Abstract
The aim of this study was to investigate the clinical significances of the mRNA expression of survivin gene and its four splice variants in the pathogenesis of colorectal cancer (CRC). CRC samples, matched adjacent tissues, and normal tissues were collected from surgical resections of 39 patients with histologically confirmed diagnosis. The mRNA expression of survivin and its four splice variants, that is, survivin-△Ex3, survivin-2B, survivin-3B, and survivin-2α, was detected using semiquantitative PCR and RT-PCR. Carcinoembryonic antigen (CEA) CAM5 was determined as control. The mRNA expression rates of survivin, survivin-△Ex3, survivin-2B, survivin-3B, surviving-2α, and CEA CAM5 in CRC samples were significantly higher than those in adjacent tissues (P < 0.01) and those in normal tissues (P < 0.01). The mRNA levels of the above variants in CRC samples were also significantly higher than those in adjacent tissues (P < 0.01) and those in normal tissues (P < 0.01). The mRNA levels of survivin, survivin-2B, and survivin-2α were not associated with any clinical variable of patients, while the levels of survivin-△Ex3 and survivin-3B were associated with lymphoid metastasis and Dukes grade (P < 0.05), and survivin-△Ex3 was associated with invasiveness. We concluded that mRNA expression rates and levels of survivin and its four splice variants elevated in CRC tissues, and expression levels of survivin-△Ex3 and survivin-3B were positively associated with tumor aggression.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common cancer worldwide and the second most common cause of cancer mortality [1]. Currently, surgical resection remains a curative option for CRC treatment. However, most patients with CRC are not candidate for surgical operations because of the advanced stage of the lesions when diagnosed. Chemotherapy is commonly used for patients who are not suitable for operation and those at risk for disease recurrence after operation. As the uncertainty of outcomes after surgery and chemotherapy, there is a need to look for biomarkers evaluating the severity of the disease, predicting the prognosis of patients, and targeting the pathogenic genes. Recently, the concept of molecular medicine has been introduced. A number of molecular markers are recommended, but the results remained inconclusive [2, 3]. Among those markers, survivin has been studied for decades. Survivin is involved in the regulation of cell division and survival, two key processes in cancer development. Its roles in carcinogenesis at the molecular level have been defined in the literature. The differential expression of survivin in CRC versus normal tissues makes it a promising biomarker in diagnosis and treatment [4–6]. The majority of studies have focused on wild-type survivin (or termed survivin), but less is known about the function of survivin splicing variants, that is, survivin-△Ex3, survivin-2B, survivin-3B, and survivin-2α in CRC [4, 5]. Studies about their clinical significances in CRC patients have not been fully documented. In the present study, we simultaneously investigated the mRNA expression of survivin and its four transcript variants in CRC, adjacent, and normal colorectal tissues from surgical resections in order to explore the clinical significances of them in the development of CRC.
Materials and methods
Patients and specimens
Thirty-nine consecutive patients (males 21 and females 18, age range 36–82 years) undergoing surgical resections for CRC at the Department of General Surgery of this hospital between November 2008 and November 2009 were recruited. The diagnosis of colorectal adenocarcinoma was confirmed by histology. The patients who received chemotherapy or radiation therapy either before or after surgery were excluded from the study. Matched samples from CRC, adjacent tissues (2.5 cm beyond cancer margins), and normal tissues (10 cm beyond cancer margins) were obtained at the time of operations, immediately preserved in liquid nitrogen and then stored at −80 °C until total RNA extraction. Standard tissues were taken, fixed in 10 % formalin, and embedded in paraffin wax. Histological samples were cut from paraffin-embedded blocks and stained with hematoxylin and eosin for light microscopic examination. Clinicopathological data were prospectively collected from each patient. The stages of CRC were assigned according to TNM and Dukes grades [7, 8]. The study protocols were approved by the ethics committee of this hospital affiliated to Guangzhou Medical College. Written consent was obtained from each patient.
Total RNA extraction and cDNA synthesis
Total RNA was extracted by chloroform–isopropanol–ethanol method using Trizol kit (Invitrogen. USA) according to the manufacturer’s instructions. The A260/A280 ratio of RNA was determined with colorimeter between 1.85 and 2.00. RNA integrity was qualified with formaldehyde degeneration gel electrophoresis at 80 V for 15 min. Three electrophoresis bands (5S, 18S, 28S) were visualized. Complementary DNA (cDNA) was synthesized following the instructions on M-MLV reverse transcriptase kit (Promega Co. USA). Briefly, 2 g of total RNA, 0.5 μg Oligo-dT15 primers, and 12 μl DEPC-treated H2O in a final 15 μl reaction volume were incubated at 70 °C for 5 min and subsequently on ice for 5 min to synthesize RNA primer compound. Then, 5 μl M-MLV buffers, 1.25 μl dNTP, 0.625 μl RNasin, 1 μl M-MLV reverse transcriptase, and 2.125 μl DEPC-treated H2O constituted RT reaction mixture. Afterward, 15 μl RNA primer compound and 10 μl RT reaction mixture were blended, incubated at 37 °C for 60 min and then at 70 °C for 15 min to synthesize cDNA.
Quantitative PCR
The mRNA of survivin-2B, survivin-3B, survivin-2α, and carcinoembryonic antigen (CEA) CAM5 (as positive control) was quantified by real-time quantitative PCR with SYBR GreenIon DNA Engine OpticonTM2 System (MJ Research Inc. Canada), while mRNA of survivin and survivin-△Ex3 was quantified with semiquantitative PCR (Bio-Rad Co. USA). The expression of housekeeping gene glyceraldehyde 3-phosphate dehydrogenase (GAPDH), as an internal control, and CEA CAM5 mRNA, as a positive control, was evaluated at the same time. Forward and reverse primer pairs for survivin, survivin-2B, survivin-△Ex3, survivin-3B, survivin-2α, GAPDH, and CEA CAM5 mRNA (provided by Invitrogen Inc., Shanghai, China) were referred from the literature [9, 10] (Table 1). cDNA was subjected to amplification in a final volume of 25 μl reaction mixtures, which contained 1 μl cDNA, 12.5 μl Go Taq colorless master mixes, 1 μl forward primer, 1 μl reverse primer, and 9.5 μl DEPC-treated H2O. Initial denaturation at 95 °C for 10 min was followed by different PCR conditions. Survivin: 31 cycles of denaturation at 95 °C for 30 s, annealing at 53 °C for 30 s, and elongation at 72 °C for 45 s; survivin-2B: 40 cycles of denaturation at 95 °C for 10 s, annealing at 57 °C for 30 s, and elongation at 72 °C for 45 s; survivin-△Ex3: 33 cycles of denaturation at 95 °C for 30 s, annealing at 55 °C for 30 s, and elongation at 72 °C for 45 s; survivin-3B and survivin 2α: 40 cycles of denaturation at 95 °C for 10 s, annealing at 51 °C for 30 s, and elongation at 72 °C for 45 s; CEA: 40 cycles of denaturation at 95 °C for 10 s, annealing at 53 °C for 30 s, and elongation at 72 °C for 45 s. The PCR conditions for GAPDH were as follows: initial denaturation at 95 °C for 10 min, then 40 cycles of denaturation at 95 °C for 30 s, annealing at 56 °C for 30 s, and elongation at 72 °C for 30 s, and again elongation at 72 °C for 5 min. PCR standard curves for real-time quantitative were generated from 6 serials tenfold dilution of specific purified cDNA from an initial concentration of 100 ng substrates.
Statistical analysis
All statistical analyses were performed by the SPSS 13.0 software package for Windows (SPSS Inc. Chicago, IL, USA). Continuous data were expressed as mean ± standard deviation (SD) and examined by Student’s t test. Wilcoxon rank sum test was applied for paired samples. Categorical variables were analyzed with χ 2 test and McNemar test. Bonferroni corrections were applied for multiple comparisons. A p value <0.05 (two tails) was considered statistically significant.
Results
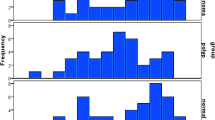
Qualification of PCR products
Electrophoresis bands of total RNA (5S, 18S, 28S) visualized under ultraviolet transillumination suggested RNA integrity (Fig. 1). The electrophoresis bands of PCR products of survivin, survivin-△Ex3, survivin-2B, survivin-3B, survivin-2α, CEA CAM5, and GAPDH were shown at 87, 109, 90, 60, 81, 145, and 222 bp, respectively, which were consistent with the theoretical length (Figs. 2, 3). Melting curves of GAPDH, survivin-2B, survivin-3B, survivin-2α, and CEA CAM5 suggested unique and specific PCR products. The regression coefficients (r 2) of the internal control gene (GAPDH) and the target genes in standard curves were 0.999. All parameters mentioned above supported the reliability of the results.
Expression rates of survivin and its splice variants (Table 2)
The expression rates of survivin, survivin-△Ex3, survivin-2B, survivin-3B, survivin-2α, and CEA CAM5 in CRC samples were significantly higher than those in adjacent tissues (P < 0.001) and those in normal tissues (P < 0.001). The expression rates of survivin-△Ex3 and survivin-2B in adjacent tissues were also significantly higher than those in normal tissues (P < 0.05).
Expression levels of survivin and its splice variants (Table 3)
The mRNA levels of survivin, survivin-△Ex3, survivin-2B, survivin-3B, survivin-2α, and CEA CAM5 in CRC samples were significantly higher than those of adjacent tissues (P < 0.001) and normal tissues (P < 0.001). The mRNA levels of survivin, survivin-△Ex3, and survivin-2B in adjacent tissues were also significantly higher than those in normal tissues (P < 0.05).
Survivin expression levels and clinicopathologic valuables of CRC patients
Gender, age, and tumor location were not associated with mRNA levels of survivin, any splice variant, and CEA CAM5. The mRNA levels of survivin, survivin-2B, and survivin-2α were not associated with any clinicopathologic valuable of CRC patients. However, elevated levels of survivin-△Ex3, survivin-3B, and CEA CAM5 were associated with lymphoid metastasis and advanced Dukes stages (P < 0.05). In addition, the elevated level of survivin-△Ex3 was associated with invasiveness and CEA CAM5 was associated with histological subtypes (Table 4).
Discussion
Apoptosis plays an important role in the progression and homeostasis of tissues. Deregulation of apoptosis is involved in carcinogenesis by abnormally prolonging cell survival, facilitating the accumulation of transforming mutations and promoting resistance to immunosurveillance. Survivin is a member in the inhibitors of apoptosis (IAP) family regulating cell cycles and controlling programmed cell death (apoptosis) [4, 5]. The over-expression of survivin may obliterate this apoptotic checkpoint and allow aberrant progression of transformed cells through mitosis. Human survivin gene has four dominants and two hidden exons. In addition to wild-type survivin (or termed survivin), alternative splicing of survivin pre-mRNA results in four different mRNAs, which encode four distinct proteins, that is, survivin-△Ex3, survivin-2B, survivin-3B, and survivin-2α [4, 5]. Each splice variant may modulate survivin function by interacting with survivin during mitosis [11]. Although the roles of survivin in carcinogenesis have been reported profusely in the literature, the effect of its splice variants on cancer development has not been fully documented especially in the field of CRC.
In normal adult tissues, survivin and its isoforms are undetectable, or expressed at a very low level, which can only be detected by very sensitive quantitative real-time PCR. Over-expression of survivin has been fully reported in a broad spectrum of malignancies including CRC [12, 13]. The significances of survivin over-expression with clinicopathological features of CRC patients have been investigated, but the results are not conclusive. Most papers supported a positive association of survivin expression in CRC samples with some clinicopathological characteristics of patients. Elevated survivin expression was correlated significantly with decrease in patient survival [14–16], high rate of recurrence [14], advanced TNM stage [17, 18], lymph node involvement [19, 20], liver metastasis [17], poor response to chemoradiotherapy [21, 22]. The apoptotic index was significantly lower and proliferating cell nuclear antigen (PCNA) labeling index was significantly higher in survivin-positive CRC cases than in survivin-negative ones [23, 24]. The immunoreactivity of survivin gradually increased in the transition from low to high dysplasia colorectal adenoma and eventually carcinoma [25]. In different studies mentioned above, survivin over-expression might present correlation with different clinicopathological parameters. Still, some studies found no significant difference of survivin expression in different tumor size and site, morphologic subtype, tumor grade, and clinical stage of CRC patients [26]. In the peripheral blood, circulating cancer cells expressing survivin mRNA were detected in 44.0 % CRC patients [27]. Survivin has been suggested to be a useful molecular marker for the diagnosis and prognosis [19], as well as a therapeutic target for CRC [6, 28].
Roles of survivin-△Ex3 and survivin-2B discovered in 1990s in carcinogenesis have been reported more profusely than those of survivin-3B and survivin-2α discovered in middle of the 2000s [29–31]. Over-expression of survivin-△Ex3 has been reported in a variety of cancers including acute and chronic lymphocytic leukemia [32], gastric cancers [33]. However, the roles of survivin-2B in carcinogenesis are still controversial. Some papers showed that both survivin-2B and survivin-△Ex3 played a role similar to that of survivin, whereas others indicated survivin-2B might act differently from survivin and survivin-△Ex3. When survivin-△Ex3 preserved its anti-apoptotic potential, survivin-2B might lose this potential and even play an opposing role to survivin in CRC patients [26]. Low survivin-2B expression or low survivin-2B/survivin ratio was found in patients with many malignancies including neuroblastoma [34], renal cell carcinoma [35], brain cancer [36], and gastric cancers [33, 37]. The different subcellular localization of survivin-△Ex3 (in the nucleus) and survivin-2B (in cytoplasm) may provide evidence for the functional diversity [38]. Other studies disagreed with these findings. Significantly, elevated expression of survivin, survivin-△Ex3, and survivin-2B was reported in astrocytoma [39], which were associated with a poorer prognosis [40].
In the field of CRC, Suga [26] found no significant difference in the expression levels of survivin and its splice variants in patients in different stages, but the expression ratio of survivin-2B/survivin was lower in late stage than that in early stage, which suggested a high survivin-2B/survivin ratio predicting good prognosis. Antonacopoulou reveled that the expression of all five survivin splice variants was elevated in CRC compared to that in normal tissue [41]. Pavlidou [13] reported that the mRNA expression of survivin was correlated with the expression of survivin-2B, survivin-ΔΕx3, and the ratio of survivin-2B/survivin, survivin-ΔΕx3/survivin. Associations were also found between the expression of survivin, survivin-ΔΕx3 and tumor size, invasiveness; between survivin-2B and morphologic cancer type; between the ratio of survivin-ΔEx3/survivin and prognosis. No association was observed between the expression of these three isoforms and TNM grade, metastasis, Dukes stage. Noton [11] demonstrated neither of survivin-2B nor survivin-ΔEx3 acted as competitor of survivin during mitosis. Studies in cancer cell lines also found no significant change of survivin-2B expression [11, 34]. On the whole, while some observations suggested that Survivin-2B might act as a natural antagonist against survivin, other studies, especially those regarding to CRC, disagreed with this finding. It is still difficult to integrate all of the information mentioned above, because the results have been contradictory.
So far, there have been only a few data regarding to survivin-2α and survivin-3B in this field. They were high expressed in several primary tumors and malignant cell lines [4]. Functional assays showed that survivin-2α might attenuate the anti-apoptotic activity of survivin. Subcellular localization and immunoprecipitation suggested a physical interaction between survivin-2α and survivin [31]. De Maria [42] reported that while the expression of survivin, survivin-△Ex3, and survivin-2B was significantly increased in oral squamous cell carcinoma, survivin-3B had only minor (not significant) increase. Knauer [43] found that only survivin-3B, but none of the other splice isoforms was cytoprotective. Sawai [44] found that survivin-3B decreased the invasion inhibition of colon cancer cells with 5-fluorouracil.
To our knowledge, this is the first study to simultaneously investigate the pathogenetic function of survivin and its four splice variants in CRC patients. Our study demonstrated that the mRNA expression rates and levels of survivin and its four splice variants were increased in CRC, which was consistent with most previous reports. Our findings that the increased expression rates and levels of survivin-∆Ex3 and survivin-3B, but not those of survivin-2B and survivin-2α, were related to CRC aggression and progression agreed with the results in most literature. Our results did not support the natural antagonistic function of survivin-2B to survivin, which was similar to most recent reports in CRC. The present study showed over-expression of survivin-2α in CRC, which has not been documented before.
There are some limitations in this study. Firstly, the sample size of the study may not be big enough to support a powerful conclusion. Although we found survivin over-expression in CRC, the difference did not reach significance. Secondly, we did not perform a study on the protein level to confirm our findings on gene (mRNA) level. On the whole, this study added new data to the knowledge already existed on survivin and its entire splice variants in CRC. Our findings may lead to better understanding of survivin as a biomarker for CRC diagnosis as well as a target for genetic therapy. Further larger studies are required in order to examine these findings.
References
Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90. doi:10.3322/caac.20107.
Graziano F, Cascinu S. Prognostic molecular markers for planning adjuvant chemotherapy trials in Dukes’ B colorectal cancer patients: how much evidence is enough? Ann Oncol: official journal of the European Society for Medical Oncology/ESMO. 2003;14(7):1026–38.
Eschrich S, Yang I, Bloom G, Kwong KY, Boulware D, Cantor A, Coppola D, Kruhoffer M, Aaltonen L, Orntoft TF, Quackenbush J, Yeatman TJ. Molecular staging for survival prediction of colorectal cancer patients. J Clin Oncol: official journal of the American Society of Clinical Oncology. 2005;23(15):3526–35. doi:10.1200/JCO.2005.00.695.
Li F. Role of survivin and its splice variants in tumorigenesis. Br J Cancer. 2005;92(2):212–6. doi:10.1038/sj.bjc.6602340.
Reed JC, Bischoff JR. BIRinging chromosomes through cell division–and survivin’ the experience. Cell. 2000;102(5):545–8.
Miura K, Fujibuchi W, Unno M. Splice isoforms as therapeutic targets for colorectal cancer. Carcinogenesis. 2012;33(12):2311–9. doi:10.1093/carcin/bgs347.
Gonen M, Weiser MR. Whither TNM? Semin Oncol. 2010;37(1):27–30. doi:10.1053/j.seminoncol.2009.12.009.
Mitchell PJ, Ravi S, Grifftiths B, Reid F, Speake D, Midgley C, Mapstone N. Multicentre review of lymph node harvest in colorectal cancer: are we understaging colorectal cancer patients? Int J Colorectal Dis. 2009;24(8):915–21. doi:10.1007/s00384-009-0697-z.
Schultz IJ, Kiemeney LA, Witjes JA, Schalken JA, Willems JL, Swinkels DW, de Kok JB. Survivin mRNA expression is elevated in malignant urothelial cell carcinomas and predicts time to recurrence. Anticancer Res. 2003;23(4):3327–31.
Span PN, Tjan-Heijnen VC, Heuvel JJ, de Kok JB, Foekens JA, Sweep FC. Do the survivin (BIRC5) splice variants modulate or add to the prognostic value of total survivin in breast cancer? Clin Chem. 2006;52(9):1693–700. doi:10.1373/clinchem.2006.071613.
Noton EA, Colnaghi R, Tate S, Starck C, Carvalho A, Ko Ferrigno P, Wheatley SP. Molecular analysis of survivin isoforms: evidence that alternatively spliced variants do not play a role in mitosis. J Biol Chem. 2006;281(2):1286–95. doi:10.1074/jbc.M508773200.
Williams NS, Gaynor RB, Scoggin S, Verma U, Gokaslan T, Simmang C, Fleming J, Tavana D, Frenkel E, Becerra C. Identification and validation of genes involved in the pathogenesis of colorectal cancer using cDNA microarrays and RNA interference. Clin Cancer Res: an official journal of the American Association for Cancer Research. 2003;9(3):931–46.
Pavlidou A, Dalamaga M, Kroupis C, Konstantoudakis G, Belimezi M, Athanasas G, Dimas K. Survivin isoforms and clinicopathological characteristics in colorectal adenocarcinomas using real-time qPCR. World J gastroenterol: WJG. 2011;17(12):1614–21. doi:10.3748/wjg.v17.i12.1614.
Fang YJ, Lu ZH, Wang GQ, Pan ZZ, Zhou ZW, Yun JP, Zhang MF, Wan DS. Elevated expressions of MMP7, TROP2, and survivin are associated with survival, disease recurrence, and liver metastasis of colon cancer. Int J Colorectal Dis. 2009;24(8):875–84. doi:10.1007/s00384-009-0725-z.
Xi RC, Biao WS, Gang ZZ. Significant elevation of survivin and living expression in human colorectal cancer: inverse correlation between expression and overall survival. Onkologie. 2011;34(8–9):428–32. doi:10.1159/000331132.
Abd El-Hameed A. Survivin expression in colorectal adenocarcinoma using tissue microarray. J Egypt Natl Canc Inst. 2005;17(1):42–50.
Lee YY, Yu CP, Lin CK, Nieh S, Hsu KF, Chiang H, Jin JS. Expression of survivin and cortactin in colorectal adenocarcinoma: association with clinicopathological parameters. Dis Markers. 2009;26(1):9–18. doi:10.3233/DMA-2009-0598.
Hernandez JM, Farma JM, Coppola D, Hakam A, Fulp WJ, Chen DT, Siegel EM, Yeatman TJ, Shibata D. Expression of the antiapoptotic protein survivin in colon cancer. Clin Colorectal Cancer. 2011;10(3):188–93. doi:10.1016/j.clcc.2011.03.014.
Yang D, Schneider S, Azuma M, Iqbal S, El-Khoueiry A, Groshen S, Agafitei D, Danenberg KD, Danenberg PV, Ladner RD, Lenz HJ. Gene expression levels of epidermal growth factor receptor, survivin, and vascular endothelial growth factor as molecular markers of lymph node involvement in patients with locally advanced rectal cancer. Clin Colorectal Cancer. 2006;6(4):305–11. doi:10.3816/CCC.2006.n.049.
Chu XY, Chen LB, Wang JH, Su QS, Yang JR, Lin Y, Xue LJ, Liu XB, Mo XB. Overexpression of survivin is correlated with increased invasion and metastasis of colorectal cancer. J Surg Oncol. 2012;105(6):520–8. doi:10.1002/jso.22134.
Kim K, Chie EK, Wu HG, Kim SG, Lee SH, Kang GH, Hyun CL, Ha SW. High survivin expression as a predictor of poor response to preoperative chemoradiotherapy in locally advanced rectal cancer. Int J Colorectal Dis. 2011;26(8):1019–23. doi:10.1007/s00384-011-1180-1.
Fraunholz I, Rodel C, Distel L, Rave-Frank M, Kohler D, Falk S, Rodel F. High survivin expression as a risk factor in patients with anal carcinoma treated with concurrent chemoradiotherapy. Radiat Oncol. 2012;7:88. doi:10.1186/1748-717X-7-88.
Kawasaki H, Toyoda M, Shinohara H, Okuda J, Watanabe I, Yamamoto T, Tanaka K, Tenjo T, Tanigawa N. Expression of survivin correlates with apoptosis, proliferation, and angiogenesis during human colorectal tumorigenesis. Cancer. 2001;91(11):2026–32.
Chen WC, Liu Q, Fu JX, Kang SY. Expression of survivin and its significance in colorectal cancer. World J Gastroenterol: WJG. 2004;10(19):2886–9.
Lin LJ, Zheng CQ, Jin Y, Ma Y, Jiang WG, Ma T. Expression of survivin protein in human colorectal carcinogenesis. World J Gastroenterol: WJG. 2003;9(5):974–7.
Suga K, Yamamoto T, Yamada Y, Miyatake S, Nakagawa T, Tanigawa N. Correlation between transcriptional expression of survivin isoforms and clinicopathological findings in human colorectal carcinomas. Oncol Rep. 2005;13(5):891–7.
Yie SM, Lou B, Ye SR, Cao M, He X, Li P, Hu K, Rao L, Wu SM, Xiao HB, Gao E. Detection of survivin-expressing circulating cancer cells (CCCs) in peripheral blood of patients with gastric and colorectal cancer reveals high risks of relapse. Ann Surg Oncol. 2008;15(11):3073–82. doi:10.1245/s10434-008-0069-x.
Sampath J, Pelus LM. Alternative splice variants of survivin as potential targets in cancer. Curr Drug Discov Technol. 2007;4(3):174–91.
Mahotka C, Wenzel M, Springer E, Gabbert HE, Gerharz CD. Survivin-deltaEx3 and survivin-2B: two novel splice variants of the apoptosis inhibitor survivin with different antiapoptotic properties. Cancer Res. 1999;59(24):6097–102.
Badran A, Yoshida A, Ishikawa K, Goi T, Yamaguchi A, Ueda T, Inuzuka M. Identification of a novel splice variant of the human anti-apoptosis gene survivin. Biochem Biophys Res Commun. 2004;314(3):902–7.
Caldas H, Honsey LE, Altura RA. Survivin 2alpha: a novel Survivin splice variant expressed in human malignancies. Mol Cancer. 2005;4(1):11. doi:10.1186/1476-4598-4-11.
Nakagawa Y, Yamaguchi S, Hasegawa M, Nemoto T, Inoue M, Suzuki K, Hirokawa K, Kitagawa M. Differential expression of survivin in bone marrow cells from patients with acute lymphocytic leukemia and chronic lymphocytic leukemia. Leuk Res. 2004;28(5):487–94. doi:10.1016/j.leukres.2003.10.013.
Meng H, Lu CD, Sun YL, Dai DJ, Lee SW, Tanigawa N. Expression level of wild-type survivin in gastric cancer is an independent predictor of survival. World J Gastroenterol: WJG. 2004;10(22):3245–50.
Islam A, Kageyama H, Hashizume K, Kaneko Y, Nakagawara A. Role of survivin, whose gene is mapped to 17q25, in human neuroblastoma and identification of a novel dominant-negative isoform, survivin-beta/2B. Med Pediatr Oncol. 2000;35(6):550–3.
Mahotka C, Krieg T, Krieg A, Wenzel M, Suschek CV, Heydthausen M, Gabbert HE, Gerharz CD. Distinct in vivo expression patterns of survivin splice variants in renal cell carcinomas. Int J Cancer (J int cancer). 2002;100(1):30–6. doi:10.1002/ijc.10450.
Yamada Y, Kuroiwa T, Nakagawa T, Kajimoto Y, Dohi T, Azuma H, Tsuji M, Kami K, Miyatake S. Transcriptional expression of survivin and its splice variants in brain tumors in humans. J Neurosurg. 2003;99(4):738–45. doi:10.3171/jns.2003.99.4.0738.
Krieg A, Mahotka C, Krieg T, Grabsch H, Muller W, Takeno S, Suschek CV, Heydthausen M, Gabbert HE, Gerharz CD. Expression of different survivin variants in gastric carcinomas: first clues to a role of survivin-2B in tumour progression. Br J Cancer. 2002;86(5):737–43. doi:10.1038/sj.bjc.6600153.
Mahotka C, Liebmann J, Wenzel M, Suschek CV, Schmitt M, Gabbert HE, Gerharz CD. Differential subcellular localization of functionally divergent survivin splice variants. Cell Death Differ. 2002;9(12):1334–42. doi:10.1038/sj.cdd.4401091.
Huang Y, Chen X, Chen N, Nie L, Xu M, Zhou Q. Expression and prognostic significance of survivin splice variants in diffusely infiltrating astrocytoma. J Clin Pathol. 2011;64(11):953–9. doi:10.1136/jclinpath-2011-200066.
Vivas-Mejia PE, Rodriguez-Aguayo C, Han HD, Shahzad MM, Valiyeva F, Shibayama M, Chavez-Reyes A, Sood AK, Lopez-Berestein G. Silencing survivin splice variant 2B leads to antitumor activity in taxane–resistant ovarian cancer. Clin Cancer Res: an official journal of the American Association for Cancer Research. 2011;17(11):3716–26. doi:10.1158/1078-0432.CCR-11-0233.
Antonacopoulou AG, Floratou K, Bravou V, Kottorou A, Dimitrakopoulos FI, Marousi S, Stavropoulos M, Koutras AK, Scopa CD, Kalofonos HP. The survivin-31 snp in human colorectal cancer correlates with survivin splice variant expression and improved overall survival. Anal Cell Pathol (Amst). 2010;. doi:10.3233/ACP-2010-0537.
De Maria S, Pannone G, Bufo P, Santoro A, Serpico R, Metafora S, Rubini C, Pasquali D, Papagerakis SM, Staibano S, De Rosa G, Farina E, Emanuelli M, Santarelli A, Mariggio MA, Lo Russo L, Lo Muzio L. Survivin gene-expression and splicing isoforms in oral squamous cell carcinoma. J Cancer Res Clin Oncol. 2009;135(1):107–16. doi:10.1007/s00432-008-0433-z.
Knauer SK, Bier C, Schlag P, Fritzmann J, Dietmaier W, Rodel F, Klein-Hitpass L, Kovacs AF, Doring C, Hansmann ML, Hofmann WK, Kunkel M, Brochhausen C, Engels K, Lippert BM, Mann W, Stauber RH. The survivin isoform survivin-3B is cytoprotective and can function as a chromosomal passenger complex protein. Cell Cycle. 2007;6(12):1502–9.
Sawai K, Goi T, Hirono Y, Katayama K, Yamaguchi A. Survivin-3B gene decreases the invasion-inhibitory effect of colon cancer cells with 5-fluorouracil. Oncol Res. 2010;18(11–12):541–7.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ge, QX., Li, YY., Nie, YQ. et al. Expression of survivin and its four splice variants in colorectal cancer and its clinical significances. Med Oncol 30, 535 (2013). https://doi.org/10.1007/s12032-013-0535-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-013-0535-6