Abstract
Single nucleotide polymorphism (SNP) rs17849071 was recently reported to be inversely associated with PIK3CA amplification in follicular thyroid cancer, but the main function of this SNP remains unclear. In this study, by using PCR and sequencing method, we explored whether this SNP was associated with P53 expression status and other clinicopathological characteristics in 62 Chinese breast cancer (BCa) patients. In our results, P53 protein accumulation was significantly associated with HER2 overexpression (P = 0.013) and Ki-67 expression (P = 0.007), which were in accord with previous studies. Besides, there was a significantly inverse relationship between P53 protein expression and rs17849071 GT+GG genotype in Chinese BCa patients (P = 0.044). The SNP was not related to other important BCa markers such as estrogen receptor, progestin receptor, and HER2. Among different BCa intrinsic subtypes, no significant differences were found on P53 expression status (P = 0.356) or rs17849071 polymorphism (T>G) (P = 0.813). In conclusion, SNP rs17849071 GT+GG genotype was inversely associated with P53 protein accumulation in BCa samples. Studies with larger sample size focusing on exploring the relationship of rs17849071 polymorphisms, P53 accumulation, P53 mutations, and PIK3CA amplification might be needed.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, over 1.1 million women are diagnosed with breast cancer (BCa) annually, and 410,000 die from the disease each year [1]. BCa is a highly heterogeneous disease. Biomarkers such as estrogen receptor (ER), progesterone receptor (PR), and HER2 can provide useful information for BCa typing and individualized treatment.
In addition to the biomarkers mentioned above, P53 protein, which is encoded by the TP53 gene, is another frequently used marker of BCa. TP53 is one of the most frequently mutated genes in human cancers. P53 has many important biological functions, including regulation of the cell cycle, apoptosis, senescence, DNA metabolism, angiogenesis, and cellular differentiation. Mutations of TP53 frequently lead to accumulation of mutant forms of P53 protein, which can be detected using immunohistochemical staining in clinical practice. P53 protein overexpression is associated with the presence of any TP53 mutation, especially missense mutations [2]. Several cohort studies have shown that P53 protein accumulation contributes to an increased risk of progression to BCa [3, 4]. Some reports showed that P53 expression might be associated with a significant decrease in BCa survival [5–7]. However, the prognostic value of P53 overexpression in BCa remains controversial.
In addition to the TP53 gene, alpha catalytic subunit of phosphoinositol-3-kinase (PIK3CA) is frequently mutated in BCa [8]. PI3K (phosphatidylinositol 3-kinase) is composed of 85-kDa and 110-kDa subunits. The 85-kDa subunit acts as an adaptor, coupling the 110-kDa subunit (p110) to activated protein tyrosine kinases. PI3K was originally believed to phosphorylate the 3-hydroxy group of inositol phospholipids. PI3KCA activation, either by mutation or gene amplification, initiates a signal transduction pathway that promotes growth, metabolism, and survival in cancer cells [9, 10]. Activation of normal P53 protein may downregulate PIK3CA/Akt signaling [11]. It is also noteworthy that several reports have shown that amplification of PIK3CA is frequently associated with TP53 mutations [11–14].
Recently, Xing et al. reported that SNP rs17849071, which had been shown to be a germline genetic event, was inversely associated with PIK3CA amplification in follicular thyroid cancer. However, the main function of this SNP remains unclear. It would be interesting to elucidate the association between the rs17849071 SNP and clinically important characteristics, including P53 protein expression, and to explore the possible function of this SNP. In this study, we investigated the relationship between rs17849071 and the expression of ER, PR, HER2, P53, and Ki-67 in BCa. It was found that SNP rs17849071 was significantly and inversely associated with P53 protein expression in BCa.
Methods and materials
Patients and breast cancer samples
Tumor and tumor-adjacent tissue samples were obtained from 62 BCa patients diagnosed at the Anyang Tumor Hospital (Henan Province, China) between September 2010 and October 2011. The patients were all of Han descent and female. None of the patients had received pre-operative hormonal therapy related to their BCa prior to the biopsy/mastectomy procedure. Following surgery, standard immunohistochemical analysis was performed on tumor specimens and the results were confirmed by two experienced clinical pathologists. All tumors were classified according to the World Health Organization Histological Typing of Breast Tumors, and the clinical stage of each patient was determined according to the 5th Edition of the UICC TNM Classification of Malignant Tumors. The characteristics of patients and tumors are shown in Table 1. All patients signed an informed consent form, and the research protocol was approved by the hospital’s Institutional Review Board.
Immunohistochemical scoring
Histopathological analyses were performed using formalin-fixed, paraffin-embedded tumor tissue. Monoclonal mouse antibodies against ERα, PR, HER2, P53, and Ki-67 (1:50–1:200 dilution, DAKO, Denmark) were used. ER, PR, HER2, P53, and Ki-67 protein status was recorded in the pathology reports. Scoring was conducted using previously published criteria [14]. ER/PR staining was designated as positive when nuclear staining occurred in ≥10 % of tumor cells [15]. To assess HER2 expression, the membrane staining pattern was estimated and scored on a scale of 0–3+. Tumors with scores of ≥2 were considered to be positive for HER2 overexpression. For P53 protein, nuclear staining of tumor specimens was evaluated from a single slide by using a semiquantitative scoring system for intensity and percent of positive nuclei. The system assesses nuclear staining intensity using a 4-level ordered categorical variable (none or <10 % = 0, 10–25 % = 1, 25–50 % = 2, >50 % = 3). Tumors with a score of ≥1 for P53 were considered to be P53 protein-positive. A threshold of ≥20 % was considered to be Ki-67 positive.
Genomic DNA extraction, polymerase chain reaction, and DNA sequencing
DNeasy® Blood & Tissue Kits (QIAGEN 69506) were used to purify DNA from tumor tissues of BCa patients, according to the manufacturer’s instructions. A region of the PIK3CA gene containing rs17849071 in intron 9 was amplified using the primers 5′-GATTGGTTCTTTCCTGTCTCTG-3′ (forward) and 5′-CCACAAATATCAATTTACAACCATTG-3′ (reverse) [16]. PCR was performed using a previously described protocol [17]. Briefly, after an initial 3-min denaturing at 95 °C, each temperature was maintained for 40 s for 6 step-down increments, for 2 cycles each. For each of the step-down increments, the denaturing temperature was 95 °C and the extension temperature was 72 °C, with annealing temperatures of 66, 64, 62, 60, 58 and 56 °C. Subsequently, temperatures of 95, 54, and 72 °C were each maintained for 40 s for 30 cycles, followed by a final elongation step at 72 °C for 5 min. PrimeSTAR® HS DNA Polymerase (Takara Code: DR010A) was used to ensure high accuracy and amplification efficiency, according to the manufacturer’s instructions. PCR products were subjected to electrophoresis on a 1.5 % agarose gel, along with a molecular size marker (DL2000, TaKaRa), to confirm their quality. The PCR products were then sent to Taihe Biotechnology Co., Ltd. (Beijing, China), where all amplified PCR products were sequenced (ABI 3730xl DNA Analyzer, Applied Biosystems), using the sequencing primer 5′-TTGCTTTTTCTGTAAATCATCTGTG-3′.
Statistical analysis
Fisher’s exact test or chi-squared tests were used to assess associations among categorical variables. All P values were two-sided, and results were considered statistically significant at P < 0.05. Analyses were performed using SPSS 18.0 software (SPSS Inc., Chicago, IL, USA).
Results
P53 protein accumulation was significantly associated with HER2 overexpression and Ki-67 expression in BCa
Correlations between patient and tumor characteristics and P53 expression status are shown in Table 1. The BCa patients were all female, with a median age of 52.6 (range, 30–72) years. Most tumors were infiltrating ductal carcinomas (n = 60, 96.8 %), and 2 were infiltrating lobular carcinomas (n = 2, 3.2 %). Most tumors were in stage II (n = 45, 72.6 %). P53 protein accumulation was significantly associated with HER2 overexpression (P = 0.013) and Ki-67 expression (P = 0.007), but not with disease stage, maximum diameter, or ER or PR expression status.
Inverse relationship between heterozygous genotype GT, homozygous genotype of the minor allele G at rs17849071, and P53 expression in BCa
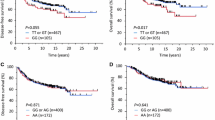
As shown in Fig. 1, in the 62 BCa specimens, three genotypes were identified by direct sequencing of intron 9 of the PIK3CA gene. The homozygous genotype TT (Fig. 1a) accounted for 88.7 % (n = 55) of cases, the heterozygous genotype GT (Fig. 1b) accounted for 9.7 % (n = 6) of cases, and the homozygous genotype of the minor allele G (Fig. 1c) at rs17849071 accounted for 1.6 % (n = 1) of cases. As Xing et al. reported, this SNP is a germline genetic event and it shows high frequency in health control [17]. We performed several PCR and gene sequencing tests in tumors, tumor-adjacent tissue, and blood samples from the same BCa patients and found the same results (data not shown). Of the 29 P53 protein-negative tumor samples, the GT/GG genotype accounted for 20.7 % (n = 6) of cases, but among the 33 P53 protein-positive samples, only 1 (3.0 %) sample with the GT/GG genotype was identified. As shown in Fig. 1d, P53 protein expression status was significantly and inversely associated with the heterozygous genotype GT, and the homozygous genotype of the minor allele G at rs17849071 in BCa specimens (P = 0.044).
Inverse relationship between the heterozygous genotype GT, the homozygous genotype of the minor allele G at rs17849071 and P53 expression in breast tumors. The homozygous genotype of the major allele T at rs17849071 (a). The heterozygous genotype of minor allele G and major allele T at rs17849071 (b). And the homozygous genotype of the minor allele G at rs17849071 (c). d shows that in the P53-negative group (n = 29), a larger number of cases and a higher percentage of heterozygous genotype GT and minor homozygous genotype GG (n = 6, 20.7 %) were found. In the P53-positive group (n = 33), only one heterozygote GT was identified (n = 1, 3.03 %). The difference was statistically significant (P = 0.044)
The association between rs17849071 polymorphism (T>G) and breast tumor characteristics
As shown in Table 2, six cases heterozygous for the minor allele G and the major allele T and one case homozygous for of the minor allele G at rs17849071 were identified among the 62 Chinese BCa patients. The other 55 subjects were all homozygous for the major allele, T, at rs17849071. No significant association was observed between the GT/GG genotype and ER, PR, HER2, or Ki-67 expression status. However, in the TT genotype group, the percentage of P53-positive subjects was strikingly higher than that in the GT/GG genotype group (58.2 vs. 14.3 %).
The distribution of P53 expression and rs17849071 in the clinicopathological surrogate subtypes of BCa
As suggested by the Expert Panel of the 13th St. Gallen International Breast Cancer Conference (2013), BCa can be divided into four main intrinsic subtypes [18]. As shown in Table 3, the percentage of P53-negative samples was highest in the Luminal A subtype (57.1 %) and lowest in the HER2 overexpression (20.0 %) subtype. The rs17849071 GT/GG genotype is most common in the Luminal A intrinsic subtype (14.3 %) and least common in the HER2 overexpression (0 %) subtype. However, with our relatively small sample size, no significant differences were observed in P53 expression status (P = 0.356) or rs17849071 polymorphism (T>G) (P = 0.813) among the different BCa intrinsic subtypes.
Discussion
TP53 mutation is a hallmark of cancer. It occurs in almost half of all human cancers and always results in the expression of a mutant P53 protein that has acquired transforming activity [19]. The majority of TP53 mutations result in the substitution of single amino acids in the central region of the P53 protein, generating a spectrum of variants [20]. P53 protein overexpression is associated with the presence of any TP53 mutation, especially missense mutations [2]. When mutations occur, the normal P53 tumor-suppressive functions are disrupted and P53 can instead acquire oncogenic properties via gain-of-function mechanisms.
Kim et al. [21] showed that overexpression of P53 is a prognostic marker for hormone receptor-positive BCa, especially in pre-menopausal women. Some reports have also shown that response to endocrine therapy is negatively associated with P53 expression status [22–24]. In the present study, we did not evaluate the prognostic value of P53 expression, but found that the percentage of P53 positive was high in the HER2 overexpression subtype, which is in accordance with previously published reports [25]. It should be noted that in our study, the percentage of P53 accumulation was even higher (87.5 %) in the Luminal B-like (HER2-positive) subtype (data not shown). These results may be explained by the relationship between P53 and HER2 expression. Yamashita et al. [26] reported that the coexistence of HER2 overexpression and P53 protein accumulation is a strong prognostic molecular marker in BCa; the authors also demonstrated a significant association between P53 and HER2 [26]. These data are in accordance with our results.
The most notable result of our study was the inverse relationship between P53 protein expression and the rs17849071 GT+GG genotype in BCa patients. This rs17849071 SNP was not associated with other clinical characteristics such as ER, PR, or HER2 expression. To date, the only data available for rs17849071 indicated that in follicular thyroid cancer, the occurrence of rs17849071 G/T was strikingly low, and that the heterozygous genotype (GT) was inversely associated with PIK3CA amplification in thyroid tumors [17]. Evaluating the relationship between P53 protein expression and PIK3CA amplification may further illuminate the mechanisms underlying the observed results.
PIK3CA is the second most frequently mutated gene in BCa, following the TP53 gene. PIK3CA is also associated with various types of cancer [13, 27]. PIK3CA amplification is believed to enhance PI3 K signaling and Akt activity and subsequently to promote cellular proliferation and survival. Typical markers of PI3 K pathway activation, such as pAKT, pS6, and p4EBP1, are highly expressed in the basal-like and HER2E mRNA subtypes and are correlated with PIK3CA amplification [8].
Singh et al. [28] reported that P53 negatively regulates PIK3CA transcript and protein levels in a PTEN-independent manner. Furthermore, Astanehe et al. [29] reported that P53 can directly bind to the PIK3CA promoter and inhibit its activity. Inactivation of P53 may lead to subsequent upregulation of PIK3CA and its downstream signaling. In a genomic landscape study, TP53 mutations were found to be closely related to copy number gains of 3q26, where PIK3CA was located [30]. In fact, many studies have shown that TP53 mutations are positively associated with PIK3CA amplification in various types of tumors [14, 29, 31]. In this study, we showed that the rs17849071 SNP is inversely associated with P53 protein accumulation in BCa. Further studies investigating whether this SNP is also inversely associated with TP53 mutations, as well as PIK3CA amplification in BCa are warranted.
The following limitations of the present study should be considered. The sample size was relatively small, and the results should be confirmed in larger studies. Furthermore, although immunohistochemical staining is a widely used method, it is semiquantitative and subjective, and the results depend on the threshold set during scoring. It should be noted that some types of TP53 mutations might also lead to negative results of P53 protein detection by IHC. Direct detection of TP53 mutations in tumors may provide more accurate data.
In summary, we analyzed associations between breast tumor characteristics and P53 expression status and found that P53 protein accumulation is significantly associated with HER2 overexpression and Ki-67 expression. We further evaluated the association between the rs17849071 polymorphism (T>G) and breast tumor characteristics and found a significant inverse relationship between P53 protein expression and the rs17849071 GT+GG genotype in Chinese BCa patients. Future studies employing larger sample sizes will be necessary to confirm these results and to evaluate the relationship between the rs17849071 SNP and the TP53 mutation and PIK3CA amplification in BCa patients. It will also be necessary to evaluate the potential prognostic value of this SNP in BCa, especially in various BCa subtypes. Meanwhile, studies that explore the potential molecular mechanisms linking rs17849071 to P53 protein overexpression are warranted.
References
Montazeri A. Health-related quality of life in breast cancer patients: a bibliographic review of the literature from 1974 to 2007. J Exp Clin Cancer Res. 2008;27(1):32.
Rossner P Jr, Gammon MD, Zhang YJ, et al. Mutations in p53, p53 protein overexpression and breast cancer survival. J Cell Mol Med. 2009;13(9b):3847–57.
Rohan TE, Hartwick W, Miller AB, et al. Immunohistochemical detection of c-erbB-2 and p53 in benign breast disease and breast cancer risk. J Natl Cancer Inst. 1998;90(17):1262–9.
Rohan TE, Li SQ, Hartwick R, et al. p53 Alterations and protein accumulation in benign breast tissue and breast cancer risk: a cohort study. Cancer Epidemiol Biomark Prev. 2006;15(7):1316–23.
Caffo O, Doglioni C, Veronese S, Bonzanini M, Marchetti A, Buttitta F, Fina P, Leek R, Morelli L, Palma PD, et al. Prognostic value of p21(WAF1) and p53 expression in breast carcinoma: an immunohistochemical study in 261 patients with long-term follow-up. Clin Cancer Res. 1996;2:1591–9.
Montero S, Guzman C, Vargas C, Ballestin C, Cortes-Funes H, Colomer R. Prognostic value of cytosolic p53 protein in breast cancer. Tumour Biol. 2001;22:337–44.
Linjawi A, Kontogiannea M, Halwani F, Edwardes M, Meterissian S. Prognostic significance of p53, bcl-2, and Bax expression in early breast cancer. J Am Coll Surg. 2004;198:83–90.
Cancer Genome Atlas Network. Comprehensive molecular portraits of human breast tumours. Nature. 2012;490(7418):61–70.
Gaikwad SM, Ray P. Non-invasive imaging of PI3 K/Akt/mTOR signalling in cancer. Am J Nucl Med Mol Imag. 2012;2(4):418–31.
Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature. 2011;474(7353):609–15.
Kolasa IK, Rembiszewska A, Felisiak A, et al. PIK3CA amplification associates with resistance to chemotherapy in ovarian cancer patients. Cancer Biol Ther. 2009;8(1):21–6.
Lee JW, Soung YH, Kim SY, et al. PIK3CA gene is frequently mutated in breast carcinomas and hepatocellular carcinomas. Oncogene. 2005;24(8):1477–80.
Campbell IG, Russell SE, Choong DYH, et al. Mutation of the PIK3CA gene in ovarian and breast cancer. Cancer Res. 2004;64(21):7678–81.
Kadota M, Sato M, Duncan B, et al. Identification of novel gene amplifications in breast cancer and coexistence of gene amplification with an activating mutation of PIK3CA. Cancer Res. 2009;69(18):7357–65.
Stemke-Hale K, Gonzalez-Angulo AM, Lluch A, et al. An integrative genomic and proteomic analysis of PIK3CA, PTEN, and AKT mutations in breast cancer. Cancer Res. 2008;68(15):6084–91.
Samuels Y, Wang Z, Bardelli A, et al. High frequency of mutations of the PIK3CA gene in human cancers. Science. 2004;304(5670):554.
Xing JC, Tufano RP, Murugan AK, et al. Single nucleotide polymorphism rs17849071 G/T in the PIK3CA gene is inversely associated with follicular thyroid cancer and PIK3CA amplification. PLoS ONE. 2012;7(11):e49192.
Goldhirsch A, Winer EP, Coates AS, et al. Personalizing the treatment of women with early breast cancer: highlights of the St. Gallen international expert consensus on the primary therapy of early breast cancer 2013. Ann Oncol. 2013;24(9):2206–23.
Vousden KH, Lu X. Live or let die: the cell’s response to p53. Nat Rev Cancer. 2002;2(8):594–604.
Walerych D, Napoli M, Collavin L, et al. The rebel angel: mutant p53 as the driving oncogene in breast cancer. Carcinogenesis. 2012;33(11):2007–17.
Kim HS, Yom CK, Kim HJ, et al. Overexpression of p53 is correlated with poor outcome in premenopausal women with breast cancer treated with tamoxifen after chemotherapy. Breast Cancer Res Treat. 2010;121(3):777–88.
Knoop AS, Bentzen SM, Nielsen MM, et al. Value of epidermal growth factor receptor, HER2, p53, and steroid receptors in predicting the efficacy of tamoxifen in high-risk postmenopausal breast cancer patients. J Clin Oncol. 2001;19(14):3376–84.
Berry DA, Muss HB, Thor AD, et al. HER-2/neu and p53 expression versus tamoxifen resistance in estrogen receptor–positive, node-positive breast cancer. J Clin Oncol. 2000;18(20):3471–9.
Berns EM, Klijn JG, Van Putten WL, et al. p53 protein accumulation predicts poor response to tamoxifen therapy of patients with recurrent breast cancer. J Clin Oncol. 1998;16(1):121–7.
Jung SY, Jeong J, Shin SH, et al. Accumulation of p53 determined by immunohistochemistry as a prognostic marker in node negative breast cancer; analysis according to St Gallen consensus and intrinsic subtypes. J Surg Oncol. 2011;103(3):207–11.
Yamashita H, Nishio M, Toyama T, et al. Coexistence of HER2 over-expression and p53 protein accumulation is a strong prognostic molecular marker in breast cancer. Breast Cancer Res. 2004;6(1):R24–30.
Ma YY, Wei SJ, Lin YC, et al. PIK3CA as an oncogene in cervical cancer. Oncogene. 2000;19(23):2739–44.
Singh B, Reddy PG, Goberdhan A, et al. p53 regulates cell survival by inhibiting PIK3CA in squamous cell carcinomas. Genes Dev. 2002;16(8):984–93.
Astanehe A, Arenillas D, Wasserman WW, et al. Mechanisms underlying p53 regulation of PIK3CA transcription in ovarian surface epithelium and in ovarian cancer. J Cell Sci. 2008;121(5):664–74.
Wojnarowicz PM, Oros KK, Quinn MCJ, et al. The genomic landscape of TP53 and p53 annotated high grade ovarian serous carcinomas from a defined founder population associated with patient outcome. PLoS ONE. 2012;7(9):e45484.
Nakayama K, Nakayama N, Jinawath N, et al. Amplicon profiles in ovarian serous carcinomas. Int J Cancer. 2007;120(12):2613–7.
Acknowledgments
This work was supported by Funding from the Guang’anmen’s Hospital (Grant No. 2011S244).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Standards
We declare that the experiments comply with the current laws of China.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pang, B., Sun, SP., Gao, L. et al. A single nucleotide polymorphism in PIK3CA gene is inversely associated with P53 protein expression in breast cancer. Med Oncol 31, 30 (2014). https://doi.org/10.1007/s12032-014-0030-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0030-8