Abstract
Lack of effective biomarkers is one of the challenges in current chemotherapy to predict drug response and sensitivity. This study was carried out to investigate the relationships between the expressions of class III β-tubulin, microtubule-associated protein tau (MAPT), survivin, and the sensitivity of primary gastric cancer (GC) to paclitaxel treatment. Reverse transcription PCR and Western blot were used to evaluate the mRNA and protein expressions of class III β-tubulin, MAPT, and survivin in fifty-four GC tissues. Viable tumor cells from gastric carcinomas were tested for their sensitivity to paclitaxel using adenosine triphosphate-based tumor chemosensitivity assay in vitro. Out of 54 samples, 30 samples were sensitive to paclitaxel, while the other 24 samples were resistant. The overall efficacy of paclitaxel was 55.56 % (30/54). The mRNA expressions of class III β-tubulin and survivin were significantly correlated with the histological grade (P = 0.029, 0.009, respectively). The sensitivity of GC patients to paclitaxel treatment was inversely correlated with the mRNA and protein expressions of class III β-tubulin (P < 0.01), MAPT (P < 0.05), and survivin (P < 0.05). A significant positive correlation was found between class III β-tubulin and MAPT expression at mRNA and protein levels (mRNA: P = 0.037; protein: P = 0.001). Our results indicate that the expression levels of class III β-tubulin, MAPT, and survivin are good biomarkers for predicting the sensitivity of GC to paclitaxel treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is one of the most aggressive diseases in gastrointestinal oncology worldwide. The worldwide incidence of GC has declined rapidly in recent few decades, but the rate of decline is variable in different regions [1]. The prognosis of GC is poor because most patients are diagnosed at the advanced stage. Surgery is the mainstay for the treatment of resectable GC, but the recurrence of GC is often seen in most advanced GCs even after a complete resection. Therefore, the combination of surgery with chemo and/or radiotherapy has become the established treatment for locally advanced GCs. Currently, several acceptable perioperative chemotherapy regimens are used for the treatment of locally advanced GCs. Paclitaxel, as an important anticancer drug, has been widely used and achieved some good results in treating GCs. However, the efficacy and side effects of paclitaxel vary between individual patients. Thus, it is necessary to screen some biomarkers for predicting the sensitivity of GC patients to paclitaxel, thus maximizing antitumor effect but minimizing the toxicity of paclitaxel treatment.
Taxane plays a role in cell apoptosis by binding to β-tubulin and exerts the growth-inhibitory effect through the induction of cell cycle arrest at G2/M phase [2, 3]. Class III β-tubulin is a kind of tubulin that impairs the microtubule stability, and its high expression reduces the chemosensitivity of many cancers to taxane [4–7]. Tau, as one of the microtubule-associated proteins, promotes cytoskeletal microtubule polymerization and stability and regulates tubulin dynamics. Tau is widely expressed in many tissues, mostly in neurons and glial cells. Recent studies demonstrated that the overexpression of microtubule-associated protein tau (MAPT) may result in drug resistance to microtubule targeting agents and is associated with the resistance to taxane-related chemotherapies [8–10].
Survivin, a member of the family of inhibitor of apoptosis proteins (IAPs), functions as a pivotal regulator of mitosis and programmed cell death. Survivin specifically combines with spindle microtubules, inhibits cell apoptosis, enhances cell proliferation, and promotes angiogenesis [11–13]. It is highly expressed in a board range of solid tumors and hematological malignancies, but is not found in most terminally differentiated cells [14]. Previous evidences demonstrated that increased survivin expression is associated with a low sensitivity to paclitaxel and an unfavorable prognosis of various malignancies including breast, lung, and GCs [15–17].
In the present study, we investigated the relationships between the expressions of class III β-tubulin, MAPT, survivin, and the sensitivity of GCs to paclitaxel treatment in order to identify the biological predictors to chemosensitivity and guide clinical individual chemotherapy. Drug sensitivity was evaluated by adenosine triphosphate-based tumor chemosensitivity assay (ATP-TCA), while the mRNA and protein expressions of class III β-tubulin, MAPT, and survivin were examined by RT-PCR and Western blot.
Materials and methods
Patients and specimens
All fifty-four GC specimens and relevant clinical data were obtained from the Department of Gastrointestinal Surgery, the First Affiliated Hospital of Nanjing Medical University (Nanjing, China), between May 2008 and April 2009. All patients were not treated with chemotherapy or radiotherapy before surgery. Clinicopathological characteristics of the patients are summarized in Table 1. All specimens included in this study were classified as adenocarcinomas by the experienced pathologists. The histological classification and grading were performed according to the standards of national GC. This study was approved by the Ethics Committee of Institute. Informed consent was obtained from all subjects in accordance with the Declaration of Helsinki. Tumor tissues were collected during primary surgery and divided into two parts. One fresh part was used for ATP-TCA, while the other was frozen and used for the detection of mRNA and protein expressions.
ATP-TCA
The ATP-TCA was performed within 24 h after surgery as previously described [18–20]. Briefly, the fresh tumor tissues were placed into RPMI 1640 medium containing 100 IU/ml penicillin, 100 μg/ml streptomycin, and 2.5 μg/ml amphotericin B. After enzymatic dissociation, tumor cells were washed in serum-free complete assay medium and purified by density centrifugation to remove debris. Approximately 2 × 104 cells were seeded into each well of a 96-well polypropylene microplate. Paclitaxel was tested at six dilutions corresponding to 6.25, 12.5, 25, 50, 100, and 200 % of a standard tumor drug concentration (TDC) (100 % TDC of paclitaxel is 50 μg/ml). As controls, one row wells of each plate were only incubated with complete medium (M0), while one row wells were treated with maximum ATP inhibitor. Hundred microliters of complete medium with or without paclitaxel was added to each well and incubated for 6 days at 37 °C with 5 % CO2. ATP was extracted with tumor cell extraction reagent (DCS, Innovative Diagnostik systeme, Hamburg, Germany) and measured by microplate luminometer (Berthod Diagnostic system, Germany). A sensitivity index ranging from 0 to 600 was calculated by summing up the percentage of cell viability at six drug concentrations [21]. Thus, a sensitivity index of 0 indicates maximum drug sensitivity, whereas a sensitivity index of 600 is minimum drug sensitivity.
Four categories of ex vivo sensitivity were defined as follows: (a) high sensitivity, IC90 ≤ 90 % TDC, IC50 ≤ 25 % TDC, index < 300; (b) partial sensitivity, IC90 > 90 % TDC, IC50 ≤ 25 % TDC, index < 300; (c) weak sensitivity, index < 300; and (d) resistance, index ≥ 300 [22, 23].
RNA isolation and RT-PCR
Total RNA was extracted from frozen gastric carcinoma tissues using Trizol (Invitrogen, Grand Island, NY) following the manufacturer’s protocols. One microgram of RNA was transcribed into cDNA using Exscript™ RT reagent Kit (TaKaRa) according to the manufacturer’s instructions. The primers for RT-PCR were as follows: class III β-tubulin (sense: 5′-AGCAAGGTGCGTGAGGAGTA-3′, antisense: 5′-AAGCCGGGCATGAAGAAGT-3′), with a product size of 353 bp; MAPT (sense: 5′-GGCTCATTAGGCAACATCC-3′, antisense: 5′-AGCTGGGGCGAGTCTACCAT-3′), with a product size of 308 bp; survivin (sense: 5′-TGTCAGCCCAACCTTCACAT-3′, antisense: 5′-AAACAGGTCTGGGGTTCGTG-3′), with a product size of 406 bp; internal control β-actin (sense: 5′-GTTGCGTTACACCCTTTCTT-3′, antisense: 5′- ACCTTCACCGTTCCAGTTT-3′), with a product size of 147 bp. PCR was performed following the manufacturer’s instructions. The cycling conditions were 5 min at 94 °C, followed by 30 cycles of denaturation at 94 °C for 30 s, annealing at 55 °C for 30 s, and extension at 70 °C for 30 s. Amplified DNA fragments were resolved by electrophoresis on 1.5 % agarose gel containing ethidium bromide. The expression levels of class III β-tubulin, MAPT, and survivin were normalized to the β-actin expression.
Western blot
Frozen tumor tissues were minced in RIPA lysis buffer. Protein concentration was determined by BCA assay. Forty micrograms of total proteins of each sample were separated on 10 % (class III β-tubulin, MAPT) or 12 % (survivin) SDS-PAGE gels and transferred onto nitrocellulose membrane (Roche, USA). The membranes were blocked in 5 % non-fat milk for 1 h at room temperature and then immunoblotted with specific antibodies against class III β-tubulin (Santa Cruz, 1:200), MAPT (Bioworld, 1:500), survivin (Cell Signaling, 1:500), and GAPDH (KangChen Bio-tech, 1:2000) at 4 °C overnight. The membranes were incubated with horseradish peroxidase (HRP)-conjugated goat anti-mouse IgG (Santa Cruz, 1:2000) secondary antibody for 1 h at room temperature. The blots were detected by enhanced chemiluminescence reagent (Amersham Pharmacia Biotechnology, USA) and analyzed using Quantity One software (Bio-Rad, USA).
Statistical analysis
All statistical analyses were performed using SPSS 16.0. Data are presented as mean ± standard deviation (SD). The correlation between gene expressions levels and clinicopathological data was analyzed using the Student’s t test and one-way ANOVA. χ 2 test was used to evaluate the relationship between drug sensitivity and clinicopathological data. Spearman correlation coefficient was used to analyze the correlation between their expression levels and drug sensitivity. All values are presented based on two-tailed statistical analysis. P < 0.05 was considered to be statistically significant.
Results
Drug sensitivity of GCs to paclitaxel treatment
ATP-TCA was used to detect the sensitivity of GCs to paclitaxel treatment. Among total 54 patients, 6 patients were highly sensitive, 14 patients were partly sensitive, 10 patients were weakly sensitive, and other 24 cases were resistant. The overall efficacy of paclitaxel treatment was 55.56 % (30/54). The sensitivity of GCs to paclitaxel was not related with gender, age, histological grade, and lymph node metastasis (P > 0.05, Table 2).
Gene expression of class III β-tubulin, MAPT, and survivin in GC tissues
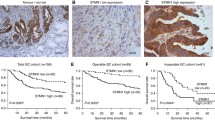
The mRNA expression levels of class III β-tubulin, MAPT, and survivin were examined by RT-PCR, and representative electrophoresis graph was shown in Fig. 1. Statistical analysis revealed that moderately differentiated GC tissues had significantly lower levels of class III β-tubulin and survivin than the poorly differentiated GC tissues (P = 0.029 and P = 0.009, respectively) (Table 3). There were no significant differences in the mRNA expressions of class III β-tubulin, MAPT, and survivin in consideration of gender, age, tumor depth, or lymph node metastasis (P > 0.05).
The relationships between the chemosensitivity to paclitaxel and the mRNA and protein expressions of class III β-tubulin, MAPT, and survivin
Figure 2 showed a typical protein electrophoresis graph. Spearman correlation coefficient was applied to analyze the relationships between the chemosensitivity to paclitaxel and the mRNA and protein expressions of class III β-tubulin, MAPT, and survivin. A significant inverse correlation was observed between the mRNA and protein expressions of class III β-tubulin and chemosensitivity of GC to paclitaxel (mRNA: r = 0.375, P = 0.005, Fig. 3A; protein: r = 0.367, P = 0.006, Fig. 3B). Patients with lower class III β-tubulin expression levels had a higher sensitivity to paclitaxel. As shown in Fig. 3C and D, the mRNA and protein levels of MAPT were inversely correlated with the chemosensitivity to paclitaxel treatment (mRNA: r = 0.301, P = 0.027; protein: r = 0.281, P = 0.040). Moreover, we observed that the survivin mRNA and proteins levels were inversely correlated with the chemosensitivity to paclitaxel treatment (mRNA: r = 0.333, P = 0.014, Fig. 3E; protein: r = 0.288, P = 0.035, Fig. 3F). We further noticed that the mRNA and protein expressions of class III β-tubulin were positively correlated with those of MAPT (mRNA: r = 0.284, P = 0.037; protein: r = 0.440, P = 0.001).
The relationships between the paclitaxel sensitivity index and expression levels of class III β-tubulin, MAPT, and survivin in 54 GC samples. A sensitivity index of 0 indicates maximum drug sensitivity, whereas a sensitivity index of 600 refers to minimum drug sensitivity. The mRNA (a) and protein (b) levels of class III β-tubulin were positively correlated with the resistance to paclitaxel (mRNA: r = 0.375, P = 0.005; protein: r = 0.367, P = 0.006). The mRNA (c) and protein (d) levels of MAPT were positively correlated with the resistance to paclitaxel (mRNA: r = 0.301, P = 0.027; protein: r = 0.281, P = 0.040). The mRNA (e) and protein (f) expression levels of survivin were positively correlated with the resistance to paclitaxel (mRNA: r = 0.333, P = 0.014; protein: r = 0.288, P = 0.035)
Discussion
In the present study, we investigated the relationships between the expressions of class III β-tubulin, MAPT, survivin, and the chemosensitivity of GCs to paclitaxel treatment. ATP-TCA technique has been widely used to evaluate cell viability through the measurement of luciferin–luciferase (Lu–Lu) bioluminescence reaction [24–26]. Moreover, this technique has been successfully applied to a number of different tumor entities such as ovarian, breast, colorectal, gastric, lung cancer, and malignant melanoma [27–30]. Here, we used ATP-TCA assay to examine the chemosensitivity of cells derived from human GC tissues to paclitaxel treatment, and we observed that more than half of the GC patients were sensitive to this chemotherapy drug with varying intensity. However, chemosensitivity results from an in vitro research cannot be directly translated into clinical practice because there are complex factors in vivo to determine the response to chemotherapy.
In the present study, we found that class III β-tubulin and MAPT were widely expressed in gastric carcinoma tissues. However, there was no significant correlation between these two biomarkers and the clinicopathological parameters, except for the expression of class III β-tubulin mRNA and histological grades. Low-level class III β-tubulin expression was associated with a better differentiation, which is considered as a predictive marker for prognosis. Moreover, we observed a clear relationship between the expression of class III β-tubulin and MAPT and the chemosensitivity to paclitaxel. High levels of class III β-tubulin and MAPT were associated with the reduced response of GCs to paclitaxel chemotherapy, indicating that paclitaxel might easily combine with tubulin and induce cell apoptosis under lower levels of class III β-tubulin and MAPT. The high levels of class III β-tubulin and MAPT may contribute to stabilize microtubules and promote mitosis, reducing the killing effect of paclitaxel, which leads to chemoresistance. The similar observations have been found in a number of malignancies including lung [31], ovarian [32], and breast [8] cancer. In addition, class III β-tubulin expression was positively correlated with MAPT expression both in mRNA and protein level. Thus, we speculate that these two proteins might have synergistic effect on inducing paclitaxel resistance through the influence on the microtubule-associated structures, which needs further study.
Survivin, the smallest member of the IAP family, is one of the most cancer-specific proteins and is dysregulated in almost all human tumors. Overexpression of survivin also correlates with tumor progression and induces anticancer drug resistance. Here, we found that survivin was constantly expressed in all of the GC tissues, and lower expression level of survivin was correlated with better response to paclitaxel chemotherapy. This finding is consistent with the previous report [15], indicating that survivin is a reliable biomarker for predicting chemosensitivity of GC to paclitaxel therapy. Antisense survivin RNA can induce apoptosis in GC cells and increase docetaxel-induced cytotoxicity by decreasing mdr-1 [33]. Consistent with the observation in resent research [34], we observed that moderately differentiated GC tissues had lower expression of survivin than the poorly differentiated ones, suggesting that overexpression of survivin might be an unfavorable prognostic indicator in GC.
Since a large number of previous studies on tumor sensitivity to chemotherapy were carried out at a single level of either gene or protein expression, and the accurate experimental methods were relatively rare. Using ATP-TCA technique, here we observed the association between the chemosensitivity of GCs to paclitaxel treatment and the expressions of class III β-tubulin, MAPT, and survivin at both mRNA and protein levels and drew the consistent trend on the two levels. These results would provide strong evidences for clinical practice.
In conclusion, the mRNA and protein levels of class III β-tubulin, MAPT, and survivin were correlated with the chemosensitivity of GCs to paclitaxel treatment in the ex vivo study. Lower expression of class III β-tubulin, MAPT, and survivin is associated with higher susceptibility to paclitaxel treatment. Combined detection of these three biomarkers may contribute to the improvement of GC to paclitaxel chemotherapy, although further investigations on a large number of samples are needed before clinical practice.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
El-Kareh AW, Labes RE, Secomb TW. Cell cycle checkpoint models for cellular pharmacology of paclitaxel and platinum drugs. AAPS J. 2008;10(1):15–34.
Seve P, Mackey J, Isaac S, Tredan O, Souquet PJ, Perol M, et al. Class III beta-tubulin expression in tumor cells predicts response and outcome in patients with non-small cell lung cancer receiving paclitaxel. Mol Cancer Ther. 2005;4(12):2001–7.
Mozzetti S, Ferlini C, Concolino P, Filippetti F, Raspaglio G, Prislei S, et al. Class III beta-tubulin overexpression is a prominent mechanism of paclitaxel resistance in ovarian cancer patients. Clin Cancer Res. 2005;11(1):298–305.
Dumontet C, Isaac S, Souquet PJ, Bejui-Thivolet F, Pacheco Y, Peloux N, et al. Expression of class III beta tubulin in non-small cell lung cancer is correlated with resistance to taxane chemotherapy. Bull Cancer. 2005;92(2):E25–30.
Seve P, Reiman T, Isaac S, Trillet-Lenoir V, Lafanechere L, Sawyer M, et al. Protein abundance of class III beta-tubulin but not delta2-alpha-tubulin or tau is related to paclitaxel response in carcinomas of unknown primary site. Anticancer Res. 2008;28(2B):1161–7.
Tommasi S, Mangia A, Lacalamita R, Bellizzi A, Fedele V, Chiriatti A, et al. Cytoskeleton and paclitaxel sensitivity in breast cancer: the role of beta-tubulins. Int J Cancer. 2007;120(10):2078–85.
Andre F, Hatzis C, Anderson K, Sotiriou C, Mazouni C, Mejia J, et al. Microtubule-associated protein-tau is a bifunctional predictor of endocrine sensitivity and chemotherapy resistance in estrogen receptor-positive breast cancer. Clin Cancer Res. 2007;13(7):2061–7.
Mimori K, Sadanaga N, Yoshikawa Y, Ishikawa K, Hashimoto M, Tanaka F, et al. Reduced tau expression in gastric cancer can identify candidates for successful paclitaxel treatment. Br J Cancer. 2006;94(12):1894–7.
Smoter M, Bodnar L, Duchnowska R, Stec R, Grala B, Szczylik C. The role of tau protein in resistance to paclitaxel. Cancer Chemother Pharmacol. 2011;68(3):553–7.
Kamihira S, Yamada Y, Hirakata Y, Tomonaga M, Sugahara K, Hayashi T, et al. Aberrant expression of caspase cascade regulatory genes in adult T-cell leukaemia: survivin is an important determinant for prognosis. Br J Haematol. 2001;114(1):63–9.
Samuel T, Okada K, Hyer M, Welsh K, Zapata JM, Reed JC. cIAP1 Localizes to the nuclear compartment and modulates the cell cycle. Cancer Res. 2005;65(1):210–8.
Tran J, Master Z, Yu JL, Rak J, Dumont DJ, Kerbel RS. A role for survivin in chemoresistance of endothelial cells mediated by VEGF. Proc Natl Acad Sci USA. 2002;99(7):4349–54.
Sah NK, Khan Z, Khan GJ, Bisen PS. Structural, functional and therapeutic biology of survivin. Cancer Lett. 2006;244(2):164–71.
Wang TT, Wei J, Qian XP, Yu LX, Liu BR. Differential gene expression of the inhibitor of apoptosis proteins in docetaxel-resistant gastric cancer cells. Zhonghua Zhong Liu Za Zhi. 2008;30(8):573–7.
Lu J, Tan M, Huang WC, Li P, Guo H, Tseng LM, et al. Mitotic deregulation by survivin in ErbB2-overexpressing breast cancer cells contributes to taxol resistance. Clin Cancer Res. 2009;15(4):1326–34.
Yang H, Fu JH, Hu Y, Huang WZ, Zheng B, Wang G. Relationship between survivin expression and chemosensitivity of human lung cancer cells. Zhonghua Yi Xue Za Zhi. 2007;87(27):1934–7.
Andreotti PE, Cree IA, Kurbacher CM, Hartmann DM, Linder D, Harel G, et al. Chemosensitivity testing of human tumors using a microplate adenosine triphosphate luminescence assay: clinical correlation for cisplatin resistance of ovarian carcinoma. Cancer Res. 1995;55(22):5276–82.
Cree IA. Luminescence-based cell viability testing. Methods Mol Biol. 1998;102:169–77.
Wu H, Huang M, Lu M, Zhu W, Shu Y, Cao P, et al. Regulation of microtubule-associated protein tau (MAPT) by miR-34c-5p determines the chemosensitivity of gastric cancer to paclitaxel. Cancer Chemother Pharmacol. 2013;71(5):1159–71.
Ugurel S, Schadendorf D, Pfohler C, Neuber K, Thoelke A, Ulrich J, et al. In vitro drug sensitivity predicts response and survival after individualized sensitivity-directed chemotherapy in metastatic melanoma: a multicenter phase II trial of the Dermatologic Cooperative Oncology Group. Clin Cancer Res. 2006;12(18):5454–63.
Kurbacher CM, Cree IA, Bruckner HW, Brenne U, Kurbacher JA, Muller K, et al. Use of an ex vivo ATP luminescence assay to direct chemotherapy for recurrent ovarian cancer. Anticancer Drugs. 1998;9(1):51–7.
Kurbacher CM, Cree IA. Chemosensitivity testing using microplate adenosine triphosphate-based luminescence measurements. Methods Mol Med. 2005;110:101–20.
Kuzmits R, Rumpold H, Muller MM, Schopf G. The use of bioluminescence to evaluate the influence of chemotherapeutic drugs on ATP-levels of malignant cell lines. J Clin Chem Clin Biochem. 1986;24(5):293–8.
Maehara Y, Anai H, Tamada R, Sugimachi K. The ATP assay is more sensitive than the succinate dehydrogenase inhibition test for predicting cell viability. Eur J Cancer Clin Oncol. 1987;23(3):273–6.
Petty RD, Sutherland LA, Hunter EM, Cree IA. Comparison of MTT and ATP-based assays for the measurement of viable cell number. J Biolumin Chemilumin. 1995;10(1):29–34.
Glaysher S, Gabriel FG, Johnson P, Polak M, Knight LA, Parker K, et al. Molecular basis of chemosensitivity of platinum pre-treated ovarian cancer to chemotherapy. Br J Cancer. 2010;103(5):656–62.
Qi CJ, Ning YL, Zhu YL, Min HY, Ye H, Qian KQ. In vitro chemosensitivity in breast cancer using ATP-tumor chemosensitivity assay. Arch Pharm Res. 2009;32(12):1737–42.
Glaysher S, Yiannakis D, Gabriel FG, Johnson P, Polak ME, Knight LA, et al. Resistance gene expression determines the in vitro chemosensitivity of non-small cell lung cancer (NSCLC). BMC Cancer. 2009;9:300.
Wang L, Liu B, Wang T, Ding Y, Qian X, Zhao Y. Detection of cell-free ERCC1 and thymidylate synthase (TS) mRNA in malignant effusions and its association with anticancer drug sensitivity. Anticancer Res. 2008;28(2A):1085–91.
Wang LF, Yin HT, Qian XP, Wei J, Zhao Y, Yu LX, et al. Beta-tubulin III mRNA expression and docetaxel sensitivity in non-small cell lung cancer. Clin Invest Med. 2009;32(6):E278.
Umezu T, Shibata K, Kajiyama H, Terauchi M, Ino K, Nawa A, et al. Taxol resistance among the different histological subtypes of ovarian cancer may be associated with the expression of class III beta-tubulin. Int J Gynecol Pathol. 2008;27(2):207–12.
Ma R, Chen XH, Zhang QF, Zhu L, Tang LP, Wang J, et al. Exploration on the increased sensitivity to docetaxel and reversing mechanism of drug resistance of antisense survivin RNA in gastric cancer cell line SGC7901 cells. Zhonghua Zhong Liu Za Zhi. 2007;29(2):89–92.
Liu JL, Gao W, Kang QM, Zhang XJ, Yang SG. Prognostic value of survivin in patients with gastric cancer: a systematic review with meta-analysis. PLoS One. 2013;8(8):e71930.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
He, W., Zhang, D., Jiang, J. et al. The relationships between the chemosensitivity of human gastric cancer to paclitaxel and the expressions of class III β-tubulin, MAPT, and survivin. Med Oncol 31, 950 (2014). https://doi.org/10.1007/s12032-014-0950-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0950-3