Abstract
Impairment of mitochondrial metabolism, particularly the electron transport chain (ETC), as well as increased oxidative stress might play a significant role in pathogenesis of Alzheimer’s disease (AD). Some effects of drugs used for symptomatic AD treatment may be related to their direct action on mitochondrial function. In vitro effects of pharmacologically different cognitives (galantamine, donepezil, rivastigmine, 7-MEOTA, memantine) and nootropic drugs (latrepirdine, piracetam) were investigated on selected mitochondrial parameters: activities of ETC complexes I, II + III, and IV, citrate synthase, monoamine oxidase (MAO), oxygen consumption rate, and hydrogen peroxide production of pig brain mitochondria. Complex I activity was decreased by galantamine, donepezil, and memantine; complex II + III activity was increased by galantamine. None of the tested drugs caused significant changes in the rate of mitochondrial oxygen consumption, even at high concentrations. Except galantamine, all tested drugs were selective MAO-A inhibitors. Latrepirdine, donepezil, and 7-MEOTA were found to be the most potent MAO-A inhibitors. Succinate-induced mitochondrial hydrogen peroxide production was not significantly affected by the drugs tested. The direct effect of cognitives and nootropics used in the treatment of AD on mitochondrial respiration is relatively small. The safest drugs in terms of disturbing mitochondrial function appear to be piracetam and rivastigmine. The MAO-A inhibition by cognitives and nootropics may also participate in mitochondrial neuroprotection. The results support the future research aimed at measuring the effects of currently used drugs or newly synthesized drugs on mitochondrial functioning in order to understand their mechanism of action.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alzheimer’s disease (AD) is a progressive neurodegenerative disorder. It is the most common cause of dementia characterized by a progressive impairment of memory and a decline of various cortical functions (e.g., judgment, orientation, behavior). Therapeutic strategies for AD treatment are designed to target cholinergic hypofunctioning, N-methyl-D-aspartate (NMDA) receptor overactivation, amyloid β (Aβ) by interfering with its synthesis, aggregation or degradation, and/or mitochondria and monoamine oxidase (MAO) [1]. Current options for AD treatment are very limited and are based on the administration of cholinesterase (ChE) inhibitors (donepezil, rivastigmine, galantamine) and/or the NMDA receptor antagonist, memantine [2, 3]. Nootropic drugs, such as piracetam and latrepirdine, are also used to treat cognitive impairment in the elderly and for dementia.
Drugs used therapeutically for AD such as donepezil, rivastigmine, and galantamine positively affect cholinergic central transmission, decrease the enzymatic degradation of acetylcholine by the inhibition of acetylcholinesterase (AChE, E.C. 3.1.1.7), and increase both the concentration and persistence of acetylcholine in the synaptic cleft [4]. The first AChE inhibitor licensed for AD therapy was tacrine, which was withdrawn from the market due to its toxicity. 7-methoxytacrine (9-amino-7-methoxy-1,2,3,4-tetrahydroacridine, 7-MEOTA), a tacrine derivative, has lower toxicity than tacrine and was described as a candidate molecule for AD treatment [5, 6]. 7-MEOTA derivatives were synthesized and extensively investigated to find less toxic compounds affecting more AD pathological mechanisms [6, 7]. Galantamine, donepezil, and rivastigmine have been shown to possess neuroprotective properties through a mechanism likely unrelated to AChE inhibition [8, 9]. Memantine, a non-cholinergic alternative to AChE inhibitors for AD treatment, preferentially blocks glutamate NMDA receptors without disruption of their normal physiological activity [10]. Latrepirdine (Dimebon™) has been suggested as a neuroprotective agent affecting numerous cellular functions, calcium influx, mitochondrial function, and intracellular metabolic pathways [11] including activation of the energy sensor AMP-activated protein kinase and a reduction of neuronal excitability [12]. Piracetam is described as a metabolic enhancer, which ameliorated the impairment of mitochondrial function induced by β-amyloid (Aβ) [13] or improved mitochondrial dysfunction following oxidative stress [14].
The understanding of the complexity of AD and its underlying mechanisms could be helpful in the search and development of new AD treatments [15]. The brain cells are very vulnerable to oxidative stress due to their high metabolic rate and high production of reactive oxygen species (ROS) as a by-product of oxidative phosphorylation (OXPHOS) in the electron transport chain (ETC) system [16]. The production of ROS by the mitochondria is considered in the pathogenesis of neurodegenerative disorders [17, 18]. Mitochondrion-derived ROS are sufficient to trigger Aβ production, and Aβ itself leads to mitochondrial dysfunction and increased ROS levels [19]. The role of mitochondrial enzyme monoamine oxidase (MAO; EC 1.4.3.4) is important to study in this context because MAO affects both hydrogen peroxide (H2O2) production and metabolism of intraneuronal monoamine neurotransmitters. MAO activity is inhibited by many different pharmacological substances [20–22]. Investigating the direct action of ChE inhibitors on components of the monoamine system could be useful for both understanding their therapeutic and/or adverse effects and for the development of new drugs with increased therapeutic efficiency due to dual acetylcholinergic and monoaminergic action. The current study tested the hypothesis that some effects of cognitives and nootropic drugs may be linked to changes in mitochondrial functions. The aim of our study was to detect the direct effects of drugs used in AD treatment plus the effect of 7-MEOTA, a candidate molecule for AD treatment, on activity of ETC complexes, citrate synthase (CS) activity, and the oxygen consumption rate in isolated mitochondria. The effects of 7-MEOTA, memantine, rivastigmine, donepezil, galantamine, latrepirdine, and piracetam were also examined on MAO activity and H2O2 production by mitochondria.
Methods and Materials
Media and Chemicals
Buffered sucrose (sucrose 0.32 mol/L, HEPES 4 mmol/L, pH 7.4) was used as isolation medium and preservation medium for isolated mitochondria. Krebs-Henseleit buffer (KH buffer) consisted of 118 mmol/L NaCl, 4.7 mmol/L KCl, 1.2 mmol/L KH2PO4, 1.2 mmol/L MgSO4·7H2O, 25 mmol/L NaHCO3, 11.1 mmol/L glucose (pH 7.4). The mitochondrial respiration medium (MiR05) consisted of sucrose 110 mmol/L, K+-lactobionate 60 mmol/L, taurine 20 mmol/L, MgCl2.6H2O 3 mmol/L, KH2PO4 10 mmol/L, EGTA 0.5 mmol/L, BSA essentially fatty acid free 1 g/L and HEPES 20 mmol/L, adjusted to pH 7.1 with KOH (32). Other media were used in enzyme assays. Radiochemicals, 5-hydroxytryptamine [3H] trifluoroacetate ([3H]serotonin) and 2-phenylethylamine [ethyl-1-14C] hydrochloride ([14C]PEA) were purchased from American Radiolabeled Chemicals, Inc. (St. Louis, MO, USA), other chemicals from Sigma-Aldrich Co. (St. Louis, MO, USA).
Isolation of Brain Mitochondria
The mitochondrial fraction and purified mitochondria were isolated and prepared from pig brain cortex as described previously [20, 23]. Samples of mitochondria purified on a sucrose gradient were stored on ice until the assay. The fresh crude mitochondrial fraction (stored on ice) was used for measurement of mitochondrial oxygen consumption rate. Fresh purified mitochondria (stored on ice) were used in experiments with H2O2 production. The frozen crude mitochondrial fraction (stored at −70 °C) was used for determination of enzyme activities. The protein concentration was determined by the Lowry method [24], with bovine serum albumin as the standard.
Activity of Citrate Synthase and Respiratory Complexes
Purified mitochondria were resuspended with hypotonic buffer (25 mmol/L potassium phosphate, 5 mmol/L MgCl2, pH 7.2) and ultrasonicated three times to achieve the maximum enzymatic activity. Samples were incubated with selected drugs at a concentration of 50 μmol/L for 30 min at 30 °C. Each independent measurement had a control. Samples were measured in 3 mL of total reaction volume at 30 °C; the final protein concentration was 150 μg/mL. The activity of ETC complexes and CS was measured spectrophotometrically using Uvicon XL spectrophotometer (SECOMAM, Alès, France).
Complex I (NADH dehydrogenase (ubiquinone), EC 1.6.5.3)
The method used has been previously described [25, 26] Complex I activity was measured as the rotenone-sensitive rate of NADH oxidation at 340 nm. The reaction was started by the addition of coenzyme Q1 (in a final concentration 33 μmol/L) and measured for 10 min.
Complex II + III (Succinate cytochrome c oxidoreductase, EC 1.8.3.1)
Mitochondrial complex II + III activity was measured spectrophotometrically as antimycin A sensitive rate of cytochrome c reduction at 550 nm using succinate as a substrate [27].
Complex IV (cytochrome c oxidase, COX, EC 1.9.3.1).
COX activity was measured as a decrease in absorbance during the oxidation of reduced cytochrome c at 550 nm [28].
Citrate synthase (CS, EC 2.3.3.1).
CS activity was measured as a color change of 5,5′-dithiobis-(2-nitrobenzoic) acid (DNTB); the reaction was initiated by the addition of 0.5 mmol/L oxaloacetate and absorbance was measured at 412 nm for 3 min [29].
Mitochondrial Respiration
Mitochondrial oxygen consumption rate was measured at 37 °C using a titration-injection high-resolution oxygraph (Oxygraph-2 k, Oroboros Instruments, Innsbruck, Austria) with Clark-type electrodes. Experimental protocols were adapted from previous studies [30, 31]. The respiration medium MiR05 (oxygen solubility factor: 0.92) was added into chambers to a final volume of 2 mL. The crude mitochondrial fraction was added to a final protein concentration between 0.05–0.20 mg/mL. Plasma membranes were permeabilized by digitonin (573 μg digitonin/mg protein). The respiratory rate of mitochondria in respiratory states related to electron entry through complex I and complex II was assessed using specific mitochondrial substrates: malate + pyruvate for complex I-linked respiration, succinate + rotenone for complex II-linked respiration. Two parallel samples were titrated and measured simultaneously. The final drug concentrations were between 1.25–100 μmol/L, except for piracetam, whose effect was measured up to 10 mmol/L. Oligomycin, rotenone, and antimycin A were used as inhibitors of ATP synthase, complex I and complex III, respectively.
Monoamine Oxidase Activity
MAO-A and MAO-B activities were determined by means of radiochemistry using a previously published method [32, 33]. Briefly, the reaction mixture in KH buffer containing the mitochondria and various drug concentrations was preincubated for 60 min at 37 °C. The reaction was initiated by the addition of a radiolabelled substrate. The final sample volume was 250 μl containing 200 μg of protein, 3.2 μmol/L [3H]serotonin for MAO-A or 10 μmol/L [14C]PEA for MAO-B, and 0.1 μmol/L to 100 mmol/L of drug. MAO activity was measured at 37 °C for 30 min for MAO-A and for 1 min for MAO-B. The reaction was stopped by the addition of 250 μl of 2 N hydrochloric acid. The reaction products were extracted into benzene:ethyl acetate 1:1 (v/v), and the radioactivity of extracts in organic phase were measured by liquid scintillation counting (LS 6000IC, Beckman Instruments, Inc., Fullerton, CA, USA).
Hydrogen Peroxide Release
Purified mitochondria in a final concentration of 0.10 mg/mL were incubated in buffer (26.85 mmol/L Hepes, 114.1 mmol/L sucrose, 100 mmol/L KCl, 1.342 mmol/L K2HPO4, pH 7.3) with 10 mmol/L succinate, 1.0 mmol/L ADP, and 50 μmol/L of selected cognitives or nootropics for 30 min at 37 °C. The extramitochondrial release of H2O2 was determined using 7.5 μmol/L Ampliflu™ Red in the presence of 1.5 units/mL horseradish peroxidase, according to a previously described and slightly modified method [34]. In total, 0.5 μmol/L rotenone and 1.25 μg/mL antimycin A were used to inhibit activities of complex I and complex III, respectively, after 5 min in every measurement. Fluorescence was monitored continuously for 15 min in a fluorometer (Fluoromax-3, Jobin Yvon, Horiba) at an excitation of 571 nm and an emission of 585 nm. The fluorescence intensity was converted to H2O2 concentration based on measurement of the fluorescence increase after addition of a known amount of H2O2 [35].
Data Analysis and Statistics
Enzyme activities were measured as the slope of time dependence of absorbance using LabPower Junior software (SECOMAM). Relative changes of enzyme activities induced by the drugs were determined assuming that the control sample activity is equal to 100 %. Data from high-resolution respirometry were collected and analyzed using DatLab 4.3 software (Oroboros Instruments, Innsbruck, Austria). Respiratory rates were expressed as mass-specific oxygen flux (pmol O2 consumed per second/mg of protein in the sample).
Drug-induced inhibition of respiratory rate and MAO activity was analyzed using a four-parameter logistic regression (SigmaPlot, Systat Software Inc., Richmond, CA, USA) to quantify IC 50 (concentration of a drug that is required for 50 % inhibition) and the residual activity at high drug concentration. Data were expressed as the mean ± standard error.
The results were analyzed by the data analysis software system STATISTICA (version 12.0, StatSoft, Inc., Tulsa, OK, USA). One-sample t tests for single means were used to determine whether enzyme activity in the sample with drug added was significantly different from the control. For H2O2 production, the effect of inhibitors in the control sample was evaluated by t-test for dependent samples. Comparisons between controls and samples with the drug were performed using ANOVA, and the Dunnett test was utilized for post hoc comparisons. The data are expressed as the mean ± standard deviation.
Results
Activity of CS and Respiratory Chain Complexes
Drug-induced changes in cellular energetics characterized by activity of CS and individual ETC complexes were measured in purified mitochondria. None of the tested drugs significantly affected the CS activity. Significantly decreased complex I activity was caused by donepezil (p = 0.029), galantamine (p = 0.049), and memantine (p = 0.010, Fig. 1a). Significantly increased complex II + III activity was observed after incubation with galantamine (p = 0.021, Fig. 1b). Complex IV was insignificantly increased after incubation with latrepirdine (p = 0.070, Fig. 1c).
Drug-induced changes in activity of the a complex I, b complex II + III, and c complex IV in pig brain mitochondria. The sample was incubated with a drug at 30 °C for 30 min, and the enzyme activity was determined relative to control sample with solvent added without the drug. Values are the means ± standard deviation at 3–7 independent measurements. Equality of enzyme activity in sample with drug to enzyme activity in the sample without drug was tested using a t test for single means against 100 % (*p < 0.05)
Mitochondrial Respiration
Drug-induced changes in oxygen consumption rate were measured in isolated pig brain mitochondria incubated with substrates for complex I or complex II-linked respiration. A slight decrease in complex I-linked respiration was observed for galantamine and memantine. Increases were induced only by rivastigmine; piracetam, latrepirdine, 7-MEOTA and donepezil did not change the oxygen consumption rate (Fig. 2a). Complex II-linked respiration was insignificantly increased by memantine, slightly increased by latrepirdine, galantamine, and donepezil; piracetam, 7-MEOTA, and rivastigmine did not change the oxygen consumption rate (Fig. 2b). No change was statistically significant. Note the effect of piracetam was measured up to a concentration of 10 mmol/L without any change (data not shown).
Drug-induced changes of a complex I-linked respiration, b complex II-linked respiration in pig brain mitochondria. Dose-response curves are displayed as plots of the relative respiratory rate against the drug concentration, presuming that the relative respiratory rate equals 1 at zero drug concentration. Lines show a tendency to decrease, increase or no change in the respiratory rate with increasing drug concentrations. Values are the means of 3–7 independent measurements. t tests for single means against the control sample with solvent added without the drug did not confirm significant changes in mitochondrial respiration, even at high drug concentrations. The effect of rotenone and antimycin A is shown in embedded graphs to illustrate their inhibitory effects on complex I-and complex II-linked respiration
The effects of rotenone and antimycin A on complex I-and complex II-linked respiration were measured under the same experimental conditions to confirm the sensitivity of our respiratory assay to known inhibitors of respiration (inset graphs in Fig. 2). We confirmed the full inhibition of both complex I-linked respiration by rotenone and complex II-linked respiration by antimycin A.
Monoamine Oxidase Activity
The dose-dependent effects of pharmacologically different cognitives and nootropic drugs on MAO-A and MAO-B activity were measured in pig brain mitochondria.
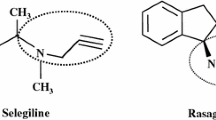
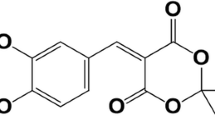
MAO-A activity was fully inhibited by all tested drugs; however, higher half maximal inhibitory concentrations (IC 50) of cognitive enhancers were observed compared to the known MAO inhibitors, such as iproniazid, pargyline, and clorgyline (Fig. 3a, Table 1). MAO-A was inhibited by the drugs tested in the following order: pargyline > clorgyline > iproniazid > donepezil = latrepirdine =7-MEOTA > memantine = rivastigmine > galantamine > piracetam. Piracetam, galantamine, rivastigmine, and memantine are very weak inhibitors of MAO-A activity. Donepezil, latrepirdine, and 7-MEOTA are relatively strong MAO inhibitors. MAO-B activity was fully inhibited by latrepirdine and memantine; partial inhibition was caused by 7-MEOTA, donepezil, and galantamine. Rivastigmine induced an initial increase in MAO-B activity followed by a rapid decrease (full inhibition) at very high concentrations. Piracetam caused monotonic increase of MAO-B activity, even at very high (millimolar) concentrations (Fig. 3b). IC 50 values characterizing MAO-B inhibition were higher than MAO-A inhibition, except for galantamine (Table 1).
Changes in basal monoamine oxidase type (MAO) activity caused by cognitive enhancers in the crude mitochondrial fraction of pig brain. Concentration-response curves are displayed as plots of the initial enzyme activity against the drug concentration for a MAO-A and b MAO-B. The samples were incubated with drugs at 37 °C for 60 min, and the reaction was started by the addition of 3.2 μmol/L [3H]serotonin for MAO-A and by the addition of 10 μmol/L [14C]phenylethylamine for MAO-B. Median effective concentrations (IC 50) were calculated using nonlinear regression analysis software. Values are the means calculated from at least five independent measurements. Lines represent the best fit curves using the four-parameter logistic function, except for effect of rivastigmine and piracetam on MAO-B activity. Inhibitory effects of pargyline, clorgyline, and iproniazid are displayed for comparison
Hydrogen Peroxide Release
The effects of cognitives and nootropics on the release of hydrogen peroxide from purified pig brain mitochondria were determined fluorometrically after 30-min incubation with succinate. The addition of rotenone (complex I inhibitor) and antimycin A (complex III inhibitor) followed. The results are summarized in Fig. 4. In the control sample (with added solvent without drug), rotenone had no effect, and antimycin A caused a significant increase in succinate-induced H2O2 release (p < 0.001). Compared to the control, the succinate + rotenone + antimycin A-induced increase in H2O2 release was not significantly affected by any drug tested in this study (Fig. 4).
Drug-induced changes of hydrogen peroxide release from purified brain mitochondria. The samples (0.10 mg protein/mL) were incubated with drugs (50 μmol/L) or with solvent (control) at 30 °C for 30 min in presence of 10 mmol/L succinate. Samples were supplemented with 1.5 units/mL of horseradish peroxidase and 7.5 μmol/L Ampliflu™ Red, and fluorescence of resorufin was monitored. In total, 0.5 μmol/L rotenone and 1.25 μg/mL antimycin A was added to inhibit the activity of complex I and complex III, respectively. Values are the means ± SEM of 3–5 independent measurements. For controls, comparison between hydrogen peroxide release in the presence of succinate, succinate + rotenone, or succinate + rotenone + antimycin A were evaluated by t-tests for dependent samples (***p < 0.001). Comparisons between control and samples with drug added were performed using ANOVA and post-hoc Dunnett test, which did not find significant changes in the hydrogen peroxide release for any tested cognitive drug
Discussion
To determine the effect of cognitives and nootropics for AD treatment in mitochondrial energy metabolism, we investigated the in vitro effect of piracetam, latrepirdine, 7-MEOTA, galantamine, donepezil, rivastigmine, and memantine on mitochondrial respiration, enzyme activities of CS and ETC complexes, mitochondrial ROS release, and MAO activity in isolated brain mitochondria.
The Effects of Cognitives and Nootropics on Mitochondrial Complexes and Respiration
CS is localized in the mitochondrial matrix and commonly used as a quantitative enzyme marker for the presence of intact mitochondria. We did not observe any significant drug-induced changes in CS activity, which confirms CS activity as a proper mitochondrial marker also during pharmacotherapy with cognitive enhancers. Many drugs have been shown to induce a mild and transient inhibition of complex I, which plays a role in their mechanisms of action. Inhibitory effect of tacrine on complex I activity was found in vitro in pig brain mitochondria [36]. We observed mild complex I inhibition by galantamine, donepezil, and memantine, indicating the possible involvement of mitochondrial dysfunction on the adverse effects of high doses of these drugs (Fig. 1a). The activity of complexes II + III and IV was unchanged by all of the drugs examined in the study, except for a significant increase in complex II + III activity by galantamine (Fig. 1b).
The in vitro effects of some cognitives and nootropics on the activity of mitochondrial complexes in isolated mitochondria are apparently linked to high concentrations of these drugs (50 μmol/L). Such concentrations are higher than plasma concentrations at therapeutic doses of the drugs (latrepirdine <0.05 μmol/L, 7-MEOTA <0.2 μmol/L, galantamine 0.2–0.5 μmol/L, donepezil 0.08–0.13 μmol/L, rivastigmine 0.01–0.10 μmol/L, memantine 0.5–1.0 μmol/L), except for piracetam (200–2000 μmol/L). The use of high doses of tested drugs in in vitro experiments can be justified in part by the fact that there is an accumulation of some drugs in the brain and that their intraneuronal concentrations are unknown. Moreover, information on in vitro mitochondrial effects at high drug concentrations can be useful for the design of in vivo experiments, which should confirm or disprove these effects at therapeutic doses.
Galantamine mildly inhibited complex I activity, stimulated complex II + III activity, and did not significantly affect either complex IV activity or the oxygen consumption rate. It can be speculated that the direct inhibitory effects of galantamine on complex I can be compensated by the stimulatory effect of the drug on complex II + III. Memantine partially inhibited complex I activity, did not affect complex II + II or complex IV activity, slightly decreased complex I-linked respiration, and increased complex II-linked respiration. These results are consistent and correspond to previous findings where memantine was protective against the effects of 3-nitropropionic acid (complex II inhibitor) but was ineffective in protection against rotenone-induced toxicity (complex I inhibitor) in spiny striatal neurons. We partially confirmed the results of an earlier in vitro study on the direct effects of acute memantine exposure on isolated mitochondria. In that study when the oxygen consumption rate was increased, complex I activity was increased, and complex IV activity was decreased at high (60 μmol/L) memantine concentrations [37]. However, the differences in complex I- and complex II-linked respiration were not determined in this study. Donepezil was found to gently inhibit complex I (Fig. 1a) with no effect on complex II + III, complex IV, or mitochondrial respiration. It appears that the direct effect of donepezil on ETC activity is not included in the non-cholinergic mechanisms that are associated with its neuroprotective profile [9].
One clinical study found that the cellular respiration supported by complex I and complex II substrates as well as activities of complexes II, III, and IV were increased in AD patients treated with rivastigmine [38]. The mechanisms by which rivastigmine would stimulate ETC are uncertain. Compensatory mechanisms of declines or increases of individual complexes in OXPHOS are also possible. Our data show that there is no significant direct effect of rivastigmine on individual respiratory complexes, and respiration characterizing ECT activity as a whole is indicative of stimulatory effects. Therefore, effects of rivastigmine on mitochondrial respiration may support its neuroprotective action.
7-MEOTA and its derivatives are considered candidate molecules for AD treatment, due to lower toxicity, better antioxidant properties, interaction with muscarinic and nicotinic receptors, and safer metabolization compared to tacrine [5]. In our study, we found that 7-MEOTA did not change the activity of mitochondrial complexes I, II + III, or IV and did not affect the mitochondrial oxygen consumption rate. From this perspective, the 7-MEOTA does not exhibit anti-mitochondrial effects.
Piracetam is supposed to enhance mitochondrial function or at least protect against mitochondrial damage in the aging brain or in people with dementia [39]. Piracetam has been found to improve mitochondrial dysfunction following oxidative stress [14] and also to ameliorate the detrimental effects of Aβ on brain functions [13]. In the current study, piracetam did not induce any change in the activity of complexes I, II + III, or IV. Neither complex I- nor complex II-linked respiration was affected by piracetam at concentrations up to 10 mmol/L. Our results indicate that the piracetam-induced beneficial effect on cognition is not associated with its rapid direct effect on the mitochondrial electron transport system activity. Thus, piracetam seems to be very safe in terms of mitochondrial toxicity even at very high concentrations. This confirmed the results of a previous study, which showed that piracetam did not affect mitochondrial membrane potential and ATP levels in PC12 cells under basal conditions without additional insult [14].
Latrepirdine action is believed to be involved in improving cellular energy balance, stabilizing mitochondrial function by increasing the threshold for nonselective mitochondrial pore opening, increasing the calcium retention capacity of mitochondria and reducing lipid peroxidation [40]. We observed that latrepirdine caused nonsignificant changes in activities of ETC complexes, and in the oxygen consumption rate. A lack of an effect of latrepirdine on mitochondrial respiration and/or activity of the ETC complexes does not indicate an association with its therapeutic effects.
Inhibition of MAO Activity
MAO catalyzes the oxidative deamination of a variety of biogenic and xenobiotic amines with concomitant H2O2 production. MAO activity is inhibited by many psychotropic drugs [20]; and MAO inhibitors are considered potential candidates for AD treatment, due to their ability to inhibit oxidative damage. A series of new multifunctional MAO/ChE inhibitors have been synthesized for AD treatment [41, 42].
While MAO inhibition is not a primary biochemical effect related to therapeutic action of cognitives and nootropics, it can be supposed that changes in MAO activity may be related to some of the effects of these drugs on serotonergic, noradrenergic, and dopaminergic neurotransmission. Moreover, MAO inhibition may participate in antioxidant and neuroprotective effects of cognitives and nootropics. We found that the most potent MAO inhibitors are latrepirdine, 7-MEOTA, and donepezil. The IC 50 of approximately 5 μmol/L for inhibition of MAO-A indicates that MAO-A activity may be inhibited at therapeutic doses of these drugs. Thus, neuroprotective and antidepressant or mood altering effects can be of added value to the improved cognition by treatment with these drugs. Latrepirdine, 7-MEOTA, donepezil, and memantine were found to be selective MAO-A inhibitors (Table 1), which is in conflict with previous findings that latrepirdine in rat brain homogenate [43] and donepezil in rat liver homogenate [41] preferentially inhibited MAO-B. We suppose that the purification of mitochondria may play a role in this discrepancy because the presence of non-mitochondrial membranes may affect the concentrations of free substances. The lowest potency to inhibit MAO-A was found for piracetam; however, 1 mmol/L piracetam plasma concentration may be reached during therapy, which is sufficient to partially inhibit MAO-A. In contrast, a stimulatory effect on MAO-B was found for piracetam. These findings indicate that the resulting effect of piracetam on MAO activity may be different in various tissues/cells with different representations of MAO-A and MAO-B [44].
Hydrogen Peroxide Production
Respiratory complexes I and III are taken as the source of the most ROS in mitochondria, and ROS generation and release can be regulated by the choice of substrates and inhibitors. During complex I-linked respiration, ROS are produced from complexes I and III, whereas complex II-linked respiration leads to ROS production to some extent by complex III but also through reverse electron flow to complex I. Electron flow through the complexes can be inhibited selectively, e.g., by rotenone (complex I) and antimycin A (complex III), resulting in an alteration in the production of ROS [16].
We measured the drug’s effect on the release of mitochondrial H2O2 in the presence of succinate + rotenone + antimycin A. Although such ROS production is non-physiological, it can be used to evaluate the protective effect of cognitives and nootropics on mitochondrial ROS production.
In the absence of a tested drug (in the control sample), succinate-dependent H2O2 generation was relatively low, and rotenone (complex I inhibitor) had no significant effect. In contrast, antimycin A (complex III inhibitor) significantly stimulated (approximately four-fold) H2O2 production in controls (Fig. 4). Because reverse electron transport was inhibited by rotenone and complex I substrates were not added, this antimycin-induced H2O2 production could be assigned to complex III.
H2O2 production in the presence of succinate + rotenone + antimycin A was not significantly different in control samples and samples with added cognitive enhancers. This is consistent with the finding that the complex II-linked mitochondrial oxygen consumption rate was not significantly altered by the same drugs. Our results confirmed that there are neither protective nor deteriorative effects of cognitive enhancers on succinate + rotenone + antimycin A-stimulated ROS production in mitochondria.
In conclusion, the different in vitro effects of piracetam, latrepirdine, 7-MEOTA, galantamine, donepezil, rivastigmine, and memantine on mitochondrial respiration, the enzymatic activity of CS and ETC complexes, H2O2 production, and MAO activity support the presumed hypothesis for the independent mode of the mitochondrial action of various cognitives and nootropics. We confirmed that the cognitives and nootropics utilized in this study have a relatively small direct effect on selected mitochondrial functions, even at high concentrations. The high drug concentration required for this direct mitochondrial effect indicates that non-receptor mechanisms play a role. The inhibitory effects of these drugs on MAO-A may participate in mitochondrial neuroprotection; however, they should be taken into account if there is a co-administration of drugs affecting monoaminergic transmission. Drug-induced changes in mitochondrial functions should be included in a panel of tests for newly synthetized drugs in order to rule out their mitochondrial toxicity and have a better understanding of their mechanisms of action.
References
Zheng H, Fridkin M, Youdim MB (2012) Novel chelators targeting cell cycle arrest, acetylcholinesterase, and monoamine oxidase for Alzheimer’s therapy. Curr Drug Targets 13(8):1089–1106
Hroudová J, Singh N, Fišar Z, Ghosh KK (2016) Progress in drug development for Alzheimer’s disease: an overview in relation to mitochondrial energy metabolism. Eur J Med Chem 121:774–784. doi:10.1016/j.ejmech.2016.03.084
Zemek F, Drtinova L, Nepovimova E, Sepsova V, Korabecny J, Klimes J, Kuca K (2014) Outcomes of Alzheimer’s disease therapy with acetylcholinesterase inhibitors and memantine. Expert Opin Drug Saf 13(6):759–774. doi:10.1517/14740338.2014.914168
Nieoullon A (2010) Acetylcholinesterase inhibitors in Alzheimer’s disease: further comments on their mechanisms of action and therapeutic consequences. Psychol Neuropsychiatrie du vieillissement 8(2):123–131. doi:10.1684/pnv.2010.0208
Soukup O, Jun D, Zdarova-Karasova J, Patocka J, Musilek K, Korabecny J, Krusek J, Kaniakova M, Sepsova V, Mandikova J, Trejtnar F, Pohanka M, Drtinova L, Pavlik M, Tobin G, Kuca K (2013) A resurrection of 7-MEOTA: a comparison with tacrine. Curr Alzheim Res 10(8):893–906
Korabecny J, Musilek K, Holas O, Nepovimova E, Jun D, Zemek F, Opletalova V, Patocka J, Dohnal V, Nachon F, Hroudova J, Fisar Z, Kuca K (2010) Synthesis and in vitro evaluation of N-(Bromobut-3-en-2-yl)-7-methoxy-1,2,3,4-tetrahydroacridin-9-amine as a cholinesterase inhibitor with regard to Alzheimer’s disease treatment. Mol (Basel, Switzerland) 15(12):8804–8812. doi:10.3390/molecules15128804
Korabecny J, Musilek K, Holas O, Binder J, Zemek F, Marek J, Pohanka M, Opletalova V, Dohnal V, Kuca K (2010) Synthesis and in vitro evaluation of N-alkyl-7-methoxytacrine hydrochlorides as potential cholinesterase inhibitors in Alzheimer disease. Bioorg Med Chem Lett 20(20):6093–6095. doi:10.1016/j.bmcl.2010.08.044
Arias E, Gallego-Sandin S, Villarroya M, Garcia AG, Lopez MG (2005) Unequal neuroprotection afforded by the acetylcholinesterase inhibitors galantamine, donepezil, and rivastigmine in SH-SY5Y neuroblastoma cells: role of nicotinic receptors. J Pharmacol Exp Ther 315(3):1346–1353. doi:10.1124/jpet.105.090365
Ye CY, Lei Y, Tang XC, Zhang HY (2015) Donepezil attenuates Abeta-associated mitochondrial dysfunction and reduces mitochondrial Abeta accumulation in vivo and in vitro. Neuropharmacology. doi:10.1016/j.neuropharm.2015.02.020
Lipton SA (2004) Paradigm shift in NMDA receptor antagonist drug development: molecular mechanism of uncompetitive inhibition by memantine in the treatment of Alzheimer’s disease and other neurologic disorders. J Alzheimer’s Dis : JAD 6(6 Suppl):S61–S74
Sabbagh MN, Shill HA (2010) Latrepirdine, a potential novel treatment for Alzheimer’s disease and Huntington’s chorea. Curr Opin Invest Drugs (London, England : 2000) 11(1):80–91
Weisova P, Alvarez SP, Kilbride SM, Anilkumar U, Baumann B, Jordan J, Bernas T, Huber HJ, Dussmann H, Prehn JH (2013) Latrepirdine is a potent activator of AMP-activated protein kinase and reduces neuronal excitability. Transl Psychiatry 3:e317. doi:10.1038/tp.2013.92
Kurz C, Ungerer I, Lipka U, Kirr S, Schutt T, Eckert A, Leuner K, Muller WE (2010) The metabolic enhancer piracetam ameliorates the impairment of mitochondrial function and neurite outgrowth induced by beta-amyloid peptide. Br J Pharmacol 160(2):246–257. doi:10.1111/j.1476-5381.2010.00656.x
Keil U, Scherping I, Hauptmann S, Schuessel K, Eckert A, Muller WE (2006) Piracetam improves mitochondrial dysfunction following oxidative stress. Br J Pharmacol 147(2):199–208. doi:10.1038/sj.bjp.0706459
Zhang HY (2012) New insights into huperzine A for the treatment of Alzheimer’s disease. Acta Pharmacol Sin 33(9):1170–1175. doi:10.1038/aps.2012.128
Mattiasson G (2004) Analysis of mitochondrial generation and release of reactive oxygen species. Cytom Part A: J Int Soc Anal Cytol 62(2):89–96. doi:10.1002/cyto.a.20089
Hirst J, King MS, Pryde KR (2008) The production of reactive oxygen species by complex I. Biochem Soc Trans 36(Pt 5):976–980. doi:10.1042/bst0360976
Drose S, Brandt U (2008) The mechanism of mitochondrial superoxide production by the cytochrome bc1 complex. J Biol Chem 283(31):21649–21654. doi:10.1074/jbc.M803236200
Leuner K, Schutt T, Kurz C, Eckert SH, Schiller C, Occhipinti A, Mai S, Jendrach M, Eckert GP, Kruse SE, Palmiter RD, Brandt U, Drose S, Wittig I, Willem M, Haass C, Reichert AS, Muller WE (2012) Mitochondrion-derived reactive oxygen species lead to enhanced amyloid beta formation. Antioxid Redox Signal 16(12):1421–1433. doi:10.1089/ars.2011.4173
Fišar Z, Hroudová J, Raboch J (2010) Inhibition of monoamine oxidase activity by antidepressants and mood stabilizers. Neuro Endocrinol Lett 31(5):645–656
Fisar Z (2010) Inhibition of monoamine oxidase activity by cannabinoids. Naunyn Schmiedeberg’s Arch Pharmacol 381(6):563–572. doi:10.1007/s00210-010-0517-6
Fišar Z, Hroudová J, Korábečný J, Musílek K, Kuča K (2011) In vitro effects of acetylcholinesterase reactivators on monoamine oxidase activity. Toxicol Lett 201(2):176–180. doi:10.1016/j.toxlet.2010.12.023
Pinna G, Broedel O, Eravci M, Stoltenburg-Didinger G, Plueckhan H, Fuxius S, Meinhold H, Baumgartner A (2003) Thyroid hormones in the rat amygdala as common targets for antidepressant drugs, mood stabilizers, and sleep deprivation. Biol Psychiatry 54(10):1049–1059
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ (1951) Protein measurement with the Folin phenol reagent. J Biol Chem 193(1):265–275
Folbergrová J, Jesina P, Haugvicová R, Lisý V, Houstek J (2010) Sustained deficiency of mitochondrial complex I activity during long periods of survival after seizures induced in immature rats by homocysteic acid. Neurochem Int 56(3):394–403. doi:10.1016/j.neuint.2009.11.011
Hroudova J, Fisar Z (2010) Activities of respiratory chain complexes and citrate synthase influenced by pharmacologically different antidepressants and mood stabilizers. Neuro Endocrinol Lett 31(3):336–342
Trounce IA, Kim YL, Jun AS, Wallace DC (1996) Assessment of mitochondrial oxidative phosphorylation in patient muscle biopsies, lymphoblasts, and transmitochondrial cell lines. Methods Enzymol 264:484–509
Rustin P, Chretien D, Bourgeron T, Gerard B, Rotig A, Saudubray JM, Munnich A (1994) Biochemical and molecular investigations in respiratory chain deficiencies. Clin Chim Acta; Int J Clin Chem 228(1):35–51
Srere PA (1969) Citrate synthase: [EC 4.1.3.7 citrate oxaloacetate-lyase (CoA acetylating)]. Methods Enzymol 13:3–11
Hroudová J, Fišar Z (2012) In vitro inhibition of mitochondrial respiratory rate by antidepressants. Toxicol Lett 213(3):345–352. doi:10.1016/j.toxlet.2012.07.017
Pesta D, Gnaiger E (2012) High-resolution respirometry: OXPHOS protocols for human cells and permeabilized fibers from small biopsies of human muscle. Methods Mol Biol (Clifton, NJ) 810:25–58. doi:10.1007/978-1-61779-382-0_3
Ekstedt B (1976) Substrate specificity of the different forms of monoamine oxidase in rat liver mitochondria. Biochem Pharmacol 25(10):1133–1138
Egashira T, Takayama F, Yamanaka Y (1999) The inhibition of monoamine oxidase activity by various antidepressants: differences found in various mammalian species. Jpn J Pharmacol 81(1):115–121
Liu Y, Fiskum G, Schubert D (2002) Generation of reactive oxygen species by the mitochondrial electron transport chain. J Neurochem 80(5):780–787
Ross T, Szczepanek K, Bowler E, Hu Y, Larner A, Lesnefsky EJ, Chen Q (2013) Reverse electron flow-mediated ROS generation in ischemia-damaged mitochondria: role of complex I inhibition vs. depolarization of inner mitochondrial membrane. Biochim Biophys Acta 1830(10):4537–4542. doi:10.1016/j.bbagen.2013.05.035
Hroudová J, Fišar Z, Korábečný J, Kuča K (2011) In vitro effects of acetylcholinesterase inhibitors and reactivators on complex I of electron transport chain. Neuro Endocrinol Lett 32(3):259–263
McAllister J, Ghosh S, Berry D, Park M, Sadeghi S, Wang KX, Parker WD, Swerdlow RH (2008) Effects of memantine on mitochondrial function. Biochem Pharmacol 75(4):956–964. doi:10.1016/j.bcp.2007.10.019
Casademont J, Miro O, Rodriguez-Santiago B, Viedma P, Blesa R, Cardellach F (2003) Cholinesterase inhibitor rivastigmine enhance the mitochondrial electron transport chain in lymphocytes of patients with Alzheimer’s disease. In: J Neurol Sci, vol 206. vol 1. Netherlands, pp 23–26
Stockburger C, Kurz C, Koch KA, Eckert SH, Leuner K, Muller WE (2013) Improvement of mitochondrial function and dynamics by the metabolic enhancer piracetam. Biochem Soc Trans 41(5):1331–1334. doi:10.1042/bst20130054
Ustyugov A, Shevtsova E, Bachurin S (2015) Novel sites of neuroprotective action of Dimebon (latrepirdine). Mol Neurobiol. doi:10.1007/s12035-015-9249-4
Wang L, Esteban G, Ojima M, Bautista-Aguilera OM, Inokuchi T, Moraleda I, Iriepa I, Samadi A, Youdim MB, Romero A, Soriano E, Herrero R, Fernandez Fernandez AP, Ricardo Martinez M, Marco-Contelles J, Unzeta M (2014) Donepezil + propargylamine +8-hydroxyquinoline hybrids as new multifunctional metal-chelators, ChE and MAO inhibitors for the potential treatment of Alzheimer’s disease. Eur J Med Chem 80:543–561. doi:10.1016/j.ejmech.2014.04.078
Lu C, Zhou Q, Yan J, Du Z, Huang L, Li X (2013) A novel series of tacrine-selegiline hybrids with cholinesterase and monoamine oxidase inhibition activities for the treatment of Alzheimer’s disease. Eur J Med Chem 62:745–753. doi:10.1016/j.ejmech.2013.01.039
Shadurskaia SK, Khomenko AI, Pereverzev VA, Balaklevskii AI (1986) Neuromediator mechanisms of the effect of the antihistamine agent dimebone on the brain. Biull Eksp Biol Med 101(6):700–702
Stancheva SL, Alova LG (1988) Effect of centrophenoxine, piracetam and aniracetam on the monoamine oxidase activity in different brain structures of rats. Farmakol Toksikol 51(3):16–18
Acknowledgments
Supported by International Post-Doc Research Fund of Charles University, by project PRVOUK-P26/LF1/4 given by Charles University and by grants AZV 15-28967A and 15-28616A, Ministry of Health, Czech Republic. Authors are grateful to Mr. Zdeněk Hanuš for his technical assistance.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Singh, N., Hroudová, J. & Fišar, Z. In Vitro Effects of Cognitives and Nootropics on Mitochondrial Respiration and Monoamine Oxidase Activity. Mol Neurobiol 54, 5894–5904 (2017). https://doi.org/10.1007/s12035-016-0121-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12035-016-0121-y