Abstract
The prognosis for patients with lung cancer is poor with an average of 5-year overall survival rate of only 10–15 % taking all clinical stages together. The aim of this study was to elucidate the impact of the radiotherapy regimen on survival. Clinical data were collected from all the Swedish Oncology Departments for 1,287 patients with a diagnosed non-small cell lung cancer (NSCLC) subjected to curatively intended irradiation (≥50 Gy) during the years 1990 to 2000. The included patients were identified based on a manual search of all medical and radiation charts at the oncology departments from which the individual patient data were collected. Patients who did not have a histopathological diagnosis date and/or death date/last follow-up date as well as patients being surgically treated were excluded from the study (n = 592). Thus, 695 patients were included in the present study. Patients who received hyperfractionated radiotherapy (HR) had a higher local control rate compared with patients receiving conventional fractionation (CF) (38 vs. 49 % local relapse). The difference in survival between the two radiotherapy regimens was statistically significant in a univariate Cox analysis (p = 0.023) in favor of HR. This significance was, however, not retained in a multivariate Cox analysis (p = 0.56). Thus, the possible beneficial effects of hyperfractionation are still unclear and need to be further investigated in well-controlled prospective clinical trials, preferably including systemic treatment with novel drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The leading cause of cancer-related mortality worldwide is lung cancer [1] with an average of 5-year overall survival rate of only 10–15 % taking all clinical stages together [2]. Surgery is regarded as the treatment of choice for operable patients in stages I–IIIA, and these patients display a better 5-year survival rate [3]. However, many patients present with a locally advanced disease (stage IIIB) or comorbidities rendering less than 20 % of them amenable to surgery [4]. Thus, curatively intended radiotherapy, alone or in combination with chemotherapy, in many cases offers the only possibility of cure in localized NSCLC. Radical curatively intended radiotherapy for NSCLC has during the past decades typically been given once daily five times a week in daily fractions of 1.8–2.0 Gy to a total dose of 60–66 Gy delivered to the primary tumor and metastatic lymph nodes over a period of 6–7 weeks, whereas uninvolved mediastinal lymph nodes have been treated electively with the same fractionation with a total dose of 45 Gy [5, 6]. However, despite a huge number of studies including accelerated fractionation [7] and hypo- and hyperfractionation [8, 9] with the aim of improving local control and survival without increasing the risk for late complications, the optimal radiotherapy regimen for the treatment of NSCLC remains uncertain.
The aim of this study was to retrospectively investigate a large cohort of patients with NSCLC, who have undergone curatively intended radiotherapy, to elucidate the impact of the radiotherapy regimen on survival.
Materials and methods
The present study was performed in collaboration between all the Swedish Oncology Departments. Data were collected including all detectable patients with a diagnosed NSCLC, based on a review of all the radiation charts at each individual oncology department. All patients were subjected to curatively intended radiotherapy (≥50 Gy) during the time period of 1990–2000. The study was reviewed and approved by a research ethical committee (Uppsala research ethics committee, Dnr 2005: 025). The included patients were identified based on a manual search of all radiation charts from which the individual patients were identified and their medical charts retrieved. This manual search was carried out by a reference group composed of five oncologists, who visited all the oncology departments and reviewed the charts together with the medically responsible doctor for the treatment of lung cancer at the specific site. Clinical data were collected from all the Swedish Oncology Departments for 1,287 patients. Patients who did not have a histopathological diagnosis date and/or death date/last follow-up date as well as surgically treated patients were then excluded. Information regarding fractionation schedules was available for 695 patients, and these were included in the present analyses. The following variables were investigated: age, gender, time period, histopathology (defined as squamous cell carcinoma, adenocarcinoma or other non-small cell histopathology), stage (reevaluated by three of the authors based on available information in the charts as well as based on available X-ray investigations), all given treatment (first line as well as subsequent treatment), radiotherapy regimen (dose, fractionation), adverse effects of treatment, occurrence of relapse and cause of death.
Data were missing for some patients regarding some of these variables. However, these patients were not excluded from the study unless there was a lack of data required to estimate survival. Unfortunately, this causes inconsistencies among some of the frequencies accounted for in the results section of this article.
Statistics
Patient characteristics at diagnosis were presented using standard descriptive statistics.
Overall survival was analyzed with Kaplan–Meier product-limit estimates. Survival curves for different categories were compared using the log-rank test. The follow-up time was calculated from the date of diagnosis to death or last follow-up until the end of 2008. Age was defined as age at diagnosis.
Overall survival was also analyzed using Cox proportional hazards regression models. Univariate and multivariate analyses were performed. The multivariate models were adjusted by gender and age at diagnosis. Results were presented as hazard ratios with 95 % confidence intervals (95 % CI). In addition, p values were given where p < 0.05 was regarded as statistically significant.
Results
Patient characteristics
Of the 695 patients, 233 (34 %) were women. The median age and range was 65.0 (36–87) years. The dominating histopathology was squamous cell carcinoma (n = 369, 55 %), followed by adenocarcinoma (n = 173, 26 %), whereas the rest of the tumors were classified as other NSCLC histopathology (n = 125, 19 %). The predominant clinical stage was stage IIIb, which made up more than half of the patient population (n = 308, 52 %). Mean radiation dose and range given was 60.0 (50–74) Gy. Hyperfractionated radiotherapy (HR) was given to 105 patients (15 %), whereas the rest of the patients were treated with conventional fractionation. For patients receiving HR, the most common radiation regimen (given to 70 % of the patients) was 1.7 Gy in 36 or 38 fractions (range 1.5–1.8 Gy in 27–40 fractions), whereas for CF, the most common radiation regimens (given to 66 % of the patients) were 2 Gy in 28 or 30 fractions or 1.8 Gy in 33 fractions (range 1.5–2.5 Gy in 20–40 fractions). The total radiation dose was on average higher in the HR group (86 % ≥ 60 Gy as compared with 59 % ≥ 60 in the CF group), whereas the radiation field size was similar in both groups. Chemotherapy (induction and/or concomitant) was given more often to patients receiving HR. The difference was most pronounced for induction chemotherapy which was given to 53 (50 %) of the patients in the HR group, as compared with 74 (13 %) of the patients in the CF group. Among the adverse effects of treatment investigated (hoarseness, esophagitis, mucositis, radiation pneumonitis), esophagitis was the most prevalent as it was described in 276 (40 %) of the patients. Radiation pneumonitis was described in 94 (14 %) of the patients, whereas mucositis and hoarseness occurred in 57 (8 %) and 24 (3 %) patients, respectively. Esophagitis was more common in patients receiving HR than in patients who received CF (61 and 36 %, respectively), whereas radiation pneumonitis was less common with HR (8 and 15 %, respectively). Chemotherapy was given to a total of 194 (28 %) of 681 patients; of these 194 patients, 67 (35 %) received it only concomitantly with radiation treatment and 78 (40 %) were given it in a neoadjuvant setting only. Furthermore, 49 (25 %) patients were given both concomitant and induction chemotherapy. Relapse (distant or local) occurred in 484 (82 %) of 588 patients, with no difference between patients receiving HR and CF. However, when considering only local relapse in the previously irradiated area, local relapse was less common in the group receiving HR than in the CF group (38 and 49 %, respectively). Regarding the occurrence of distant relapse (CNS, liver, skeleton, lung and sites defined as “other”), there was no major difference between patients receiving HR and patients treated with CF. In the second-line setting, 113 (16 %) of 695 patients received chemotherapy. For the 520 patients, where information concerning cause of death was available, 490 (94 %) died from lung cancer, while 30 (6 %) died due to other causes. A summary of patient characteristics, given treatment, occurrence of relapse and cause of death is provided in Tables 1, 2.
Survival and radiotherapy regimen
The estimated median overall survival of all 695 patients was 12.0 months (95 % CI: 11.2–13.0 months), and the 5-year survival rate was estimated to 5.0 %. When comparing patients receiving HR to those receiving CF, the latter group had a significantly poorer overall survival (p = 0.022, log-rank test). The estimated median overall survival for patients receiving HR was 14.6 months (95 % CI: 11.4–19.4 months) and for patients who received CF it was 11.7 months (95 % CI: 11.0–12.7 months). The 5-year survival rate was estimated to 10.5 and 4.0 % for patients receiving HR and CF, respectively. The survival for patients with HR and CF, respectively, is shown in Fig. 1.
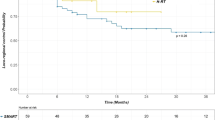
When comparing fraction size, patients receiving <2.0 Gy per fraction had a significantly better survival than those receiving ≥2.0 Gy per fraction (p = 0.038, log-rank test). Furthermore, when comparing fraction size with and without hyperfractionation, it was shown that patients who were given HR in fractions of <2.0 Gy had a significantly better overall survival than patients given CR (p = 0.046, log-rank test), irrespectively of fraction size for CR. (see Figs. 2, 3).
When comparing total radiation dose, patients receiving ≥60 Gy had a significantly better overall survival than those receiving <60 Gy (p < 0.0085, log-rank test). When comparing total radiation dose with and without hyperfractionation, there was a significant difference among groups (p = 0.018, log-rank test) indicating that patients who were given HR in a total dose of ≥60 Gy had a better overall survival than patients in the other groups (see Figs. 4, 5).
When comparing patients who had not been given chemotherapy in a neoadjuvant or concomitant fashion in addition to HR or CF radiotherapy, we found a tendency for a better median overall survival and 5-year survival rate for patients who received HR (14.6 months and 8.5 %, respectively) compared to those who received CF (11.5 months and 3.5 %, respectively). The difference was, however, not statistically significant (p = 0.15, log-rank test). The same tendency in favor of HR was found when comparing patients who had been treated with chemotherapy in a neoadjuvant or concomitant fashion in addition to HR or CF radiotherapy. Median overall survival and 5-year survival rate were 15.8 months and 12.3 %, respectively, for patients who received HR, and 12.7 months and 5.4 %, respectively, for the group receiving CF. However, this difference did not, however, reach statistical significance (p = 0.16, log-rank test). The survival for patients with HR and CF, with and without the addition of chemotherapy, is shown in Figs. 6, 7. When comparing patients in different stages receiving HR and CF, there was a tendency toward better survival for HF in stages III–IV, although the improvement was only borderline statistically significant (p = 0.059). Median overall survival and 5-year survival rate in stages III–IV were 15.2 months and 10.8 %, respectively, for patients who received HR, and 11.5 months and 4.9 %, respectively, for the group receiving CF. The survival for patients in stages I–II and III–IV treated with HR and CF, respectively, is shown in Figs. 8, 9. Estimated median survival and 5-year survival rate for different subgroups are presented in Table 3.
Univariate Cox analyses showed that the variables histopathology (SCC), stage, fraction size, total radiation dose and hyperfractionation were statistically significantly associated with survival, while gender, age and time period were not. Chemotherapy was only borderline significant (p = 0.081) (Table 4).
A multivariate Cox analysis was performed including age and gender as well as the statistically significant variables mentioned above. Also, chemotherapy was included. In this analysis, stage and histopathology were still found to be significantly associated with survival. Here, chemotherapy was also shown to be independently associated with better survival, whereas fraction size, total radiation dose and hyperfractionation lost their statistical significance (Table 5).
Discussion
Radiotherapy is a key component of curatively intended treatment of locally advanced and otherwise medically inoperable NSCLC. However, the prognosis for these patients remains still poor despite numerous attempts of refining the radiotherapy regimen as well as adding chemotherapy to the treatment [8].
In the present study, we show that there is a survival benefit for patients receiving HR as compared to patients receiving CF. This benefit was retained when comparing patients receiving only fractions of <2.0 Gy and total doses >60 Gy suggesting that the benefit of HR is independent of fraction size and total dose. Also, there is a survival benefit for patients receiving HR both when comparing patients receiving radiotherapy alone as well as when comparing patients receiving chemoradiotherapy in addition to radiotherapy. Due to the limited number of patients in these groups, the survival benefit did not, however, prove to be statistically significant. In a univariate Cox analysis, patients treated with HR had a statistically significantly better overall survival, but this survival benefit was not retained in a multivariate Cox analysis. The analysis did not show hyperfractionation to be independently associated with a better survival when simultaneously taking into account other prognostic factors, such as stage and chemotherapy, thus suggesting a more complex picture with possible confounding factors. It is worth noting that there were a higher percentage of patients in the HR group that received chemotherapy. Moreover, patients in the HR group received higher total radiation doses.
The strength of the present study is the size of the cohort and its population-based character, as well as the review of individual charts with a long follow-up period. All patients diagnosed with NSCLC and given curatively intended radiotherapy during 1990–2000 in a well-defined geographical area with a common health care system (Sweden) were included. A total of 695 patients with fractionation data were included in the analyses which makes it one of the largest studies in which individual data have been collected retrospectively in non-operated patients receiving curatively intended radiation treatment. However, there are some limitations with the present study setting. The TNM classification was based on the available imaging techniques during the different time intervals. Thus, there may be a stage migration with time and more sensitive staging techniques. Moreover, the majority of patients were not autopsied, especially among the elderly patient population, and thus, the cause of death might not have been thoroughly investigated. The specimens that were used at the time for histological classification of the patients in the present study were never reviewed for a second opinion. Also, there were missing values for some of the explanatory variables, which might have lead to a selection bias.
In hyperfractionated radiotherapy, the dose per fraction is reduced to below 1.8 Gy and a larger number of doses are given, which allows an escalation of the total dose given to the patient. In clinical practice, hyperfractionation is usually given as two daily fractions (b.i.d.) of 1.1–1.3 Gy, up to a total dose of 60–79.2 Gy [7, 9]. The radiobiological rationale behind the concept of hyperfractionation is based on exploiting the different capacity of tumor cells and the surrounding late responding normal tissue to recover from sublethal radiation damage [10]. Some small phase III trials that have randomized NSCLC patients into groups receiving either conventional radiotherapy or hyperfractionated radiotherapy have yielded promising results with 2-year overall survival rates in favor of hyperfractionated radiotherapy [11, 12]. In the RTOG 88-08/Eastern Cooperative Oncology Group (ECOG) 4588 randomized phase III trial, hyperfractionation to 69.6 Gy was compared with conventional fractionation to 60 Gy in a total of 306 patients with stage II–IIIB NSCLC [13]. The median survival was 11.4 months after conventional fractionation and 12.3 months after hyperfractionation, a difference which was not statistically significant. In the randomized phase III CHARTWEL trial by Baumann et al., the authors compared continuous hyperfractionated accelerated radiotherapy (60 Gy/40 fractions/2.5 weeks) with conventional fractionation (66 Gy/33 fractions/6.5 weeks) and found no statistically significant overall survival difference after 2, 3 and 5 years [14]. However, there was a significant trend for improved loco-regional control after CHARTWEL compared to CF with increasing UICC, T or N stage. In order to combine a shortening of the overall time of radiotherapy and a reduction in dose per fraction, accelerated hyperfractionated radiotherapy schedules were developed [9]. In continuous hyperfractionated accelerated radiotherapy (CHART), a total of 54 Gy is given in 36 fractions over 12 consecutive days including the weekend with a 6-h interval. In a large multicenter randomized controlled trial, CHART was compared with conventional radiotherapy given up to 60 Gy, and the results showed a significant survival improvement with CHART, giving a 2-year survival probability of 30 % for those treated with CHART as compared with 21 % for the conventional fractionation group [15]. The question whether chemotherapy in addition to hyperfractionated radiotherapy could provide a survival benefit was addressed in a prospective randomized trial by Jeremec et al. [16]. The authors showed that HR combined with concomitant chemotherapy offered significantly higher 5-year survival rates than HR alone (46 vs. 25 %). This is in line with the results from the present study although the difference did not reach statistical significance. A meta-analysis on nine randomized trials comparing modified radiotherapy (accelerated, hyperfractionated or both) to CF (one 1.8- to 2-Gy fraction per day, 5 days a week) in patients with non-metastatic lung cancer showed that modified fractionation improved overall survival compared to conventional RT (hazard ratio 0.87) with 3 % [17]. Among the radiotherapy-associated adverse effects, we found that esophagitis was more prevalent in the HR group, whereas radiation pneumonitis was more common in the patients receiving CF. This is in line with the results from the ECOG 2597 study where grade 3–4 esophageal toxicity was more common in the HR group (25 vs. 16 % in the CF group) while grade 3–4 pulmonary toxicity was only observed in the CF group (11 % of the patients) [18]. However, due to the difficulty of obtaining an accurate assessment of adverse effect in a retrospective fashion, the present results have to be interpreted carefully. Despite controversial results from the small number of phase III studies that have addressed this issue, radiobiological data indicate that there is reason to believe that hyperfractionation may improve survival in NSCLC, at least in a subgroup of patients [10]. In this large retrospective study, we show that there seems to be a local control benefit associated with hyperfractionated radiotherapy as compared with conventional fractionation in patients with NSCLC. However, whether HR also yields an improved survival in these patients warrants further investigation in future prospective clinical trials.
References
Minna JD, Fong K, Zochbauer-Muller S, Gazdar AF. Molecular pathogenesis of lung cancer and potential translational applications. Cancer J. 2002;8(Suppl 1):S41–6.
Baujat B, Bourhis J, Blanchard P et al. Hyperfractionated or accelerated radiotherapy for head and neck cancer. Cochrane Database Syst Rev. 2010;12:CD002026.
Benschop K, Minnaar R, Koen G et al. Detection of human enterovirus and human parechovirus (HPeV) genotypes from clinical stool samples: polymerase chain reaction and direct molecular typing, culture characteristics, and serotyping. Diagn Microbiol Infect Dis. 2010;682:166–73.
Free CM, Ellis M, Beggs L, Beggs D, Morgan SA, Baldwin DR. Lung cancer outcomes at a UK cancer unit between 1998–2001. Lung Cancer. 2007;572:222–8.
Bonomi M, Blanco-Savorio A, Cerchietti L, et al. Continuous hyperfractionated accelerated radiation therapy week-end less in combination with neoadjuvant chemotherapy for the treatment of stage III non-small-cell lung cancer. Lung Cancer. 2008;601:75–82.
Perez CA, Stanley K, Rubin P, et al. A prospective randomized study of various irradiation doses and fractionation schedules in the treatment of inoperable non-oat-cell carcinoma of the lung. Preliminary report by the radiation therapy oncology group. Cancer. 1980;4511:2744–53.
Baumann M, Appold S, Petersen C, Zips D, Herrmann T. Dose and fractionation concepts in the primary radiotherapy of non-small cell lung cancer. Lung Cancer. 2001;33(Suppl 1):S35–45.
Arriagada R, Komaki R, Cox JD. Radiation dose escalation in non-small cell carcinoma of the lung. Semin Radiat Oncol. 2004;144:287–91.
Saunders MI. Programming of radiotherapy in the treatment of non-small-cell lung cancer—a way to advance care. Lancet Oncol. 2001;27:401–8.
Saunders M, Dische S, Barrett A, Harvey A, Griffiths G, Palmar M. Continuous, hyperfractionated, accelerated radiotherapy (CHART) versus conventional radiotherapy in non-small cell lung cancer: mature data from the randomised multicentre trial. CHART Steering committee. Radiother Oncol. 1999;522:137–48.
Kagami Y, Nishio M, Narimatsu N, Ogawa H, Sakurai T. Prospective randomized trials comparing hyperfractionated radiotherapy with conventional radiotherapy in stage III non-small cell lung cancer. Nihon Igaku Hoshasen Gakkai Zasshi. 1992;5210:1452–5.
Fu S, Jiang GL, Wang LJ. Hyperfractionated irradiation for non-small cell lung cancer (NSCLC)—a phase III clinical trial. Zhonghua Zhong Liu Za Zhi. 1994;164:306–9.
Sause W, Kolesar P, Taylor SI, et al. Final results of phase III trial in regionally advanced unresectable non-small cell lung cancer: radiation therapy oncology group, eastern cooperative oncology group, and southwest oncology group. Chest. 2000;1172:358–64.
Baumann M, Herrmann T, Koch R et al. Final results of the randomized phase III CHARTWEL-trial (ARO 97-1) comparing hyperfractionated-accelerated versus conventionally fractionated radiotherapy in non-small cell lung cancer (NSCLC). Radiother Oncol. 2011;1001:76–85.
Saunders M, Dische S, Barrett A, Harvey A, Gibson D, Parmar M. Continuous hyperfractionated accelerated radiotherapy (CHART) versus conventional radiotherapy in non-small-cell lung cancer: a randomised multicentre trial. CHART Steering committee. Lancet. 1997;3509072:161–5.
Jeremic B, Shibamoto Y, Milicic B, et al. Hyperfractionated radiation therapy with or without concurrent low-dose daily cisplatin in locally advanced squamous cell carcinoma of the head and neck: a prospective randomized trial. J Clin Oncol. 2000;187:1458–64.
Saunders KJ, Spradlin JE. Conditional discrimination in mentally retarded subjects: programming acquisition and learning set. J Exp Anal Behav. 1993;603:571–85.
Belani CP, Wang W, Johnson DH, et al. Phase III study of the eastern cooperative oncology group (ECOG 2597): induction chemotherapy followed by either standard thoracic radiotherapy or hyperfractionated accelerated radiotherapy for patients with unresectable stage IIIA and B non-small-cell lung cancer. J Clin Oncol. 2005;2316:3760–7.
Acknowledgments
The authors would like to thank the Cancer Foundation at Gävle Hospital, The Research Fund at the Department of Oncology, Uppsala University Hospital and the Cancerfoundation, Umeå, Norrland. Also, the authors would like to thank all those who have helped with the gathering of patients and their medical charts.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Holgersson, G., Bergqvist, M., Nyman, J. et al. The impact of hyperfractionated radiotherapy regimen in patients with non-small cell lung cancer. Med Oncol 30, 320 (2013). https://doi.org/10.1007/s12032-012-0320-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12032-012-0320-y