Abstract
Transforming growth factor β1 (TGF-β1) and inhibitor of differentiation/DNA-binding 1 (Id-1) have been shown to be associated with aggressive metastatic behavior of cancer cells in many malignant tumors. However, their role in gastric cancer (GC) has not been established. In this study, we investigated the relationship between expression of Id-1 and TGF-β1 in GC as well as their association with GC progression. The immunohistochemical analysis of 71 human GC samples indicated that both Id-1 and TGF-β1 were markedly upregulated in tumor tissue compared with the adjacent tissue; in addition, a significant positive correlation was found between the expression levels of Id-1 and TGF-β1 by Pearson’s correlation analysis. Furthermore, the investigation of the association of Id-1 and TGF-β1 with patient clinical characteristics revealed that Id-1 expression was significantly correlated with tumor differentiation, while TGF-β1 was associated with lymph node metastasis. The results were validated in vitro by using a GC cell line, AGS. The expression of Id-1 was upregulated at 24 and 48 h after the treatment with TGF-β1, whereas it did not affect the proliferation of cells. TGF-β1 also influenced the expression of N-cadherin and β-catenin. Our results suggested that Id-1 and TGF-β1 played important roles in the progression of GC, in which Id-1 might act as a downstream mediator of TGF-β1 signaling through a regulatory mechanism involving N-cadherin and β-catenin. The TGF-β1/Id-1 axis might serve as a future therapeutic target for GC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Gastric cancer (GC) is one of the most common malignancies worldwide. Despite the declining incidence, GC remains the second leading cause of cancer-related deaths [1, 2]. The advances in diagnostic techniques and treatment strategies ensure an early detection and low mortality rate for early stages of GC [3, 4]; however, the candidate prognostic biomarkers for patients with advanced metastasized GC need to be further explored.
Inhibitor of cell differentiation/DNA-binding (Id) proteins is a family of helix–loop–helix (HLH) transcription factors (Id-1–Id-4). They regulate cell cycle and cell differentiation by antagonizing the DNA-binding activity of basic HLH transcription factors [5]. Accumulated evidence suggests that Id-1 plays multiple roles in the progression of various cancers via stimulation of angiogenesis [6, 7], inhibition of differentiation [8, 9], and induction of metastasis [10–13]. Clinical studies involving GC patients have revealed a significant association of Id-1 overexpression with cancer invasion and metastasis [14–16]. Further studies demonstrate that inhibition of GC cells differentiation by Id-1 contributes to GC progression [17, 18]. However, the molecular mechanism underlying Id-1 functions in GC progression is not fully elucidated.
Transforming growth factor β1 (TGF-β1), polypeptide belonging to the TGF-β family of growth factors, is shown to be upregulated in the tumor microenvironment and contributes to tumor metastasis [19, 20]. Once TGF-β1 binds to its receptor, the receptor is phosphorylated and then activates the downstream signaling mediator SMAD2/3 to exert its biological activities [21]. It has been reported that overexpression of TGF-β1 in head and neck epithelia causes severe inflammation and angiogenesis, which may consequently contribute to the malignant phenotype mediated by vascular endothelial growth factor (VEGF) and activin receptor-like kinase 1 (ALK1) [22–24]. Previous findings have also shown that TGF-β1 induces migration and invasion of tumor cells and promotes metastasis by upregulating the protein level of matrix metalloproteinase-9 [25, 26].
Although both Id-1 and TGF-β1 are involved in tumor progression, their interrelationship in carcinogenesis requires further clarification. To date, several reports have suggested that Id-1 expression may be involved in TGF-β-signaling pathway, but the data are controversial. Id-1 expression is downregulated by TGF-β1 in prostate epithelial cell lines [27–29]. On the contrary, Id-1 proves to be significantly upregulated by stimulating TGF-β3 in endothelial cells [30], and TGF-β1 in metastatic breast tumor cells [31] and in prostate cancer cells [32]. However, to the best of our knowledge, there are no reports elucidating the relationship between TGF-β1 and Id-1 and their functions in GC progression.
In this study, we investigated the relationship between Id-1 and TGF-β1 in shaping the permissive GC microenvironment. The results showed that the expression of Id-1 and TGF-β1 was increased in GC tissue compared with that in the adjacent tissue and was positively associated with tumor differentiation and lymph node metastasis, respectively. Moreover, a significant positive correlation between the expression of Id-1 and TGF-β1 was revealed in GC tissue. These results were further validated in GC AGS cells, which showed an increase of Id-1 expression, as well as N-cadherin and β-catenin, after stimulation with TGF-β1.
Materials and methods
Tissue specimens
Seventy-one GC patients who received surgical treatment at Zhongshan Hospital (Shanghai, China) between June 2011 and December 2011 were enrolled in our study. The evaluation of the resected tumor specimens was performed according to the guidelines of the Japanese Gastric Carcinoma Association. Stage grading was performed in accordance with the TNM classification of gastric carcinoma (UICC). None of the patients received radiotherapy, chemotherapy, or other medical interventions before the surgery. Specimens were collected only from patients who underwent complete clinical and pathological evaluation. Informed consent was obtained from all individuals. The study was approved by the Research Ethics Committee of Zhongshan Hospital.
Immunohistochemistry
Tumors and adjacent non-cancerous tissue samples were harvested from the 71 GC patients, fixed in formaldehyde and embedded in paraffin. Immunohistochemistry of paraffin sections (5 μm) was carried out using a two-step protocol. Briefly, sections were deparaffinized with xylene and rehydrated with graded ethanol solutions. After blocking the endogenous peroxide activity by incubation in 0.3 % H2O2, antigen retrieval was performed by placing the sections in boiling citrate or ethylenediamine tetraacetic acid (EDTA) buffer for 10 min, and non-specific binding sites were blocked with 5 % goat serum in 1× phosphate buffered saline (1× PBS, pH 7.4). The slides were incubated with primary antibodies against Id-1 and TGF-β1 (1:25 and 1:200, respectively; Abcam; MA, USA), horseradish peroxidase (HRP)-conjugated secondary antibodies (1:200; KPL; MD, USA), and 3,3′-diaminobenzidine (DAB) solution (Sigma-Aldrich; MO, USA). Negative control slides without the primary antibodies were included in all assays. All specimens were counterstained with hematoxylin and examined under light microscopy.
Evaluation of immunohistochemical staining
Each immunostained slide was observed at 200× and 400× magnifications. At least five 400× magnification images were processed and analyzed using ImageJ software (National Institutes of Health; Bethesda, MD, USA). For each specimen, the percentages of positively stained areas relative to the total observed areas of tumor cell (% area) were determined. The average percentage was calculated to ensure the sample representativeness and homogeneity for accurate statistical analysis.
Cell line and culture conditions
The human gastric adenocarcinoma AGS cell line was maintained in a 5 % CO2-humidified atmosphere at 37 °C in RPMI-1640 medium (Biowest; France) supplemented with 10 % fetal bovine serum (FBS; Biowest).
Immunocytochemistry
AGS cells were seeded in 24-well plates with cover slips in RPMI-1640 supplemented with 10 % FBS. After cell attachment, the medium was changed to 1 % FBS with or without TGF-β1 (10 ng/mL; PeproTech; NJ, USA) and continuously cultured. The cells were collected at 24 and 48 h, respectively, fixed with 4 % paraformaldehyde for 15 min and permeabilized with 0.3 % Triton X-100 for 10 min. After blocking with 5 % goat serum in 1× PBS with 0.3 % Triton X-100, the cells were incubated with mouse anti-Id-1 (1:25), rabbit anti-N-cadherin (1:200; Epitomics; USA), and rabbit anti-β-catenin (1:200; Abcam) overnight at 4 °C. Cell monolayers were then incubated with fluorescein isothiocyanate (FITC)-labeled secondary antibody (1:200; KPL) for 2 h at room temperature and stained with 1 μg/μL of 4′,6-diamidino-2-phenylindole (DAPI; Sigma-Aldrich; USA) in PBS with 0.3 % Triton X-100. After three washes with 1× PBS, the slides were mounted and analyzed using a fluorescence microscope (magnification ×200; H55OS; Nikon; Japan) or a laser-scanning confocal microscope (magnification ×400; TCS-SP5; Leica Camera AG; Germany).
Western blotting
Cells were treated as described above and harvested at the indicated time points. Whole-cell lysates were prepared by re-suspending cells in RIPA lysis buffer (Beyotime; China), and protein concentrations were measured using the BCA protein assay kit (Beyotime). Equal amounts of denatured proteins were resolved by polyacrylamide gel electrophoresis and analyzed by immunoblotting with primary antibodies against Id-1 (1:50), Snail (1:500), β-catenin (1:2,000), Twist (1:100) (all from Abcam), E-cadherin (1:2,000), N-cadherin (1:6,000), and Vimentin (1:3,000) (all from Epitomics); GAPDH (1:10,000; KangChen Bio-tech Inc., China) was used as a loading control. After the incubation with HRP-conjugated secondary antibodies (1:4,000), the signals were visualized by the ECL system (Thermo Fisher Scientific Inc., MA, USA) and quantified using a Gel-Pro analyzer (Media Cy-bernetics Inc., Silver Spring, MD, USA). The experiments were performed in triplicate.
Cell proliferation assay
Cell proliferation was quantitatively evaluated using the Cell Count kit-8 (CCK-8; Beyotime, China). Cells were plated in 96-well plates at a density of 2 × 104 cells/mL. After 12 h of incubation, RPMI-1640 with 1 % FBS and TGF-β1 was added to the experimental group. The cells were incubated for the indicated times. CCK-8 solution (10 μL) was then added to each well, and cells were incubated for an additional 2 h at 37 °C. The absorbance at 450 nm (OD450) was determined using a microplate reader (Model 680; Bio-Rad, CA, USA); RPMI 1640 containing 10 μL CCK-8 was used as blank. The proliferation index (PI) was calculated using the formula: PI = OD450 of the experimental group/OD450 of the control group.
Statistical analysis
Experimental data were presented as the mean + SEM of at least three independent experiments performed in duplicate. Statistical analysis was performed using GraphPad Prism 5 (GraphPad Software; USA) and SPSS 20.0 software (SPSS; Chicago, IL, USA). Differences between tumor and adjacent tissue were analyzed by the Wilcoxon test. To assess the relationship between variables and clinical pathology parameters, all cases were divided into high and low expression groups (classified by the median value), and then a chi-squared test was performed. Pearson’s correlation analysis was used to explore the association between Id-1 and TGF-β1. Two-tailed levels of significance were used and P < 0.05 was considered statistically significant.
Results
Clinical and pathological characteristics of GC patients
The clinic-pathological characteristics of 71 gastric carcinoma patients were summarized in Table 1. The specimens included 47 male (66.2 %) and 24 female (33.8 %). The cutoffs of age and tumor size were set at their median values, 62 and 4 cm, respectively. The patients underwent surgical resection including radical (65, 91.6 %) and palliative (6, 8.4 %) gastrectomy. Differentiated tumors were classified as stage II (15 patients, 21.1 %) and III (56, 78.9 %). As defined by the location of primary tumor, T1 was diagnosed in 3 (4.2 %) cases, whereas T2 in 12 (16.9 %) cases, T3 in 12 (16.9 %) cases, and T4 in 44 (62.0 %) cases. Regional lymph nodes metastasis and distant metastasis were diagnosed in 48 (67.6 %) and 7 (9.9 %) cases, respectively. The TNM stage grouping was distributed as follows: I, 11 cases, 15.5 %; II, 20 cases, 28.2 %; III, 33 cases, 46.5 %; and IV, 7 cases, 9.8 %.
Expression of Id-1 and TGF-β1 in GC tissue
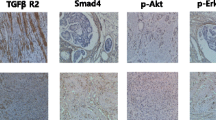
Specimens collected from tumor and adjacent tissues of GC patients were analyzed for Id-1 and TGF-β1 expression by immunohistochemistry. Representative images of Id-1 and TGF-β1 immunostaining were shown in Fig. 1a–h. Id-1 expression was predominantly observed in the cytoplasm of GC cells. The expression of TGF-β1 was identified as positive in the cytoplasm of tumor cells. The expression of Id-1 and TGF-β1 was quantitatively evaluated as the percentage of positively stained area relative to the total analyzed cell area (% area); the statistical results were shown in Table 2 and Fig. 1i. Compared with the adjacent tissue, GC tissue showed significantly higher levels of both Id-1 (P < 0.01) and TGF-β1 (P < 0.01).
Id-1 and TGF-β1 expression in 71 human gastric carcinoma. a–h Representative Id-1 and TGF-β1 immunohistochemistry images of adjacent tissue and tumor tissue. Magnification: a, c, e, and g ×200; b, d, f, and h ×400. i Statistical summary of Id-1 and TGF-β1 staining intensity in adjacent tissue and tumor tissue (**P < 0.01). Note that increased Id-1 and TGF-β1 expression in tumor tissue was observed in adjacent tissue. Error bars represent the mean intensity + SEM
Association between Id-1 and TGF-β1 expression and clinical characteristics
Further analyses were undertaken to evaluate the association of the levels of Id-1 and TGF-β1 in tumors with the clinical parameters of 71 GC patients. Based on Id-1 and TGF-β1 expression levels determined as % area by immunohistochemistry (median expression values were 3.407 and 8.344, respectively), the patients were divided into high and low expression groups. As shown in Table 3, the statistical analysis by chi-square test revealed no significant correlation of Id-1 and TGF-β1 expression with patients’ age, gender, tumor size, primary tumor parameters (T stage), distant metastasis, and TNM stage grouping. However, Id-1 showed a statistically significant association with tumor differentiation (P = 0.048), whereas TGF-β1 levels were positively correlated with regional lymph node metastasis (P = 0.028).
Correlation between Id-1 and TGF-β1 expression
The association between Id-1 and TGF-β1 levels in tumor tissue was assessed by Pearson’s correlation analysis. The results shown in Fig. 2 revealed a significant positive correlation between Id-1 and TGF-β1 expression levels (r = 0.503, P < 0.01): in the scatter plot, the linear regression analysis was carried out to show the linear trend between the two variables, indicating an apparent association between Id-1 and TGF-β1 in GC.
Id-1 expression stimulated by TGF-β1 in AGS cells
Based on the verified correlation between Id-1 and TGF-β1 in human specimens, we further investigated Id-1 expression following the treatment with TGF-β1 in GC cell line AGS in vitro. Immunocytochemistry analysis revealed that Id-1 was localized to the cell cytoplasm and nucleus (Fig. 3a–c), while Western blotting results showed Id-1 upregulation in TGF-β1-treated AGS cells compared with untreated cells (P < 0.05, Fig. 3d, e). The effect of TGF-β1 on cellular proliferation was assessed by the treatment of cells with different concentrations of TGF-β1 (0, 2, 5, 10, 20, and 50 ng/mL) by CCK-8 assay. The results showed that there was no significant difference in the proliferation between TGF-β1-treated cells and control cells, irrespective of the incubation time (Fig. 3f). Overall, these results showed that TGF-β1 upregulated Id-1 expression in GC cells independent of cell proliferation.
Effect of TGF-β1 on Id-1 expression and proliferation in AGS cells. a and b Expression of Id-1 protein was detected by immunofluorescence at 24 h (a) and 48 h (b) in the absence or presence of 10 ng/mL TGF-β1. The representative images were acquired with a magnification of ×200. c Statistical data were represented as the average gray value + SEM of three independent experiments (*P < 0.05). d and e Western blotting analysis of Id-1 protein expression. GAPDH was used as an internal control. Each bar represents the mean + SEM (*P < 0.05). The results were consistent with data of immunofluorescence. f Effect of different concentrations of TGF-β1 on AGS cells was determined by CCK-8 at 24 and 48 h. No difference was found among the six groups
Expression of epithelial-mesenchymal transition-related proteins
The epithelial-mesenchymal transition (EMT) occurs as a key process in tumor metastasis [33]. To investigate whether TGF-β1 affects EMT in GC, we assessed the expression of EMT-related proteins in TGF-β1-treated AGS cells. The levels of N-cadherin, Vimentin, β-catenin, Snail, and Twist were evaluated after stimulation by TGF-β1. Western blotting results revealed that N-cadherin and β-catenin were significantly upregulated by TGF-β1 (P < 0.05 and P < 0.01, respectively), but there was no change in Vimentin, Snail, and Twist levels compared with control cells (Fig. 4a, b). These results were corroborated by the cell immunofluorescence staining (Fig. 4c–f). Besides, the staining results further showed the distributions of detected proteins in AGS cells. N-cadherin was localized to cell membrane, whereas β-catenin was detected in cytoplasm (as shown in Fig. 4c, d). Vimentin was found in cytoplasm, while Snail was expressed in nucleus (as shown in Fig. 4e, f).
Expression changes of EMT-related proteins. a Expression levels of N-cadherin, vimentin, β-catenin, Snail, Twist, and GAPDH were detected by Western blotting at 24 h in the absence or presence of 10 ng/mL TGF-β1. GAPDH was used as an internal control. b Statistical data of Western blotting were represented as the average gray value + SEM of three independent experiments (*P < 0.05; **P < 0.01). All the data were normalized by the expression of GAPDH. c–f Cellular immunofluorescence staining of N-cadherin, β-catenin, vimentin, and snail. The representative images were acquired with a magnification of ×400 under laser-scanning confocal microscope
Discussion
In recent years, the relationship between Id-1 and TGF-β1 has become a promising direction in cancer research. In metastatic breast tumor cells, Id-1 levels increase almost twofold in response to TGF-β1 stimulation, suggesting that Id-1 may be a mediator of TGF-β-induced responses to facilitate tumor reinitiation [31]. In addition, it has been demonstrated that SMAD, the classical downstream mediator of TGF-β1 signaling, can directly interact with Id-1 in promoting breast tumors for lung metastasis [34, 35]. A recent study of prostate cancer cells also demonstrates that TGF-β1 increases the proliferation and migration of cancer cells by upregulating the expression of Id-1 [32]. Taken together, these findings imply that Id-1 is a TGF-β1 target gene and their vital roles in affecting the metastasizing potential of cancer cells.
In this study, we found that the expression levels of Id-1 and TGF-β1 in 71 human GC samples were higher than those in the adjacent tissue, which was consistent with previous findings. Higher Id-1 expression has been also detected in human ovarian tumors compared with borderline tumors [8]; similar results have been obtained in prostate cancer biopsy samples [36] and esophageal squamous cell carcinoma specimens [11]. The aberrant expression of TGF-β1 has been linked to pathological conditions in urinary tract [37], plasma [38], and tumor specimens [39–41]. The results of our study showed that the expression of Id-1 was related to tumor differentiation, while TGF-β1 expression was associated with regional lymph node metastasis, suggesting that Id-1 and TGF-β1 levels could be significant predictors of gastric carcinoma progression.
Another novel finding of this study was the positive correlation between the expression of Id-1 and TGF-β1 in GC. Id-1 has been identified as a regulator of VEGF, and the combination of these two proteins has been proposed as a potential target for cancer therapy [42, 43]. It has been established that Id-1 is co-expressed with a number of factors implicated in cancer cell invasiveness, including CD44 [44], epidermal growth factor receptor (EGFR) [45], and thrombospondin 1 (TSP-1) [46]; however, the relationship between Id-1 and TGF-β1 remains unclear. Here, we found that the expression of Id-1 showed a statistically significant positive correlation with that of TGF-β1. To the best of our knowledge, this is the first demonstration of a direct association between Id-1 and TGF-β1 in GC, which suggests that the combination of Id-1 and TGF-β1 might promote the invasion and progression of GC.
In order to validate the clinical findings and further explore the possible mechanism, in vitro experiments on AGS cell line were performed. After the treatment of TGF-β1, the expression of Id-1 increased and this elevation might relate to time. This demonstrated that Id-1 might mediate the downstream effects of the TGF-β pathway. These results are in agreement with the findings in breast and prostate cancers [31, 32], but incompatible with those in breast epithelial cells, where TGF-β inhibited Id-1 expression [47]. This switched expression of Id-1 in response to TGF-β1 may be caused by the loss of TGF-β growth-inhibitory responses [35]. At the same time, we examined the effect of TGF-β1 on the proliferation of AGS at different concentrations. The results showed that Id-1 expression induced by TGF-β1 was independent of cell number.
Given the well-established relationship between EMT, tumor metastasis, and TGF-β1, we also examined the expression of EMT-related proteins [48, 49]. We found that N-cadherin and β-catenin expression was significantly upregulated by TGF-β1 treatment, which was consistent with previous results showing the association between EMT proteins and TGF-β1. We proposed that N-cadherin and β-catenin are upregulated by TGF-β1 via Id-1, because earlier data have indicated that the expression of Id-1 has a positive correlation with that of N-cadherin and β-catenin, probably via the PI3K/Akt signaling pathway [50, 51]. Besides, one recent research in breast cancer has revealed that TGF-β1 can induce Id-1 expression, while Snail or Twist overexpresses [52]. Therefore, based on our data and previous findings, we propose a hypothesis that TGF-β1 stimulates the expression of Id-1, which in turn upregulates the levels of N-cadherin and β-catenin through activation of the PI3K/Akt signaling pathway. This hypothesis needs further experimental support.
In conclusion, our study demonstrated that both Id-1 and TGF-β1 were upregulated in GC compared with the adjacent tissue and that this effect was related to GC progression. Moreover, the expression of Id-1 was positively correlated with that of TGF-β1 in GC samples. The experiments in vitro showed that Id-1 levels were upregulated by TGF-β1, further confirming the association between Id-1 and TGF-β1 in GC. These results indicate that in gastric tumor cells, Id-1 may be a specific downstream target of TGF-β1, suggesting important roles of Id-1 and TGF-β1 in GC development. Thus, this study provides new insights into the mechanism by which TGF-β1/Id-1 axis control tumor progression and may lead to new treatment strategies in GC.
References
Hartgrink HH, Jansen EP, van Grieken NC, van de Velde CJ. Gastric cancer. Lancet. 2009;374(9688):477–90.
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Oue N, Aung PP, Mitani Y, Kuniyasu H, Nakayama H, Yasui W. Genes involved in invasion and metastasis of gastric cancer identified by array-based hybridization and serial analysis of gene expression. Oncology. 2005;69(Suppl. 1):17–22.
Yasui W, Oue N, Aung PP, Matsumura S, Shutoh M, Nakayama H. Molecular-pathological prognostic factors of gastric cancer: a review. Gastric Cancer. 2005;8(2):86–94.
Perk J, Iavarone A, Benezra R. Id family of helix–loop–helix proteins in cancer. Nat Rev Cancer. 2005;5(8):603–14.
Lyden D, Young AZ, Zagzag D, Yan W, Gerald W, O’Reilly R, et al. Id1 and Id3 are required for neurogenesis, angiogenesis and vascularization of tumour xenografts. Nature. 1999;401(6754):670–7.
Volpert OV, Pili R, Sikder HA, Nelius T, Zaichuk T, Morris C, et al. Id1 regulates angiogenesis through transcriptional repression of thrombospondin-1. Cancer Cell. 2002;2(6):473–83.
Schindl M, Schoppmann SF, Ströbel T, Heinzl H, Leisser C, Horvat R, et al. Level of Id-1 protein expression correlates with poor differentiation, enhanced malignant potential, and more aggressive clinical behavior of epithelial ovarian tumors. Clin Cancer Res. 2003;9(2):779–85.
Kebebew E, Peng M, Treseler PA, Clark OH, Duh Q-Y, Ginzinger D, et al. Id1 gene expression is up-regulated in hyperplastic and neoplastic thyroid tissue and regulates growth and differentiation in thyroid cancer cells. J Clin Endocrinol Metab. 2004;89(12):6105–11.
Fong S, Itahana Y, Sumida T, Singh J, Coppe J-P, Liu Y, et al. Id-1 as a molecular target in therapy for breast cancer cell invasion and metastasis. Proc Natl Acad Sci. 2003;100(23):13543–8.
Yuen H, Chan Y, Chan K, Chu Y, Wong ML, Law SY, et al. Id-1 and Id-2 are markers for metastasis and prognosis in oesophageal squamous cell carcinoma. Br J Cancer. 2007;97(10):1409–15.
Soroceanu L, Murase R, Limbad C, Singer E, Allison J, Adrados I, et al. Id-1 is a key transcriptional regulator of glioblastoma aggressiveness and a novel therapeutic target. Cancer Res. 2013;73(5):1559–69.
Sumida T, Murase R, Onishi-Ishikawa A, McAllister SD, Hamakawa H, Desprez P-Y. Targeting Id1 reduces proliferation and invasion in aggressive human salivary gland cancer cells. BMC Cancer. 2013;13(1):141.
Oien KA, Vass JK, Downie I, Fullarton G, Keith WN. Profiling, comparison and validation of gene expression in gastric carcinoma and normal stomach. Oncogene. 2003;22(27):4287–300.
Wang Q, Tsao SW, Fu S, Xue W, Meng X, Feng H, et al. Overexpression of Id-1 in gastric adenocarcinoma: implication for a novel diagnostic marker. Anticancer Res. 2004;24(2B):881–6.
Iwatsuki M, Fukagawa T, Mimori K, Nakanishi H, Ito S, Ishii H, et al. Bone marrow and peripheral blood expression of ID1 in human gastric carcinoma patients is a bona fide indicator of lymph node and peritoneal metastasis. Br J Cancer. 2009;100(12):1937–42.
Han S, Guo C, Hong L, Liu J, Liu C, Wang J, et al. Expression and significance of Id1 helix–loop–helix protein overexpression in gastric cancer. Cancer Lett. 2004;216(1):63–71.
Jang TJ, Jung KH, Choi EA. Id-1 gene downregulation by sulindac sulfide and its upregulation during tumor development in gastric cancer. Int J Cancer. 2006;118(6):1356–63.
Massague J. The transforming growth factor-beta family. Annu Rev Cell Biol. 1990;6(1):597–641.
Yang L, Pang Y, Moses HL. TGF-β and immune cells: an important regulatory axis in the tumor microenvironment and progression. Trends Immunol. 2010;31(6):220–7.
Massagué J, Blain SW, Lo RS. TGFβ signaling in growth control, cancer, and heritable disorders. Cell. 2000;103(2):295–309.
Lu S-L, Reh D, Li AG, Woods J, Corless CL, Kulesz-Martin M, et al. Overexpression of transforming growth factor β1 in head and neck epithelia results in inflammation, angiogenesis, and epithelial hyperproliferation. Cancer Res. 2004;64(13):4405–10.
Oh SP, Seki T, Goss KA, Imamura T, Yi Y, Donahoe PK, et al. Activin receptor-like kinase 1 modulates transforming growth factor-β1 signaling in the regulation of angiogenesis. Proc Natl Acad Sci. 2000;97(6):2626–31.
Benckert C, Jonas S, Cramer T, von Marschall Z, Schäfer G, Peters M, et al. Transforming growth factor β1 stimulates vascular endothelial growth factor gene transcription in human cholangiocellular carcinoma cells. Cancer Res. 2003;63(5):1083–92.
Sun L, Diamond ME, Ottaviano AJ, Joseph MJ, Ananthanarayan V, Munshi HG. Transforming growth factor-β1 promotes matrix metalloproteinase-9-mediated oral cancer invasion through Snail Expression. Mol Cancer Res. 2008;6(1):10–20.
Gomes LR, Terra LF, Wailemann RA, Labriola L, Sogayar MC. TGF-β1 modulates the homeostasis between MMPs and MMP inhibitors through p38 MAPK and ERK1/2 in highly invasive breast cancer cells. BMC Cancer. 2012;12(1):26.
Ling M, Wang X, Tsao S, Wong Y. Down-regulation of Id-1 expression is associated with TGFβ1-induced growth arrest in prostate epithelial cells. Biochim Biophys Acta (BBA) Gen Subj. 2002;1570(3):145–52.
Di K, Wong YC, Wang X. Id-1 promotes TGF-β1-induced cell motility through HSP27 activation and disassembly of adherens junction in prostate epithelial cells. Exp Cell Res. 2007;313(19):3983–99.
Di K, Ling MT, Tsao SW, Wong YC, Wang X. Id-1 modulates senescence and TGF-β1 sensitivity in prostate epithelial cells. Biol Cell. 2006;98(9):523–33.
Goumans M-J, Valdimarsdottir G, Itoh S, Rosendahl A, Sideras P, ten Dijke P. Balancing the activation state of the endothelium via two distinct TGF-β type I receptors. EMBO J. 2002;21(7):1743–53.
Padua D, Zhang XH-F, Wang Q, Nadal C, Gerald WL, Gomis RR, et al. TGFβ primes breast tumors for lung metastasis seeding through angiopoietin-like 4. Cell. 2008;133(1):66–77.
Strong N, Millena AC, Walker L, Chaudhary J, Khan SA. Inhibitor of differentiation 1 (Id1) and Id3 proteins play different roles in TGFβ effects on cell proliferation and migration in prostate cancer cells. Prostate. 2012;73(6):624–33.
Huber MA, Kraut N, Beug H. Molecular requirements for epithelial–mesenchymal transition during tumor progression. Curr Opin Cell Biol. 2005;17(5):548–58.
Gupta GP, Massague J. Cancer metastasis: building a framework. Cell. 2006;127(4):679–95.
Gomis RR, Alarcón C, Nadal C, Van Poznak C, Massagué J. C/EBPβ at the core of the TGFβ cytostatic response and its evasion in metastatic breast cancer cells. Cancer Cell. 2006;10(3):203–14.
Ouyang XS, Wang X, Lee DT, Tsao SW, Wong YC. Over expression of ID-1 in prostate cancer. J Urol. 2002;167(6):2598–602.
Tsai JF, Jeng JE, Chuang LY, Yang ML, Ho MS, Chang WY, et al. Elevated urinary transforming growth factor-beta1 level as a tumour marker and predictor of poor survival in cirrhotic hepatocellular carcinoma. Br J Cancer. 1997;76(2):244–50.
Krasagakis K, Tholke D, Farthmann B, Eberle J, Mansmann U, Orfanos CE. Elevated plasma levels of transforming growth factor (TGF)-beta1 and TGF-beta2 in patients with disseminated malignant melanoma. Br J Cancer. 1998;77(9):1492–4.
Maehara Y, Kakeji Y, Kabashima A, Emi Y, Watanabe A, Akazawa K, et al. Role of transforming growth factor-beta 1 in invasion and metastasis in gastric carcinoma. J Clin Oncol. 1999;17(2):607–14.
Gorsch SM, Memoli VA, Stukel TA, Gold LI, Arrick BA. Immunohistochemical staining for transforming growth factor beta 1 associates with disease progression in human breast cancer. Cancer Res. 1992;52(24):6949–52.
Bacman D, Merkel S, Croner R, Papadopoulos T, Brueckl W, Dimmler A. TGF-beta receptor 2 downregulation in tumour-associated stroma worsens prognosis and high-grade tumours show more tumour-associated macrophages and lower TGF-beta1 expression in colon carcinoma: a retrospective study. BMC Cancer. 2007;7:156.
Meteoglu I, Meydan N, Erkus M. Id-1: regulator of EGFR and VEGF and potential target for colorectal cancer therapy. J Exp Clin Cancer Res. 2008;27:69.
Kim MS, Park TI, Lee YM, Jo YM, Kim S. Expression of Id-1 and VEGF in non-small cell lung cancer. Int J Clin Exp Pathol. 2013;6(10):2102–11.
Anido J, Saez-Borderias A, Gonzalez-Junca A, Rodon L, Folch G, Carmona MA, et al. TGF-beta receptor inhibitors target the CD44(high)/Id1(high) glioma-initiating cell population in human glioblastoma. Cancer Cell. 2010;18(6):655–68.
Ding Y, Wang G, Ling MT, Wong YC, Li X, Na Y, et al. Significance of Id-1 up-regulation and its association with EGFR in bladder cancer cell invasion. Int J Oncol. 2006;28(4):847–54.
Yang S, Guo LJ, Tang XF, Tan K, Gong RG, Li A, et al. The alteration of Id-1 and TSP-1 expression in mucoepidermoid carcinoma associated with its clinical features and prognosis. Int J Oral Maxillofac Surg. 2010;39(1):29–35.
Kang Y, Chen CR, Massague J. A self-enabling TGFbeta response coupled to stress signaling: Smad engages stress response factor ATF3 for Id1 repression in epithelial cells. Mol Cell. 2003;11(4):915–26.
Thiery JP. Epithelial-mesenchymal transitions in tumour progression. Nat Rev Cancer. 2002;2(6):442–54.
Xu J, Lamouille S, Derynck R. TGF-beta-induced epithelial to mesenchymal transition. Cell Res. 2009;19(2):156–72.
Zhang X, Ling MT, Wang Q, Lau CK, Leung SC, Lee TK, et al. Identification of a novel inhibitor of differentiation-1 (ID-1) binding partner, caveolin-1, and its role in epithelial-mesenchymal transition and resistance to apoptosis in prostate cancer cells. J Biol Chem. 2007;282(46):33284–94.
Li B, Tsao SW, Li YY, Wang X, Ling MT, Wong YC, et al. Id-1 promotes tumorigenicity and metastasis of human esophageal cancer cells through activation of PI3K/AKT signaling pathway. Int J Cancer. 2009;125(11):2576–85.
Stankic M, Pavlovic S, Chin Y, Brogi E, Padua D, Norton L, et al. TGF-beta-Id1 signaling opposes Twist1 and promotes metastatic colonization via a mesenchymal-to-epithelial transition. Cell Rep. 2013;5(5):1228–42.
Acknowledgments
This work was supported by grants from the National Science Foundation of China (No. 30871312) and the National Basic Research Program of China (973 program, No. 2011CB910700).
Conflict of interest
The authors have no conflict of interest to declare.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Huiying Ma, Ye Wei and Yongmei Leng have equally contributed to this article.
Rights and permissions
About this article
Cite this article
Ma, H., Wei, Y., Leng, Y. et al. TGF-β1-induced expression of Id-1 is associated with tumor progression in gastric cancer. Med Oncol 31, 19 (2014). https://doi.org/10.1007/s12032-014-0019-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-014-0019-3