Abstract
Novel (nua) kinase family 1 (NUAK1) is a member of the human adenosine monophosphate-activated protein kinases family, which is overexpressed in multiple human malignancies and thought to be involved in tumor invasion and metastasis ability. Our study is to investigate the association of NUAK1 expression with clinicopathological parameters and prognostic significance of patients with gastric cancer. The expression patterns of the NUAK1 protein in 117 primary archival gastric cancer specimens and 46 adjacent normal epithelial tissues from patients were detected by immunohistochemistry assay. Staining evaluation results were analyzed statistically in relation to various clinicopathological characters, recurrence-free survival and overall survival. High level of NUAK1 expression was detected in gastric cancer, significantly more than in adjacent normal epithelial cells. In gastric cancer, NUAK1 was positively correlated with depth of invasion, lymph node metastasis, pathological stage, surgical resection and histological differentiation. However, no correlations between NUAK1 expression and patients’ age, sex, tumor size, location, CA19-9 or CEA were detected. The recurrence-free survival and overall survival were significantly shorter for patients with NUAK1 higher scores than those with NUAK1 lower scores. Multivariate analysis identified NUAK1 was an independent prognostic factor for both recurrence-free survival and overall survival. Our findings provided convincing evidence for NUAK1 overexpression, which was tightly associated with more aggressive tumor behavior and a poor prognosis, indicating that NUAK1 is a valuable molecular biomarker for gastric cancer progression. It might also act as a promising target for both prognostic prediction and therapeutics.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is a common digestive tract cancer, ranking the second in all cancer-related deaths worldwide [1, 2]. The highest rate of gastric cancer is occurs in Eastern Asian countries especially China and Japan, whereas in Western Europe and the Unites States, gastric cancer is relatively less common [1]. Although gastric cancer can be curable if detected early, most cases of GC are asymptomatic until the advanced stages in which current therapeutic strategies are far from optimal. Therefore, to improve the poor survival rate and permit earlier diagnosis, molecular markers of more sensitivity and specificity than current ones such as the CA19-9 and carcinoembryonic antigen (CEA) are needed [3, 4].
Novel (nua) kinase family 1 (NUAK1) (also known as ARK5) is a member of the AMP-activated protein kinase (AMPK) family, which is thought to induce tumor cell survival during nutrient starvation in an Akt-dependent manner and promote tumor invasion and metastasis in multiple human malignancies [5]. Aberrant NUAK1 expression has been well documented for various human solid neoplasms, including those of colorectal cancer [6], non-small cell lung cancer [7], glioma [8], squamous cell carcinoma [9] and hepatocellular carcinoma [10]. Moreover, high NUAK1 expression is associated with aggressive cancer phenotypes, such as advanced clinical stage, increased metastatic ability and decreased patient survival [7, 8, 10], revealing NUAK1 as a potential prognostic biomarker in a panel of human malignancies. The expression pattern of NUAK1 protein in gastric cancer and especially the prognostic significance of NUAK1 protein in GC remain to be elucidated. In the present study, the NUAK1 expression in surgical specimens of GC was examined to evaluate whether this molecule is useful to predict postoperative outcome. To our knowledge, this is the first report of expression of NUAK1 in human gastric carcinoma and its relationship with survival analyses.
Materials and methods
Subjects and Postoperative follow-up
After providing informed consent, 117 patients (72 males, 45 females; median age: 63 years, range 28–86 years) were diagnosed as gastric cancer from December 2008 to January 2009 and had undergone partial or total gastrectomy (77 had total gastrectomies and 40 had partial gastrectomies) at the Department of general surgery in The First Affiliated Hospital of Anhui Medical University (AHMU)(Hefei, China) were enrolled in this study. A total of 117 tumor samples surgically resected from primary gastric cancer patients, and 46 adjacent normal epithelial tissues were selected. The main clinical and pathological characteristics of the patients are described in Table 1. Patients with GC enrolled in our study had to follow these inclusion criteria: no history of previous radiotherapy or chemotherapy and primary gastric carcinoma without other malignancies. The study protocol was approved by the Medical Ethics and Human Clinical Trial Committee of AHMU. Resected specimens were examined pathologically using the seventh edition of the tumor node metastasis (TNM) classification of the International Union Against Cancer (UICC) criteria. The preoperative serum CEA and CA19-9 levels (within 1 week prior to gastrectomy) were determined in the clinical laboratory. The cutoff value for CEA was 5 ng/ml, and that for CA19-9 was 37 U/ml.
After discharge, patients had periodic follow-up visits every 3 months for the first 2 years after surgery, every 6 months for the next 3 years, and yearly thereafter until their death or the beginning of the preparation of this article. Local recurrence and metastasis were confirmed by tumor markers levels including CEA, CA199, CA125, AFP and CA724, B-type ultrasonic inspection every 3 months and computed tomography (CT) or magnetic resonance imaging (MRI) every 6 months after gastrectomy. All patients with GC had a full-range postoperational follow-up, and intact clinical information was obtained. The follow-up period of our study ended in January 2014. Overall survival time (OS) and recurrence-free survival time (RFS) calculation was based on the duration from the day of surgery to the day of death or tumor relapse. Death of patients with GC resulting from other causes was defined as censored cases.
Immunohistochemical staining
Immunohistochemical staining was performed as described previously [11]. Briefly, antigen retrieval was carried out in 10 mmol/L citrate buffer (pH = 6.0) in a microwave oven for 20 min. The activity of endogenous peroxidase was exhausted with 3 % hydrogen peroxide for 10 min at room temperature. Rabbit NUAK1 polyclonal antibody (Santa Cruz Biotechnology, Santa Cruz, CA, USA) was applied overnight at 4 °C at optimal working concentration of 1:50. After sufficient phosphate-buffered saline rinses, sections were immunostained with horseradish peroxidase-labeled goat anti-rabbit polymers. Finally, positive staining of NUAK1 protein was visualized with diaminobenzidine, and the cell nucleus was counterstained with Mayer’s hematoxylin. For negative controls, the primary antibody was replaced with normal goat serum (Santa Cruz Biotechnology) by co-incubation at 4 °C overnight under the same experimental conditions. The slides were then dehydrated following a standard procedure and sealed with coverslips.
Evaluation of staining of NUAK1
All stained sections were evaluated and scored independently by two pathologists with no prior knowledge of the clinicopathological outcomes of the patients. If a disagreement occurred, the slides were re-examined to obtain a final consensus. Staining intensity was classified as +0 to +3: +0 point meant negative intensity, +1 point meant weak intensity, +2 points meant moderate intensity, and +3 points meant strong intensity. For semiquantitative analysis of immunoreactivity of NUAK1, an H-scoring system was used as described [12]. The numerical-scoring (NS) results were scored by multiplying the percentage of positive cells (P) by the intensity (I). The formula was: NS = P*I. For example, a tissue section stained with 25 %, +0; 10 %, +1; 65 %, +2; 0 %, +3. NS = 25*0 + 10*1 + 65*2 + 0 *3 = 140. The cutoff value for high and low NUAK1 expression was determined by measuring heterogeneity with statistical analysis of log-rank test regarding the overall survival. So we set the cutoff values of NUAK1 expression at immunohistochemistry (IHC) score of 178 or the third quartile. The lower expression group was defined as those at or below the cutoff value (178 for IHC scores) of NUAK1 expression, whereas the higher expression group consisted of patients expressing levels above the cutoff value of NUAK1 measured in the tumor.
Statistical analysis
Statistical analysis was performed using SPSS for Windows version 19.0 (SPSS, Chicago, IL, United States). The nonparametric Mann–Whitney U test was employed to evaluate the associations between various clinicopathological parameters and expression level of NUAK1 expression. Kaplan–Meier survival analysis was used to assess the difference of patient survival between the NUAK1 higher expression group and the NUAK1 lower expression group with other clinical factors. The significant differences between survival curves were determined by the log-rank test. Multivariate analysis for independent prognostic indicators was performed via establishing the Cox proportional hazards regression model. The correlations between the staining intensity of NUAK1 and TNM stage were determined using Spearman’s rank correlation coefficient. A p value < 0.05 was considered to be statistically significant in a two-tailed test.
Results
Clinical characteristics of the patients
Among the 117 patients with immunohistochemical (IHC) study, the mean tumor size (maximal diameter) was 5.3 ± 3.3 cm (median: 5.2 cm; range 0.9–15.0 cm). The tumors were located in the cardia of the stomach in 61 patients and the body/antrum in 56. As defined by the depth of wall invasion, early gastric cancer (T1) was noted in 12 cases (10.3 %; comprising lamina propria or muscularis mucosae/T1a in 2 and submucosa/T1b in 10), while advanced cancer included T2 (muscularis propria) in 30 cases, T3 (penetrates the subserosa) in 32 cases and T4 (invasion to invades serosa/T4a or invasion to adjacent structures/T4b) in 43 patients. Lymph node metastasis was found in 70 patients (59.8 %). The occurrences of the various pathologic stages were I(IA + IB; n = 9), II (IIA + IIB; n = 38), III(IIIA + IIIB + IIIC; n = 62) and IV (n = 8).
The median follow-up period was 38 months (range 4–62 months) in 117 patients. Five patients died of postoperative complications, and 6 patients died of other causes. Sixty-one patients died because of the progression of their gastric cancer.
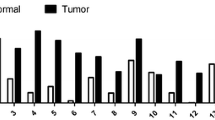
To validate the expression levels and the location of NUAK1 in GC, 117 paraffin-embedded, archival primary GC specimens and 46 corresponding adjacent noncancerous specimens were detected using immunohistochemistry. Figure 1 shows 4 representative cases of gastric tumor tissues and 2 cases of adjacent normal epithelial tissues. The higher levels of immunostaining intensity were prevalent in the cancer cells, whereas lower levels were observed in the stromal cells or fibroblasts of gastric cancer tissues. Strong NUAK1 protein staining was predominantly distributed in the cytoplasmic region of gastric cancer cells. By contrast, NUAK1 protein was barely detectable or a few weak positive in normal gastric epithelial cells of the corresponding adjacent noncarcinoma samples. Among the 117 patients analyzed using IHC, the mean score of IHC in tumor tissues was 131.0 ± 4.80 (mean ± s.e.) that was significantly greater than those (36.2 + 2.80) observed in the matching adjacent mucosa (n = 46) (p < 0.001, Wilcoxon signed-rank test). Furthermore, the paired comparison of immunoreactivity for NUAK1(n = 46) revealed that the IHC score of the cancerous tissues was greater than that of the nontumorous counterparts in 38 (82.6 %) patients, equal in 2 patients (4.3 %) and smaller in 6 patients (13.0 %).
Immunohistochemical staining of NUAK1 protein in GC or in adjacent noncancer tissues. a Showed NUAK1 staining was strong in GC tissue samples, b, c and d showed moderate staining, weak staining and barely negative staining of NUAK1 in GC tissue. The numerical scoring (NS) results of a, b, c and d were 236, 145, 50 and 26, respectively. e and f showed weak and negative staining of NUAK1 in adjacent normal gastric tissues. The numerical-scoring (NS) results of e and f were 60 and 0, respectively. Black arrows indicate different levels of cytoplasm staining. (original magnification, *400 in a–f)
Relationship between NUAK1 overexpression and patients’ clinicopathological parameters
Based on the above finding that NUAK1 protein was overexpressed in a large proportion of GC tumors, the expression of NUAK1 protein was further correlated with major clinicopathological characteristics of patients with GC. As summarized in Table 1, NUAK1 protein expression level was significantly associated with depth of invasion/T classification (p < 0.001), lymph node metastasis (p < 0.001), surgical resection (p = 0.020), pathological stage (p < 0.001) and histological differentiation (p = 0.015). However, no significant correlation was observed between the expression of NUAK1 protein and parameters such as gender (p = 0.342), age (p = 0.554), tumor location (p = 0.737), CA19-9 (p = 0.071) and CEA (p = 0.473).
Survival analysis of NUAK1 expression
The overall cumulative 5-year survival rate of the 117 patients with gastric resection was 36.1 %. Figure 2 illustrates the cumulative survival curves of patients subgrouped into the lower expression and higher expression of NUAK1. Kaplan–Meier survival analysis demonstrated that patients with high NUAK1 expression had increased risk of overall recurrence (p < 0.001; Fig. 2a) and mortality (p < 0.001; Fig. 2b) in patients with GC. Log-rank tests further confirmed that the difference between 5-year DFS and OS rates in these two groups was statistically significant (log-rank p = 0.003/0.001). The 5-year survival rate of the two groups using an IHC score cutoff value of 117 was 41.3 and 19.0 %, respectively, for the lower expression (n = 85) and higher expression (n = 32) groups.
Univariate analysis and multivariate Cox regression analysis
To examine the impact of NUAK1 overexpression on the RFS and OS, we performed univariate analysis of traditional clinicopathologic variables for prognosis. The results of univariate analysis were shown that significant indicators in the recurrence-free survival and overall survival analysis included NUAK1 overexpression (p = 0.001 and p < 0.001, respectively), tumor size (p = 0.034 and p = 0.015, respectively), depth of invasion (p = 0.007 and p = 0.005, respectively),TNM stage (p = 0.003 and p = 0.001, respectively), CA19-9(p = 0.010 and p = 0.010, respectively) and CEA (p < 0.001 and p < 0.001, respectively) were positive prognostic factors for RFS and OS in gastric cancer patients (Table 2). However, gender, age, tumor location, histological differentiation or lymph node metastasis had no prognosis value on RFS and OS of patients with gastric cancer.
Furthermore, to evaluate the independent impact of NUAK1 overexpression on RFS and OS, a multivariate Cox proportional hazards model was adjusted for tumor size, depth of invasion, TNM stage, CA19-9, CEA and NUAK1 expression. Our results demonstrated that NUAK1 expression was an independent prognostic factor for both RFS (HR = 2.103, 95 % CI 1.339–3.304; p = 0.001) and OS (HR = 2.527, 95 % CI 1.551–4.118; p < 0.001) of patients with gastric cancer. Regarding other parameters, CEA was determined to be independent prognostic factor influencing the patients’ RFS in the multivariate analysis, but TNM stage and CEA were for patients’ OS in the multivariate analysis (Table 2).
Spearman’s correlation coefficient
To further study the potential roles of NUAK1 protein in GC cancer progression, the correlations between the staining intensity of NUAK1 and TNM stage were determined using Spearman’s rank correlation coefficient. As shown in Table 3, it showed that NUAK1 expression in GC is in positive correlation with TNM stage that suggested the more advanced clinical TNM stage corresponding to the higher staining intensity of NUAK1 in GC (Rs = 0.415, p < 0.001).
Discussion
Gastric cancer is the most common digestive tract cancer and ranking the second in all cancer-related deaths worldwide [1, 2]. Mortality due to gastric cancer has risen in China over the past 2 decades, especially in rural areas and in aging populations. In China alone, there were more than 400,000 new cases diagnosed per year, leading to over 300,000 deaths accounting for 23.2 % of the total deaths from cancer every year [13]. Despite the advances in diagnostic mode, combination chemotherapy and radiation therapy, little improvement has been achieved within the last decade in terms of prognosis and quality of life for patients with gastric cancer. Even in stage I gastric cancer, 5–30 % of patients develop recurrent disease and eventually die of metastatic disease [13].Therefore, supplementing standard clinical and pathological staging with molecular markers would enable a more precise identification of patients with the highest or lowest risk of relapse following gastric cancer surgery.
AMPK (5-prime-AMP-activated protein kinase) is a major regulator of whole-body and cellular energy homeostasis and be activated by various cellular stresses that consume intracellular adenosine triphosphate. AMPK has a major function in protecting cells by converting energy metabolism from anabolic to catabolic through the inhibition and activation of various molecules, including HMG-CoA reductase, acyl-CoA carboxylase and glucose transporters [14]. Nowadays, AMPK is already known to interact with a network of complex structures and act as a tumor suppressor in the malignant behavior of cancer by altering the metabolic signal pathway in cancer cells. NUAK1 is one of 12 members of AMP-activated protein kinase family because of its great sequence homology to the catalytic domain of AMPK, which is thought to be involved in tumor invasion and metastasis ability. [15]. NUAK1 was first discovered as a major factor in Akt-dependent cell survival and migration activity in human colon and pancreatic cancer cell [16]. Kusakai et al. [17] reported that activated Akt inhibits apoptosis and stimulates invasion activity by phosphorylating the downstream substrate ARK5 at Ser600, and thereby leading to substrates such as MMPs activation and stimulation of tumor invasion and metastasis. Nowadays, NUAK1 has been reported to promote tumor progression and metastasis through the up-regulation of cell proliferation, inhibition of p53-mediated tumor suppression and activate the production of matrix metalloproteinase 2(MMP2) and MMP9 in diverse human malignancies [7, 18, 19]. Increased NUAK1 can also promote glioma cell invasion by regulating cytoskeleton rearrangement and induces gross aneuploidies and senescence in the control of cellular senescence and cellular ploidy [8, 20]. More recently, a key finding showing that NUAK1 may play a role in regulating tumor proliferation and survival through metabolic alteration in hepatocarcinoma proved that targeting cellular energy homeostasis could be a valuable strategy to eliminate Myc-deregulated tumor cells [21].Taken together, the NUAK1 pathway might play an important role in cancer progression.
The aberrant expression of NUAK1 has been previously reported in diverse human malignancies [7, 8, 10]. Our data are compatible with the NUAK1 overexpression in these articles and demonstrated that NUAK1 was frequently overexpressed in gastric cancer tissues. In this study, we verified that NUAK1 is frequently overexpressed in gastric cancer cells by immunohistochemical-staining examinations. Among the patients examined, the NUAK1 expression was up-regulated in the GC samples compared with the adjacent normal epithelial tissue samples in most of GC patients (p < 0.001, Wilcoxon signed-rank test). Higher NUAK1 expression was significantly associated with depth of invasion/T classification, lymph node metastasis, surgical resection, pathological stage/TNM stage and histological differentiation in GC (all p < 0.05). Therefore, high expression of NUAK1 may be a potential diagnostic marker for the gastric cancer.
Currently, outcome prediction is still based on critical clinical parameters, such as the clinical staging and histopathological criteria. However, the current staging classifications do not produce accurate predictions of patient outcomes. Recent advances in molecular biology of human malignancies provide a hint that the discovery molecular abnormalities may facilitate early diagnosis and prognosis prediction. Our study revealed that NUAK1 protein level was significantly positively associated with the postoperative prognosis in patients with GC, and the overall 5-year survival of NUAK1 higher expression group had a significantly shorter RFS/OS than that of NUAK1 lower expression group. These findings are consistent with the previous reports that the higher expression of NUAK1 in hepatocellular carcinoma and non-small cell lung cancer are both often associated with shorter recurrence-free/overall survival [7, 10]. Moreover, the multivariate Cox model analysis indicated that NUAK1 expression level was identified as an independent risk factor for both RFS and OS. Our data suggested that NUAK1 might play an important role in tumor prognosis and that the levels of NUAK1 expression in GC tissue samples might be used as a prognostic marker in GC patients. Additionally, the significant association between serum CEA and RFS/OS of gastric cancer was not the case in our study, which is consistent with the previous study, in which ectopic serum CEA overexpression could significantly decrease the RFS/OS of patients with gastric cancer [22].
It was found that the survival time of the stage III–IV disease patients was significantly shorter than that of the stage I–II disease patients (p < 0.05). Moreover, Spearman’s rank correlation analysis suggested the more advanced clinical TNM stage corresponding to the higher staining intensity level of NUAK1 in GC. We speculate that NUAK1 may play more important role in advanced carcinoma of stomach, and proteins that functionally and/or physically may interact with NUAK1 include many with direct roles in promoting tumor invasion in GC.
In summary, our data demonstrated that aberrant NUAK1 protein expression was tightly associated with aggressive clinical behaviors in human GC, indicating NUAK1 as a useful biomarker for both diagnosis and prognosis in GC. Since NUAK1 is overexpressed in a variety of malignancies, it would not be an appropriate diagnostic biomarker for any specific tumors. However, it might be a promising prognostic marker of many cancers. Several studies have indicated that MMP-9 [23], CXCR4 [24], and BRCA1 [25] were highly expressed and associated with advanced stage and poor prognosis in gastric cancer patients. We will combine these protein markers as a package to improve the specificity and sensitivity for the diagnosis or prognosis of gastric cancer. Finally, further investigation of NUAK1 is warranted for its potential as a prognostic and therapeutic agent. Therefore, further intensive research in both in vitro and in vivo conditions is being conducted in our laboratory to identify the exact functional mechanisms of NUAK1 in the process of malignant transformation in GC.
Conclusion
To the best of our knowledge, this is the first study to explore the prognostic value of NUAK1 protein in GC and to report that the up-regulated expression of NUAK1 protein is a predictor of different aggressive tumor behaviors such as advanced clinical stage and postoperational recurrence in patients with GC. Therefore, high expression of NUAK1 identifies high-risk patients and may be a potential novel therapeutic target for gastric carcinoma.
References
Ferlay J, Parkin DM, Steliarova-Foucher E. Estimates of cancer incidence and mortality in Europe in 2008. Eur J Cancer. 2010;46(4):765–81. doi:10.1016/j.ejca.2009.12.014.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107.
Bernal C, Aguayo F, Villarroel C, Vargas M, Diaz I, Ossandon FJ, et al. Reprimo as a potential biomarker for early detection in gastric cancer. Clin Cancer Res. 2008;14(19):6264–9. doi:10.1158/1078-0432.CCR-07-4522.
Marrelli D, Roviello F, De Stefano A, Farnetani M, Garosi L, Messano A, et al. Prognostic significance of CEA, CA 19-9 and CA 72-4 preoperative serum levels in gastric carcinoma. Oncology. 1999;57(1):55–62.
Suzuki A, Kusakai G, Kishimoto A, Shimojo Y, Miyamoto S, Ogura T, et al. Regulation of caspase-6 and FLIP by the AMPK family member ARK5. Oncogene. 2004;23(42):7067–75. doi:10.1038/sj.onc.1207963.
Kusakai G, Suzuki A, Ogura T, Miyamoto S, Ochiai A, Kaminishi M, et al. ARK5 expression in colorectal cancer and its implications for tumor progression. Am J Pathol. 2004;164(3):987–95.
Chen P, Li K, Liang Y, Li L, Zhu X. High NUAK1 expression correlates with poor prognosis and involved in NSCLC cells migration and invasion. Exp Lung Res. 2013;39(1):9–17. doi:10.3109/01902148.2012.744115.
Lu S, Niu N, Guo H, Tang J, Guo W, Liu Z, et al. ARK5 promotes glioma cell invasion, and its elevated expression is correlated with poor clinical outcome. Eur J Cancer. 2013;49(3):752–63. doi:10.1016/j.ejca.2012.09.018.
Kinoshita R, Iwadate M, Umeyama H, Taguchi YH. Genes associated with genotype-specific DNA methylation in squamous cell carcinoma as candidate drug targets. BMC Syst Biol. 2014;8(Suppl 1):S4. doi:10.1186/1752-0509-8-S1-S4.
Cui J, Yu Y, Lu GF, Liu C, Liu X, Xu YX, et al. Overexpression of ARK5 is associated with poor prognosis in hepatocellular carcinoma. Tumour Biol. 2013;34(3):1913–8. doi:10.1007/s13277-013-0735-x.
Ye YZ, Zhang ZH, Fan XY, Xu XL, Chen ML, Chang BW, et al. Notch3 overexpression associates with poor prognosis in human non-small-cell lung cancer. Med Oncol. 2013;30(2):595. doi:10.1007/s12032-013-0595-7.
Cheng WL, Wang CS, Huang YH, Liang Y, Lin PY, Hsueh C, et al. Overexpression of a secretory leukocyte protease inhibitor in human gastric cancer. Int J Cancer. 2008;123(8):1787–96. doi:10.1002/ijc.23746.
Yang L. Incidence and mortality of gastric cancer in China. World J Gastroenterol. 2006;12(1):17–20.
Hardie DG, Alessi DR. LKB1 and AMPK and the cancer-metabolism link: ten years after. BMC Biol. 2013;11:36. doi:10.1186/1741-7007-11-36.
Sun X, Gao L, Chien HY, Li WC, Zhao J. The regulation and function of the NUAK family. J Mol Endocrinol. 2013;51(2):R15–22. doi:10.1530/JME-13-0063.
Suzuki A, Kusakai G, Kishimoto A, Lu J, Ogura T, Lavin MF, et al. Identification of a novel protein kinase mediating Akt survival signaling to the ATM protein. J Biol Chem. 2003;278(1):48–53. doi:10.1074/jbc.M206025200.
Koh HJ, Toyoda T, Fujii N, Jung MM, Rathod A, Middelbeek RJ, et al. Sucrose nonfermenting AMPK-related kinase (SNARK) mediates contraction-stimulated glucose transport in mouse skeletal muscle. Proc Natl Acad Sci USA. 2010;107(35):15541–6. doi:10.1073/pnas.1008131107.
Hou X, Liu JE, Liu W, Liu CY, Liu ZY, Sun ZY. A new role of NUAK1: directly phosphorylating p53 and regulating cell proliferation. Oncogene. 2011;30(26):2933–42. doi:10.1038/onc.2011.19.
Suzuki A, Lu J, Kusakai G, Kishimoto A, Ogura T, Esumi H. ARK5 is a tumor invasion-associated factor downstream of Akt signaling. Mol Cell Biol. 2004;24(8):3526–35.
Humbert N, Navaratnam N, Augert A, Da Costa M, Martien S, Wang J, et al. Regulation of ploidy and senescence by the AMPK-related kinase NUAK1. EMBO J. 2010;29(2):376–86. doi:10.1038/emboj.2009.342.
Liu L, Ulbrich J, Muller J, Wustefeld T, Aeberhard L, Kress TR, et al. Deregulated MYC expression induces dependence upon AMPK-related kinase 5. Nature. 2012;483(7391):608–12. doi:10.1038/nature10927.
Kochi M, Fujii M, Kanamori N, Kaiga T, Kawakami T, Aizaki K, et al. Evaluation of serum CEA and CA19-9 levels as prognostic factors in patients with gastric cancer. Gastric Cancer. 2000;3(4):177–86.
Chu D, Zhang Z, Li Y, Zheng J, Dong G, Wang W, et al. Matrix metalloproteinase-9 is associated with disease-free survival and overall survival in patients with gastric cancer. Int J Cancer. 2011;129(4):887–95. doi:10.1002/ijc.25734.
Ying J, Xu Q, Zhang G, Liu B, Zhu L. The expression of CXCL12 and CXCR4 in gastric cancer and their correlation to lymph node metastasis. Med Oncol. 2012;29(3):1716–22. doi:10.1007/s12032-011-9990-0.
Chen W, Wang J, Li X, Li J, Zhou L, Qiu T, et al. Prognostic significance of BRCA1 expression in gastric cancer. Med Oncol. 2013;30(1):423. doi:10.1007/s12032-012-0423-5.
Acknowledgments
This study was funded by Key Programs of Educational Commission of Anhui Province (No. KJ2010A181) and Medical Scientific Research Foundation of Anhui Province, China (No. 09A034).
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Xiao-tian Ye and Ai-jun Guo have contributed equally to this work.
Rights and permissions
About this article
Cite this article
Ye, Xt., Guo, Aj., Yin, Pf. et al. Overexpression of NUAK1 is associated with disease-free survival and overall survival in patients with gastric cancer. Med Oncol 31, 61 (2014). https://doi.org/10.1007/s12032-014-0061-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0061-1