Abstract
KRAS gene mutations have been identified as a predictive molecular marker to predict the sensitivity of tumors to anti-EGFR therapeutics. The variability of clinical response to anti-EGFR agents has highlighted the need to select the appropriate patients who can benefit from the treatment. We examined the prevalence of KRAS mutations in 1,323 colorectal cancer patients from different regions of India and its correlation with geographic distribution and clinicopathological characteristics. DNA was extracted from formalin-fixed, paraffin-embedded tissue samples and was amplified by nested polymerase chain reaction at KRAS exon 2 and subjected to nucleotide sequencing using ABI 3100 Genetic Analyzer. The frequency of KRAS mutations was found to be 20.5 % (271/1,323). There was significant association (p < 0.05) between KRAS mutations, age and the tumor differentiation. Statistical analysis revealed significantly higher prevalence of colorectal cancer with mutated KRAS gene in northern regions of the country. No significant association was observed between KRAS mutations and gender (p > 0.05). Our study indicates that KRAS mutations in Indian colorectal cancer patients occur at lower level compared to that of Western population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common malignancy in men and women with an incidence of 1,234,000 cases contributing 10 % of the total cancer burden [1]. The incidence rates of colon cancer vary in various geographic locations with highest rates estimated in Australia/New Zealand and Western Europe. Incidence rates are substantially higher in men (663,000 cases, 10 % of the total) than in women (570,000 cases, 9.4 % of total). India constitutes a low-risk region for colorectal cancer with 36,000 cases reported annually [1]. The reasons for lower incidence in India are unclear although it is likely to be due in part to less exposure to harmful risk factors such as red and processed meat and lower prevalence of obesity. Population-based time trend studies show a rising trend in incidence of CRC in India [2].
In CRC, the novel therapies that are currently used target the epidermal growth factor (EGF) signaling pathway. Cetuximab and panitumumab are epidermal growth factor receptor (EGFR) inhibiting monoclonal antibodies that have been shown helpful in the treatment of patients with CRC. Although a significant proportion of CRC patients have had good response rates and increased progression-free and overall survival, with the treatment, many patients have had a complete absence of response to the therapeutics [3].
v-ki-ras2 Kristen rat sarcoma viral oncogene homologue (KRAS) gene mutations have been identified as a predictive molecular marker to predict the sensitivity of tumors to anti-EGFR therapeutics. The variability of clinical response to anti-EGFR agents has highlighted the need to select the appropriate patients who can benefit from the treatment. Oncogenic mutations of KRAS are involved in 30–40 % of colorectal cancers [4]. Patients with tumors harboring KRAS mutations show a lower response rate and decreased progression-free and overall survival, compared with those patients with KRAS wild-type tumors [3].
Most of the studies that investigated the predictive value of KRAS mutations were performed in Western countries. Little is known about the frequency of this biomarker in Indian population. The studies on KRAS mutations in India have been reported on small sample sizes of 100 and 212 patients [5, 6]. The primary aim of our study was to determine the frequency of KRAS mutations in a large cohort, comprising 1323 patients from various regions of India, and to statistically analyze the relationship between KRAS mutations and clinicopathological characteristics.
Materials and methods
Patients
One thousand three hundred and twenty-three patient samples with histologically confirmed colorectal adenocarcinoma (901 men and 422 women) from northern (339), southern (430), eastern (109) and western (445) regions of India were analyzed at Molecular Medicine laboratory, Reliance Life Sciences Pvt. Ltd., Navi Mumbai. Formalin-fixed, paraffin-embedded (FFPE) specimens collected during the period October 2008 to November 2012 were included in the study. The project was approved by Scientific and Ethics committees of Reliance Life Sciences Pvt. Ltd. The age of the patients ranged from 21 to 90 years with the mean age of 54 years. A summary of demographic and clinicopathological data is listed in Table 1.
DNA isolation
Formalin-fixed, paraffin-embedded tissue blocks were cut at 4 μm thickness and stained with hematoxylin and eosin (HE) for histopathological examination. Subsequently for DNA extraction, 10-μm section of tumor tissue was used. DNA was extracted by using Purelink DNA extraction kit (Life Technologies, Carlsbad, California, USA) according to manufacturer’s protocol. Deparaffinization of section was performed using xylene and ethanol. Tumor tissue was dissolved in 200 μl digestion buffer and incubated with proteinase K overnight at 50 °C. Subsequently, DNA was extracted and DNA concentration was determined at 260 nm using the Nanodrop 26 ND-1000 spectrophotometer (Nanodrop Technologies Inc. Wilmington, NC, USA).
KRAS mutation analysis
For mutation analysis, exon 1 (codons 12 and 13) of the KRAS gene was amplified from isolated genomic DNA by nested PCR using four sets of primers. Table 2 shows the list of primers used in PCR amplification and sequencing.
In total, 25–50 ng of DNA was added to a volume of 2 mM deoxynucleotide triphosphates (Biochain), 10 pmol of each primer, 5U of DNA polymerase (Promega), 0.1 % BSA, 6 % dimethylsulfoxide, 25 mM MgCl2 and 5X polymerase chain reaction (PCR) buffer (Promega). The cycling condition was as follows: 95 °C for 30 s, 40 cycles of 94 °C for 30 s, 52 °C for 30 s, 72 °C for 30 s and final extension at 72 °C for 7 min. The PCR products were electrophoresed on 2 % agarose gels, visualized in Gel-Documentation system (Amersham Pharmacia Biotech, Uppsala, Sweden) and recorded.
The PCR product spanning codons 12 and 13 obtained after amplification was subjected to nucleotide sequencing. The sequencing reactions used 5 pmol of forward and reverse primers, 5 μl volume and Big Dye Terminator v.3.3 cycle sequencing kit® and analyzed after sequencing using ABI 3100 Genetic Analyzer (Applied Biosystems, CA, USA).
Statistical analysis
The chi-square test using GraphPad Software was performed to examine statistical differences between mutation distribution based on age, gender and tumor differentiation. It was also used to compare the mutation frequency found in other studies to that in our present study. p < 0.05 was considered significant.
Results
KRAS amplification
KRAS was amplified using nested PCR and was detected in the presence of 189-base pair specific fragment on agarose gel electrophoresis in 1323 clinical samples. A representative gel image of amplified PCR product of KRAS is shown in Fig. 1.
KRAS mutation frequency
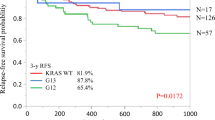
KRAS mutational status was tested in 1,323 clinical samples, of which 271 (20.5 %) harbored at least one mutation at codon 12 or 13. The spectrum of mutations is summarized in Table 3. Mutations at codon 12 are more frequent followed by codon 13. About 210 tissue samples had a mutation at codon 12 (15.9 %) and 61 at codon 13 (4.6 %) (Table 3). The incidence of KRAS mutations was almost similar in men (20.3 %) and women (20.8 %) (Table 4). The predominant mutations are G > A transitions and G > T transversions. The most frequent mutation was found to be G12D (36.2 %) of all mutations. Representative electropherograms of G12D, G12V, G12C, G12A and G13D are shown in Fig. 2. Also, one patient with colorectal carcinoma harbored the rare amino acid substitution G13V in KRAS codon 13 as shown in Fig. 3.
Statistical analysis of the various clinicopathological variables revealed a significant association (p < 0.05) between KRAS mutations, the age and the tumor differentiation. No significant association was observed between KRAS mutations and gender (p > 0.05) (Table 4).
Statistical analysis revealed significantly higher prevalence of colorectal cancer with mutated KRAS gene in northern regions of the country.
Discussion
The epidermal growth factor receptor (EGFR) plays a key role in the development and progression of CRC. It triggers a downstream signaling cascade such as RAS-RAF-MAPK and PI3K-AKT pathway, which are involved in cell proliferation differentiation, survival and invasion. Among the activating mutations downstream of EGFR, the KRAS gene mutations have been identified as the predictive biomarker for resistance to anti-EGFR antibody therapy and occur early in progression from adenoma to carcinoma [7].
In this study, we examined the incidence of KRAS mutation in 1323 Indian CRC patients and also tried to correlate the mutations with some clinical and pathological features. Previous studies have estimated the KRAS gene mutation frequency in CRC and have investigated the relationship between the mutations and various clinicopathological characteristics. To our knowledge, the present report is the first to provide data on frequency and type of KRAS mutations and the geographical distribution of colorectal cancer from a large Indian population of 1323 CRC patients.
In studies from Western population, the occurrence of KRAS mutations accounts for approximately 30–40 % of nonresponsive patients [8–11]. In this study, KRAS mutations were identified in 20.5 % of all CRCs, which is significantly lower than the usually detected frequencies in Western population.
Nearly 97 % of all KRAS mutations are localized to codon 12 or 13. Point mutations in codon 12 are most common KRAS mutations in CRC [7, 12–14]. In this study also KRAS codon 12 mutation was most frequent (15.8 %) followed by KRAS codon 13 (4.5 %).
The most frequent change is the transition of GGT to GAT in codon 12. The presence of a glycine residue in codon 12 appears to be critical for normal function of ras proteins [8]. Thus, single-base substitutions that result in the replacement of the glycine amino acid in this location result in formation of GTPase that are locked in the activating position.
In the previous studies from Western population, G12D transition is most frequently found in KRAS codon 12 followed by G12V, G12C, G12S and G12A [15, 16]. In this study we found G12D as the most frequent, which is in concordance with the earlier studies, followed by G12V, G12C, G12A and G12S. Similarly, in case of KRAS codon 13 mutations in Western population, G13D is the most frequent followed by G13C and G13R, which was the same as observed in our study where G13D is followed by G13R and G13C. We also observed a rare mutation G13V in codon 13 of KRAS.
We also investigated the clinicopathological characteristics of CRC patients with respect to KRAS mutations. We found significant association (p < 0.05) between KRAS mutations, the age and the tumor differentiation. KRAS mutation rate was significantly higher in poorly and moderately differentiated adenocarcinomas (p < 0.05). Also, the mutation rate in patients with age ≥50 years was higher than in patients with <50 years (p < 0.05) (Table 4). However, we did not find any statistically significant associations between gender and KRAS mutations. We also found statistically significant association (p < 0.05) between the frequency of KRAS mutations and the prevalence of colorectal cancer in northern parts of India compared with other regions of the country. In other reported studies using direct sequencing as the methodology and from different population background, the KRAS mutation frequency varied from 14 to 40.4 %. In our study, KRAS mutations were observed in 20.5 % of all CRCs, which is similar to the frequency reported in few studies [5, 7, 17, 18]. However, in some reports [13, 19–22] the KRAS mutation frequency was significantly different from the present study (Table 5). These variations in patterns of KRAS mutations may be due to the racial differences and etiological factors.
In summary, our study adds to the evidence that KRAS mutations in Indian CRC patients occur at lower level compared to that of Western population. However, further studies are necessary to examine the molecular background of CRC.
References
Ferlay J, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2010;127(12):2893–917.
Yeole BB, et al. Population-based survival from colorectal cancer in Mumbai, (Bombay) India. Eur J Cancer. 2001;37(11):1402–8.
Velho S. et al. BRAF, KRAS and PIK3CA mutations in colorectal serrated polyps and cancer: primary or secondary genetic events in colorectal carcinogenesis? Bmc Cancer. 2008;8.
Karapetis CS, et al. K-ras mutations and benefit from cetuximab in advanced colorectal cancer. N Engl J Med. 2008;359(17):1757–65.
Bagadi SB, et al. Combined mutational analysis of KRAS, NRAS and BRAF genes in Indian patients with colorectal carcinoma. Int J Biol Markers. 2012;27(1):27–33.
Javid G, et al. Incidence of colorectal cancer in Kashmir valley, India. Indian J Gastroenterol. 2011;30(1):7–11.
Servomaa K, Kiuru A, Kosma VM, Hirvikoski P, Rytömaa T. p53 and K-ras gene mutations in carcinoma of the rectum among Finnish women. J Clin Pathol Mol Pathol. 2000;53:24–30.
Arrington AK, et al. Prognostic and predictive roles of KRAS mutation in colorectal cancer. Int J Mol Sci. 2012;13(10):12153–68.
Valtorta E, et al. KRAS gene amplification in colorectal cancer and impact on response to EGFR-targeted therapy. International Journal of Cancer. 2013. doi:10.1002/ijc.28106.
Ozen F, et al. The proto-oncogene KRAS and BRAF profiles and some clinical characteristics in colorectal cancer in the Turkish population. Genet Test Mol Biomarkers. 2013;17(2):135–9.
Mao C, et al. KRAS, BRAF and PIK3CA mutations and the loss of PTEN expression in Chinese patients with colorectal cancer. Plos One. 2012; 7(5).
Lambrechts D, De Roock W, Prenen H, De Schutter J, Jacobs B, Biesmans B, Claes B, De Hertogh G, Van Cutsem E, Tejpar S KULeuven, Leuven, Belgium; University Hospital Gasthuisberg, KULeuven, Leuven, Belgium, The role of KRAS, BRAF, NRAS, and PIK3CA mutations as markers of resistance to cetuximab in chemorefractory metastatic colorectal cancer. Journal of Clinical Oncology. 2009;27(15 s).
Fransen K, et al. Mutation analysis of the BRAF, ARAF and RAF-1 genes in human colorectal adenocarcinomas. Carcinogenesis. 2004;25(4):527–33.
Conlin A, et al. The prognostic significance of K-ras, p53, and APC mutations in colorectal carcinoma. Gut. 2005;54(9):1283–6.
Vaughn CP, et al. Frequency of KRAS, BRAF, and NRAS mutations in colorectal cancer. Genes Chromosom Cancer. 2011;50(5):307–12.
Neumann J, et al. Frequency and type of KRAS mutations in routine diagnostic analysis of metastatic colorectal cancer. Pathol Res Pract. 2009;205(12):858–62.
Velho S, Oliveira C, Seruca R. KRAS mutations and anti-epidermal growth factor receptor therapy in colorectal cancer with lymph node metastases. J Clin Oncol. 2009;27(1):158–9.
Sameer AS, et al. Molecular gate keepers succumb to gene aberrations in colorectal cancer in Kashmiri population, revealing a high incidence area. Saudi J Gastroenterol. 2009;15(4):244–52.
Farina-Sarasqueta A, et al. The BRAF V600E mutation is an independent prognostic factor for survival in stage II and stage III colon cancer patients. Ann Oncol. 2010;21(12):2396–402.
Gao J, et al. Wild-type KRAS and BRAF could predict response to cetuximab in Chinese colorectal cancer patients. Chin J Cancer Res. 2011;23(4):271–5.
Zhu XL, et al. KRAS and BRAF gene mutations in correlation with clinicopathologic features of colorectal carcinoma in Chinese. Zhonghua Bing Li Xue Za Zhi. 2012;41(9):584–9.
Rosty C, Young J, Walsh MD, Clendenning M, Walters RJ, Pearson S, Pavluk E, Nagler B, Pakenas D, Jass JR, Jenkins MA, Win AK, Southey MC, Parry S, Hopper JL, Giles GG, Williamson E, English DR, Buchanan DD Colorectal carcinomas with KRAS mutation are associated with distinctive morphological and molecular features. Modern Pathology. 2013.
Acknowledgments
The authors gratefully acknowledge Reliance Life Sciences Pvt. Ltd., Mumbai, for financial support of the project. The authors also acknowledge Dr. Nitin Palwe for his help on statistical analysis of the data.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Patil, H., Korde, R. & Kapat, A. KRAS gene mutations in correlation with clinicopathological features of colorectal carcinomas in Indian patient cohort. Med Oncol 30, 617 (2013). https://doi.org/10.1007/s12032-013-0617-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-013-0617-5