Abstract
Lung cancer (LC) is now the leading cause of cancer mortality in the world, therefore it would be useful to identify prognostic factors to determine patient outcome. The objective of this study is to evaluate the usefulness of platelet counts at the time of diagnosis as a prognostic factor. A retrospective study of patients with histological diagnostic evidence of LC was carried in our catchment area over a 3-year period. Survival adjusted for other factors was assessed according to the platelet count at the time of diagnosis. Patients with platelet levels within the reference range (RR) (135000–381000/µl) were divided into two groups, between 135000–258000/µl and 258000–381000/µl. A third group was made up of patients with platelet counts over 381000/µl. Adjusted survival was analysed using Cox regression models. Patients with high platelets have a 37% worse survival than those with a platelet level within the RR, but lower than 258000/µl. When tumour stage is included in the covariates, platelet levels are no longer an independent survival factor. In conclusion, platelet levels at the time of diagnosis could be a useful prognostic factor in LC.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Lung cancer (LC) is the most frequent cause of death by cancer in the world, with a high mortality that reduces the 5-year survival to less than 15% [1]. It is also the most commonly diagnosed cancer in men and the third in women (after breast and uterus), with the highest incidence in the general population [1].
In view of its high incidence and mortality, controlling the known risk factors and advancing the debate on early diagnosis [2, 3]. Correctly identifying and understanding other prognostic factors may be required to allow us to optimise the management of these patients and to individualise survival probability, as well as the therapy of each patient [4].
Thrombocytosis is frequently found in patients with LC [5], which some studies have associated with a lower survival [5, 6], although a recent systematic review did not include this analytical data among the indicators for the prognostic stratification of LC [7].
A reduction in mortality and in the progression to tumour metastasis has recently been observed in patients treated with low molecular weight heparin, which could be associated with platelet activity, given the known interaction of this drug with these cells [8, 9].
The objective of our study was to evaluate whether the platelet levels at the time of diagnosis could be useful in establishing a prognosis in LC patients.
Materials and methods
All patients diagnosed with LC for the first time between 1 January 1997 and December 1999 in the Santiago de Compostela University Hospital Complex, which covers a health population of 418,000 inhabitants and has four hospital centres within the Galician public health network, were included in the study. The information on current LC cases was obtained through the Admission and Clinical Documentation Services and Histopathology. The patient clinical history was then accessed to collect the data for this study: age, sex, stage, smoking habits, histology type, comorbidity, blood platelets and date of death.
The histological classification was made according to the 1982 World Health Organisation Guidelines [10].
Four groups were established according to the distribution (quartiles) for the analysis of age.
Comorbidity was evaluated at the time of diagnosis using the Charlson Comorbidity Index [11]. Four mutually exclusive categories were established: the first three with a Charlson index equal to 0, 1, 2, respectively, and the last one when the value of the Charlson index was equal to or greater than 3.
Smoking habits were stratified into three possible, mutually exclusive, categories: never smoked, active smoker and ex-smoker.
Patients were excluded if the histocytology typing could not be confirmed or located for the follow-up. The date of death was taken from the clinical history, death register or by a telephone call to the home address.
The platelet levels were stratified into three levels. Patients with normal platelets, according to the reference ranges (RR) (between 135000 and 381000/µl) established by the Clinical Analysis Department of our hospital, were divided using the mean value of the RR (258000/µl), into two groups, from 135000 to 258000 platelets/µl, and from this value up to 381000 platelets/µl. The third group was made up of patients with platelet levels over 381000/µl. Patients with platelet values less than our laboratory RR were excluded from the study.
Each patient was followed up until 30 June 2007, or until their death.
Analysis
The normality of the distributions was assessed using the Kolmogorov–Smirnov test with Lilliefors correction. The Levene test was applied to assess the homogeneity of the variances. The chi-squared test was used for the comparison of the categorical variables. The student t test was used for the comparison of the continuous variables which followed a normal distribution, and if there was a non-Gaussian distribution, the Mann–Whitney U test was used.
The survival time was estimated in days from the time of diagnosis until the time of death, or until the last follow-up date, using the Kaplan–Meier method to calculate the survival probabilities.
The log-rank test was used to compare the survival curves.
The influence of the platelet levels on the survival of LC patients was calculated using Cox regression adjusted for the rest of the variables analysed. Two models were used, one including the tumour stage and another without including this parameter.
A P < 0.05 was considered statistically significant.
The analyses were performed using the Statistical Package for Social Sciences (SPSS) program, version 15.0 in Spanish.
Results
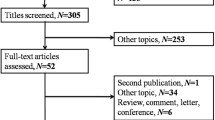
A total of 481 cases of diagnosed LC were initially collected, which is an overall incidence of 41.79/100,000 inhabitants, and when adjusted to the European population, 30.92/100,000 inhabitants. Of the 419 patients finally included in this study, 21 (5.01%) are still alive. Of those excluded, 42 cases were due to having a radiological clinical diagnosis, 11 cases of doubtful histology, 2 cases due to thrombocytopenia (low platelets) and 7 cases due to not being located in the follow-up (the clinical history suggested they had moved to other areas). The general characteristics of the patients are presented in Table 1. Stages III B and IV were diagnosed in 75.3% of the cases.
A total of 103 (21.9%) patients with LC had thrombocytosis.
Patients with a high platelet count are younger, have a lower survival and are in more advanced stages than those included in other groups, with no differences observed in the rest of the parameters analysed (Table 2).
The survival analysis showed that patients with a thrombocytosis have a 37% lower survival than those of group 1 (normal platelets, but below the mean of the RR) (Fig. 1, Table 3). No differences were observed between the two groups with normal platelets, or between the patients with a thrombocytosis and those of group 2 (normal platelets, but above the mean of the RR). On including the stage among the covariables, no independent effect of the platelet count was seen on the survival (Table 4), as would be expected given the association observed between the stage and the platelet count (Table 2).
Discussion
Our data suggest that thrombocytosis, measured at the time of diagnosis, may be an independent indicator of a poor prognosis in LC, coinciding with that obtained in other studies with Japanese and Danish populations [5, 6].
Thrombocytosis is a common finding in oncological disease, reported to be present in 10% to 60% of LC patients [5, 6, 12].
Higher platelet levels are observed in the younger age group of our population, as has been mentioned in other patients with LC and in a general population [6, 13, 14], without showing any significant differences between the different histology types [5, 12]. Contradictory results have been reported in the literature as regards the tumour stage. Thus, in a Danish population, an association was seen, as in our patients, between the increase in platelets and the more advanced stages of the tumour disease [5], while in the study by Aoe with a Japanese population this association was not observed [6].
The mechanism for producing thrombocytosis seems to be due to an increase in platelet production, different mechanisms have been described in patients with tumours which could explain this thrombocytopoietic action, with the participation of many mediators such as, IL-6, IL-1, GM-CSF or thrombopoietin [15–17].
The causes of a lower survival in patients with a thrombocytosis mainly include, physiological mechanisms associated with the incidence of vascular disease, increased tumour resistance to chemotherapy and progression of the tumour to more advanced stages.
The relationship between a more advanced tumour stage and higher mortality [18, 19] is also reasonably well established. Given the higher frequency of thrombocytosis in patients with advanced stages, this fact in itself could explain the poor prognosis of this patient group.
On the other hand, it could be due to the increased cardiovascular disease associated with the high platelet count, as a higher incidence of deep vein thrombosis and ischaemic heart disease [20–22] has been reported.
As regards resistance to chemotherapy treatments, it has been mentioned that PD-ECGF (platelet-derived endothelial cell growth factor) alters the sensitivity to some of these drugs [23].
On the other hand, different factors, such as angiogenesis, haematogenous or lymphatic dissemination and the resistance of tumour cells to the intrinsic defence mechanism of the body, could also play a part in the progression to more advanced stages.
The involvement of bone marrow haematopoietic precursors that express Vascular Endothelial Growth Factor Receptor-1 (VEGF-GR1) also seems to well known in the regulation of the metastatic dissemination of the tumour [24], and that angiogenesis is also essential for tumour growth [25]. Platelets synthesise and transport several angiogenic factors such as, VEGF, Platelet-Derived Growth Factor (PDGF), basic Fibroblastic Growth Factor (bFGF), Epidermal Growth Factor (EGF) or Matrix Metalloproteinases (MMPs) [23, 26].
These facts have been contrasted in animal models, where it has been demonstrated that the administration of a monoclonal antibody against VEGF slows down tumour growth [27].
The haematogenous dissemination of the tumour may be promoted by some platelet products, as MMPs or thrombospondin help tumour cells adhere to the epithelium. They also create an environment of hyper-permeability, which enables them to enter other tissues [26, 28]. Likewise, activated platelets may also assist in the invasion of the extracellular matrix by tumour cells by degrading heparin sulphate [29].
Thrombocytosis has also been associated with increased lymphatic involvement in LC and in other tumours [30–33]. Increased levels of bFGF and VEGF have been correlated with a lower survival in LC [32]. Lymph angiogenesis, probably started in intra-tumoral lymphatics [33–35], has also been demonstrated in these platelet products.
Reinforcing this hypothesis, it is known that inhibition of VEGF receptor-3 blocks lymphatic ganglia metastases in the initial phases, but not when they are established. This suggests that there must be critical periods in the tumour spreading process [36, 37].
Although, on the other hand, other authors mention associations in the opposite direction, by observing a better prognosis in LC patients with increased b-FGF [38, 39] levels. This would point to more complex inter-relationships between the different mechanisms involved, or even some “threshold” levels could be established to produce an effect or the opposite.
It has also been demonstrated that certain platelet products protect tumour cells by their destruction of immune system mechanisms, making the activation of natural killer cells difficult [40, 41], or by making them resistant to hypoxia-induced apoptosis [23].
In conclusion, our results seem to support the need to take the platelet levels into account when establishing a prognosis on LC patients.
Also having more information on prognostic factors could help make more reliable predictions of the progress of the disease (a particularly important point in diseases with such a high mortality), improve the efficiency of treatments used, better overall management of the disease, as well as a more accurate stratification of the groups included in scientific studies.
Owing to this being a retrospective study, this makes it difficult to establish definitive conclusions on the causal relationship between lower survival and high blood platelets. It is yet to be defined whether the increase in platelets is a final event, a result of the interaction by mediators released by the tumour, or is the cause of the progression of the disease.
References
Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics 2002. CA Cancer J Clin. 2005;55(2):74–108. doi:10.3322/canjclin.55.2.74.
Alberg AJ, Ford JG, Samet JM, American College of Chest Physicians. Epidemiology of lung cancer: ACCP evidence-based clinical practice guidelines (2nd ed.). Chest. 2007;132(3 Suppl):29S–55S. doi:10.1378/chest.07-1347.
Black WC. Computed tomography screening for lung cancer: review of screening principles and update on current status. Cancer. 2007;16 [Epub ahead of print].
Berghmans T, Lafitte JJ, Thiriaux J, VanHoutte P, Lecomte J, Efremidis A, et al. Survival is better predicted with a new classification of stage III unresectable non-small cell lung carcinoma treated by chemotherapy and radiotherapy. Lung Cancer. 2004;45(3):339–48.
Pedersen LM, Milman N. Prognostic significance of thrombocytosis in patients with primary lung cancer. Eur Respir J. 1996;9(9):1826–30. doi:10.1183/09031936.96.09091826.
Aoe K, Hiraki A, Ueoka H, Kiura K, Tabata M, Tanaka M, et al. Thrombocytosis as a useful prognostic indicator in patients with lung cancer. Respiration. 2004;71(2):170–3. doi:10.1159/000076679.
Watine J, Friedberg B, Charet JC. Laboratory variables and stratification of small-cell lung cancer patients: recommendations for therapeutic trials and for clinical practice guidelines. Ann Biol Clin (Paris). 2004;62(2):189–96.
Lee AY, Rickles FR, Julian JA, Gent M, Baker RI, Bowden C, et al. Randomized comparison of low molecular weight heparin and coumarin derivatives on the survival of patients with cancer and venous thromboembolism. J Clin Oncol. 2005;23(10):2123–9. doi:10.1200/JCO.2005.03.133.
Klerk CP, Smorenburg SM, Otten HM, Lensing AW, Prins MH, Piovella F, et al. The effect of low molecular weight heparin on survival in patients with advanced malignancy. J Clin Oncol. 2005;23(10):2130–5. doi:10.1200/JCO.2005.03.134.
World Health Organization. The World Health Organization histological typing of lung tumors (2nd ed.). Am J Clin Pathol. 1982;77:123–36.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. doi:10.1016/0021-9681(87)90171-8.
Costantini V, Zacharski LR, Moritz TE, Edwards RL. The platelet count in carcinoma of the lung and colon. Thromb Haemost. 1990;64(4):501–5.
Iwasaki A, Hamanaka W, Harnada T, Maekawa S, Enatsu S, Shirakusa T. Significance of platelet counts in patients who underwent surgical treatment for lung metastasis. Int Surg. 2007;92(2):103–9.
Segal JB, Moliterno AR. Platelet counts differ by sex, ethnicity, and age in the United States. Ann Epidemiol. 2006;16(2):123–30. doi:10.1016/j.annepidem.2005.06.052.
Alexandrakis MG, Passam FH, Perisinakis K, Ganotakis E, Margantinis G, Kyriakou DS, et al. Serum proinflammatory cytokines and its relationship to clinical parameters in lung cancer patients with reactive thrombocytosis. Respir Med. 2002;96(8):553–8. doi:10.1053/rmed.2002.1328.
Lidor YJ, Xu FJ, Martínez-Maza O, Olt GJ, Marks JR, Berchuck A, et al. Constitutive production of macrophage colony-stimulating factor and interleukin-6 by human ovarian surface epithelial cells. Exp Cell Res. 1993;207(2):332–9. doi:10.1006/excr.1993.1200.
Kaser A, Brandacher G, Steurer W, Kaser S, Offner FA, Zoller H, et al. Interleukin-6 stimulates thrombopoiesis through thrombopoietin: role in inflammatory thrombocytosis. Blood. 2001;98(9):2720–5. doi:10.1182/blood.V98.9.2720.
Mulligan CR, Meram AD, Proctor CD, Wu H, Zhu K, Marrogi AJ. Unlimited access to care: effect on racial disparity and prognostic factors in lung cancer. Cancer Epidemiol Biomarkers Prev. 2006;15(1):25–31. doi:10.1158/1055-9965.EPI-05-0537.
Spira A, Ettinger DS. Multidisciplinary management of lung cancer. N Engl J Med. 2004;350(4):379–92. doi:10.1056/NEJMra035536.
Khorana AA, Francis CW, Culakova E, Lyman GH. Risk factors for chemotherapy-associated venous thromboembolism in a prospective observational study. Cancer. 2005;104(12):2822–9. doi:10.1002/cncr.21496.
Zakai NA, Wright J, Cushman M. Risk factors for venous thrombosis in medical inpatients: validation of a thrombosis risk score. J Thromb Haemost. 2004;2(12):2156–61. doi:10.1111/j.1538-7836.2004.00991.x.
Ly HQ, Kirtane AJ, Murphy SA, Buros J, Cannon CP, Braunwald E, et al. Association of platelet counts on presentation and clinical outcomes in ST-elevation myocardial infarction (from the TIMI Trials). Am J Cardiol. 2006;8(1):1–5. doi:10.1016/j.amjcard.2006.01.046.
Akiyama S, Furukawa T, Sumizawa T, Takebayashi Y, Nakajima Y, Shimaoka S, et al. The role of thymidine phosphorylase, an angiogenic enzyme, in tumor progression. Cancer Sci. 2004;95(11):851–7. doi:10.1111/j.1349-7006.2004.tb02193.x.
Kaplan RN, Riba RD, Zacharoulis S, Bramley AH, Vincent L, Costa C, et al. VEGFR1-positive haematopoietic bone marrow progenitors initiate the pre-metastatic niche. Nature. 2005;438:820–7. doi:10.1038/nature04186.
Locopo N, Fanelli M, Gasparini G. Clinical significance of angiogenic factors in breast cancer. Breast Cancer Res Treat. 1998;52(1–3):159–73. doi:10.1023/A:1006175504673.
Jurasz P, Alonso D, Castro-Blanco S, Murad F, Radomski MW. Generation and role of angiostatin in human platelets. Blood. 2003;102(9):3217–23. doi:10.1182/blood-2003-02-0378.
Ilhan N, Ilhan N, Deveci F. Functional significance of vascular endothelial growth factor and its receptor (receptor-1) in various lung cancer types. Clin Biochem. 2004;37(9):840–5. doi:10.1016/j.clinbiochem.2004.03.012.
Walz DA. Thrombospondin as a mediator of cancer cell adhesion in metastasis. Cancer Metastasis Rev. 1992;11(3–4):313–24. doi:10.1007/BF01307185.
Yahalom J, Eldor A, Biran S, Fuks Z, Vlodavsky I. Platelet-tumor cell interaction with the subendothelial extracellular matrix: relationship to cancer metastasis. Radiother Oncol. 1985;3(3):211–25. doi:10.1016/S0167-8140(85)80030-X.
Lu CC, Chang KW, Chou FC, Cheng CY, Liu CJ. Association of pretreatment thrombocytosis with disease progression and survival in oral squamous cell carcinoma. Oral Oncol. 2007;43(3):283–8. doi:10.1016/j.oraloncology.2006.03.010.
Shimada H, Oohira G, Okazumi S, Matsubara H, Nabeya Y, Hayashi H, et al. Thrombocytosis associated with poor prognosis in patients with esophageal carcinoma. J Am Coll Surg. 2004;198(5):737–41. doi:10.1016/j.jamcollsurg.2004.01.022.
Iwasaki A, Kuwahara M, Yoshinaga Y, Shirakusa T. Basic fibroblast growth factor (bFGF) and vascular endothelial growth factor (VEGF) levels, as prognostic indicators in NSCLC. Eur J Cardiothorac Surg. 2004;25(3):443–8. doi:10.1016/j.ejcts.2003.11.031.
Saintigny P, Kambouchner M, Ly M, Gomes N, Sainte-Catherine O, Vassy R, et al. Vascular endothelial growth factor-C and its receptor VEGFR-3 in non-small-cell lung cancer: concurrent expression in cancer cells from primary tumour and metastatic lymph node. Lung Cancer. 2007;58(2):205–13. doi:10.1016/j.lungcan.2007.06.021.
Cao Y. Direct role of PDGF-BB in lymphangiogenesis and lymphatic metastasis. Cell Cycle. 2005;4(2):228–30.
Cao R, Eriksson A, Kubo H, Alitalo K, Cao Y, Thyberg J. Comparative evaluation of FGF-2-, VEGF-A-, and VEGF-C-induced angiogenesis, lymphangiogenesis, vascular fenestrations, and permeability. Circ Res. 2004;94(5):644–70. doi:10.1161/01.RES.0000118600.91698.BB.
He Y, Rajantie I, Pajusola K, Jeltsch M, Holopainen T, Yla-Herttuala S, et al. Vascular endothelial cell growth factor receptor 3-mediated activation of lymphatic endothelium is crucial for tumor cell entry and spread via lymphatic vessels. Cancer Res. 2005;65(11):4739–46. doi:10.1158/0008-5472.CAN-04-4576.
Roberts N, Kloos B, Cassella M, Podgrabinska S, Persaud K, Wu Y, et al. Inhibition of VEGFR-3 activation with the antagonistic antibody more potently suppresses lymph node and distant metastases than inactivation of VEGFR-2. Cancer Res. 2006;66(5):2650–7. doi:10.1158/0008-5472.CAN-05-1843.
Guddo F, Fontanini G, Reina C, Vignola AM, Angeletti A, Bonsignore G. The expression of basic fibroblast growth factor (bFGF) in tumor-associated stromal cells and vessels is inversely correlated with non-small cell lung cancer progression. Hum Pathol. 1999;30(7):788–94. doi:10.1016/S0046-8177(99)90139-9.
Brattström D, Bergqvist M, Larsson A, Holmertz J, Hesselius P, Rosenberg L, et al. Basic fibroblast growth factor and vascular endothelial growth factor in sera from non-small cell lung cancer patients. Anticancer Res. 1998;18(2A):1123–7.
Palumbo JS, Talmage KE, Massari JV, La Jeunesse CM, Flick MJ, Kombrinck KW, et al. Platelets and fibrin(ogen) increase metastatic potential by impeding natural killer cell-mediated elimination of tumor cells. Blood. 2005;105(1):178–85. doi:10.1182/blood-2004-06-2272.
Nieswandt B, Hafner M, Echtenacher B, Mannel DN. Lysis of tumor cells by natural killer cells in mice is impeded by platelets. Cancer Res. 1999;59(6):1295–300.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gonzalez Barcala, F.J., Garcia Prim, J.M., Moldes Rodriguez, M. et al. Platelet count: association with prognosis in lung cancer. Med Oncol 27, 357–362 (2010). https://doi.org/10.1007/s12032-009-9217-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12032-009-9217-9