Abstract
RAB27A is a member of Rab family GTPases involved in cellular vesicle trafficking, and TP53 has recently been implicated in regulating the exosome secretion pathway. Because exosome secretion plays an important role in modulating tumor microenvironment and invasive growth, we hypothesized that RAB27A and TP53 expression might be associated with aggressive behavior in pancreatic ductal adenocarcinoma (PDAC), one of the most deadly human malignancies. We determined protein expression of RAB27A and TP53 in 265 pancreatic tissues (186 carcinomas and 79 normal or benign tissues) by immunohistochemistry analysis on tissue microarray and found their expression was correlated with patients’ clinical parameters and overall survival. We found that RAB27A and TP53 protein expression was significantly higher in cancerous tissues compared to normal and benign tissues. High RAB27A protein expression (RAB27A+) was significantly associated with tumor stage and vascular invasion. No correlation between RAB27A and TP53 expression was observed. Patients with high RAB27A expression and high TP53 expression had a poor overall survival. Our data indicate that RAB27A expression is an independent prognostic marker for PDAC, and RAB27A-regulated exosome secretion pathway may represent a novel therapeutic target in pancreatic cancer .
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pancreatic ductal adenocarcinoma (PDAC), arising from the exocrine pancreas and comprising 95 % of pancreatic cancer cases, is one of the most aggressive and lethal forms of human malignancy. Worldwide, PDAC is the twelfth most common cancer and the seventh leading cause of cancer-related deaths with an annual incidence of 338,000 and mortality of 330,000 (Cancer Incidence and Mortality Worldwide in 2012, International Agency for Research on Cancer) [1]. The prognosis of PDAC is dismal with an overall survival of less than 5 % in 5 years. This is because that majority of the patients is diagnosed at an advanced stage who are no longer eligible for surgical resection with a median survival of 3.5 months, while only 10–15 % of the patients are eligible for curative surgical resection with a slightly longer median survival of 12.6 months [2]. In addition, there is no effective targeted therapy. Conventional chemotherapy is only for palliative care to reduce symptoms and improve quality of life but is not effective in prolonging overall survival in patients with advanced metastatic disease [3, 4].
To better understand and improve the dismal outcome of PDAC, reliable prognostic markers and novel therapy targets are needed. Recently, the exosome secretion signaling pathway has emerged as a novel mechanism for cancer invasion and metastasis [5]. Exosomes are 40- to 100-nm membrane vesicles derived from the multivesicular endosomes and released upon fusion with the plasma membrane. Cancer cells utilize exosomes to communicate with the environment through delivery of surface proteins and release of growth factors and cytokines to establish invasive tumor growth [6]. It has been demonstrated that exosome messaging contributes to tumor immune escape [7] and metastatic niche preparation [8].
RAB27A belongs to the Rab family of small GTPases, the master regulator of vesicle fusion and trafficking. It was originally isolated from human melanoma cells and melanocytes. Its expression has been detected in most of normal tissues and tumor cell lines [9]. Abnormal expression of RAB27A has been observed in breast, lung, bladder, rectal, prostate, and liver cancers and associated with aggressive tumor behavior [10–15]. In glioma cell lines, ectopic expression of RAB27A increases cell viability, promotes proliferation and invasion, and suppresses apoptosis [16]. In vivo, RAB27A expression has been shown as a prognostic marker in glioma and hepatocellular carcinoma [15, 17].
TP53 is one of the most important tumor suppressor genes, which is mutated in over 50 % of human malignancies [18]. It regulates DNA repair, cell cycle, and apoptosis and therefore plays an essential role in maintaining genetic stability [19]. Recent studies have also indicated the role of TP53 in regulation of exosome secretion: On the one hand, exosomes can stabilize TP53 protein to create a tumor permissive environment [20]; on the other hand, TP53 transcribes key regulators of endosomal compartment, thus regulates exosome production and secretion [21–23]. However, the interaction between RAB27A and TP53 in regulating exosome secretion has not been reported. Both TP53 protein accumulation and TP53 mutation have been detected in PDAC [24, 25].
Thus far, no study has investigated the role of exosome secretory pathway in PDAC and the potential roles by RAB27A and TP53 in the pathway. To determine whether RAB27A could be used as a prognostic marker and a therapeutic target in pancreatic cancer, we analyzed RAB27A and TP53 expression by immunohistochemistry analysis in both benign and malignant pancreatic tissues using tissue microarrays (TMAs). We correlated RAB27A and TP53 expression with clinicopathological characteristics as well as overall survival in patients with pancreatic cancers.
Materials and methods
Human tissue specimens and patient clinical information
A total of 265 formalin-fixed paraffin-embedded (FFPE) tissue samples were collected from 211 patients. These include 186 pancreatic cancers, 54 matched normal surgical margins, and 25 benign pancreatic lesions. All tissue blocks were obtained from the Department of Pathology, Affiliated Hospital of Nantong University from 2003 to 2010. Clinical characteristics of cancer patients were extracted from their medical record, including: age, sex, tumor location, differentiation grade, perineural and vascular invasion, and tumor stage. None of the cancer patients received any types of treatments (radiation therapy, chemotherapy, or immunotherapy) before surgery. Overall survival (OS) was defined as the period from initial biopsy confirmed diagnosis to death. Patients who were alive at the last follow-up date were censored from the analysis. The study protocol was approved by the Human Research Ethics Committee of the Affiliated Hospital of Nantong University, Jiangsu, China. All participants signed written informed consent. All data have been anonymized and deidentified.
Tissue microarray (TMA) construction and immunohistochemistry analysis (IHC)
TMA was generated using the manual Tissue Microarrayer System Quick Ray (UT06, UNITMA, Korea) in the Department of Clinical Pathology, Nantong University Hospital, Jiangsu, China. Specifically, core tissue biopsies (2 mm in diameter) were taken from ~70 individual FFPE blocks and arranged in a new recipient paraffin block. A total of four TMAs were made, and four-micron sections were cut and placed on super frost-charged glass microscope slides to generate TMA slides.
Tissue sections were deparaffinized and rehydrated through graded alcohols. Endogenous peroxidase activity was blocked by incubation in 3 % H2O2. Antigen retrieval was carried out with 0.01 M citrate buffer pH 6.0 and microwave heat induction. RAB27A was detected by mouse monoclonal anti-human RAB27A antibody (dilution 1:200) (Abcam, ab55667), and TP53 was detected by rabbit polyclonal anti-human TP53 antibody (dilution 1:100) (DAKO, M3629). Reactions were detected with Envision+™ peroxidase kit (Dako, Carpinteria, CA, USA). Color development was accomplished by incubating with 3,3′-diaminobenzidine plus (Dako, Carpinteria, CA, USA), counterstained with hematoxylin, dehydrated through graded alcohols, cleared in xylene, and coverslipped with permanent mounting media.
All cases were reviewed and scored without knowledge of clinical characteristics. The expression of RAB27A and TP53 was scored using the semiquantitative H-score method, taking into account both the staining intensity and the percentage of cells at that intensity [26]. The staining intensity was scored as 0 (no staining), 1+ (weak staining), 2+ (moderate staining), or 3+ (intense staining). For each of the four staining intensity scores, the percentage of cells stained at the respective intensity was determined and multiplied by the intensity score to yield an intensity percentage score. The final staining scores were then calculated from the sum of the four intensity percentage scores; thus, the staining score had a minimum value of 0 (no staining) and a maximum of 300 (100 % of cells with 3+ staining intensity) [27].
Statistical analysis
For statistical analysis, the continuous RAB27A and TP53 expression data from IHC were first converted into dichotic data (low vs. high) using specific cutoff values, which were selected to be significant in terms of OS using the X-tile software program (The Rimm Lab at Yale University; http://www.tissuearray.org/rimmlab) [27–29].
Student’s t test and Pearson’s Chi-square test were used to determine the statistical significance of differences between comparison groups. The correlation between RAB27A and TP53 protein expression was calculated using Spearman’s test. The cumulative patient survival was estimated using the Kaplan–Meier method, and a log-rank test was used to compare the survival curves. A Cox proportional hazards model was used to calculate univariate and multivariate hazard ratios for the variables. A p value of less than 0.05 was considered statistically significant. All statistical analyses were carried out using the SPSS 19.0 statistical software package (SPSS Inc., Chicago, IL).
Results
RAB27A or TP53 expression in pancreatic tissues
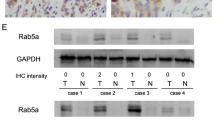
RAB27A protein was localized in the cytoplasm, while TP53 protein was localized in the nuclei (Fig. 1). Using the X-tile software program for TMA data analysis (http://www.tissuearray.org/rimmlab ), we first identified significant cutoff point in terms of OS in pancreatic cancers. For RAB27A, the cutoff 90 was selected: Score 0–90 was considered low expression, while 91–300 was considered high expression. For TP53, the cutoff point 60 was selected: Score 0–60 was considered low expression, while 61–300 was considered high expression. For all subsequent analyses, RAB27A and TP53 protein expression levels were considered either as “low” or “high” using these cutoff values.
Representation of RAB27A and TP53 protein expression in pancreatic benign and malignant tissues on TMA sections. a Pancreatic cancer with high RAB27A expression and no TP53 expression; b pancreatic cancer with low RAB27A expression and high TP53 expression; c benign pancreatic ductal epithelium with no RAB27A expression and no TP53 expression; column 1 and 2 are RAB27A staining with ×40 (bar 500 μm) and ×400 (bar 50 μm) magnification, respectively, and column 3 and 4 are TP53 staining with ×40 (bar 500 μm) and ×400 (bar 50 μm) magnification, respectively
Although high RAB27A expression was detected in benign pancreatic lesions and normal surgical margins, the frequency of high RAB27A expression (RAB27A+) was significantly higher in pancreatic cancers (p = 0.034) (Table 1). Similarly, the frequency of high TP53 expression (TP53+) was also significantly higher in cancers (p = 0.001) than in benign lesions and normal surgical margins. Interestingly, high RAB27A and TP53 coexpression (RAB27A+/TP53+) was only detected in pancreatic cancers, and none of benign pancreatic lesions and normal surgical margins had RAB27A+/TP53+ staining, although not all cancers show coexpression of RAB27A and TP53.
Association of RAB27A and TP53 expression with clinicopathological characteristics in pancreatic cancers
Next, we examined the correlation between RAB27A or TP53 protein expression and clinical parameters among pancreatic cancer patients. High RAB27A expression was significantly associated with vascular invasion (p = 0.016) and tumor stage (p = 0.021), especially with tumor size (p = 0.008) and distant metastasis (p = 0.008), while high TP53 expression was significantly associated with tumor stage (p = 0.041), especially lymph node (p = 0.036) and distant metastasis (p = 0.003), and marginally associated with perineural invasion (p = 0.067) (Table 2). High RAB27A and TP53 coexpression (RAB27A+/TP53+) was significantly associated with vascular invasion (p = 0.015), tumor stage (p = 0.001), especially tumor size (p = 0.003) and distant metastasis (p < 0.001), marginally associated with perineural invasion (p = 0.074). No correlation between RAB27A and TP53 expression was detected.
Prognostic value of RAB27A and TP53 protein expression in pancreatic cancer
We also determined prognostic factors in pancreatic cancers using both univariate and multivariate analysis. High RAB27A expression (HR 2.427, 95 % CI 1.268–4.643; p = 0.007) was significantly associated with poor OS in univariate analysis, as well as high TP53 expression (HR 2.795, 95 % CI 1.450–5.384; p = 0.002), and high RAB27A/high TP53 (RAB27A+/TP53+) coexpression (HR 3.808, 95 % CI 1.625–8.923; p = 0.002). Differentiation (tumor grade) was also significantly associated with poor OS in univariate analysis (HR 2.106, 95 % CI 1.015–4.369; p = 0.045). But regional lymph node metastasis was marginally associated with poor OS (HR 1.759, 95 % CI 0.931–3.324; p = 0.082). In multivariate analysis, only high RAB27A expression and high TP53 expression remained significantly associated with poor OS (HR 2.938, 95 % CI 1.236–6.986; p = 0.015 and HR 3.340, 95 % CI 1.347–8.282; p = 0.009, respectively) (Table 3) (Fig. 2).
Survival curves of pancreatic cancer by the Kaplan–Meier method and the log-rank test. a Overall survival curves of RAB27A+ (green line, 1) and RAB27A- (blue line, 0); b overall survival curves of TP53+ (green line, 1) and TP53- (blue line, 0); c overall survival curves of RAB27A+/TP53+ (blue line, 1), RAB27A+/TP53- or RAB27A-/TP53+ (green line, 2), RAB27A-/TP53+ (yellow line, 3)
Discussion
In this study, we have determined RAB27A and TP53 protein expression in pancreatic tissues by immunohistochemistry analysis on tissue microarray. We found that both RAB27A and TP53 protein expressions were significantly higher in cancerous tissues than in normal and benign tissues. Both high RAB27A protein expression and high TP53 protein expression were associated with tumor stage and distant metastasis. High RAB27A protein expression was also associated with vascular invasion, though we did not detect correlation between RAB27A and TP53 expression. In both univariate analysis and multivariate analysis, we found that high RAB27A expression and high TP53 expression were significantly associated with patients’ poor overall survival.
To the best of our knowledge, this is the first study investigating RAB27A protein expression as well as its prognostic value in PDAC. Our data are consistent with studies of RAB27A in other types of cancer. Dong et al. [15] demonstrated higher RAB27A expression in primary hepatocellular carcinoma than in matched normal adjacent tissues; significant association of RAB27A expression with tumor stage, differentiation grade, and OS. In bladder cancer, both RAB27A and its effectors are abnormally expressed [12]; in glioma, RAB27A was highly expressed in tumor tissues when compared to normal brain tissues and patients with high RAB27A expression had significantly worse prognosis [17]; in breast cancer, RAB27A confers the invasive and metastatic phenotypes by promoting the secretion of insulin-like growth factor II (IGF-II) [10]. Similarly, our observation on TP53′s prognostic value in PDAC is consistent with previous reports from pancreatic cancer and other cancers [30–33].
RAB27A was originally isolated as a novel Rab family small GTP-binding protein from human melanoma cells and melanocytes, implicated in melanosome production [9]. Mutations in RAB27A gene cause a rare human hereditary disease called Griscelli syndrome, which is characterized by silver hair (dysfunction in melanosome transport in melanocytes) and immunodeficiency (dysfunction in granule exocytosis by cytotoxic T lymphocytes) [34, 35]. Because RAB27A is frequently dysregulated in tumor cells, several studies investigated its role in exosome secretion in tumor cells and its influence on tumor microenvironment and invasive tumor growth and metastasis. Silencing RAB27A reduces exosome secretion in breast cancer cells [36] and lung cancer cells [11]. RAB27A is a key component of the secretory pathway in prostate cancer cells (18,413,239). Webber et al. [14] showed that inactivating RAB27A could eliminate TGFβ1 containing exosomes and abolish tumor-promoting stromal myofibroblast differentiation in prostate cancer. Interestingly, a recent study by Bobrie et al. [8] indicates that RAB27A can modify tumor microenvironment and promote tumor progression through both exosome-dependent and exosome-independent pathways, raising the possibility that RAB27A participates in additional tumor-promoting signaling pathways.
Recent studies suggest that besides regulating genomic instability, TP53 protein also regulates exosome secretion. Lespagnol et al. [37] demonstrated that DNA damage-induced exosome secretion is TP53 dependent, as well as senescence-associated exosome release [38]. Mechanistically, it has been shown that TP53 protein responds to stress signals by regulating the transcription of a variety of genes, including TSAP6, playing a role in exosome production and sorting [23, 39]. In addition, TP53 also regulates Chmp4C, Caveolin-1, DRAM, which are involved in the regulation of endosomal compartment [21, 22]. Our data do not support the hypothesis that TP53 regulates exosome secretion in PDAC through RAB27A, but could not rule out the possibility of weak or indirect interaction between RAB27A and TP53 due to the nature of our study design.
Our study has several limitations: First, it is a retrospective observational study, the use of archived convenient samples could introduce bias, and thus, the conclusions might not be applicable to the general population. Larger prospective studies are needed to confirm our findings. Secondly, TMA technology utilizes small sections of tissue blocks to analyze target protein expression, and the expression pattern might not represent the expression pattern of the whole tissue block, thus introducing potential biases in the data. Thirdly, IHC data are subjective and semiquantitative, and additional objective methods are needed to evaluate and confirm RAB27A and TP53 expression in tumor cells. Finally, we do not know whether and how RAB27A protein influences the tumor microenvironment in PDAC. Future in vitro studies are needed to investigate the mechanism of RAB27A and TP53-mediated exosome secretion in pancreatic cancer development.
In conclusion, we have shown that high RAB27A protein expression is an independent prognostic marker in PDAC. Because of the essential role of RAB27A in exosome secretion, future research is warranted to investigate whether RAB27A plays a key role shaping tumor microenvironment and whether RAB27A is a valid novel therapy target in metastatic pancreatic cancer.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61:69–90.
Bilimoria KY, Bentrem DJ, Ko CY, Ritchey J, Stewart AK, Winchester DP, Talamonti MS. Validation of the 6th edition AJCC pancreatic cancer staging system: report from the national cancer database. Cancer. 2007;110:738–44.
He XY, Yuan YZ. Advances in pancreatic cancer research: moving towards early detection. World J Gastroenterol. 2014;20:11241–8.
Bilici A. Prognostic factors related with survival in patients with pancreatic adenocarcinoma. World J Gastroenterol. 2014;20:10802–12.
Peinado H, Aleckovic M, Lavotshkin S, Matei I, Costa-Silva B, Moreno-Bueno G, Hergueta-Redondo M, Williams C, Garcia-Santos G, Ghajar C, Nitadori-Hoshino A, Hoffman C, Badal K, Garcia BA, Callahan MK, Yuan J, Martins VR, Skog J, Kaplan RN, Brady MS, Wolchok JD, Chapman PB, Kang Y, Bromberg J, Lyden D. Melanoma exosomes educate bone marrow progenitor cells toward a pro-metastatic phenotype through met. Nat Med. 2012;18:883–91.
Hoshino D, Kirkbride KC, Costello K, Clark ES, Sinha S, Grega-Larson N, Tyska MJ, Weaver AM. Exosome secretion is enhanced by invadopodia and drives invasive behavior. Cell Rep. 2013;5:1159–68.
Bhatia A, Kumar Y. Cellular and molecular mechanisms in cancer immune escape: a comprehensive review. Expert Rev Clin Immunol. 2014;10:41–62.
Bobrie A, Krumeich S, Reyal F, Recchi C, Moita LF, Seabra MC, Ostrowski M, Thery C. Rab27a supports exosome-dependent and -independent mechanisms that modify the tumor microenvironment and can promote tumor progression. Cancer Res. 2012;72:4920–30.
Chen D, Guo J, Miki T, Tachibana M, Gahl WA. Molecular cloning and characterization of rab27a and rab27b, novel human rab proteins shared by melanocytes and platelets. Biochem Mol Med. 1997;60:27–37.
Wang JS, Wang FB, Zhang QG, Shen ZZ, Shao ZM. Enhanced expression of rab27a gene by breast cancer cells promoting invasiveness and the metastasis potential by secretion of insulin-like growth factor-ii. Mol Cancer Res. 2008;6:372–82.
Li W, Hu Y, Jiang T, Han Y, Han G, Chen J, Li X. Rab27a regulates exosome secretion from lung adenocarcinoma cells a549: involvement of epi64. APMIS 2014;122:1080–87.
Ho JR, Chapeaublanc E, Kirkwood L, Nicolle R, Benhamou S, Lebret T, Allory Y, Southgate J, Radvanyi F, Goud B. Deregulation of rab and rab effector genes in bladder cancer. PLoS One. 2012;7:e39469.
Supiot S, Gouraud W, Campion L, Jezequel P, Buecher B, Charrier J, Heymann MF, Mahe MA, Rio E, Cherel M. Early dynamic transcriptomic changes during preoperative radiotherapy in patients with rectal cancer: a feasibility study. World J Gastroenterol. 2013;19:3249–54.
Webber JP, Spary LK, Sanders AJ, Chowdhury R, Jiang WG, Steadman R, Wymant J, Jones AT, Kynaston H, Mason MD, Tabi Z, Clayton A. Differentiation of tumour-promoting stromal myofibroblasts by cancer exosomes. Oncogene 2014. doi:10.1038/onc.2013.560.
Dong WW, Mou Q, Chen J, Cui JT, Li WM, Xiao WH. Differential expression of rab27a/b correlates with clinical outcome in hepatocellular carcinoma. World J Gastroenterol. 2012;18:1806–13.
Wu X, Hu A, Zhang M, Chen Z. Effects of rab27a on proliferation, invasion, and anti-apoptosis in human glioma cell. Tumour Biol. 2013;34:2195–203.
Wang H, Zhao Y, Zhang C, Li M, Jiang C, Li Y. Rab27a was identified as a prognostic biomaker by mrna profiling, correlated with malignant progression and subtype preference in gliomas. PLoS One. 2014;9:e89782.
Hollstein M, Sidransky D, Vogelstein B, Harris CC. P53 mutations in human cancers. Science. 1991;253:49–53.
Vogelstein B, Kinzler KW. P53 function and dysfunction. Cell. 1992;70:523–6.
Dutta S, Warshall C, Bandyopadhyay C, Dutta D, Chandran B. Interactions between exosomes from breast cancer cells and primary mammary epithelial cells leads to generation of reactive oxygen species which induce DNA damage response, stabilization of p53 and autophagy in epithelial cells. PLoS One. 2014;9:e97580.
Feng Z. P53 regulation of the igf-1/akt/mtor pathways and the endosomal compartment. Cold Spring Harb Perspect Biol. 2010;2:a001057.
Yu X, Riley T, Levine AJ. The regulation of the endosomal compartment by p53 the tumor suppressor gene. FEBS J. 2009;276:2201–12.
Yu X, Harris SL, Levine AK. The regulation of exosome secretion: a novel function of the p53 protein. Cancer Res. 2006;66:4795–801.
Casey G, Yamanaka Y, Friess H, Kobrin MS, Lopez ME, Buchler M, Beger HG, Korc M. P53 mutations are common in pancreatic cancer and are absent in chronic pancreatitis. Cancer Lett. 1993;69:151–60.
Cowley MJ, Chang DK, Pajic M, Johns AL, Waddell N, Grimmond SM, Biankin AV. Understanding pancreatic cancer genomes. J Hepatobiliary Pancreat Sci. 2013. doi:10.1007/s00534-013-0610-6.
Detre S, Saclani Jotti G, Dowsett M. A “Quickscore” method for immunohistochemical semiquantitation: validation for oestrogen receptor in breast carcinomas. J Clin Pathol. 1995;48:876–8.
Zhai X, Zhu H, Wang W, Zhang S, Zhang Y, Mao G. Abnormal expression of emt-related proteins, s100a4, vimentin and e-cadherin, is correlated with clinicopathological features and prognosis in hcc. Med Oncol. 2014;31:970.
Ni S, Xu L, Huang J, Feng J, Zhu H, Wang G, Wang X. Increased zo-1 expression predicts valuable prognosis in non-small cell lung cancer. Int J Clin Exp Pathol. 2013;6:2887–95.
Sun R, Wang X, Zhu H, Mei H, Wang W, Zhang S, Huang J. Prognostic value of lamp3 and tp53 overexpression in benign and malignant gastrointestinal tissues. Oncotarget 2014.
Oshima M, Okano K, Muraki S, Haba R, Maeba T, Suzuki Y, Yachida S. Immunohistochemically detected expression of 3 major genes (cdkn2a/p16, tp53, and smad4/dpc4) strongly predicts survival in patients with resectable pancreatic cancer. Ann Surg. 2013;258:336–46.
Chen J, Tang H, Wu Z, Zhou C, Jiang T, Xue Y, Huang G, Yan D, Peng Z. Overexpression of rbbp6, alone or combined with mutant tp53, is predictive of poor prognosis in colon cancer. PLoS One. 2013;8:e66524.
Arriaga JM, Bravo IA, Bruno L, Morales Bayo S, Hannois A, Sanchez Loria F, Pairola F, Huertas E, Roberti MP, Rocca YS, Aris M, Barrio MM, Baffa Trasci S, Levy EM, Mordoh J, Bianchini M. Combined metallothioneins and p53 proteins expression as a prognostic marker in patients with dukes stage b and c colorectal cancer. Hum Pathol. 2012;43:1695–703.
Mojarad S, Venturini B, Fulgenzi P, Papaleo R, Brisigotti M, Monti F, Canuti D, Ravaioli A, Woo L, Dlay S, Sherbet GV. Prediction of nodal metastasis and prognosis of breast cancer by ann-based assessment of tumour size and p53, ki-67 and steroid receptor expression. Anticancer Res. 2013;33:3925–33.
Fukuda M. Rab27 and its effectors in secretory granule exocytosis: a novel docking machinery composed of a rab27. Effector complex. Biochem Soc Trans. 2006;34:691–5.
Van Gele M, Dynoodt P, Lambert J. Griscelli syndrome: a model system to study vesicular trafficking. Pigment Cell Melanoma Res. 2009;22:268–82.
Zheng Y, Campbell EC, Lucocq J, Riches A, Powis SJ. Monitoring the rab27 associated exosome pathway using nanoparticle tracking analysis. Exp Cell Res. 2013;319:1706–13.
Lespagnol A, Duflaut D, Beekman C, Blanc L, Fiucci G, Marine JC, Vidal M, Amson R, Telerman A. Exosome secretion, including the DNA damage-induced p53-dependent secretory pathway, is severely compromised in Tsap6/steap3-null mice. Cell Death Differ. 2008;15:1723–33.
Lehmann BD, Paine MS, Brooks AM, McCubrey JA, Renegar RH, Wang R, Terrian DM. Senescence-associated exosome release from human prostate cancer cells. Cancer Res. 2008;68:7864–71.
Amzallag N, Passer BJ, Allanic D, Segura E, Thery C, Goud B, Amson R, Telerman A. Tsap6 facilitates the secretion of translationally controlled tumor protein/histamine-releasing factor via a nonclassical pathway. J Biol Chem. 2004;279:46104–12.
Acknowledgments
This study was supported by the postdoctoral study (2013-40-5) and translational medicine research (TDFzh2014011) from the Affiliated Hospital of Nantong University, Jiangsu, China.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Wang, Q., Ni, Q., Wang, X. et al. High expression of RAB27A and TP53 in pancreatic cancer predicts poor survival. Med Oncol 32, 372 (2015). https://doi.org/10.1007/s12032-014-0372-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0372-2