Abstract
The purpose of this study was to evaluate the efficacy of cabazitaxel for patients with metastatic castration-resistant prostate cancer (mCRPC) after sequential therapy with docetaxel (DTX) and single or dual regimens of novel androgen receptor-axis-targeted (ARAT) agents. We retrospectively reviewed 84 consecutive patients treated with cabazitaxel at Kobe University Hospital and related hospitals from September 2014 to September 2016. The association of each prognostic parameter with progression-free survival (PFS) was evaluated, including the sequence of therapy. Patients were divided according to their treatment after receiving cabazitaxel as follows: group 1 (after DTX and single regimen of novel ARAT agent) and group 2 (after DTX and dual novel ARAT agents). Median PFS for cabazitaxel treatment was 10.3 months (range 4.5–14.2 months). Prostate-specific antigen (PSA) response rates (≥30%) were 46.8 and 46.1% in group 1 and group 2, respectively [p = 0.96, hazard ratio (HR) 1.02, 95% confidence interval (CI) 0.57–1.80]. PSA response rates (≥50%) were 43.8 and 26.9% in patients of group 1 and group 2, respectively (p = 0.18, HR 1.54, 95% CI 0.78–3.04). Univariate analysis revealed that PFS for cabazitaxel treatment was significantly associated with baseline alkaline phosphatase, bone metastasis, and prior sequential therapy. Multivariate analysis revealed that bone metastasis and prior sequential therapy were independently associated with PFS. Prior sequential therapy with single regimen or dual regimens of novel ARAT agents was independently associated with PFS of patients with mCRPC treated with cabazitaxel. The effect of cabazitaxel after the administration of DTX and single novel ARAT agent was more sustained.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Approved life-prolonging therapies employing chemotherapy and novel androgen receptor-axis-targeted (ARAT) agents are available for patients with castration-resistant prostate cancer (CRPC) [1]. Cabazitaxel, a second-generation taxane, was approved by the U.S. Food and Drug Administration (FDA) in June 2010 as a treatment option for patients with metastatic CRPC (mCRPC) previously treated with docetaxel (DTX).
However, insufficient data are available to indicate the efficacy of cabazitaxel following sequential therapy including DTX and novel ARAT agents though some investigators found that cabazitaxel may maintain clinical activity after sequential therapy [2]. Here, we addressed the differences in efficacy of cabazitaxel administered to patients with mCRPC after they were treated with DTX and novel ARAT agents.
Patients and methods
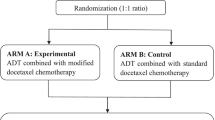
This study was conducted under institutional review board (IRB) approval of Kobe University Hospital (approval No. 1470). After institutional review board approval, records from 84 consecutive patients treated with cabazitaxel at Kobe University Hospital and affiliated hospitals were reviewed. All patients had received DTX. Treatment with cabazitaxel was initiated from September 2014 to September 2016 and was administered after DTX and single or dual novel ARAT agents. Patients were classified according to the timing of treatment with cabazitaxel as follows: group 1 (pretreated with a single ARAT regimen) and group 2 (pretreated with dual regimens of ARAT). Each ARAT agent (abiraterone and enzalutamide) was not administered again after discontinuing therapy using the same agents.
Patients’ background characteristics, laboratory data, clinical symptoms, treatment history, clinical stage of prostate cancer before cabazitaxel, and prognostic profiles during chemotherapy with DTX were recorded. Clinical staging was determined according to the American Joint Committee on Cancer classification, considering pathological examination of specimens from transurethral resection, computed tomography, magnetic resonance imaging, and bone scans. During treatment with cabazitaxel, the Common Terminology Criteria in Adverse Events (version 4.0) were used to report hematological or nonhematological toxicity. Toxic effects were reported from the introduction of cabazitaxel to introduction of the next sequential therapy.
Patients were evaluated after receiving a single cycle of cabazitaxel, and an increase in the levels of PSA preceding this first evaluation was considered flare if followed by a decrease in PSA. Levels of PSA were measured before the start of each treatment cycle. Progression-free survival (PFS) was defined as time from initiation of cabazitaxel to disease progression (radiologic, PSA, clinical progression, or a combination; or death from any cause). PSA progression was defined as a PSA increase ≥25% compared the nadir of baseline PSA levels. Before initiating treatment, laboratory and clinical data were recorded, including the baseline levels of PSA, hemoglobin (Hb), lactate dehydrogenase, alkaline phosphatase (ALP), and Eastern Corporative Oncology Group Performance Status (ECOG PS). During the administration of any line of therapy, a PSA response was defined as a ≥30 or ≥50% decrease in PSA compared with baseline levels.
Statistical analysis
The association of each prognostic parameter on PFS was evaluated using univariate and multivariate analyses. All statistical analyses were performed using JMP version 13.0 (SAS Institute, Cary, NC, USA), and p < 0.05 indicates a significant difference. Differences in multiple parameters were compared using an unpaired t test or the χ 2 test. Progression-free survival (PFS) and overall survival (OS) were calculated using the Kaplan–Meier method, and the significance of differences was determined using the log-rank test. The prognostic significance of a factor was assessed using the Cox proportional hazards regression model.
Results
A summary of patients and treatment characteristics is shown in Table 1. Upon initiation of cabazitaxel treatment, patients in group 1 had better performance status (p = 0.01, HR 6.26, 95% CI 1.23–31.73), lower PSA levels (p < 0.01, HR 5.05, 95% CI 1.75–14.57) and Hb levels (p = 0.04, HR 1.63, 95% CI 1.00–2.68). Other baseline factors did not significantly differ between the two treatment groups. In group 1, 14 (41.1%) and 20 patients (58.8%) received abiraterone and enzalutamide as prior AR-targeted therapy, respectively. In group 2, 29 patients (90.6%) received continuous therapy with dual regimens of novel ARAT agents after DTX.
The median PFS was 10.3 months (range 4.5–14.2 months), and the median PFSs of groups 1 and 2 were 11.7 and 7.9 months (p = 0.03), respectively (Fig. 1). Disease progression and mortality occurred in 33 (48.4%) and 15 patients (22.7%), respectively.
PSA response rates ≥30% in groups 1 and 2 were 46.8 and 46.1%, respectively (p = 0.96, HR 1.02, 95% CI 0.57–1.80) (Table 2). PSA response rates ≥50% were 43.8 and 26.9% in groups 1 and 2, respectively (p = 0.18, HR 1.54, 95% CI 0.78–3.04). A waterfall plot of the best PSA response is shown in Fig. 2. The red and blue columns represent patients in groups 1 and 2, respectively. The 6, 12, and 18-month PFS rates of patients in group 1 were 79.5, 61.4, and 26.3% and 44.5, 32.5, and 16.2% in group 2, respectively.
During treatment with cabazitaxel, most patients experienced toxicities (Table 2). Of 66 patients analyzed, 64.7 and 71.9% of patients in groups 1 and group 2, experienced neutropenia, respectively, which was the most common hematotoxicity. Furthermore, 14.7 and 18.8% patients in groups 1 and 2 experienced fatal febrile neutropenia, respectively. In contrast, 70.6 and 71.9% patients in groups 1 and 2 experienced nonhematological toxicities such as diarrhea, fatigue, nausea, alopecia, edema, and hepatopathy. There were no significant differences in toxicities experienced by each group.
Univariate analysis revealed that PFS was significantly associated with ALP at baseline, bone metastasis, and the number of prior treatments with novel ARAT agents (Table 3). Furthermore, multivariate analysis revealed that the latter and bone metastasis were independently associated with PFS.
Discussion
In July 2010, the FDA approved cabazitaxel, which is a second-generation taxane that improves survival of patients with progressive mCRPC previously treated with DTX. The TROPIC open-label randomized phase 3 trial of cabazitaxel found that cabazitaxel can prolong OS by 2.4 months compared with mitoxantrone (15.1 vs 12.7 months) [3].
There are clinically approved life-prolonging therapies other than cabazitaxel, such as novel ARAT agents for treating patients with CRPC. However, insufficient data are available, indicating the efficacy of sequential therapy using these new agents. For example, Sonpavde et al. conducted a retrospective study of 350 men previously treated with DTX and found that OS was significantly longer when cabazitaxel was used versus abiraterone in a first-line setting after DTX (p = 0.02, HR 0.13, 95% CI 0.02–0.73) [4]. Wissing et al. compared patients who received DTX, followed by cabazitaxel and then abiraterone, with those who received DTX, followed by abiraterone and then cabazitaxel [5]. Patients treated with cabazitaxel in a first-line setting after DTX experienced longer PFS (9.5 vs 7.7 months, p = 0.02), although there was no significant difference in OS between groups. The retrospective study of Maines et al. suggests that patients treated with cabazitaxel in a first-line setting after DTX experience longer OS compared with patients treated with cabazitaxel in a second-line setting, after treatment with DTX and one novel ARAT agent (76.4 vs 61.3%) [6].
Other investigators evaluated the efficacy of cabazitaxel administered after treatment with DTX and single novel ARAT agent. For example, Nakouzi et al. found that OS and PFS of 79 patients with CRPC, who had progressed after treatment with DTX and abiraterone, were 10.9 and 4.4 months, respectively, and that 35% of patients treated with cabazitaxel exhibited 50% PSA responses [2]. Therefore, these data indicate that cabazitaxel maintains clinical activity to a certain extent even after patients received DTX and one novel AR-targeting agent.
At the St Gallen Conference held in 2015, 73% of panel members recommended cabazitaxel in a third-line setting after second-line DTX (post-first-line novel ARAT agent) [7]. Chi et al. used a treatment algorithm based on available prospective and retrospective data and found that cabazitaxel was administered in the setting of post-DTX and novel ARAT agent to most patients with CRPC [8]. In contrast, the Clinical Practice Guidelines in Oncology recommend administration of cabazitaxel to patients with mCRPC after treatment with DTX (category 1) [9]. Consequently, when patients receive sequential therapy with CRPC, cabazitaxel is often used after DTX and single regimen of a novel ARAT agent or the latter alone. However, some patients hesitate and reject chemotherapy because of its adverse effects, although chemotherapy is their only option. Cabazitaxel is therefore sometimes administered to patients after DTX and dual regimens of novel androgen-directed agents. However, the efficacy of cabazitaxel in such a setting requires further study.
Insufficient data are available that help determine the efficacy of cabazitaxel administered after patients are treated with dual novel ARAT agents. For example, Pezaro et al. evaluated the effectiveness of cabazitaxel prior to treatment with abiraterone with or without enzalutamide for patients with mCRPC treated with first-line DTX. The statistical significance of the effects of cabazitaxel was not evaluated because only five patients were treated with cabazitaxel after DTX and dual novel ARAT agents [10]. Few published reports evaluated the difference of the efficacy of cabazitaxel after DTX and single regimen or dual regimens of novel ARAT agents.
In the present study, we analyzed numerous factors, including the sequence of therapy that influenced the effectiveness of cabazitaxel. Parameters that effect OS or PFS were analyzed by others. For example, Meisel reported that severe neutropenia is an adverse effect caused by treatment with cabazitaxel and is independently associated with OS of patients with mCRPC [11]. Halabi et al. found that Hb levels before cabazitaxel, the length of standard hormone therapy, and ECOG PS are related to OS [12]. Accordingly, we analyzed factors that influenced PFS of patients with mCRPC. Our study confirms that the timing of treatment with cabazitaxel is an important prognostic factor of PFS. Early use of cabazitaxel leads to treatment with novel AR-targeting agents of patients with CRPC who are heavily pretreated. In contrast, Badrising et al. found that late use of enzalutamide achieves a 23% response rate, suggesting the efficacy of late use of novel ARAT agents [13]. These data support the early use of cabazitaxel.
In the present study, there was a lower frequency of neutropenia compared with the TROPIC trial [3]. The administration of pegylated granulocyte colony-stimulating factor (PEG-G-CSF) may suppress neutropenia (Table 2). In contrast, febrile neutropenia and nonhematological affects were not less frequent compared with those reported by the TROPIC trial [3]. It is important therefore to closely monitor patients during treatment with cabazitaxel, although death caused by cabazitaxel is unreported.
The present study has several limitations. First, this was a retrospective study with a relatively short observation period. Second, tolerability and response to previous treatment may have influenced the choice of treatment among patients unfit for early treatment with cabazitaxel. Third, this study did not detect a significant difference in OS. Nevertheless, to the best of our knowledge, the present study is the first to evaluate the efficacy of cabazitaxel “after cross-resistance.”
Conclusions
Our data suggest that the sequence of new therapeutic agents was independently associated with PFS of patients with mCRPC who were treated with cabazitaxel. Despite equivalent PSA responses, the effects of cabazitaxel administered after treatment with single regimen of novel ARAT agent and DTX may be more sustained. Further investigations and prospective studies are required to develop the optimal sequential therapy of patients with CRPC.
References
Cornford P, Bellmunt J, Bolla M, Briers E, Santis MD, Gross T, et al. EAU-ESTRO-SIOG guidelines on prostate cancer. Part II: treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur Urol. 2017;71:630–42.
Al Nakouzi N, Le Moulec S, Albigès L, Wang C, Beuzeboc P, Gross-Goupil M, et al. Cabazitaxel remains active in patients progressing after docetaxel followed by novel androgen receptor pathway targeted therapies. Eur Urol. 2015;68:228–35.
De Bono JS, Oudard S, Ozguroglu M, Hansen S, Machiels JP, Kocak I, et al. Prednisone plus cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomized open-label trial. Lancet. 2010;376:1147–54.
Sonpavde G, Bhor M, Hennessy D, Bhowmik D, Shen L, Nicacio L, et al. Sequencing of cabazitaxel and abiraterone acetate after docetaxel in metastatic castration-resistant prostate cancer: treatment patterns and clinical outcomes in multicenter community-based US oncology practices. Clin Genitourin Cancer. 2015;13:309–18.
Wissing MD, Coenen JL, Van Den Berg P, Westgeest HM, van den Eerwegh AJ, van Oort IM, et al. CAST: a retrospective analysis of cabazitaxel and abiraterone acetate sequential treatment in patients with metastatic castrate-resistant prostate cancer previously treated with docetaxel. Int J Cancer. 2015;136:E760–72.
Maines F, Caffo O, Veccia A, Trentin C, Tortora G, Galligioni E, et al. Sequencing new agents after docetaxel in patients with metastatic castration-resistant prostate cancer. Crit Rev Oncol Hematol. 2015;96:498–506.
Gillessen S, Omlin A, Attard G, de Bono JS, Efstathiou E, Fizazi K, et al. Management of patients with advanced prostate cancer: recommendations of the St. Gallen Advanced Prostate Cancer Consensus Conference (APCCC) 2015. Ann Oncol. 2015;26:1589–604.
Chi K, Hotte SJ, Joshua AM, North S, Wyatt AW, Collins LL, et al. Treatment of mCRPC in the AR-axis-targeted therapy-resistant state. Ann Oncol. 2015;26:2044–56.
Mohler JL, Armstrong AJ, Bahnson RR, D’Amico AV, Davis BJ, Eastham JA, et al. Prostate Cancer, Version 1.2016. J Natl Compr Cancer Netw. 2016;14:19–30.
Pezaro CJ, Omlin AG, Altavilla A, Lorente D, Ferraldeschi R, Bianchini D, et al. Activity of cabazitaxel in castration-resistant prostate cancer progressing after docetaxel and next-generation endocrine agents. Eur Urol. 2014;66:459–65.
Meisel A, von Felten S, Vogt DR, Liewen H, de Wit R, de Bono J, et al. Severe neutropenia during cabazitaxel treatment is associated with survival benefit in men with metastatic castration-resistant prostate cancer (mCRPC): a post hoc analysis of the TROPIC phase III trial. Eur J Cancer. 2016;56:93–100.
Halabi S, Lin CY, Small EJ, Armtrong AJ, Kaplan EB, Petrylak D, et al. Prognostic model predicting metastatic castration-resistant prostate cancer survival in men treated with second-line chemotherapy. J Natl Cancer Inst. 2013;105:1729–37.
Badrising SK, van der Noort V, Hamberg P, Coenen JL, Aarts MJ, van Oort IM, et al. Enzalutamide as a fourth-or fifth-line treatment option for metastatic castration-resistant prostate cancer. Oncology. 2016;91:267–73.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was waived for individual participants included in the study given the retrospective nature of this work and in accordance with the institutional review board.
Rights and permissions
About this article
Cite this article
Bando, Y., Hinata, N., Terakawa, T. et al. Activity of cabazitaxel in patients with metastatic castration-resistant prostate cancer after treatment with single or dual regimens of novel androgen receptor-targeting agents. Med Oncol 34, 163 (2017). https://doi.org/10.1007/s12032-017-1024-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-017-1024-0