Abstract
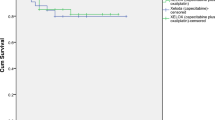
Neo-adjuvant chemo-radiotherapy (CT–RT) has been shown to decrease local recurrence rate in locally advanced rectal cancer. This multicenter phase II trial was conducted to evaluate the feasibility, safety and effectiveness of a combination of pre-operative radiotherapy and concurrent Capecitabine plus Oxaliplatin (XELOXART Trial). From October 2008 to May 2011, fifty consecutive patients affected with T3/T4 and/or N+ rectal cancer were enrolled. Treatment protocol consisted of 50.4 Gy in 28 fractions, Oxaliplatin 60 mg/m2 once a week for 6 weeks and oral Capecitabine 825 mg/m2 twice daily from day 1 to 14 and from day 22 to 35. Surgery was planned 6–8 weeks after. Main endpoints were pathological complete response rate (pCR) and the type of surgery performed compared to the planned one at diagnosis. 50 patients were included; pCR (ypT0N0M0) was achieved in 6 patients (12 %). Tumour downstaging was observed in 27 patients (54 %), and nodal downstaging in 32 patients (64 %). A total of 32 patients had lower rectal cancer, with 24 candidate for abdominal-perineal resection. At the end of CT–RT, a total of 12/24 (50 %) underwent conservative surgery. Grade 3 toxicity (fatigue and diarrhoea) occurred in 4 % of patients; grade 4 sensory neuropathy occurred in 2 % of patients. Perioperative complications of any grade occurred in 10 % of patients. Pre-operative CT–RT with Capecitabine-Oxaliplatin was well tolerated and resulted in an encouraging sphincter preservation and tumour downstaging rate. No improvements in terms of pathological complete response rate were shown.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Combined modality treatment with total mesorectal excision (TME), radiotherapy (RT) and chemotherapy (CT) achieved a substantial improvement in outcome for locally advanced rectal cancer patients [1]. In recent years, two phase III randomised clinical trials, namely the European Organisation for Research and Treatment (EORTC) 22921 and the Fédération Francophone de Cancérologie Digestive (FFCD) 9293, reached satisfactory evidence that the addition of 5-Fluorouracil (5-FU)-based chemotherapy to pre-operative pelvic radiation therapy might prolong local control and increase pathological complete response (pCR) rate [2, 3]. However, a significant benefit for the primary endpoint of these studies, Overall Survival (OS), could not be demonstrated [4]. Nevertheless, the German phase III randomised study (CAO/ARO/AIO-94-Study) demonstrated increased local control and decreased acute and late toxicity of pre-operative 5-FU-based chemoradiation (CT–RT) if compared to standard post-operative CT–RT [5], and infused 5-FU or oral fluoropyrimidines are currently the conventional agents to be combined with radiation in the neoadjuvant setting [6]. This approach leads to a consistent local control rate in this subset of patients, with local relapses being reduced to 5–10 % [3]. However, distant spread still occurs in almost 1/3 of the cases, due to ineffective micrometastatic disease control [7], and several additional agents have been tested in phase II–III studies in order to improve clinical results [8]. Oxaliplatin has been variously combined either with 5-FU or with Capecitabine concomitantly with radiation therapy in the neoadjuvant setting [9–12], with the aim of improving complete response rates (pathological complete responses, pCR) and allowing for less aggressive surgical interventions.
The present phase II prospective trial was designed to investigate safety and clinical activity of a schedule of weekly intravenous Oxaliplatin, oral Capecitabine and radiotherapy; primary endpoints were pathological complete response (pCR), tumour downstaging and sphincter-saving procedure rates.
Materials and methods
Eligibility criteria
The institutional review board approved the study, and all included patients signed a written informed consent. All enrolled patients had histologically confirmed rectal adenocarcinoma localised within 12 cm from the anal verge, clinically staged as ‘locally advanced’ disease with or without perirectal lymph nodes involvement (T3–4/N0 or T1–4/N1–2), without evidence of any distant spread. Other inclusion criteria included an Eastern Cooperative Oncology Group (ECOG) performance status of 0–1, age 18–75, neutrophils ≥1.5 × 109/l and platelets ≥100 × 109/l, adequate renal function (creatinine clearance >50 ml/min) and liver function (serum bilirubin ≤1.5 of the upper limit of normal range, liver transaminase or alkaline phosphatase concentrations ≤2.5 of the upper limit of normal range). Exclusion criteria were as follows: systemic disease at diagnosis, prior radiation to the pelvic region, a medical history of other synchronous or metachronous tumours (except for non-melanomatous skin cancer, non-muscle-invasive bladder cancer and cervical carcinoma), medical contraindications to chemo-radiation and abdominal surgery, symptoms of bowel occlusion and/or gastrointestinal bleeding, malabsorption syndrome, peripheral neuropathy, psychiatric disease hampering compliance to the administration of oral chemotherapy, pregnancy and breast-feeding. All patients provided written informed consent before treatment; adjunctively, the present study was approved by the Ethical Review Board of our Institution Hospital and conducted in accordance with the Declaration of Helsinki.
Pre-treatment evaluation
All patients were evaluated prior to accrual by the gastrointestinal multidisciplinary team of our Institutional Hospital (medical oncologist, radiation oncologist and abdominal surgeon). The clinical evaluation comprised a complete medical history with physical examination, including digital rectal examination and complete laboratory tests (complete blood count, electrolytes, renal and liver function and carcinoembryonic antigen). Staging included a chest and abdominal computed tomography scan (CT), a magnetic resonance imaging (MRI) of the pelvic region and an endoscopic transrectal ultrasounds (EUSs).
Radiotherapy
RT was delivered with a linear accelerator (LINAC) using a Megavoltage source of 10–18 MV through a 3D conformal field arrangement (3DCRT), developed over a 4-field box technique. Patients were located in supine position with both an indexed shaped knee rest and ankle support (CIVCO Medical Solutions, Kalona, IO, USA) in order to prevent from hip rotation. For planning purposes, a CT scan was performed and 3-mm-slice-thick axial images were obtained from the top of the L4 vertebral body to the bottom of the lower trochanters. An isocentre was found using the CT-simulation software Oncentra Masterplan v. 3.0 (Nucletron, Veendhal, The Netherlands) within the pelvic region, and it was subsequently marked on the patient’s skin under laser guidance. In order to avoid imaging artefacts during the contouring phase, we decided not to opacify the rectum with barium enema. The clinical target volume (CTV) encompassed the macroscopical primary tumour site, the entire mesorectal region and internal iliac and pre-sacral lymph nodes up to the level of the fifth lumbar vertebra. The anal sphincter complex was included for low-lying tumours (<5 cm from the anal verge). The planning target volume (PTV) was then generated by the addition of a 5-mm isotropic margin to the CTV. All patients received 45 Gy to the pelvic region followed by a boost dose of 5.4 Gy to the primary tumour with a 3-cm cranio-caudal margin, for a total nominal dose of 50.4 Gy in 1.8 Gy daily fraction over 5.5 weeks.
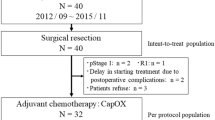
Chemotherapy
Chemotherapy consisted of Oxaliplatin (Eloxatin®; Sanofi-Aventis, Bridgewater, NJ, USA) 60 mg/m2 of body surface area administered intravenously over 2 h on days 1, 8, 15, 22, 29 and Capecitabine (Xeloda®, Hoffmann-La Roche Ltd, Basel, Switzerland) 825 mg/m2 of body surface area given twice a day on days 1–14 and 22–35. Blood counts were routinely evaluated before every CT administration; prophylactic antiemetic therapy consisted of granisetron 3 mg and dexametasone 8 mg intravenously. Treatment interruptions were planned if grade 3–4 toxicity was recorded, according to the National Cancer Institute Common Terminology Criteria for Adverse Events (NCI CTC version 3.0), while continuation at reduced dose could be performed in case of symptoms resolution or toxicity profile reduction down to grade 1. Patients were taken off the study in case of persistence of toxicity ≥ G2 over 2 weeks or in case of repeated episodes of toxicity ≥G2 occurring despite dose reduction. Adjuvant chemotherapy with 5-FU/leucovorin and Oxaliplatin (FOLFOX 4) was planned for high-risk patients (high tumour grading, young age, bowel occlusion, perforation or bleeding, perineural and vascular invasion, mucinous component), while low-risk patients underwent different adjuvant chemotherapy regimens according to objective response to pre-operatory CT–RT, specifically 5-FU/LV (Mayo Clinic schedule) if in pCR after neoadjuvant treatment or FOLFOX4 if less than pCR could be detected.
Imaging response evaluation
Four weeks after the completion of CT–RT, all patients underwent a complete restaging procedure with abdomino-pelvic CT and pelvic MRI. Objective response evaluation was assessed according to the Response Evaluation Criteria in Solid Tumours (RECIST) Criteria, whenever possible [13–16].
Surgery
Surgery was performed within 6 weeks after the completion of neoadjuvant CT–RT. At the time of diagnosis, the surgeon was asked to indicate, based on radiological findings and digital rectal examination, the type of surgical procedure deemed necessary for the specific patient. At the end of the combined pre-operative CT–RT, the same surgeon conducted a decisional re-assessment in order to choose between anterior resection of the rectum and abdominal-perineal resection based on the site of tumour presentation and the volume of residual disease. Surgery should have satisfied the following characteristics: (a) proximal, distal and radial margins of resection unaffected by tumour; (b) distance between the lower border of the tumour and resection margin ≥1 cm; (c) binding of the inferior mesenteric artery at the origin; (d) mandatory TME.
All patients underwent open surgery.
Pathology, study endpoints and statistics
The primary endpoint was pathological complete response rate (pCR). Secondary endpoints were objective responses (downstaging/downsizing), sphincter-sparing resection rate (locally advanced disease cancer and/or lower rectal tumours) and microscopic complete resections (R0) rate. The pCR rate after surgery was prospectively defined as grade 3+ or 4 according to the grading system proposed by Ruo et al. [17], with >96 % of pathological response. All lymph nodes within each surgical specimen were analysed and categorised as pN0 or pN+. The pCR rate was presented with 95 % confidence intervals (CIs) using the Pearson-Clopper method. As secondary endpoints we considered the rate of sphincter preservation, R0 resection in patients with T3–T4 tumours, downstaging rate (defined as a decrease in T and/or N value) and safety.
This study was designed as a single-stage phase II trial according to the method of Fleming; pCR rate was considered as the primary endpoint of effectiveness; a pCR rate of 25 % was considered to fulfil the criteria for a promising clinical activity of the combined modality approach. With a total of 43 evaluable patients (and a response rate of at least 25 %), a power of 80 % and a type-I error of 5 % were achieved. The planned sample size was increased to 50 patients to allow for dropouts.
Results
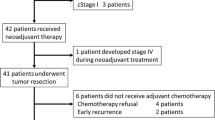
The study started in October 2008, and the last patient was enroled in May 2011. Fifty patients were accrued. Since 1 patient was not evaluable by transrectal ultrasounds owing to rectal stenosis, a T3N1 stage was decided based on MRI findings. Patients’ characteristics are summarised in Table 1. Mean age at diagnosis was 60 (range 36–77); 35 patients (70 %) were male, while 15 (30 %) were female; all patients showed an Eastern Cooperative Oncology Group (ECOG) performance status 0–1 at the time of treatment. Most of patients had T3N+ disease (42/50; 84 %). Mean Carcino-Embryonic antigen (CEA) dosage was 14.8 ng/ml (range 0.8–237 ng/ml). The majority (92 %) of clinical presentations were within the lower (64 %) and mid (28 %)-rectum. The distance between the macroscopic tumour and the anal verge was ≤6 cm in 32 patients (64 %), between 6 and 10 cm in 14 patients (28 %) and >10 cm in 4 patients (8 %).
The whole CT–RT schedule was completed in all but 2 patients; one of them developed severe diarrhoea and enteritis, with discontinuation of RT–CT during the second treatment week (9 delivered fractions of radiation); the other one could just reach given dose of 45 Gy because of severe neurotoxicity. Twenty-one/50 patients completed the planned RT program with no interruptions; conversely, 28/50 patients experienced unplanned treatment gaps of meanly 1.8 days (range 1–6 days). Moreover, chemotherapy dose modifications occurred in 3 patients (6 %). All patients were evaluated for toxicity profile, but only toxicities ≥G2 were reported. The most serious toxic event occurred during the study was G4 sensory neuropathy (Guillain-Barrè syndrome).
No significant haematologic toxicities were noted (only 1 patient with G2 thrombocytopenia); 12 patients (24 %) experienced Grade 2 diarrhoea, while 4 of them (8 %) had Grade 3. One G3 proctitis was reported, and a G2 Capecitabine-induced palmar plantar erythro-dysesthesia (Hand–Foot Syndrome) occurred in 1 patient. Two patients, respectively, experienced G2 and G3 asthenia. A detailed toxicity profile is shown in Table 2.
Radical macroscopic and microscopic resection (R0) was achieved in 45/50 patients (90 %). Specifically, 4 out of 5 R1 resections (at circumferential margin) were observed in patients submitted to anterior resection and 1 in patients who underwent abdominal-perineal resection. Proximal and caudal margins were negative in all patients.
After nodal dissection, 8 lymph nodes on average (range: 0–27) were retrieved in the pathological specimen. In 38 out of 50 patients (76 %), a sphincter preservation resection was planned before CT–RT and was confirmed at reassessment after CT–RT. Twenty-four out of 32 patients with low-lying tumours were candidate at diagnosis for abdominal-perineal resection with permanent colostomy, and in this group, the sphincter preservation rate after CT–RT was 50 % (12/24).
Sphincter function was subjectively judged acceptable by each of the analysed patients. Few post-surgical-related morbidities were noticed: 3 anastomotic fistulae (2 entero-vaginalis fistula and 1 entero-cutaneous fistula), 1 gluteal abscess, 1 jejunal perforation.
A pathologic complete response (pCR—ypT0N0) was achieved in 6 patients (12 %); two patients achieved ypT0N1 disease.
Disease downstaging was observed in 27 out of 50 patients (54 %), while nodal downstaging was observed in 32 out of 50 patients (64 %). Disease progression was observed in 3 patients (2 with tumour upstaging and 1 with nodal upstaging). A detailed overview of overall responses is shown in Table 3.
Discussion
In locally advanced rectal cancer, main therapeutic goals of radiochemotherapy are to achieve high local control rates, to reduce distant failure rate and improve sphincter preservation. Data from the Polish randomised study evaluating pre-operative CT–RT versus exclusive RT demonstrated a high rate of downstaging for the association arm [18]. The EORTC 22921 trial had a 2 × 2 factorial design and randomised pre-operative radiotherapy (45 Gy) versus pre-operative CT–RT (45 Gy combined with 5-FU/Leucovorin). Results demonstrated an increased LC rate for the CT–RT arm, namely 91 versus 83 % [2]. Similar results were found in the French FFCD 9203 study, with a local recurrences rate of 16.5 and 8 %, respectively, for the radiation alone and the association arm [3]. Oral Capecitabine allows to mimic 5-FU continuous infusion, and the association of agents such as Oxaliplatin and irinotecan with fluoropyrimidines, based on several data obtained in metastatic colorectal cancer, has been transferred in the neoadjuvant setting of rectal cancer [19, 20]. Capecitabine combined to Oxaliplatin with radiotherapy have been assessed in several studies in different regimens including Capecitabine in days 1–14 and 22–35, and Oxaliplatin in days 1, 8, 22, 29 [21–24]; continuous Capecitabine 7 days/week and Oxaliplatin in days 1 and 29 [25] and again continuous Capecitabine 5 days/week and weekly Oxaliplatin [26, 27].
The present study failed to show any advantage in terms of increased pCR rate with the combination of Oxaliplatin and Capecitabine plus RT when compared to other series. The 12 % pCR rate is slightly inferior to that of other studies [22, 25], and this might be due to the presence of 2 ypT0N1 patients showing micrometastases in regional lymph nodes, decreasing the total rate of pCR. Conversely, a substantial percentage of patients presented tumour and nodal downstaging (54 and 64 %, respectively). This finding is markedly important since lymph nodes involvement at the end of neoadjuvant CT–RT is a strong predictor for survival [21]. Up to 90 % of patients achieved a R0 resection at the circumferential margin (a possible surrogate endpoint for tumour response); this is consistent with a high quality of surgical procedures and a strong efficacy of the pre-operative approach, even if most part of the patients were affected with T3 cancers; this data compares favourably with the 92 % R0 resection rate of the ACCORD 12/0405-Prodige 2 study [12]. Sphincter-saving procedures were performed in 76 % of the patients: this is a widely positive finding since 64 % of the patients presented with low-lying tumours (<6 cm from the anal verge), even superior than other reported studies [24]. These results duplicate the finding of Rodel et al. with a sphincter preservation rate of 50 % for lower rectal tumours candidate to Miles resection [22]. The most common non-haematological toxicity in our study was grade 3 diarrhoea, occurring in 8 % of the patients. Other major toxicities could be considered anecdotal. Oxaliplatin has been tested within the contest of phase III randomised trial in the ACCORD 12/0405-Prodige 2 French study and in the NSABP R-04 trial (with Capecitabine and RT), in the STAR-01 Italian trial and in the German CAO/ARO/AIO-04 trial (with 5-FU and RT) [12, 28–30]. Both the French and Italian trials, together with the US preliminary data, failed to demonstrate a statistically significant benefit in pathological response rate by the addition of Oxaliplatin in the experimental arm (with an increase in grade 3–4 toxicity rate). However, the study by Gerard et al. showed a substantial (even if non-significant) trend to an improved pathological response rate with Oxaliplatin. Since the experimental arm of the French trial used Oxaliplatin combined with dose-escalated radiation therapy (50 Gy), it is impossible to determine which agent could be considered responsible for the outcome improvement. Nevertheless, a recent update of the French Phase III Trial, with median follow-up time of 3 years, showed no benefits in terms of clinical outcome (LC, DFS and OS) with the adjunct of Oxaliplatin to combined RT–CT [31]. Only the German trial found out a statistically significant advantage in terms of pCR rate, with the adjunct of weekly Oxaliplatin (17 vs. 13 % of pCR rate). This finding might be due to the 5-FU schedule employed in the control group, which may be considered as suboptimal (since a chemotherapy gap was planned in the third week of RT), allowing for the contribution of Oxaliplatin in the determination of the outcome difference between the 2 arms [30]. The other indicators of local treatment efficacy (R0 resections rate, circumferential margins <1 mm, lymph node negativity) did not differ alongside treatment modality [30]. Thus, these results should be interpreted with caution.
In conclusion, our study demonstrates that the combination of RT + Capecitabine and Oxaliplatin in patients affected with locally advanced rectal cancer is feasible and safe in terms of toxicity and results in a consistent rate of R0 resection, sphincter-saving procedure and downstaging, without any improvement in the pCR rate. On the basis of our results and those of previous studies, cumulative clinical evidence is lacking on the benefit of adding Oxaliplatin to standard CT–RT. Several reasons behind this negative finding could be discussed: one key issue is that we currently know that pCR cannot be considered an adequate endpoint for clinical outcomes [32], and the aforementioned Phase III trials were either designed with objective response as primary endpoint (underpowered to detect significant differences in classical survival endpoints such as local control, disease-free survival, overall survival such as the ACCORD12/0405-Prodige 2 trial [31]), or preliminary data are available on response rate, but not on primary endpoints (e.g. the Italian STAR trial [28]). Also RT dose/volumes issues as potential confounding factors should be taken into account in outcome evaluation [33]. As a consequence, even if Oxaliplatin is not currently advised in association with RT-Fluoropyrimidines in clinical practice, several ongoing phase III trials are testing the combination between RT/Capecitabine/Oxaliplatin and/or new drugs in the neoadjuvant setting. Most of these studies are designed with endpoints such as disease-free survival or time to local recurrence, that appear more appropriate (even at the price of longer time to be completed), and results will clarify the role of this drug in combination with RT in the forthcoming years.
References
Valentini V, Aristei C, Glimelius B, et al. Multidisciplinary rectal cancer management: 2nd European rectal cancer consensus conference (EURECA-CC2). Radiother Oncol. 2009;92:148–63.
Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, Daban A, Bardet E, Beny A, Ollier JC. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006;355:1114–23.
Gérard TC, Conroy T, Bonnetain F, Bouché O, Chapet O, Closon-Dejardin MT, Untereiner M, Leduc B, Francois E, Maurel J, Seitz JF, Buecher B, Mackiewicz R, Ducreux M, Bedenne L. Preoperative radiotherapy with or without concurrentand leucovorin in T3–4 rectal cancers: results of FFCD 9203. J Clin Oncol. 2006;24:4620–5.
Bonnetain F, Bosset JF, Gerard JP, et al. Eur J Cancer. 2012;48:1781–90.
Sauer R, Becker H, Hohenberger W, et al. Preoperative versus postoperative chemo-radiotherapy for rectal cancer. N Engl J Med. 2004;351:1731–40.
Minsky BD, Roedel C, Valentini V. Combined modality therapy for rectal cancer. Cancer J. 2010;16:253–61.
Valvo F, Mantello G, Coco G, et al. Rectal cancer multidisciplinary treatment: evidences, consensus and perspectives. Tumori. 2010;96:185–90.
Rodel C, Sauer R. Integration of novel agents into combined-modality treatment for rectal cancer patients. Strahlenther Onkol. 2007;183:227–35.
Gerard JP, Chapet O, Nemoz C, et al. Preoperative concurrent chemoradiotherapy in locally advanced rectal cancer with high-dose radiation and oxaliplatin-containing regimen: the Lyon R0–04 phase II trial. J Clin Oncol. 2003;21:1119–24.
Rodel C, Grabenbauer GG, Papadopoulos T, et al. PhaseI/II trial of capecitabine, oxaliplatin and radiation for rectal cancer. J Clin Oncol. 2003;21:3098–104.
Aschele C, Friso ML, Pucciarelli S, et al. A phase I-II study of weekly oxaliplatin, 5-forouracil continuos infusion and preoperative radiotherapy in locally advanced rectal cancer. Ann Oncol. 2005;16:1140–6.
Gerard JP, Azria D, Gourgou-Bourgade S, et al. Comparison of two neoadjuvant chemoradiotherapy regimens for locally advanced rectal cancer: results of the phase III Trial ACCORD 12/0405-Prodige 2. J Clin Oncol. 2010;28:1638–44.
Colorectal Cancer Collaborative Group. Adjuvant radiotherapy for rectal cancer: a sistematic overview of 8507 patients from 22 randomised trials. Lancet. 2001;358:1291–304.
Gastrointestinal Tumor Study Group. Adjuvant therapy of colon cancer: results of a prospectively randomized trial. N Engl J Med. 1984;310:737–43.
Krook JE, Moertel CG, Gunderson LL, et al. Effective surgical adjuvant therapy for high-risk rectal carcinoma. N Engl J Med. 1991;324:709–15.
O’Connell MJ, Martenson JA, Wieand HS, et al. Improving adjuvant therapy for rectal cancer by combining protracted-infusion fluorouracil with radiation therapy after curative surgery. N Engl J Med. 1995;331:502–7.
Ruo L, Tickoo S, Klimstra DS, et al. Long-term prognostic significance of extent of rectal response to preoperative radiation and chemotherapy. Ann Surg. 2002;236:75–81.
Bujko K, Nowacki MP, Nasierosska-Guttmejer A, et al. Sphincter preservation following preoperative radiotherapy for rectal cancer: report of a randomised trial comparing short-term radiotherapy vs. conventionally fractionated radiochemotherapy. Radiother Oncol. 2004;72:15–24.
Van Cutsem E, Hoff PM, Harper P, et al. Oral capecitabine vs intravenous 5-fluorouracil and leucovorin: integrated efficacy data and novel analyses from two large, randomized, phase III trials. Br J Cancer. 2004;90:1190–7.
Twelves C, Wong A, Nowacki MP, et al. Capecitabine as adjuvant treatment for stage III colon cancer. N Engl J Med. 2005;352:2696–704.
Koeberle D, Burkhard R, von Moos R, et al. Phase II study of capecitabine and oxaliplatin given prior to and concurrently with preoperative pelvic radiotherapy in patients with locally advanced rectal cancer. Br J Cancer. 2008;98:1204–9.
Roedel C, Liersch T, Hermann RM, et al. Multicenter phase II trial of chemoradiation with oxaliplatin for rectal cancer. J Clin Oncol. 2007;25:110–7.
Roedel C, Martus P, Papadoupolos T, et al. Prognostic significance of tumor regression after preoperative chemoradiotherapy for rectal cancer. J Clin Oncol. 2005;23:8688–96.
Glynne-Jones R, Sebag-Montefiore D, McDonald A, et al. A phase I dose escalation study of continuous oral capecitabine in combination with oxaliplatin and pelvic radiation (XELOX-RT) in patients with locally advanced rectal cancer. Ann Oncol. 2006;17:50–6.
Machiels JP, Duck L, Honhon B, et al. Phase II study of preoperative oxaliplatin, capecitabine and external beam radiotherapy in patients with rectal cancer: the RadiOxCape study. Ann Oncol. 2005;16:1898–905.
Rutten H, Sebag-Montefiore D, Glynne-Jones R, et al. Capecitabine, oxaliplatin, radiotherapy, and excision (CORE) in patients with MRI-defined locally advanced rectal adenocarcinoma: results of an international multicenter phase II study. J Clin Oncol. 2006;24(18S):(abstract 3528).
Glynne-Jones R, Dunst J, Sebag-Montefiore D. The integration of oral capecitabine into chemoradiation regimens for locally advanced rectal cancer: how successful have we been? Ann Oncol. 2006;17:361–71.
Aschele CP, Cionini L, Lonardi S, et al. Primary tumor response to preoperative chemoradiation with or without oxaliplatin in locally advanced rectal cancer: pathologic results of the STAR-01 randomized trial. J Clin Oncol. 2011;29:2773–80.
Roh MS, Yothers GA, O’ Connell MJ, et al. The impact of capecitabine and oxaliplatin in the preoperative multimodality treatment in patients with carcinoma of the rectum: NSABP R-04. Proc Am Soc Clin Oncol. 2011;29(suppl):abstract 3503.
Rodel C, Liersch T, Becker H, et al. Preoperative chemoradiation and postoperative chemotherapy with fluorouracil and oxaliplatin versus fluoracil alone in locally advanced rectal cancer: initial results of the German CAO/ARO/AIO-04 randomised phase 3 trial. Lancet Oncol. 2012;13:679–87.
Gerard JP, Azria D, Gourgou-Bourgade S, et al. Clinical outcome of the ACCORD 12/0405 PRODIGE 2 randomized trial in rectal cancer. J Clin Oncol. 2012;30:4558–65.
Methy N, Bedenne L, Conroy T, et al. Surrogate endpoints for overall survival and local control in neo-adjuvant rectal cancer trials: statistical evaluation based on the FFCD 9203 trial. Ann Oncol. 2010;21:518–24.
Tepper JE, Wang AZ. Improving local control in rectal cancer: radiation sensitizers or radiation dose? J Clin Oncol. 2010;28:1623–4.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ricardi, U., Racca, P., Franco, P. et al. Prospective phase II trial of neoadjuvant chemo-radiotherapy with Oxaliplatin and Capecitabine in locally advanced rectal cancer (XELOXART). Med Oncol 30, 581 (2013). https://doi.org/10.1007/s12032-013-0581-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-013-0581-0