Abstract
Gastroenteropancreatic (GEP) neuroendocrine tumors (NETs) represent a heterogeneous group of tumors that is associated with an indolent course. Octreotide has a positive effect on disease stabilization in well-differentiated midgut NETs, but a meaningful survival analysis was not possible due to insufficient events. Higher doses of octreotide long-acting release (LAR) are often used in clinical practice for control of carcinoid symptoms and our objective was to determine if dose of octreotide correlates with survival. We reviewed all patients with advanced GEP NETs who initiated treatment with octreotide LAR between 2000 and 2013 in a large, representative Canadian province. We compared overall survival in patients who received low (< 30 mg) compared to high (≥ 30 mg) doses of octreotide. A total of 170 patients were identified. Baseline characteristics in the low- and high-dose groups were similar: median age 62/63 years, 50/58% were male, 46/48% originated from the small bowel, and 74/66% had liver metastases at diagnosis. The median time from diagnosis to treatment initiation was 5.5 and 6.0 months. Octreotide LAR was initiated with the intent of symptom management (71%), disease stabilization (23%), or biomarker control (6%). Median overall survival (OS) was better in the high-dose group, 66 months compared to 22 months (multivariate HR 0.5, p < 0.01). Age ≥ 65 (HR 1.9, p < 0.01), ECOG ≥ 2 (HR 2.7, p < 0.01), and pancreatic NETs (HR 1.7, p = 0.03) were all predictors of worse survival. Our findings suggest that octreotide may confer survival benefits in GEP NETs. Further prospective studies are warranted to validate the impact of high-dose octreotide on outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Neuroendocrine tumors (NETs) originating from the gastrointestinal (GI) tract represent an uncommon group of heterogeneous tumors. The estimated incidence in the Western world is 2.5–5.0 per 100,000 patients with an increasing incidence over the years [1, 2]. The difficulty in studying NETs is several fold: multiple classification systems, variable clinical behaviors, difficulty in imaging these tumors, and long disease survival rates requiring prolonged follow-up.
A common characteristic of gastroenteropancreatic (GEP) NETs is the expression of somatostatin receptors [3]. Somatostatin analogs were first introduced to manage the symptoms related to functional NETs causing carcinoid syndrome. Population studies have shown that the overall survival of patients with NETs was greatly improved since the 1980s, which was close to the time when somatostatin was introduced [1, 3].
Somatostatin analogs, such as octreotide, are recognized for their antitumor effects in well-differentiated NETs and have been shown to improve survival [4,5,6,7]. The development of octreotide into an anticancer agent differs from many other contemporary oncology drugs. Since octreotide long-acting release (LAR) has been in use for carcinoid symptom management for many years, there were no dose finding studies prior to the PROMID study to help determine optimal antitumor dose.
The first clinical study to suggest a possible antitumor effect of octreotide alone, a somatostatin analog, was published in 2009 [6]. The PROMID study showed that in patients with metastatic NETs arising from the midgut, treatment with octreotide 30 mg compared to placebo improved progression-free survival [6]. Although no difference was detected in overall survival, patients were likely not followed long enough to detect a difference. Another somatostatin analog, lanreotide, was studied in patients with metastatic NETs arising from any GI or lung primary [7]. Results of the CLARINET study are similar when compared to the PROMID study using octreotide. Patients receiving lanreotide had an improvement in progression-free survival but not overall survival [7]. Somatostatin analogs are well tolerated and often needed in the management of NET patients with carcinoid syndrome. These agents are now considered a standard of care in the management of these tumors.
Since somatostatin was long in use for symptom management before its antitumor effects were known, the optimal dosage for tumor control remains unknown. When used for symptom control, the recommended dosage for octreotide is to start at 20 mg intramuscularly (IM) and increase to 30 mg IM as needed for symptom control. Although not approved in doses over 30 mg, dose escalation beyond 30 mg is often done in clinical practice to control carcinoid symptoms [8,9,10,11,12]. Several publications have reported on the safety and tolerability of increasing the dose beyond 30 mg every 4 weeks for various indications including carcinoid symptoms, chemotherapy-induced diarrhea, and acromegaly [8,9,10,11,12,13,14]. Anthony et al. reported on the patterns of octreotide use for metastatic NETs over a period of 6 years, which included 15% of patients who received doses of octreotide LAR above 30 mg [9]. The most common adverse effects experienced were injection site discomfort, hyperglycemia, and cholelithiasis [9]. Other studies have reported on octreotide LAR doses of up to 120 mg every 4 weeks [10]. A review on dose optimization of somatostatin analogs showed that dose escalations were common and safe [11]. The most common adverse events experienced with dose escalation were diarrhea, abdominal pain, nausea, cholelithiasis, anorexia, and fatigue [11]. In our current study, we reviewed all patients with GI origin NETs treated with octreotide to characterize the pattern of octreotide use in the real-world setting and examine any associations between the dose of octreotide and treatment outcomes.
Methods
Study setting
The British Columbia Cancer Agency is a provincial program in Canada that provides population-based cancer treatment to approximately 5 million residents. It consists of five regional centers that are geographically distributed to ensure equal access to cancer care within the province. Affiliated community centers are responsible delivering treatment in remote areas. The Gastrointestinal Cancer Outcomes Database prospectively collects demographic and outcomes information on all patients who are seen at any one of the five regional centers. The follow-up rates on internal audit were over 95%. Research ethics approval was obtained from the British Columbia Cancer Agency and University of British Columbia institutional review board prior to the conduct of this study.
Study cohort
We performed a retrospective study of all patients with advanced GEP NETs who initiated treatment from 2000 to 2013. Outcomes data were updated in 2016 to ensure that all patients had long-term follow-up for this indolent disease. All adult patients aged 18 years or older with histologic confirmation of NET who initiated treatment with octreotide after the year 2000 and received at least one cycle of treatment were included in our study. All NETs with GI origin, including pancreatic NETs were included in our analysis. To capture a large number of patients in a rare tumor site, our inclusion criteria were broad. Those with initially resected disease that later progressed to advanced metastatic disease were included. Patients who received cytotoxic therapy or peptide receptor radionuclide therapy (PRRT) in addition to octreotide were also included in our study.
Patients with high-grade neuroendocrine carcinomas or small-cell carcinomas were excluded. As the WHO classification has changed during the study period, we applied the current definition to the old pathology reports whenever the information was available. Those who have a documented Ki67 > 20% or a mitotic count > 20/10 hpf were excluded. If they were not available, patients who received chemotherapy with the intent of treating small-cell carcinomas due to clinical behavior were also excluded from the analysis.
Study outcomes
Patients were reviewed for their baseline characteristics, which are summarized in Table 1. Tumor characteristics that were examined included site of tumor origin, Ki67 if available, presence of metastatic disease, and presence of liver metastases. Tumor burden within the liver could not be accurately accounted for based on the available imaging as they were often described as multiple metastases without a discrete measurement of size or number of lesions in the liver. However, carcinoid symptoms at the time octreotide was initiated were well documented. We included carcinoid symptoms of diarrhea, flushing, and carcinoid heart disease. Diarrheal symptoms were further classified as mild (< 4 stools/day), moderate (4–6 stools/day), and severe (> 7 stools/day). The presence of flushing without any other carcinoid symptoms was classified as mild. The presence of any clinically significant congestive heart failure secondary to carcinoid heart disease was considered severe symptoms. The intent of initiating octreotide as well as the reasons for increasing the dose of octreotide were divided into symptom control, biomarker elevation, and tumor control.
As patients were followed over a long period, we estimated octreotide exposure using the total cumulative dose divided by the total number of cycles to arrive at the mean dose per cycle. One cycle of octreotide was defined as a 4-week period. As a proportion of NET patients have a long indolent disease course, using the total dose received would create skewed results favoring those who received more cycles of octreotide. Using the median dose per cycle would be fraught with the same issue. Therefore, we believe that using the mean dose per cycle provides the best estimate in examining any associations between octreotide dose and outcome. Overall survival was compared between patients who received an average octreotide dose of less than 30 mg per cycle (low dose) and patients who received an average dose of octreotide 30 mg or above per cycle (high dose). Sensitivity analyses were conducted by using different cut-offs. Because findings were largely consistent, only results from the main analysis are presented.
We also attempted to correlate dose increases above 30 mg of octreotide with any corresponding changes in the commonly used tumor markers for NETs: chromogranin A (CGA) and urine 5-HIAA. Unfortunately, radiologic responses could not be followed as imaging was not done regularly among patients after dose increases of octreotide.
Statistical analysis
The baseline characteristics of patients who received low-dose octreotide are compared to high-dose cohort using the χ2 test. Overall survival was estimated from the time of administration of first cycle of octreotide to remove lead time bias. Overall survival was estimated using the Kaplan–Meier method and the log rank test was used to determine if there were any significant differences between the low-dose and high-dose groups. Multivariate Cox regression was performed to generate hazard ratios and 95% confidence intervals while adjusting for confounders such as age, gender, ECOG, presence of liver metastases, severity of carcinoid symptoms, site of tumor origin, and use of chemotherapy or PRRT. All p values were two sided where a p value of < 0.05 was considered statistically significant. All analyses were performed using SPSS version 24.0. Descriptive statistics were used to summarize tumor marker response after an increase in the dose of octreotide.
Results
We identified 170 patients with GEP NETs who initiated treatment with octreotide from 2000 to 2013 and received at least one cycle of therapy. The median mean dose per 28-day cycle of octreotide LAR was 27 mg. Patients were analyzed in two groups: those who received a mean dose of less than 30 mg per cycle were considered the low-dose group and those who received a mean dose of 30 mg or more were considered the high-dose group. Baseline characteristics between the two groups are similar and summarized in Table 1. The median age of diagnosis was 62 years in the low-dose octreotide group and 63 years in the high-dose octreotide group. Other demographics such as gender and ethnicity were balanced between groups. ECOG performance status was similar with most patients having a performance status of 0–1. Sites of tumor origin were also similar. About 50% of tumors originated from the small bowel, 24% were from the pancreas, and the remainder arose from other GI primaries such as the stomach, cecum, appendix, and rectum. One hundred and forty-six (86%) patients had advanced metastatic or unresectable disease at the time of diagnosis. In the entire cohort, metastases to the liver were common (70% in both low- and high-dose groups). The median time from diagnosis of metastatic disease to treatment initiation with octreotide was 5.5–6.0 months and this was not different between groups. The severity of carcinoid symptoms was different with about 50% of patients in the low-dose group having very mild carcinoid symptoms versus 24% in the high-dose group.
Octreotide was initiated for different reasons in patients who were treated with low-dose octreotide compared to those who were treated with high-dose octreotide. Treatment was started in the low-dose group most often for management of symptoms related to carcinoid syndrome. In the high-dose octreotide group, more patients were started on the drug with a goal of disease or biochemical control. Interestingly, the reasons for increasing the dose of octreotide did not differ between the two groups. The majority of patients had dose increases for symptom management. The findings are summarized in Table 2.
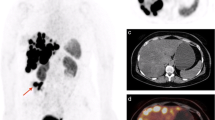
At the time of analysis, 71% of patients had died with a median follow-up time of 85 months. In the entire cohort, median OS was 40 months. Overall survival estimated from time of initiation of octreotide was worse in patients who received low-dose octreotide compared to high-dose octreotide (median OS 22 months vs. 66 months, respectively, p < 0.01) (Fig. 1). The effect of dose on OS remained statistically significant in multivariate analyses that adjusted for confounders (HR 0.5, 95% CI 0.3–0.7, p < 0.01). In multivariate analyses, age negatively impacted survival with patients aged over 65 years performing significantly worse (HR 1.9, 95% CI 1.3–2.9, p < 0.01). ECOG performance status also predicted survival (HRs 1.9 and 2.7 in patients with ECOG 1 and ECOG ≥ 2, respectively (p < 0.01)). Patients with NETs originating from the pancreas had worse outcomes compared with small bowel primaries (HR 1.7, 95% CI 1.1–2.8, p = 0.03). Sensitivity analysis was performed using a cut-off of mean octreotide dose of 27 mg per cycle and the results were similar showing a median OS of 24 months compared to 66 months and HR 0.4 (95% CI 0.3–0.6, p < 0.01). There were too few patients in our cohort who received an octreotide scan around the time of treatment initiation to make any meaningful conclusions about those who were octreotide avid compared to those who were not.
We also examined tumor marker levels of chromogranin A (CGA) and 24 h urine 5HIAA to explore if there were any biomarker relationships with octreotide dose. Only limited data were available as tumor markers were not consistently done within 3 months of dose increases. We identified 49 patients who had chromogranin A levels measured before and after dose increases of octreotide to over 30 mg/cycle. The median baseline CGA level was 220 µg/L (10–3800 µg/L) and the median CGA level measured within 3 months of increasing octreotide LAR to 30 mg was 120 µg/L (5–3900 µg/L). There was a non-significant trend to lower CGA levels after increasing octreotide LAR to 30 mg (p = 0.09) (Fig. 2). Only 17 patients had 24-h urine 5-HIAA levels done within 3 months of a dose increase and no associations were found between the pre- and post-dose increase biomarker levels (median 79 µmol/day and 58 µmol/day, p = 0.8).
Discussion
Our current study suggests a dose–response relationship of octreotide LAR and improved survival. High-dose octreotide LAR was an independent factor of improved survival. It is widely accepted that somatostatin analogs have active antitumor activity as demonstrated by a longer time to progression in prospective randomized studies and it is considered the standard of care in many jurisdictions [6, 7, 15, 16]. Our results suggest that dose optimization of octreotide LAR likely has added benefit and may inform the future development of somatostatin analog-based therapies.
Patients in our study cohort appear to have poor survival when measured from the time of treatment initiation, with a median OS of 40 months. There may be several explanations for this finding. Most patients had a long delay from time of metastatic disease to treatment initiation. A long interval without tumor directed therapy may be sufficient to impact survival. It is also important to note that only patients who have carcinoid symptoms are eligible to receive octreotide LAR during the study timeframe. This was an institutional policy that was enforced due in part to funding issues and interpretation of available data. Yao et al. found that carcinoid symptoms were associated with worse survival using a population database [17]. As a result, our study cohort may be selected for those with poorer prognosis.
A significant benefit in OS of 20 months was observed in our high-dose cohort. Limited data are available for the association of dose with survival. Chanda et al. conducted a retrospective analysis on 54 patients with GI NETs and found that those who received higher than octreotide LAR 30 mg had a longer time to radiographic progression. These patients also experienced improved 1-year survival rates [12]. We identified one study that examined overall survival as an endpoint [18]. Using the SEER database, Shen et al. identified a cohort of patients older than age 65 with a diagnosis of metastatic NET and who received treatment with octreotide LAR within 12 months of diagnosis [18]. The authors found that patients who received a higher dose within the first three cycles had better survival outcomes. This cohort of patients likely had more aggressive behavior compared to our current study as all patients required initiation of treatment within 12 months of diagnosis. In contrast, our study captured each patient’s dose exposure throughout the entire treatment period, which may be more reflective of a dose–response relationship.
Given the long period of follow-up in our current study and the use of an average dose, we did not feel that we would be able to accurately record and quantify symptom control with dose escalation in our study. Instead, we looked for changes in CGA and 24-h urine 5-HIAA levels as a surrogate measure and found a non-significant trend towards improved CGA with dose increases of octreotide LAR above 30 mg. Previously, a similar study conducted in our province found variable tumor marker responses to increases in octreotide LAR dose [19]. However, symptom control was better with higher doses of octreotide LAR [19]. Other studies have also demonstrated good associations between high-dose octreotide LAR and carcinoid symptom control [20, 21]. Ferolla et al. followed 28 patients prospectively who had refractory symptoms to octreotide LAR 30 mg every 4 weeks. They found that when the dosing interval was decreased to every 3 weeks, patients achieved clinical control of carcinoid symptoms. These results reflect the poor sensitivity and specificity of CGA and 24-h urine 5HIAA as tumor markers. However, better symptom control with higher doses of octreotide LAR further supports the notion that a dose–response relationship exists. It is plausible that those with a higher symptom burden require a higher dose of octreotide LAR to saturate all somatostatin receptors.
Several limitations exist in our study. First, this represents a retrospective analysis with inherent selection bias. Although we tried to adjust for differences in patient and disease factors, residual confounding remains in our multivariate analyses. Second, our patient cohort is heterogeneous. For patients who were diagnosed years ago and did not start treatment until 2000, we may lack all information necessary to apply the 2010 WHO grading system for NETs to select for well-differentiated tumors. Since patients with high-grade disease are likely to skew study results, each patient’s treatment course was reviewed and excluded if the treatment intent was chemotherapy for small-cell carcinomas. Third, using the mean octreotide dose per 4-week cycle does not accurately describe a dose–response relationship. However, it is a better approximation of dose exposure compared to using the total cumulative dose or a median dose. These limitations should be weighed against the study’s strengths, which include its large sample size and long duration of follow-up.
In summary, many patients with advanced GEP NETs who require initiation of treatment due to carcinoid symptoms or progressive disease do not experience prolonged survival. Octreotide has been demonstrated in prospective trials to have an antitumor effect on well-differentiated NETs. Our results add to the current literature by demonstrating an association between higher octreotide LAR doses and improved survival. Consideration should be given to future prospective studies to determine the optimal dose and timing for tumor control for this safe and effective medication. Further, recent studies of peptide receptor radionuclide therapy, which exploits somatostatin receptor expression, have shown promise [22]. Therefore, a true understanding of dose–response relationships of somatostatin analogs may help with patient selection for radionuclide therapy.
References
Yao JC, Hassan M, Phan A, et al. One hundred years after “carcinoid”: Epidemiology of and prognostic factors for neuroendocrine tumors in 35,825 cases in the United States. J Clin Oncol. 2008;26:3063–72.
Kulke MH, Shah MH, Benson AB. IIIrd, et al: Neuroendocrine tumors, version 1.2015. J Natl Compr Cancer Netw. 2015;13:78–108.
Jann H, Denecke T, Koch M, et al. Impact of octreotide long-acting release on tumour growth control as a first-line treatment in neuroendocrine tumours of pancreatic origin. Neuroendocrinology. 2013;98:137–43.
Kunz PL. Carcinoid and neuroendocrine tumors: building on success. JCO. 2015;33:1855–63.
Ricci S, Antonuzzo A, Galli L, et al. Octreotide acetate long-acting release in patients with metastatic neuroendocrine tumors pretreated with lanreotide. Ann Oncol. 2000;11:1127–30.
Rinke A, Müller H, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID study group. J Clin Oncol. 2009;27:4656–63.
Caplin ME, Pavel M, Ćwikła JB, et al. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371:224–33.
Rosenoff SH, Gabrail NY, Conklin R, et al. A multicenter, randomized trial of long-acting octreotide for the optimum prevention of chemotherapy-induced diarrhea: results of the STOP trial. J Support Oncol. 2006;4:289–94.
Anthony L, Vinik AI. Evaluating the characteristics and the management of patients with neuroendocrine tumors receiving octreotide LAR during a 6-year period. Pancreas. 2011;40:987–94.
Ruszniewski P, Ish-Shalom S, Wymenga M, et al. Rapid and sustained relief from the symptoms of carcinoid syndrome: results from an open 6-month study of the 28-day prolonged-release formulation of lanreotide. Neuroendocrinology. 2004;80:244–51.
Ludlam WH, Anthony L. Safety review: dose optimization of somatostatin analogs in patients with acromegaly and neuroendocrine tumors. Adv Ther. 2011;28:825.
Chadha MK, Lombardo J, Mashtare T, et al. High-dose octreotide acetate for management of gastroenteropancreatic neuroendocrine tumors. Anticancer Res. 2009;29:4127–30.
Broder MS, Beenhouwer D, Strosberg JR, et al. Gastrointestinal neuroendocrine tumors treated with high dose octreotide-LAR: a systematic literature review. World J Gastroenterol. 2015;21:1945–55.
Wolin EM, Jarzab B, Eriksson B, et al. Phase III study of pasireotide long-acting release in patients with metastatic neuroendocrine tumors and carcinoid symptoms refractory to available somatostatin analogues. Drug Des Dev Ther. 2015;9:5075–86.
Yao JC, Shah MH, Ito T, et al. Everolimus for advanced pancreatic neuroendocrine tumors. N Engl J Med. 2011;364:514–23.
Raymond E, Dahan L, Raoul J, et al. Sunitinib malate for the treatment of pancreatic neuroendocrine tumors. N Engl J Med. 2011;364:501–13.
Halperin DM, Shen C, Dasari A, et al. Frequency of carcinoid syndrome at neuroendocrine tumour diagnosis: a population-based study. Lancet Oncol. 2017;18:525–34.
Shen C, Xu Y, Dasari A, et al. Octreotide LAR dosage and survival among elderly patients with distant-stage neuroendocrine tumors. Oncologist. 2016;21:308–13.
Al-Efraij K, Aljama MA, Kennecke HF. Association of dose escalation of octreotide long-acting release on clinical symptoms and tumor markers and response among patients with neuroendocrine tumors. Cancer Med. 2015;4:864–70.
Strosberg JR, Benson AB, Huynh L, et al. Clinical benefits of above-standard dose of octreotide LAR in patients with neuroendocrine tumors for control of carcinoid syndrome symptoms: a multicenter retrospective chart review study. Oncologist. 2014;19:930–6.
Ferolla P, Faggiano A, Grimaldi F, et al. Shortened interval of long-acting octreotide administration is effective in patients with well-differentiated neuroendocrine carcinomas in progression on standard doses. J Endocrinol Invest. 2012;35:326–31.
Strosberg J, El-Haddad G, Wolin E, et al. Phase 3 trial of 177Lu-dotatate for midgut neuroendocrine tumors. N Engl J Med. 2017;376:125–35.
Funding
None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declared that they have no competing interest.
Ethical approval
All procedures performed in this study involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Specifically, the Health Research Ethics Board (HREB) approved this study before its conduct.
Informed consent
Because this study was a secondary analysis of retrospective data, there was no direct contact with any participants. Therefore, informed consent was waived by the ethics committee.
Rights and permissions
About this article
Cite this article
Lau, S.C., Abdel-Rahman, O. & Cheung, W.Y. Improved survival with higher doses of octreotide long-acting release in gastroenteropancreatic neuroendocrine tumors. Med Oncol 35, 123 (2018). https://doi.org/10.1007/s12032-018-1189-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-018-1189-1