip); (6) a CMS group injected with escitalopram (CMS+Escit); and (7) a CMS group injected with duloxetine (CMS+Dulox). See the “Pharmacological Tools” section for ADs-specific details.
Vehicle-injected groups did not differ from the same experimental groups without injection in any of the parameters analyzed, and their values have been pooled in all the figures.
Chronic Mild Stress (CMS) Protocol
The CMS protocol used was a modification of the one proposed by Willner [15]. Our group has previously used this CMS protocol showing that it induces a depressive-like behavior when analyzed by means of the modified forced swim test, sucrose test, splash test, and elevated plus maze test, as well as a response to the administration of the ADs here employed [9, 16, 17]. The protocol consists of a series of different stressors that were changed daily (two stressors/day), given in an unpredictable basis, for a period of 21 days. The stressors included the following: (a) food deprivation, (b) water deprivation, (c) cage tilting, (d) soiled cage, (e) grouped housing after a period of water deprivation, (f), stroboscopic illumination (150 flashes/min), and (g) intermittent illumination every 2 h.
Pharmacological Tools
The employed ADs (from Sigma-Aldrich, Spain) were the tricyclic antidepressant (TCA) Desipramine hydrochloride (D3900) (20 mg/kg, i.p.), the selective serotonin reuptake inhibitor (SSRI) Escitalopram oxalate (E4786) (15 mg/kg, i.p.), and the serotonin-norepinephrine reuptake inhibitor (SNRI) (S)-Duloxetine hydrochloride (SML0474) (15 mg/kg; i.p.).
In order to explore therapeutic effects of the drugs, we choose a protocol close to clinical reality: vehicle or ADs were administered during the last 7 days of the CMS protocol. The administered doses have shown antidepressant activity in rodents in previously published studies using similar protocols. The drugs employed are neither new nor experimental drugs; these are well-established ADs, widely used in preclinical studies and in the treatment of patients, and without effects on non-stressed animals. Accordingly, and in order to reduce the number and the suffering of animals following the 3Rs principles, we did not perform behavioral tests on these rats. The result that these tests would yield, that the CMS protocol induces a depressive-like behavior, and that treatment with canonical antidepressants (i.e., TCAs, SSRIs, and SNRIs) reverses the behavior induced by the stress protocol has been extensively published with these drugs and doses in this model [18, 19].
Tissue Samples
To avoid variations in corticosterone levels caused by the circadian rhythm, biological samples were always obtained at the same time of the day, namely between 3 and 4 p.m. Samples from CMS-exposed animals were taken immediately after day 21 of stress.
After terminal anesthesia using sodium pentobarbital (320 mg/kg i.p. Vetoquinol®, Spain; CN:570681.8), the brain was removed from the skull and frontal cortical areas were excised from the brain and frozen at − 80 °C until assayed.
Homogenization of the Samples
A widely utilized method that provides a high-purity cytosolic fraction, practically without nuclear contamination, was employed [20]. Briefly, FC was homogenized in 300 mL buffer [10 mmol/L N-2-hydroxyethylpiperazine-N-2-ethanesulfonic acid (pH 7.9); 1 mmol/L EDTA, 1 mmol/L EGTA, 10 mmol/L KCl, 1 mmol/L dithiothreitol, 0.5 mmol/L phenylmethylsulfonyl fluoride, 0.1 mg m/L aprotinin, 1 mg/mL leupeptin, 1 mg/mL Na-p-tosyll-lysinechloromethylketone, 5 mmol/L NaF, 1 mmol/L NaVO4, 0.5 mol/L sucrose, and 10 mmol/L Na2MoO4]. After 15 min, Nonidet P-40® (Roche, Mannheim, Germany) was added to reach a 0.5% concentration. The tubes were gently vortexed for 15 s, and nuclei were collected by centrifugation at 5000g for 5 min. Supernatants were considered as the cytosolic fraction. All steps of the fractionation were carried out at 4 °C.
Western Blot Analysis
To determine the expression levels of serotonin transporter (SERT) and norepinephrine transporter (NET), cytosolic extracts from FC samples were used (see previous section for details).
After adjusting protein levels (see the “Protein Assay” section) in the homogenates and mixing them with Laemmli sample buffer (Bio-Rad, Hercules, CA, USA), 20 mL (1 mg/mL) was loaded and the proteins were size-separated in 10% SDS-polyacrylamide gel electrophoresis (90 V).
After the gel electrophoresis, the membranes were blocked in 30 mL Tris-buffered saline containing 0.1% Tween 20 and 5% skim milk/BSA, then the membranes were incubated with specific primary antibodies against SERT (sc-1458, Santa Cruz Biotechnology, 1:500) and NET (sc-67,216, Santa Cruz Biotechnology, 1:750). After washing with a TBS-Tween solution, the membranes were incubated with the respective horseradish peroxidase-conjugated secondary antibodies for 90 min at room temperature and revealed by ECLTM-kit following the manufacturer’s instructions (Amersham Ibérica, RTN2236; Spain).
Blots were imaged using an Odyssey® Fc System (Li-COR Biosciences) and quantified by densitometry (NIH ImageJ® software). All densitometries are expressed in arbitrary units of optical density (O.D.). Several exposition times were analyzed to ensure linearity of the band intensities. Loading controls (blots shown in the respective figures) were β-actin (Sigma A5441).
Protein Assay
Protein levels were measured using Bradford method based on the principle of protein-dye binding.
PCR Analysis
Primer oligonucleotides for PCR were designed with the Primer3 tool [21]. Target specificity was checked by in silico PCR using the USCS GenomeBrowser [22] and Blast (NCBI) for cDNA and gDNA; only primer pairs with no unintended targets were selected (Table 1).
PCR analyses were carried out homogenizing frontal cortex in 600 mL of TRIZOL® reagent (Invitrogen, Life Technologies, CA, USA) in the TissueLyser LT (QUIAGEN®, Venlo, Netherlands). Frequency used was 50 oscillations per second for 5 min at 4 °C.
Total cytoplasmic RNA was prepared from samples following TRIZOL® datasheet; aliquots were converted to cDNA using random hexamer primers. Semi-quantitative changes in mRNA levels were estimated by real time-PCR (RT-PCR) using the following cycling conditions: 35 cycles of denaturation at 95 °C for 10 s, annealing at 58–63 °C for 15 s depending on the specific set of primers, and extension at 72 °C for 20 s. Reactions were carried out in the presence of SYBR green (Quantimix Easy Master Mix Biotools, B&M labs 10607-4154) in a 20-L reaction in a Rotor-Gene (Corbett Research, Mortlake, NSW, Australia). Relative mRNA concentrations were calculated from the take-off point of reactions using included software, and tubulin levels used to normalize data.
As some of target genes have only one exon, the intron-spanning primer design was impossible in these cases. For this reason, purity and impact of possible genomic DNA contamination were monitored using both RNA samples and ValidPrime™ protocol (TATAA Biocenter, Odinsgatan, Sweden) as control for genomic background.
Serotonin and Norepinephrine Brain Levels
Serotonin and norepinephrine levels in the FC tissue homogenate (see the “Homogenization of the Samples” section) were measured using commercially available ELISA kits (Labor Diagnostika Nord, Nordhorn, Germany) following the manufacturer’s instructions.
Chemicals and Statistical Analyses
Unless otherwise stated, the chemicals were from Sigma-Aldrich (Spain). Data are expressed as mean ± SEM and a one-way ANOVA with a Tukey post hoc test was employed for comparisons between groups. Data were analyzed using the Brown-Forsythe test to assess Gaussian distribution. In those cases in which the data did not follow a Gaussian distribution, a nonparametric ANOVA with a Kruskal-Wallis test followed by a Dunn’s post hoc test was performed. A p value < 0.05 was considered statistically significant.
Results
Effects of CMS and Antidepressant Treatments on the Whole Serotonin (5-HT) and Norepinephrine (NE) Levels in the FC
No differences were detected in 5-HT levels among all the experimental groups (one-way ANOVA F(4,33) = 1.598, p = 0.1980; Fig. 1a).
Effects of CMS and AD treatments on the whole serotonin (5-HT) and norepinephrine (NE) levels in the FC. No changes detected in the 5-HT levels after the CMS or the antidepressant treatments (a). The CMS did not modify the NE amount but desipramine decreased it (b). The vehicle-injected groups did not differ from the same experimental groups without injection, and their values have been pooled in the figure. Data are means ± SEM of 6–8 rats per group; ##p < 0.01 vs. CMS; $p < 0.01 vs. CMS+Desip; One-way ANOVA following Tukey post hoc test
Whole NE levels did not change after CMS, but desipramine decreased NE amount compared with the CMS and CMS+Escitalopram groups (one-way ANOVA-Tukey F(4,38) = 5.198, p = 0.0019; Fig. 1b).
Effects of CMS and Antidepressant Treatments on the Expression of Serotonin and Norepinephrine Transporters in the FC
CMS did not affect the serotonin transporter (SERT) protein expression in the FC. Desipramine and escitalopram treatments did not change the expression of the SERT but Duloxetine upregulated the SERT expression compared with the control and CMS+Desipramine groups (one-way ANOVA-Tukey F(4,36) = 5.349, p = 0.0017; Fig. 2a).
Effects of CMS and AD treatments on the protein expression of 5-HT and NE transporters in the FC. CMS did not affect the protein expression of the serotonin transporter (SERT) (a) and upregulated the expression of the norepinephrine transporter (NET) (b). Desipramine and escitalopram did not change the expression of the SERT but duloxetine increased it (a). The NE transporter (NET) expression was not affected by ADs (b). The vehicle-injected groups did not differ from the same experimental groups without injection, and their values have been pooled in the figure. The densitometric data of the band of interest were normalized by beta-actin. Blots were cropped (black lines) for improving the clarity and conciseness of the presentation. Data are means ± SEM of 6–8 rats per group; **p < 0.01 vs. control; $$p < 0.01 vs. CMS+Desip; One-way ANOVA following Tukey post hoc test. The values of NET (b) did not follow a Gaussian distribution; thus, a nonparametric ANOVA with a Kruskal-Wallis test followed by a Dunn’s post hoc test was performed
The CMS exposure upregulated the expression of the norepinephrine transporter (NET) in the FC (Kruskal-Wallis test-Dunn, KW statistic = 14.57, df = 4, p = 0.0057; Fig. 2b). NET protein expression was not affected by treatments, but they seemed to prevent the increase induced by the CMS, being the CMS+Duloxetine group, the one that showed a clearer trend towards avoiding the CMS-induced NET increment.
Effects of CMS and Antidepressant Treatments on the Expression of the Serotonin Receptors 5-HT1A, 5-HT1B, 5-HT2A, 5-HT2B, 5-HT2C, and 5-HT7 in the FC
CMS increased mRNA expression levels of 5-HT1A and the treatments seemed to blunt the effects of CMS on 5-HT1A although without statistical differences (one-way ANOVA-Tukey F(4,38) = 2.85, p = 0.0368; Fig. 3a). The CMS exposure had no effect on 5-HT1B mRNA but desipramine induced an upregulation in 5-HT1B mRNA levels compared with control (Kruskal-Wallis test-Dunn, KW statistic = 18.13, df = 4, p = 0.0012; Fig. 3b).
Effects of CMS and AD treatments on the expression of the 5-HT receptors 5-HT1A, 5-HT1B, 5-HT2A, 5-HT2B, 5-HT2C, and 5-HT7 in the FC. CMS increased the mRNA expression levels of 5-HT1A (a), 5-HT2B (d), and 5-HT7 (f) (p = 0.0053; two-tailed t test) when compared with the control group. CMS had no effect on mRNA levels of 5-HT1B (b), 5-HT2A (c), and 5-HT2C (e). Desipramine treatment upregulated 5-HT1B mRNA levels compared with the control group (b). Desipramine and Duloxetine upregulated 5-HT2A mRNA levels compared with the control and CMS groups (c) but none of the ADs could affect the induction of the expression of 5-HT2B caused by the CMS protocol although duloxetine made its levels similar to control (d). No effects recorded for the ADs over 5-HT2C (e). Treatments did not have any effect on 5-HT7 mRNA levels (f). The vehicle-injected groups did not differ from the same experimental groups without injection, and their values have been pooled in the figure. Data are means ± SEM of 6–8 rats per group; *p < 0.05, **p < 0.01, ***p < 0.001 vs. control; #p < 0.05, vs. CMS; One-way ANOVA following Tukey post hoc test
The postsynaptic receptor 5-HT2A did not change under CMS conditions but desipramine and duloxetine upregulated its levels compared with the control and CMS groups (one-way ANOVA-Tukey F(4,39) = 7.579, p = 0.0001; Fig. 3c). 5-HT2B increased in the FC after CMS but none of the antidepressants affected the induction of the expression of 5-HT2B caused by CMS, although duloxetine made its levels similar to control (one-way ANOVA-Tukey F(4,39) = 6.674, p = 0.0003; Fig. 3d). No effects were detected in 5-HT2C mRNA (one-way ANOVA-Tukey F(4,37) = 1.163, p = 0.3427; Fig. 3d).
There were no significant differences in 5-HT7 mRNA when all the groups were analyzed (one-way ANOVA-Tukey F(4,38) = 2.539, p = 0.0556; Fig. 3f). However, there was a trend to increase 5-HT7 levels when comparing CMS with the control group.
Effects of CMS and Antidepressant Treatments on the Expression of the Adrenergic Receptors in the FC
The α1A expression did not change in our experimental set (one-way ANOVA-Tukey F(4,39) = 2.003, p = 0.1131; Fig. 4a). The CMS exposure trended to decrease α1B mRNA and desipramine and duloxetine upregulated it (one-way ANOVA-Tukey F(4,39) = 10.87, p < 0.0001; Fig. 4b). CMS and CMS+Desipramine levels of α1D were increased compared with the control group (Kruskal-Wallis test-Dunn, KW statistic = 18.75, df = 4, p = 0.0009; Fig. 4c).
Effects of CMS and AD treatments on the expression of NE receptors α1A, α1B, α1D, α2A, α2B, α2C, β1, β2, and β3 in the FC. The CMS increased α1D (c) and trended to diminish α1B (b) and α2A (d) (two-tailed unpaired t test, p = 0.0012 and p = 0.0036, respectively) and to upregulate β3 (i) (two-tailed unpaired t test, p = 0.0121) mRNA expression. Desipramine and duloxetine increased α1B (b) and α2A (d) and desipramine also increased α2C (f) and β1 (g) levels compared with the CMS group. No effects on any of the noradrenergic receptors were detected after the escitalopram treatment. The vehicle-injected groups did not differ from the same experimental groups without injection, and their values have been pooled in the figure. Data are means ± SEM of 6–8 rats per group; *p < 0.05, **p < 0.01, ***p < 0.001 vs. control; ##p < 0.01, ###p < 0.001 vs. CMS; $p < 0.05, $$p < 0.01 vs. CMS+Desip; &p < 0.05, &&p < 0.01 vs. CMS+Escit. One-way ANOVA following Tukey post hoc test. The values of α1D (c) did not follow a Gaussian distribution; thus, a nonparametric ANOVA with a Kruskal-Wallis test followed by a Dunn’s post hoc test was performed
Desipramine and duloxetine upregulated α2A mRNA (one-way ANOVA-Tukey F(4,39) = 21.67, p < 0.0001; Fig. 4d). α2A also trended to decrease under CMS conditions (two-tailed unpaired t test t = 3.216, df = 25, p = 0.0036). The experimental procedures applied did not alter α2B mRNA expression in the FC (one-way ANOVA-Tukey F(4,39) = 1.426, p = 0.2436; Fig. 4e). Only desipramine raised α2B levels under CMS conditions (one-way ANOVA-Tukey F(4,39) = 10.78, p < 0.0001; Fig. 4f).
β1 mRNA expression increased with the duloxetine treatment (one-way ANOVA-Tukey F(4,39) = 4.713, p = 0.0034; Fig. 4g). No changes detected in the FC for β2 (one-way ANOVA-Tukey F(4,39) = 0.3681, p = 0.8299; Fig. 4h) and β3 (one-way ANOVA-Tukey F(4,39) = 2.198, p = 0.0871; Fig. 4i), but a clear difference was revealed between CMS and control for β3.
Escitalopram had no effects on noradrenergic receptors.
Discussion
The inhibition of the monoamine reuptake still epitomizes the first pharmacological approach for mood disorders treatment [23]. This study examines alterations caused by CMS on the monoaminergic neurotransmission in FC of rats. Specifically, it explores possible changes in 5-HT and NE reuptake transporters and the 5-HT and NE signaling receptors expression.
Our results did not expose changes in serotonin and norepinephrine levels after CMS in FC. The method used for the assay refers to the whole levels of neurotransmitters and it does not represent the levels acting on the synaptic cleft. Other studies describe a decline of monoamines in FC after CMS exposure employing longer experimental protocols [24, 25]. Our results may rather reflect an equilibrium among synthesis and degradation of neurotransmitters. Nevertheless, the discussion about the real existence of changes in monoamine levels in MDD continues, and there are conflicting results showing either a decrease [26] or no effects [27] on serotonin and norepinephrine plasma concentrations in patients with MDD. This situation points out to a feasible implication of other neurotransmission elements involved in the antidepressant action of classic pharmacological treatments.
The desipramine-induced noradrenergic tone reduction detected could be part of a compensatory mechanism facing the high concentrations reached in the synaptic cleft after desipramine administration. Even more, it would agree with a hypothesis proposing the diminishing in the locus coeruleus activity as necessary for the efficacy of an antidepressant drug [28].
We have employed a stress-related protocol, which as inducer of the hypothalamic-pituitary-adrenal (HPA) axis stimulates the release of catecholamines, including norepinephrine (NE). The NET serves as the primary mechanism for the inactivation of noradrenergic signaling [29]. Thus, CMS-induced NET overexpression could be a mechanism aimed to decrease the trend of augmented NE levels compared with control detected in CMS. Furthermore, antidepressant treatments prevented the CMS-induced NET overexpression agreeing with studies supporting the ability of some ADs to restore the baseline NET expression levels. A possible hypothesis is that neural adaptation resulting in enhanced monoaminergic neurotransmission may be mediating antidepressant actions [30]. In the same vein, the absence of effects of CMS on SERT expression could be explained by the fact that CMS did not modify 5-HT levels, although further research is warranted to support these hypotheses.
Inhibition or desensitization of 5-HT1A receptors exhibits antidepressant effects in the raphe nuclei [31, 32]. The 5-HT1A heteroreceptors in FC can exert an indirect suppression of the serotonin cell firing in the dorsal raphe nucleus [33] and the selective activation of postsynaptic 5-HT1A receptors plays an important role in the antidepressant response [34]. Even more, chronic fluoxetine treatment decreases the 5-HT1A binding in prefrontal cortex and hippocampus of rats [35]. Our study shows that CMS upregulates 5-HT1A, and treatments block that upregulation, further supporting the idea of antidepressant effects mediated by 5-HT1A inhibition.
The absence of 5-HT1B expression changes after CMS seems coherent with other study demonstrating that 5-HT1B remains unaltered in the anterior cingulate cortex of patients with MDD [36]. In any case, the 5-HT1B auto and heteroreceptors populations are hard to study separately due to their overlapping diffuse localization in FC; thus, 5-HT1B receptor agonists and antagonists can exhibit antidepressant properties. The use of experimental strategies that allow the study of them separately represents an important issue for future research to reach reliable findings about the 5-HT1B and its potential as a therapeutic tool [37].
Postsynaptic 5-HT2A and 5-HT2B receptors seem to be necessary for the action of ADs [38] and their upregulation empowers the neurotransmission. Thus, data observed in the CMS could form part of a compensatory mechanism triggered to maintain a minimum of serotonin working in the synaptic cleft. The effect of ADs upregulating this kind of 5-HT receptors seems to be consistent with other studies indicating that they are essential for the effects of treatments [38].
The potential of the 5-HT2C receptor is being explored in psychiatric diseases [39] and an inverse agonism/antagonism has shown antidepressant properties [40]. However, 5-HT2C mRNA suffers from extensive RNA editing processes and these post-transcriptional modifications are critical for its function [41], making mRNA expression analysis maybe insufficient to explain 5-HT2C implication in CMS. In addition, 5-HT2C agonism, partial agonism, or antagonism are still undergoing testing to assess their antidepressant ability [42].
Latest observations in rodent models and patients suggest that 5-HT7 blockade mediates antidepressant efficacy [43]. Thus, taking also into account that 5-HT7 is upregulated after CMS, future research should focus on the potential as therapeutic targets of this family of receptors for the treatment of mood disorders.
Escitalopram did not affect noradrenergic receptors, which is coherent with its specificity for serotonin since escitalopram is a SSRI. Nevertheless, we found a possible effect for escitalopram in NET expression, indicating the significance of the crosstalk among monoamine neurotransmission systems and their relevance to depressive-like behaviors [44].
Alpha (α1) receptors have been related to antidepressant responses [45]. CMS exposure decreased α1B and increased α1D adrenoceptors, whereas desipramine and duloxetine increased α1B expression. These results are consistent with studies showing that activation of the α1B-adrenoceptors associated with antagonism of α1D-adrenoceptors might be one of the mechanisms involved in the antidepressant-like activity of imipramine and other tricyclic antidepressants in rodents [46]. Nevertheless, the lack of deep research involving α1 subtypes brings to light the need of further research to elucidate their contribution to the pathophysiology of depression.
The α2-adrenoceptors can function as autoreceptors regulating NE release or heteroreceptors modulating other neurotransmitters, including serotonin [47]. Our results showed a decrease in α2A after CMS, agreeing with reports showing that α2A knockout mice develop depressive-like phenotypes [48]. Moreover, desipramine induced the expression of α2A and α2C, and duloxetine increased the expression of α2A subtype. These results are consistent with the literature suggesting that α2 receptors are essential for the antidepressant activity [48, 49] and α2A specifically for the efficacy of desipramine through its direct interaction with the receptor [50]. These results are also consistent with a previous study wherein an α2-adrenoceptor antagonist blocked the antidepressant effect of acutely administered desipramine [51]. The absence of changes in α2B subtype could be explained due to its low expression profile in FC [52]. Actually, it seems like regulation of receptors in depressive disorders is likely to vary considerably among different brain regions and even highly localized subregions [53].
The overlap between the auto and heteroreceptor population hinders the interpretation of mRNA α2 expression results. On one hand, α2A receptors are increased in FC of suicide depressive victims [53, 54]. Moreover, mirtazapine and mianserin are α2 antagonists with widely proved antidepressant properties, although it cannot be ignored that they exert actions on other receptors [3]. Alternatively, the action upon postsynaptic α2 is critical for antidepressant effects [51]; it could improve the working memory [55] and it promotes brain plasticity [56]. Bearing in mind the opposite actions described, discerning the pre or postsynaptic nature of the changes on α2 receptors represents an essential issue for future research.
There are post mortem studies showing either increased, decreased, or unaffected levels of β-receptors in subjects with depression [57, 58]. Furthermore, it has been described that chronic signaling through β3-adrenergic receptors during social stress is an adaptive response that improves behavioral function and that β3 signaling may promote emotional coping with stress [59]. Our research has found upregulated β3 expression after CMS; thus, a plausible explanation could be based on the previously mentioned adaptive response to improve behavioral performance during stress. Moreover, antidepressant-treated groups show values close to the CMS increase, reflecting the positive effects of the β3 stimulation.
Agonism of β1 and β 2 receptors (e.g., by intraventricular administration of isoproterenol) produces behavioral changes similar to those observed after administration of proven antidepressant drugs [60]. Thus, desipramine induction of β1 receptor could explain part of the beneficial effects of this antidepressant drug. This outcome seems contrary to the decrease in β1 using an 8-week CMS reported in a previous study [61]. The length of the stress exposure and the multiple adjustments among the different subtypes of noradrenergic receptors could explain this downregulation. In any case, the increase described after imipramine treatment agrees with the desipramine results in our experiment. What is more, polymorphisms for β1 receptor have been associated with antidepressant outcomes [62].
For a better interpretation, and a summary, of the alterations caused by CMS and the actions of antidepressants over the serotonergic and noradrenergic neurotransmission in FC, a diagram with their possible synaptic implications is included in Fig. 5.
CMS effects on the monoaminergic neurotransmissions and their modulation by ADs. Schematic representation of 5-HT and NE synapses including the neurotransmitters, their receptors (5-HT1A, 5-HT1B, 5-HT2A, 5-HT2B, 5-HT2C, and 5-HT7 for serotonin; α1A, α1B, α1D, α2A, α2B, α2C, β1, β2, and β3 for noradrenaline), and their reuptake transporters (SERT and NET). Double-headed arrows indicate that the receptor could be either pre or postsynaptic. Bold arrows show the CMS effect on each element and their up or downregulation with Desipramine (Desip), Escitalopram (Escit), and Duloxetine (Dulox) under CMS conditions
Conclusions
We have identified imbalances in reuptake transporters and receptors involved in the monoaminergic neurotransmission pointing towards the weakening of their signaling. Our results also show that antidepressant treatments strive for the improvement of the monoaminergic tone, being desipramine and duloxetine more influential than escitalopram over noradrenergic elements.
To our knowledge, our study is the first one tackling a whole characterization of the serotonergic and noradrenergic receptors and reuptake transporters in the most used and validated depression model—the CMS. Moreover, the simultaneous analysis of three antidepressants with different mechanisms of action adds strength to this research allowing their comparison and providing new insights into their molecular effects.
In summary, there are molecular alterations on serotonergic and noradrenergic neurotransmissions in FC induced by CMS exposure. Yet more, antidepressant treatments modulate the elements of these neurotransmission systems differentially.
There is a need of more accurate and effective drugs to treat depression with lower side effects. Our research offers new insights in this direction providing some advices for possible multi-target drug designs.
References
Friedrich MJ (2017) Depression is the leading cause of disability around the world. JAMA 317(15):1517. https://doi.org/10.1001/jama.2017.3826
Ferrari F, Villa RF (2017) The neurobiology of depression: an integrated overview from biological theories to clinical evidence. Mol Neurobiol 54(7):4847–4865. https://doi.org/10.1007/s12035-016-0032-y
Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, Mohr DC, Schatzberg AF (2016) Major depressive disorder. Nat Rev Dis Primers 2:16065. https://doi.org/10.1038/nrdp.2016.65
Artigas F (2013) Serotonin receptors involved in antidepressant effects. Pharmacol Ther 137(1):119–131. https://doi.org/10.1016/j.pharmthera.2012.09.006
Perez, D., et al. Adrenoceptors. Last modified on 10/08/2015. Accessed on 19/11/2018. IUPHAR/BPS Guide to PHARMACOLOGY, http://www.guidetopharmacology.org/GRAC/FamilyIntroductionForward?familyId=4
Pytka K, Podkowa K, Rapacz A, Podkowa A, Zmudzka E, Olczyk A, Sapa J, Filipek B (2016) The role of serotonergic, adrenergic and dopaminergic receptors in antidepressant-like effect. Pharmacol Rep 68(2):263–274. https://doi.org/10.1016/j.pharep.2015.08.007
Belmaker RH (2004) Bipolar disorder. N Engl J Med 351(5):476–486. https://doi.org/10.1056/NEJMra035354
Santarsieri D, Schwartz TL (2015) Antidepressant efficacy and side-effect burden: a quick guide for clinicians. Drugs Context 4:212290. https://doi.org/10.7573/dic.212290
Martin-Hernandez D, Bris AG, MacDowell KS, Garcia-Bueno B, Madrigal JL, Leza JC, Caso JR (2016) Modulation of the antioxidant nuclear factor (erythroid 2-derived)-like 2 pathway by antidepressants in rats. Neuropharmacology 103:79–91. https://doi.org/10.1016/j.neuropharm.2015.11.029
Taler M, Gil-Ad I, Lomnitski L, Korov I, Baharav E, Bar M, Zolokov A, Weizman A (2007) Immunomodulatory effect of selective serotonin reuptake inhibitors (SSRIs) on human T lymphocyte function and gene expression. Eur Neuropsychopharmacol 17(12):774–780. https://doi.org/10.1016/j.euroneuro.2007.03.010
Robison AJ, Vialou V, Sun HS, Labonte B, Golden SA, Dias C, Turecki G, Tamminga C et al (2014) Fluoxetine epigenetically alters the CaMKIIalpha promoter in nucleus accumbens to regulate DeltaFosB binding and antidepressant effects. Neuropsychopharmacology 39(5):1178–1186. https://doi.org/10.1038/npp.2013.319
Zhou C, Zhong J, Zou B, Fang L, Chen J, Deng X, Zhang L, Zhao X et al (2017) Meta-analyses of comparative efficacy of antidepressant medications on peripheral BDNF concentration in patients with depression. PLoS One 12(2):e0172270. https://doi.org/10.1371/journal.pone.0172270
Abdel-Razaq W, Kendall DA, Bates TE (2011) The effects of antidepressants on mitochondrial function in a model cell system and isolated mitochondria. Neurochem Res 36(2):327–338. https://doi.org/10.1007/s11064-010-0331-z
Hashioka S, McGeer PL, Monji A, Kanba S (2009) Anti-inflammatory effects of antidepressants: possibilities for preventives against Alzheimer’s disease. Cent Nerv Syst Agents Med Chem 9(1):12–19
Willner P (2005) Chronic mild stress (CMS) revisited: consistency and behavioural-neurobiological concordance in the effects of CMS. Neuropsychobiology 52:90–110. https://doi.org/10.1159/000087097
Bravo L, Mico JA, Rey-Brea R, Pérez-Nievas B, Leza JC, Berrocoso E (2012) Depressive-like states heighten the aversion to painful stimuli in a rat model of comorbid chronic pain and depression. Anesthesiology 117:613–625. https://doi.org/10.1097/ALN.0b013e3182657b3e
Martin-Hernandez D, Tendilla-Beltran H, Madrigal JLM, Garcia-Bueno B, Leza JC, Caso JR (2019) Chronic mild stress alters kynurenine pathways changing the glutamate neurotransmission in frontal cortex of rats. Mol Neurobiol 56(1):490–501. https://doi.org/10.1007/s12035-018-1096-7
Kuœmider M, Solich J, Paach P, Dziedzicka-wasylewska M (2007) Effect of citalopram in the modified forced swim test in rats. Pharmacol Rep 59:785–788
Rénéric J, Lucki I (1998) Antidepressant behavioral effects by dual inhibition of monoamine reuptake in the rat forced swimming test. Psychopharmacology 136:190–197
Gárate I, García-Bueno B, Madrigal JLM, Bravo L, Berrocoso E, Caso JR, Mico JA, Leza JC (2011) Origin and consequences of brain Toll-like receptor 4 pathway stimulation in an experimental model of depression. J Neuroinflammation 8:151. https://doi.org/10.1186/1742-2094-8-151
Untergasser A, Cutcutache I, Koressaar T, Ye J, Faircloth BC, Remm M, Rozen SG (2012) Primer3—new capabilities and interfaces. Nucleic Acids Res 40(15):e115. https://doi.org/10.1093/nar/gks596
Kent WJ, Sugnet CW, Furey TS, Roskin KM, Pringle TH, Zahler AM, Haussler D (2002) The human genome browser at UCSC. Genome Res 12(6):996–1006. https://doi.org/10.1101/gr.229102
Willner P, Scheel-Kruger J, Belzung C (2013) The neurobiology of depression and antidepressant action. Neurosci Biobehav Rev 37:2331–2371. https://doi.org/10.1016/j.neubiorev.2012.12.007
Deng XY, Li HY, Chen JJ, Li RP, Qu R, Fu Q, Ma SP (2015) Thymol produces an antidepressant-like effect in a chronic unpredictable mild stress model of depression in mice. Behav Brain Res 291:12–19. https://doi.org/10.1016/j.bbr.2015.04.052
Jia M, Li C, Zheng Y, Ding X, Chen M, Ding J, Du R, Lu M et al (2017) Leonurine exerts antidepressant-like effects in the chronic mild stress-induced depression model in mice by inhibiting neuroinflammation. Int J Neuropsychopharmacol 20(11):886–895. https://doi.org/10.1093/ijnp/pyx062
Quintana J (1992) Platelet serotonin and plasma tryptophan decreases in endogenous depression. Clinical, therapeutic, and biological correlations. J Affect Disord 24(2):55–62
Ruhe HG, Mason NS, Schene AH (2007) Mood is indirectly related to serotonin, norepinephrine and dopamine levels in humans: a meta-analysis of monoamine depletion studies. Mol Psychiatry 12(4):331–359. https://doi.org/10.1038/sj.mp.4001949
West CH, Ritchie JC, Boss-Williams KA, Weiss JM (2009) Antidepressant drugs with differing pharmacological actions decrease activity of locus coeruleus neurons. Int J Neuropsychopharmacol 12(5):627–641. https://doi.org/10.1017/S1461145708009474
Pacholczyk T, Blakely RD, Amara SG (1991) Expression cloning of a cocaine- and antidepressant-sensitive human noradrenaline transporter. Nature 350(6316):350–354. https://doi.org/10.1038/350350a0
Zhao Z, Zhang HT, Bootzin E, Millan MJ, O’Donnell JM (2009) Association of changes in norepinephrine and serotonin transporter expression with the long-term behavioral effects of antidepressant drugs. Neuropsychopharmacology 34(6):1467–1481. https://doi.org/10.1038/npp.2008.183
Bortolozzi A, Castañé A, Semakova J, Santana N, Alvarado G, Cortés R, Ferrés-Coy A, Fernández G et al (2012) Selective siRNA-mediated suppression of 5-HT1A autoreceptors evokes strong anti-depressant-like effects. Mol Psychiatry 17:612–623. https://doi.org/10.1038/mp.2011.92
Hughes ZA, Starr KR, Scott CM, Newson MJ, Sharp T, Watson JM, Hagan JJ, Dawson LA (2007) Simultaneous blockade of 5-HT1A/B receptors and 5-HT transporters results in acute increases in extracellular 5-HT in both rats and guinea pigs: in vivo characterization of the novel 5-HT1A/B receptor antagonist/5-HT transport inhibitor SB-649915-B. Psychopharmacology 192:121–133. https://doi.org/10.1007/s00213-006-0691-x
Altieri SC, Garcia-Garcia AL, Leonardo ED, Andrews AM (2013) Rethinking 5-HT1A receptors: emerging modes of inhibitory feedback of relevance to emotion-related behavior. ACS Chem Neurosci 4(1):72–83. https://doi.org/10.1021/cn3002174
Blier P, Bergeron R, de Montigny C (1997) Selective activation of postsynaptic 5-HT1A receptors induces rapid antidepressant response. Neuropsychopharmacology 16(5):333–338. https://doi.org/10.1016/S0893-133X(96)00242-4
Volle J, Bregman T, Scott B, Diwan M, Raymond R, Fletcher PJ, Nobrega JN, Hamani C (2018) Deep brain stimulation and fluoxetine exert different long-term changes in the serotonergic system. Neuropharmacology 135:63–72. https://doi.org/10.1016/j.neuropharm.2018.03.005
Veldman ER, Svedberg MM, Svenningsson P, Lundberg J (2017) Distribution and levels of 5-HT1B receptors in anterior cingulate cortex of patients with bipolar disorder, major depressive disorder and schizophrenia—an autoradiography study. Eur Neuropsychopharmacol 27(5):504–514. https://doi.org/10.1016/j.euroneuro.2017.02.011
Nautiyal KM, Tritschler L, Ahmari SE, David DJ, Gardier AM, Hen R (2016) A lack of serotonin 1B autoreceptors results in decreased anxiety and depression-related behaviors. Neuropsychopharmacology 41(12):2941–2950. https://doi.org/10.1038/npp.2016.109
Diaz SL, Narboux-Neme N, Boutourlinsky K, Doly S, Maroteaux L (2016) Mice lacking the serotonin 5-HT2B receptor as an animal model of resistance to selective serotonin reuptake inhibitors antidepressants. Eur Neuropsychopharmacol 26(2):265–279. https://doi.org/10.1016/j.euroneuro.2015.12.012
Chagraoui A, Thibaut F, Skiba M, Thuillez C, Bourin M (2016) 5-HT2C receptors in psychiatric disorders: a review. Prog Neuro-Psychopharmacol Biol Psychiatry 66:120–135. https://doi.org/10.1016/j.pnpbp.2015.12.006
Opal MD, Klenotich SC, Morais M, Bessa J, Winkle J, Doukas D, Kay LJ, Sousa N et al (2014) Serotonin 2C receptor antagonists induce fast-onset antidepressant effects. Mol Psychiatry 19(10):1106–1114. https://doi.org/10.1038/mp.2013.144
Burns CM, Chu H, Rueter SM, Hutchinson LK, Canton H, Sanders-Bush E, Emeson RB (1997) Regulation of serotonin-2C receptor G-protein coupling by RNA editing. Nature 387(6630):303–308. https://doi.org/10.1038/387303a0
Martin CB, Hamon M, Lanfumey L, Mongeau R (2014) Controversies on the role of 5-HT(2C) receptors in the mechanisms of action of antidepressant drugs. Neurosci Biobehav Rev 42:208–223. https://doi.org/10.1016/j.neubiorev.2014.03.001
Nikiforuk A (2015) Targeting the serotonin 5-HT 7 receptor in the search for treatments for CNS disorders: rationale and progress to date. CNS Drugs 29:265–275. https://doi.org/10.1007/s40263-015-0236-0
Blier P (2001) Crosstalk between the norepinephrine and serotonin systems and its role in the antidepressant response. J Psychiatry Neurosci 26(Suppl):S3–S10
Cunha MP, Pazini FL, Oliveira A, Bettio LE, Rosa JM, Machado DG, Rodrigues AL (2013) The activation of alpha1-adrenoceptors is implicated in the antidepressant-like effect of creatine in the tail suspension test. Prog Neuro-Psychopharmacol Biol Psychiatry 44:39–50. https://doi.org/10.1016/j.pnpbp.2013.01.014
Ribeiro CA, Pupo AS (2015) Involvement of alpha1B-adrenoceptors in the anti-immobility effect of imipramine in the tail suspension test. Eur J Pharmacol 750:39–42. https://doi.org/10.1016/j.ejphar.2015.01.010
Langer SZ (2015) alpha2-adrenoceptors in the treatment of major neuropsychiatric disorders. Trends Pharmacol Sci 36(4):196–202. https://doi.org/10.1016/j.tips.2015.02.006
Schramm NL, McDonald MP, Limbird LE (2001) The alpha(2a)-adrenergic receptor plays a protective role in mouse behavioral models of depression and anxiety. J Neurosci 21(13):4875–4882
Vega-Rivera NM, Lopez-Rubalcava C, Estrada-Camarena E (2013) The antidepressant-like effect of ethynyl estradiol is mediated by both serotonergic and noradrenergic systems in the forced swimming test. Neuroscience 250:102–111. https://doi.org/10.1016/j.neuroscience.2013.06.058
Cottingham C, Li X, Wang Q (2012) Noradrenergic antidepressant responses to desipramine in vivo are reciprocally regulated by arrestin3 and spinophilin. Neuropharmacology 62(7):2354–2362. https://doi.org/10.1016/j.neuropharm.2012.02.011
Zhang HT, Whisler LR, Huang Y, Xiang Y, O’Donnell JM (2009) Postsynaptic alpha-2 adrenergic receptors are critical for the antidepressant-like effects of desipramine on behavior. Neuropsychopharmacology 34(4):1067–1077. https://doi.org/10.1038/npp.2008.184
Nicholas AP, Pieribone V, Hokfelt T (1993) Distributions of mRNAs for alpha-2 adrenergic receptor subtypes in rat brain: an in situ hybridization study. J Comp Neurol 328(4):575–594. https://doi.org/10.1002/cne.903280409
Cottingham C, Wang Q (2012) alpha2 adrenergic receptor dysregulation in depressive disorders: implications for the neurobiology of depression and antidepressant therapy. Neurosci Biobehav Rev 36(10):2214–2225. https://doi.org/10.1016/j.neubiorev.2012.07.011
Gonzalez-Maeso J, Rodriguez-Puertas R, Meana JJ, Garcia-Sevilla JA, Guimon J (2002) Neurotransmitter receptor-mediated activation of G-proteins in brains of suicide victims with mood disorders: selective supersensitivity of alpha(2A)-adrenoceptors. Mol Psychiatry 7(7):755–767. https://doi.org/10.1038/sj.mp.4001067
Avery RA, Franowicz JS, Studholme C, van Dyck CH, Arnsten AF (2000) The alpha-2A-adrenoceptor agonist, guanfacine, increases regional cerebral blood flow in dorsolateral prefrontal cortex of monkeys performing a spatial working memory task. Neuropsychopharmacology 23(3):240–249. https://doi.org/10.1016/S0893-133X(00)00111-1
Ren WW, Liu Y, Li BM (2012) Stimulation of alpha(2A)-adrenoceptors promotes the maturation of dendritic spines in cultured neurons of the medial prefrontal cortex. Mol Cell Neurosci 49(2):205–216. https://doi.org/10.1016/j.mcn.2011.10.001
Klimek V, Rajkowska G, Luker SN, Dilley G, Meltzer HY, Overholser JC, Stockmeier CA, Ordway GA (1999) Brain noradrenergic receptors in major depression and schizophrenia. Neuropsychopharmacology 21(1):69–81. https://doi.org/10.1016/S0893-133X(98)00134-1
Rivero G, Gabilondo AM, Garcia-Sevilla JA, La Harpe R, Callado LF, Meana JJ (2014) Increased alpha2- and beta1-adrenoceptor densities in postmortem brain of subjects with depression: differential effect of antidepressant treatment. J Affect Disord 167:343–350. https://doi.org/10.1016/j.jad.2014.06.016
Chuang JC, Krishnan V, Yu HG, Mason B, Cui H, Wilkinson MB, Zigman JM, Elmquist JK et al (2010) A beta3-adrenergic-leptin-melanocortin circuit regulates behavioral and metabolic changes induced by chronic stress. Biol Psychiatry 67(11):1075–1082. https://doi.org/10.1016/j.biopsych.2009.12.003
O’Donnell JM, Frith S, Wilkins J (1994) Involvement of beta-1 and beta-2 adrenergic receptors in the antidepressant-like effects of centrally administered isoproterenol. J Pharmacol Exp Ther 271(1):246–254
Klimek V, Papp M (1994) The effect of MK-801 and imipramine on beta-adrenergic and 5-HT2 receptors in the chronic mild stress model of depression in rats. Pol J Pharmacol 46(1–2):67–69
Firouzabadi N, Raeesi R, Zomorrodian K, Bahramali E, Yavarian I (2017) Beta adrenoceptor polymorphism and clinical response to sertraline in major depressive patients. J Pharm Pharm Sci 20:1–7. https://doi.org/10.18433/J3W31F
Acknowledgments
We thank Dr. Karina S. MacDowell, Dr. Aline Sayd, Cristina Ulecia, and Beatriz Moreno for technical assistance.
Funding
This work was supported by the Instituto de Salud Carlos III and the Spain’s Ministry of Economy, Industry and Competitiveness (MINECO) through the Plan Estatal de I+D+i 2013–2016 (FIS-PI13/01102 and SAF2016-75500-R to JCL), the Agencia Estatal de Investigación (AEI) and Fondo Europeo de Desarrollo Regional (FEDER) (SAF2017-83053-R to JRC), and CIBERSAM (CB/07/09/0026 to JCL and SAM15PINT1514 to JRC). DMH is a postdoctoral researcher (Consejería de Educación, Juventud y Deporte-CAM y Fondo Social Europeo). HTB received a fellowship from the Consejo Nacional de Ciencia y Tecnología (CONACYT, Mexico). JRC is a postdoctoral Ramon y Cajal Fellow (Spain’s Ministry of Science, Innovation and Universities and FEDER).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Martín-Hernández, D., Pereira, M.P., Tendilla-Beltrán, H. et al. Modulation of Monoaminergic Systems by Antidepressants in the Frontal Cortex of Rats After Chronic Mild Stress Exposure. Mol Neurobiol 56, 7522–7533 (2019). https://doi.org/10.1007/s12035-019-1619-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-019-1619-x