Abstract
The purpose of this study was to evaluate the importance of diffusion-weighted magnetic resonance imaging (DW-MRI) apparent diffusion coefficient (ADC) values to predict treatment response to neoadjuvant chemotherapy (NCT) in patients with locally advanced breast cancer (LABC). Thirty-two patients with LABC underwent 2–4 cylces of NCT (docetaxel and epirubicin). The DW-MRI scans were performed within one week prior to chemotherapy and after the first course of treatment, respectively. Accordingly, tumor volumes, changes in tumor ADC values, and their degree of correlation were analyzed. The overall response (OR) was observed in 62.5% (95% CI, 45.7–79.3%) of patients after 2 cycles of NCT. The clinical complete response (CR) rate and pathological CR (pCR) rate were 15.6 and 9.4%, respectively. The stable disease (SD) rate was 34.4% (11 patients), and progressive disease (PD) was observed in only one patient (3.1%). After the first cycle of NCT, the ADC values in the CR + PR group significantly increased (P < 0.001). The initial ADC values before chemotherapy in the OR group were significantly lower than those in the SD + PD group (P < 0.001). The initial ADC values and the changes in tumor volume after chemotherapy were negatively correlated (r = −0.58, P = 0.02). The lower the initial tumor ADC value was the more obvious the decrease in tumor volume after chemotherapy. The changes in ADC values of tumors after chemotherapy and the changes in tumor volume were positively correlated (r = 0.96, P < 0.001). After chemotherapy, the greater the change in ADC value, the more the tumor volume was reduced. Using the initial ADC values of breast cancer tumors and the early changes in ADC values after NCT, we may be able to predict tumor response to chemotherapy. Tumors with low initial ADC values may be sensitive to chemotherapy; tumors with significantly increasing ADC values early after chemotherapy may be sensitive to chemotherapy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neoadjuvant chemotherapy (NCT) has been widely used for patient with locally advanced breast cancer over the last few decades [1]. The aims of neoadjuvant chemotherapy in locally advanced breast cancer (LABC) are to reduce the size of the primary tumor, rendering breast conservation surgery possible, and to improve overall survival by eradicating micrometastatic disease [2, 3]. The early knowledge of response to NCT has important consequences for optimal management, avoiding the continuation of toxic therapy in non-responding patients. In this regard, magnetic resonance imaging (MRI) is considered the best choice in evaluating the tumor and its response to the administered treatment because of its higher accuracy compared with traditional methods of physical examination, mammography, and sonography [4].
Enhanced MRI, diffusion-weighted (DW)-MRI, and MR spectroscopy (MRS) have made great progress in detection, diagnosis, efficacy monitoring, and prognosis of breast lesions. DW-MRI is a technique sensitized to the diffusive properties of water molecules, and it allows noninvasive in vivo measurements of diffusion [5]. Clinical applications of DW imaging arise from the principle that, during their random diffusion-driven displacements, water molecules probe tissue structures at a microscopic scale that is well beyond the usual image resolution [6]. Thus, DW-MRI can be used to characterize the ultrastructural properties and integrity of tissues [7]. DW-MRI was used to assess the early response of glioma [8], bone tumor [9], and breast cancer to neoadjuvant chemotherapy. In particular, DW-MRI seems to play a role in detecting early responses to chemotherapy in locally advanced breast cancer. DW-MRI, in fact, shows increased diffusion values due to cellular necrosis just after the first or second cycle of therapy treatment, before observing any reduction in the volume of the tumor [10–13].
DW-MRI depicts the restriction of water molecule diffusivity in malignant tissue as high signal intensity and yields a low apparent diffusion coefficient (ADC), which is a quantitative index of the diffusivity of water molecules [14, 15]. It has been reported that DW-MRI-derived ADC measurements inversely correlate with histopathologic assessment of primary central nervous system lymphoma (PCNSL) tumor cellular density [16]. There were limited data of the relationship between pretherapeutic ADC measurements and clinical response in patients with LABC undergoing neoadjuvant chemotherapy. The purpose of this study was to evaluate the importance of DW-MRI ADC values to predict treatment response to NCT in patients with LABC.
Methods
Patient population
Thirty-two patients with LABC, AJCC (American Joint Committee on Cancer) clinical stage III, who had received NCT with docetaxel and epirubicin from July 2007 to July 2010 were included in this prospective study. The baseline workup included a complete history and clinical examination, bilateral mammography, bilateral breast ultrasound, and DW-MRI.
A diagnosis of carcinoma was established through core needle biopsy of the primary tumor and palpable lymph nodes. The laboratory assessment consisted of a CBC, blood chemistry analysis, and measurement of the tumor markers (carcinoembryonic antigen and cancer antigen 15.3). The absence of distant metastasis was confirmed by chest X-ray, bone scan, and liver ultrasound. Patients with a primary inflammatory carcinoma or metastatic diseases in breast were excluded.
The median age was 46 years (range, 25–63 years). Eleven patients (34.4%) were postmenopausal. Patient characteristics are listed in Table 1. Patients received 2–4 cycles of preoperative NCT with docetaxel 75 mg/m2 and epirubicin 75 mg/m2 on day 1, repeated every 21 days. NCT was continued until tumors became operable in primary inoperable lesions or until breast-conserving surgery could be performed in primary operable tumors. After NCT, patients underwent appropriate surgery according to the size of their residual tumor. Radiation therapy was applied after the completion of surgery or chemotherapy if adjuvant chemotherapy was given. Postoperative irradiation treatment was delivered to the chest wall, internal mammary lymph nodes, and supraclavicular/axillary lymph nodes. Finally, patients with hormone receptor–positive tumors received tamoxifen for 5 years. All procedures were carried out with the prior informed consent of the patients. The institutional review board approved the protocol of this study.
Assessment of response to neoadjuvant chemotherapy
The pathological and clinical assessment of response to NCT was made. The clinical stage and size of the primary tumor was recorded before treatment. The measurement of the primary tumor consisted of the product of its greatest diameter and its perpendicular diameter. The clinical response was evaluated at each cycle of chemotherapy and prior to definitive surgery on day 21 of the last cycle of chemotherapy according to the product of primary tumor diameters and the axillary clinical status, and was classified as a complete response (CR), partial response (PR), stable disease (SD), or progressive disease (PD) according to standard UICC (International Union Against Cancer) criteria [17]. The patients were classified into two groups: the objective response group (OR), into which all patients classified as CR or PR were placed. In the surgical specimen, pathological responses (pCRs) were evaluated according to Kuerer et al. criteria [4]. In particular, the absence of invasive cancer on both the primary breast tumor and axillary lymph nodes qualified for PCR [18].
DW-MRI examination
DW-MRI of the array spatial sensitivity encoding technique (ASSET) was used to analyze the tumor ADC. Tumor volume was measured with the software techniques of Volume Imaging for Breast Assessment (VIBRANT). For all 32 patients, the MRI scanning, ASSET-DW-MRI, and multiphase VIBRANT examinations were carried out within 1 week prior to chemotherapy and 18–21 days after the first course of treatment, respectively.
A GE 1.5T EXCITE HD superconducting magnetic resonance scanner with 4-channel phased array surface coil for breasts was used. Patients were in the prone position with the bilateral breast drooping naturally when the MRI scans, ASSET-DW-MRI, and multiphase VIBRANT were taken. The imaging parameters were as follows: T1WI: TR/TE = 600/11.5 ms, layer thickness 4 mm, spacing 1.0 mm, array 320 × 220, NEX = 1.0. FSE T2WI: TR/TE = 4,500/90 ms, layer thickness 4 mm, spacing 1.0 mm, and array 320 × 256, NEX = 2.0. In axial scanning, 32 layers were taken in each imaging sequence. Scanning position, number of scanning layers, thickness, and spacing were repeatedly copied, FOV = 32–36 cm. ASSET-DWI was conducted with an array of 128 × 128, b = 0, 1,000 s/mm2 and 0, 600 s/mm2. The shortest TR of 32 layers was collected, TR = 6,950–7,000 ms, TE = 58 ms, ASSET R value (scan time reduction factor) = 2. After scanning, multiphase MRI images were obtained using the VIBRANT software. Applying axial or sagittal planes, the parallel bilateral breast shimming and fat suppression parameters were adjusted. The axial imaging parameters were as follows: TR/TE = 5.1/2.5 ms, TI = 17 ms, layer thickness 2.6 mm, level interpolation ZIP2, the block thickness of scanning 62–66 layers, array 420 × 310, NEX = 0.75, covering bilateral breast, 1.3 mm reconstruction, and acquisition time per phase 57 s. The sagittal imaging parameters were TR/TE = 4.9/2.4 ms, TI = 7 ms, layer thickness 3.4 mm, the block thickness of scanning 84 layers, array 300 × 192, NEX = 1.0, covering bilateral breast, 1.7 mm reconstruction, and acquisition time per phase 57 s. The contrast agent, Gd-DTPA (Magnevist meglumine) of 0.1 mmol/kg body weight was intravenously injected with 2.0 ml/s from the dorsal vein of the hand using a high-pressure syringe. Using multiphase dynamic enhancement, masks were acquired before the bolus of the contrast agent; then, the original position of patients remains unchanged and contrast agent bolus was applied immediately with the venous injection of the same volume of normal saline. Approximately 15 s after the start of the injection of contrast agents, dynamic volume enhancement was performed and 8–10 phases with no interval were continuously collected with acquisition time of 57 s for each phase.
Measurement of tumor size and ADC values
The enhanced MRI scope range is defined by the tumor. The three orthogonal diameters were measured as tumor volume before treatment (V1) and tumor volume after one cycle of chemotherapy (V2). The ADC values were analyzed by ASSET-DWI, with b values of 0–1,000 s/mm2. The value of the initial ADC before chemotherapy (ADC1) and the tumor ADC value after the first cycle of chemotherapy (ADC2) were measured. Changes in ADC values in early tumor were calculated (ΔADC = ADC2 − ADC1).
Results
Neoadjuvant treatment, clinical response rate, and surgery
Twenty-one patients received two cycles of NCT, 7 patients with 3 cycles, and 4 patients with 4 cycles. A total of 79 cycles were administered with the median number of two cycles per patient (range, 2–4). Delivered relative dose intensities were 93.7% (74 of 79) for both docetaxel and epirubicin. The OR was observed in 62.5% (95% CI, 45.7–79.3%) of patients after 2 cycles of NCT. The CR rate and pCR rate were 15.6 and 9.4%, respectively. The SD rate was 34.4% (11 patients) and PD was observed in only one patient (3.1%), occurred after 2 cycles of NCT. Surgery could be performed in all 32 patients. Breast-conserving surgery could be performed in 10 patients (31.3%). Modified radical mastectomy was performed in patients for whom breast-conserving therapy was not indicated.
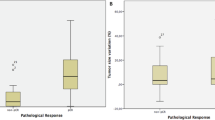
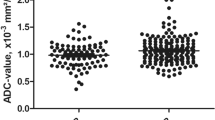
Changes in tumor ADC values before and after the first course of NCT
Tumor ADC values before and after the first course of NCT are shown in Table 2 and Fig. 1. The ADC values of CR + PR group significantly increased after chemotherapy (P < 0.001), suggesting the changes in ADC values may be associated with chemotherapy response. For the tumors sensitive to chemotherapy, early ADC value was significantly increased. The initial ADC value before chemotherapy in the CR + PR group was significantly lower than that in SD + PD group (P < 0.001), suggesting that tumors with low initial ADC values may be sensitive to chemotherapy.
Diffusion-weighted magnetic resonance imaging (DW-MRI) apparent diffusion coefficient (ADC) values in patients with locally advanced breast cancer (LABC) undergoing neoadjuvant chemotherapy (NCT). Before NCT, tumor size was 22 × 21 × 28 mm, the type of time–intensity curve (TIC) was a clearance curve, and ADC value was 0.92 (a–c); poorly differentiated tumor cells in hematoxylin-eosin (HE) staining (d); immunohistochemistry (IHC) showed HER-2 (3+) (e); After the first cycle of NCT, tumor size was 18 × 20 × 27 mm, the type of TIC was a platform curve, and ADC value was 1.12 (f–h); after three cycles of NCT, resection of tumor tissue, compared with the biopsy before NCT (d), can only see some well-differentiated glands and interstitial proliferation of fibrous tissue (i); HER-2 (2+) (j)
Changes in ADC values and tumor volume before and after the first course of NCT and their relationship
The initial ADC values of tumors (ADC1) and the ΔADC after the first course of NCT were negatively correlated (r = −0.55, P = 0.02). The lower the initial ADC values, the more the tumor ADC values increased after 1 cycle of chemotherapy. The initial ADC and the changes in tumor volume after chemotherapy were also found to be negative correlated (r = −0.58, P = 0.02). The lower the initial tumor ADC value was the more the tumor decreased in size after the first course of NCT. Changes in tumor ADC values after the first course of NCT (ΔADC) and changes in tumor volume after the first course of NCT were positively correlated (r = 0.96, P < 0.001). The larger the ΔADC for a tumor, the more significantly tumor volume decreased after chemotherapy.
Discussion
Recently, the evaluation of NCT reactions in patients with LABC is gradually becoming a hot topic for research. Research related to pathology, tumor markers, and genetics has made some progress [19], but these methods require repeated biopsy, which is an invasive procedure. Noninvasive evaluation methods include physical examination, mammography, ultrasound, and MRI. Results of noninvasive studies showed that after NCT, the compliance rates of residual tumors with pathology were 47% by palpation determination, 49.4% by mammography, and 66.3% by ultrasound. For the non-reachable tumors of clinical CR after chemotherapy, evaluation based on any single traditional method is not accurate. The reason is that the dense breast tissue on the molybdenum target X-ray film often blurs the tumor boundary, causing difficulties in judging the size of the tumor. Post-chemotherapy reactions, such as fibrosis, often lead to overestimation of tumor size in physical palpation. Recently, MRI assessment of the efficacy of NCT for breast cancer gained attention. It showed significant advantages, especially for multicenter or multifocal lesions [20]. The result of Rieber et al. showed that MRI can qualitatively evaluate tumor response after chemotherapy, with specificity of 96.3% and negative predictive value of 89.7%. Based on the study of 41 cases of reachable breast cancer, the results reported by Yeh et al. [21] confirmed that using pathology results as the gold standard, the compliance rates of clinical examination, mammography, ultrasound, and MRI were 19, 26, 35, and 71%, respectively. MRI was found to have the highest compliance rate. Unlike traditional breast MRI technology, new MRI techniques such as DW-MRI and MRS have provided quantitative measurement methods for the characteristics of breast cancer tissue. These characteristics are highly correlated to the evaluation of tumor progression and response to chemotherapy [22]. Since the changes in tumors at the molecular or cellular level occur before changes in tumor volume after treatment, the early evaluation of treatment response should not depend on the volume change. The prediction of tumor response to treatment using water diffusion changes in early stages has some clinical significance. Tissue changes can be reflected at the cellular level. This provides a valuable predictor for clinical evaluation of treatment response or efficacy of early detection.
Two kinds of water molecules exist with random motion in biological tissue. The first type includes water molecules with slow movement and low diffusion that attach to large molecules or are limited to the cell membrane. The other includes water molecules with high diffusion, which primarily exist as extracellular water molecules [23]. Affected by molecular adhesion, cell membrane permeability, tissue structure orientation, and other factors, the value of the ADC of biological tissue can reflect the state of tissue diffusion. As a result, DWI can noninvasively reflect biological characteristics of tissue through water diffusion characteristics shown by ADC values. The published results confirmed that water diffusion changes after tissue injury were mainly due to changes in volume and curvature in extracellular space [24, 25]. Extracellular space is mainly determined by cell density. Water diffusion in glioma gradually increased from dense cells of solid tumors to the loose cells of necrotic area. The water diffusion coefficient also gradually increased from active tumor to tumor necrosis after treatment [26]. Because cytotoxic drugs damage cancer cells, the cell membrane integrity and permeability are the first to change. Tumor cell density decreased after the death of tumor cells, resulting in expanding extracellular space, thereby increasing water diffusion in the damaged tumor tissue [25]. Using the ADC values showing changes in water diffusion, DWI can reflect the tumor sensitivity to the drug in the early stages of drug treatment. Preliminary findings based on animal experiments and research on patients with central nervous system tumors showed that tumor ADC values increased in the early stages after radiotherapy and chemotherapy [27–29]. In the current study, it was found that pretreatment ADC values and their early changes after treatment were related to changes in tumor volume after treatment.
As an application of DWI in ASSET technology, this study first analyzed the changes in ADC values, monitoring the response of breast cancer to NCT. ASSET-DWI can not only reduce the acquisition time, but also correct the susceptibility artifacts and reduce the pathological distortion. According to the results in this study, the initial ADC values of breast cancer before chemotherapy were negatively correlated to the tumor volume change after treatment. Changes in tumor ADC values before and after the first cycle of chemotherapy were positively correlated to changes in tumor volume. These results indicate that initial ADC values of breast cancer tumors and their early changes after NCT may be related to the tumor response to chemotherapy, as tumors with low initial ADC values may be sensitive to chemotherapy; if the ADC value at early stage after chemotherapy significantly increases, this tumor may be sensitive to chemotherapy.
In conclusion, changes in ADC values can provide a basis for early estimation of the efficacy of chemotherapy. For tumors sensitive to NCT, an increase in ADC values can occur after the first cycle of chemotherapy. These changes in ADC values occur earlier than the change in tumor volume. It is not necessary to wait for the volume changes in order to determine the efficacy of chemotherapy. This can act as a basis for early adjustment of treatment strategies. The ADC values before chemotherapy can be used as a basis for prospective judging of NCT. Considering the indications for NCT, if a tumor has high ADC value, its sensitivity to chemotherapy is lower than a tumor with a low ADC value.
References
Lee J, Im YH, Lee SH, et al. Evaluation of ER and Ki-67 proliferation index as prognostic factors for survival following neoadjuvant chemotherapy with doxorubicin/docetaxel for locally advanced breast cancer. Cancer Chemother Pharmacol. 2008;61:569–77.
Fisher B, Brown A, Mamounas E, et al. Effect of preoperative chemotherapy on local-regional disease in women with operable breast cancer: findings from national surgical adjuvant breast and bowel project B-18. J Clin Oncol. 1997;15:2483–93.
Rastogi P, Anderson SJ, Bear HD, et al. Preoperative chemotherapy: updates of national surgical adjuvant breast and bowel project protocols B-18 and B-27. J Clin Oncol. 2008;26:778–85.
Londero V, Bazzocchi M, Del Frate C, et al. Locally advanced breast cancer: comparison of mammography, sonography and MR imaging in evaluation of residual disease in women receiving neoadjuvant chemotherapy. Eur Radiol. 2004;14:1371–9.
Basser PJ, Mattiello J, LeBihan D. Estimation of the effective self-diffusion tensor from the NMR spin echo. J Magn Reson B. 1994;103:247–54.
Le Bihan D, Mangin JF, Poupon C, et al. Diffusion tensor imaging: concepts and applications. J Magn Reson Imaging. 2001;13:534–46.
Neil J, Miller J, Mukherjee P, et al. Diffusion tensor imaging of normal and injured developing human brain—a technical review. NMR Biomed. 2002;15:543–52.
Hamstra DA, Chenevert TL, Moffat BA, et al. Evaluation of the functional diffusion map as an early biomarker of time-to-progression and overall survival in high-grade glioma. Proc Natl Acad Sci USA. 2005;102:16759–64.
Hayashida Y, Yakushiji T, Awai K, et al. Monitoring therapeutic responses of primary bone tumors by diffusion-weighted image: Initial results. Eur Radiol. 2006;16:2637–43.
Pickles MD, Gibbs P, Lowry M, et al. Diffusion changes precede size reduction in neoadjuvant treatment of breast cancer. Magn Reson Imaging. 2006;24:843–7.
Theilmann RJ, Borders R, Trouard TP, et al. Changes in water mobility measured by diffusion MRI predict response of metastatic breast cancer to chemotherapy. Neoplasia. 2004;6:831–7.
Manton DJ, Chaturvedi A, Hubbard A, et al. Neoadjuvant chemotherapy in breast cancer: early response prediction with quantitative MR imaging and spectroscopy. Br J Cancer. 2006;94:427–35.
Sharma U, Danishad KK, Seenu V, et al. Longitudinal study of the assessment by MRI and diffusion-weighted imaging of tumor response in patients with locally advanced breast cancer undergoing neoadjuvant chemotherapy. NMR Biomed. 2009;22:104–13.
Koh DM, Collins DJ. Diffusion-weighted MRI in the body: applications and challenges in oncology. AJR Am J Roentgenol. 2007;188:1622–35.
Woodhams R, Matsunaga K, Iwabuchi K, et al. Diffusion-weighted imaging of malignant breast tumors: the usefulness of apparent diffusion coefficient (ADC) value and ADC map for the detection of malignant breast tumors and evaluation of cancer extension. J Comput Assist Tomogr. 2005;29:644–9.
Guo AC, Cummings TJ, Dash RC, et al. Lymphomas and high-grade astrocytomas: comparison of water diffusibility and histologic characteristics. Radiology. 2002;224:177–83.
Hayward JL, Carbone PP, Heusen JC, et al. Assessment of response to therapy in advanced breast cancer. Br J Cancer. 1977;35:292–8.
Kuerer HM, Newman LA, Smith TL, et al. Clinical course of breast cancer patients with complete pathologic primary tumor and axillary lymph node response to doxorubicin-based neoadjuvant chemotherapy. J Clin Oncol. 1999;17:460–9.
Korde LA, Lusa L, McShane L, et al. Gene expression pathway analysis to predict response to neoadjuvant docetaxel and capecitabine for breast cancer. Breast Cancer Res Treat. 2010;119:685–99.
Abraham DC, Jones RC, Jones SE, et al. Evaluation of neoadjuvant chemotherapeutic response of locally advanced breast cancer by magnetic resonance imaging. Cancer. 1996;78:91–100.
Yeh E, Slanetz P, Kopans DB, et al. Prospective comparison of mammography, sonography, and MRI in patients undergoing neoadjuvant chemotherapy for palpable breast cancer. AJR Am J Roentgenol. 2005;184:868–77.
Delille JP, Slanetz PJ, Yeh ED, et al. Invasive ductal breast carcinoma response to neoadjuvant chemotherapy: noninvasive monitoring with functional MR imaging pilot study. Radiology. 2003;228:63–9.
Mulkern RV, Zengingonul HP, Robertson RL, et al. Multi-component apparent diffusion coefficients in human brain: relationship to spin-lattice relaxation. Magn Reson Med. 2000;44:292–300.
Norris DG, Niendorf T, Leibfritz D. Health and infarcted brain tissues studied at short diffusion times: the origins of apparent restriction and the reduction in apparent diffusion coefficient. NMR Biomed. 1994;7:304–10.
Szafer A, Zhong J, Gore JC. Theoretical model for water diffusion in tissues. Magn Reson Med. 1995;33:697–712.
Chenevert TL, Brunberg JA, Pipe JG. Anisotropic diffusion in human white matter: demonstration with MR techniques in vivo. Radiology. 1990;177:401–5.
Chinnaiyan AM, Prasad U, Shankar S, et al. Combined effect of tumor necrosis factor-related apoptosis-inducing ligand and ionizing radiation in breast cancer therapy. Proc Natl Acad Sci USA. 2000;97:1754–9.
Mardor Y, Roth Y, Ochershvilli A, et al. Pretreatment prediction of brain tumors’ response to radiation therapy using high b-value diffusion-weighted MRI. Neoplasia. 2004;6:136–42.
Roth Y, Tichler T, Kostenich G, et al. High-b-value diffusion-weighted MR imaging for pretreatment prediction and early monitoring of tumor response to therapy in mice. Radiology. 2004;232:685–92.
Acknowledgments
This study is supported in part by Chinese Army Medical High-tech Important Research Fund (2010GXJS092). The authors have no commercial, proprietary, or financial interest in the products or companies described in this article.
Conflict of interest
None. The authors have no commercial, proprietary, or financial interest in the products or companies described in this article.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Xi-ru Li and Liu-quan Cheng contributed equally to this article.
Rights and permissions
About this article
Cite this article
Li, Xr., Cheng, Lq., Liu, M. et al. DW-MRI ADC values can predict treatment response in patients with locally advanced breast cancer undergoing neoadjuvant chemotherapy. Med Oncol 29, 425–431 (2012). https://doi.org/10.1007/s12032-011-9842-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12032-011-9842-y