Abstract
Opioid receptor like 1 (ORL1) receptor activation displayed an anti-nociceptive effect at spinal level for acute and neuropathic pain. SCH221510, an orally active non-peptide ORL1 agonist, was reported to be effective in treating neuropathic pain. The present study used ORL1 antagonist and siRNA to investigate that ORL1 activation mediates intrathecal SCH221510 analgesia in neuropathic pain induced by chronic constrictive injury (CCI) to rat sciatic nerve. Paw withdrawal latency and 50% mechanical threshold were measured for thermal and mechanical hypersensitivity in rats. CCI significantly decreased paw withdrawal latency and mechanical threshold. SCH221510 (3, 10, 30 μg) or ORL1 antagonist ([Nphe1]nociceptin(1-13)NH2, 10 μg) was intrathecally injected to test the behavioral effects on neuropathic pain. Intrathecal siRNA was started on 1 day before CCI surgery and maintained for 7 days. L4-L5 spinal cord ORL1 mRNA and protein were measured by real-time PCR and Western blot. The effect of intrathecal siRNA on SCH2210510 was tested in CCI rats on day 7. Intrathecal SCH221510 dose-dependently reduced thermal and mechanical hypersensitivity induced by CCI. [Nphe1]nociceptin(1-13)NH2 blocked SCH221510 analgesia in CCI rats. Intrathecal siRNA blocked ORL1 mRNA and protein increase induced by CCI. Intrathecal ORL1 siRNA did not change thermal and mechanical hypersensitivity induced by nerve injury. Intrathecal siRNA blocked SCH221510 analgesia in neuropathic pain at spinal level. Conclusively, ORL1 activation mediates SCH221510 analgesia in neuropathic pain at spinal level. The results warrant a potential clinically applicable drug in treating neuropathic pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuropathic pain is a debilitating chronic condition developed after nerve injury that patients suffering from neuropathic pain are hypersensitive to pain stimuli. The plastic changes in nociceptive neurons and central nervous descending modulatory pathways maintain the chronic status of neuropathic pain (Cohen & Mao, 2014). Neuropathic pain is refractory to treatments and severely affecting life quality of patients suffering these symptoms. There are debates on the effectiveness of neuropathic pain treatments and clinical studies have shown that limited efficacy and poor phenotypic profiling probably account for modest treatment outcomes (Finnerup, et al., 2015; Truini, 2017). In addition, morphine and other mu-opioid peptide receptor agonists have been used in treating peripheral nerve-injury-induced neuropathic pain but effects are complicated due to the side effects including abuse and addiction (Dowell, Haegerich, & Chou, 2016).
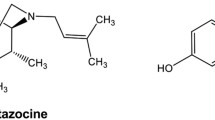
Opioid receptor like 1 (ORL1) receptor, one of the opioid receptor family, was found to bind to its natural ligand nociceptin/orphanin FQ (N/OFQ) but not to the classical opioid receptor agonists (Mogil & Pasternak, 2001). The analgesic effect of ORL1 activation depended on administration sites. Reports agreed that high doses of N/OFQ produced antinociceptive and anti-allodynia effects (Courteix, et al., 2004; Wang, Zhu, Cao, & Wu, 1999), although studies have reported that supraspinal injection of N/OFQ could produce pronociceptive or analgesic effects (Mogil, et al., 1996; Standifer, et al., 1996; Tian, et al., 1997). Variety of ORL1 agonists have been developed to decrease nerve-injury-induced thermal hypersensitivity and mechanical allodynia through spinal level administration (Obara, Przewlocki, & Przewlocka, 2005; Rizzi, et al., 2015). SCH221510 is a potent and selective non-peptide ORL1 agonist which provided the antinociceptive effect in a rodent model of inflammatory bowel disease with an oral active property (Sobczak, et al., 2014; Varty, et al., 2008). In addition, SCH221510 showed its analgesic effects on acute pain in primates and neuropathic pain in mice (Cremeans, Gruley, Kyle, & Ko, 2012; Sukhtankar, Zaveri, Husbands, & Ko, 2013), suggesting a possible therapeutic effect in neuropathic pain treatment. However, the mechanism is still elusive whether spinal ORL1 mediates SCH221510 analgesia in neuropathic pain. The present study utilized ORL1 receptor antagonist [Nphe1]nociceptin(1-13)NH2 and ORL1 siRNA to investigate ORL1 activation antinociceptive effect in sciatic nerve chronic constrictive injury (CCI) rats.
Methods and Materials
Animals
Male Sprague-Dawley rats (Experimental Animal Center, Luoyang Medical College, Luoyang, Henan, China) weighing 200–220 g were used. Rats were acclimated for 1 week before experiments. The experiment was approved by the Animals Care and Use Committee of Luoyang Medical College and conformed to the guidelines of the International Association for the Study of Pain (Zimmermann, 1983).
Surgery
The chronic constrictive injury to sciatic nerve was induced by four loose ligatures as previously described (Bennett & Xie, 1988). Under sodium pentobarbital anesthesia, left sciatic nerve was exposed and four 4-0 chronic gut sutures were tied loosely around the nerve. The incision was sutured up and rat was allowed to recover from anesthesia. The surgery was performed under sterile techniques and antibiotic ointment was applied to prevent postoperative infection. Hind paw thermal and mechanical hypersensitivity developed after CCI.
Cannulation and siRNA Administration
Intrathecal catheter was placed 3 days before nerve ligation. A PE-10 tube was inserted through the gap between vertebrae L5 and L6 and extended 1.5 cm into the subarachniod space of lumbar enlargement. The catheter was sealed at the end and embedded under the neck skin. The surgery was performed under sterile techniques and antibiotic ointment was applied to prevent postoperative infection. The cannulated rat was housed individually and allowed to recover for 3 days prior behavioral tests. One day before CCI surgery, ORL1 siRNA was intrathecally injected. Over a period of 1 min, 30 μl of sterile buffer (containing 3 μl of 20 μM siRNA (MSS276173); 12 μl oligofectamine, ThermoFisher Scientific, Grand Island, and 15 μl sterile buffered saline solution) was injected through the cannula using a Hamilton syringe. siRNA was daily injected for 7 days (Baker, Chen, Shah, & Okuse, 2011).
Behavioral Tests
Thermal and mechanical hypersensitivity were measured by paw withdrawal latency (PWL) to heat and 50% mechanical threshold (mechanical threshold calculated by up-down method with filaments of different weights) to von Frey filament on hind paws. Rats were acclimated in enclosure on a glass table for 15 min. PWL to radiant heat was measured as thermal sensitivity using IITC Model 336 Tail Flick Analgesia Meter (Life Science Instrument, Cridersville, OH, USA). The radiant heat was applied to plantar of hind paws and time between heat start and hind paw withdrawal was recorded as PWL. The radiant heat intensity was adjusted to produce a stable withdrawal latency around 10 s in naive rats with a 20-s cutoff to avoid tissue damage. Fifty percent mechanical threshold to von Frey filaments was measured as mechanical sensitivity. Rats were placed on the metal mesh floor in enclosure with 15 min acclimation. von Frey filaments (0.25, 0.65, 1.05, 1.56, 2.60, 4.89, 6.16, 8.40, 15.25, and, 21.75 g, Stoelting, Wood Dale, IL, USA) were pressed onto plantar surface, starting from 6.16 g in an up-and-down method. Next stronger filament was applied upon positive response and next lower one was used after negative response, and then 50% paw withdrawal threshold was calculated. All the behaviors were tested before CCI and on days 3, 7, 10, and 14 after CCI. Specifically, SCH221510 effects were tested at 10, 20, 30, 60, and 90 min after the drug administration on day 7. Ten microliters of SCH221510 (3, 10, and 30 μg, dissolved in 10% DMSO in saline) or ORL1 antagonist [Nphe1]nociceptin(1-13)NH2 (10 μg, dissolved in 10% acetonitrile in saline) (Tocris, Minneapolis, MN, USA) was injected through intrathecal catheter.
On day 7 after CCI, rats were decapitated and the L4-L5 segments of the spinal cord were removed. Dorsal part of the spinal cord was frozen on dry ice and kept at − 80 °C.
Real-Time PCR
Total RNA was extracted from the spinal cord tissue of untreated, CCI, and CCI with siRNA groups by Trizol (15596026, ThermoFisher Scientific, Grand Island, NY). Tissue DNA was removed by DNase, and then RNA was reversely transcribed to cDNA (A3500, Promega, Madison, WI). SYBR green (4472903, ThermoFisher Scientific, Grand Island, NY) was utilized with primers (ORL1 (OPRL1), PPR44465A; Rn18s, PPM72041A, Qiagen, Germantown, MD) to quantify levels of ORL1 mRNA in the spinal cord of those three groups; 18 s was used as an internal control.
Western Blotting
Total protein was extracted from the spinal cord tissue of untreated, CCI, and CCI with siRNA. Protein samples were separated using a 4–15% Mini-PROTEAN TGX precast polyacrylamide gel (Bio-Rad, Hercules, CA). After electrophoresis, separated proteins were transferred to a polyvinylidene difluoride membrane. ORL1 protein bands were visualized using a rabbit polyclonal primary antibody (ab66219; Abcam, Cambridge, MA; 1:1000), along with GAPDH as an internal control (A00915, GenScript, Piscataway, NJ; 1:2500), a biotinylated anti-rabbit secondary antibody (Vector Labs, Burlingame, CA; 1:400), streptavidin-HRP conjugates, and chemiluminescent substrate (Pierce, Rockford, IL). Band densitometry was performed using ImageJ (NIH, Bethesda, MD).
Statistics
Data are presented as mean ± SEM and analyzed by Prism 4.0. Repeated measures analysis of variance (ANOVA) followed by Student–Newman–Keuls test was used for post hoc analysis for differences between groups. p < 0.05 was considered statistically significant.
Results
Effects of Intrathecal SCH221510 and ORL1 Antagonist
The PWL and 50% mechanical threshold were significantly decreased 3 days after CCI injury when compared with baseline. The effects of intrathecal SCH221510 (3, 10, and 30 μg, n = 7–9) on PWL and 50% mechanical threshold were tested on day 7 after CCI. There were significant increases in PWL at 20 min (F = 4.013, p < 0.05), 30 min (F = 6.823, p < 0.01), 60 min (F = 10.522, p < 0.001), and 90 min (F = 5.631, p < 0.01) in 10 and 30 μg SCH221510 groups but not at 10 min (p > 0.05, Fig. 1a). No significant change was detected in 3 μg SCH221510 group (p > 0.05, compared with solvent). There were also significant increases in 50% mechanical threshold at 20 min (F = 5.513, p < 0.05), 30 min (F = 7.921, p < 0.01), 60 min (F = 12.124, p < 0.001), and 90 min (F = 6.138, p < 0.05) in 10 and 30 μg SCH221510 groups but not at 10 min (p > 0.05, Fig. 1b). No significant change was detected in 3 μg SCH221510 group (p > 0.05, compared with solvent).
ORL1 mediated SCH221510 analgesia in CCI rats. Intrathecal SCH221510 (3, 10, and 30 μg) analgesic effects on PWL to heat (a) and 50% mechanical threshold (b) on day 7 after chronic constrictive injury to rat sciatic nerve. Intrathecal 10 μg [Nphe1]nociceptin(1-13)NH2 blocked SCH221510 analgesic effect on PWL to heat (c) and 50% mechanical threshold (d) on day 7 after chronic constrictive injury to rat sciatic nerve. SCH SCH221510. *p < 0.05, **p < 0.01, ***p < 0.001 vs. before intrathecal injection
Intrathecal of ORL1 antagonist, [Nphe1]nociceptin(1-13)NH2 (10 μg), alone did not change either PWL or 50% mechanical threshold. Intrathecal 10 μg SCH221510 significantly increased both PWL (p < 0.05, 0.01, 0.001, and 0.01, Fig. 1c) and 50% mechanical threshold (p < 0.05, 0.01, 0.001, and 0.05, Fig. 1d) at 20, 30, 60, and 90 min as described above. When 10 μg SCH221510 and 10 μg [Nphe1]nociceptin(1-13)NH2 were intrathecally injected concurrently, [Nphe1]nociceptin(1-13)NH2 blocked SCH22150 analgesic effect on both PWL and 50% mechanical threshold (p < 0.05, 0.01, Fig. 1c, d). There were no differences in [Nphe1]nociceptin(1-13)NH2 plus SCH221510 group when compared with time point 0 min on PWL and 50% mechanical threshold (p > 0.05, Fig. 1c, d).
ORL1 siRNA Blocked ORL1 mRNA and Protein Increases Induced by CCI
ORL1 mRNA and protein from the spinal cord L4-L5 segments were measured in untreated, CCI, and CCI plus ORL1 siRNA groups. Real-time PCR result showed that ORL1 mRNA in CCI rats was 4.19 times of that in untreated group when normalized to 18 s (p < 0.01). ORL1 siRNA significantly blocked nerve-injury-induced ORL1 mRNA increase when compared to CCI group (p < 0.05) (Fig. 2a). ORL1 protein levels in the spinal cord L4-L5 segments were measured by Western blot. The result showed that nerve injury increased ORL1 protein (p < 0.01, CCI vs. untreated) and ORL1 siRNA blocked CCI-induced ORL1 protein increase (p < 0.05, CCI plus ORL1 siRNA vs. CCI) (Fig. 2b). All ORL1 protein bands were normalized to GAPDH.
ORL1 siRNA decreased spinal mRNA and protein increase by CCI. a Histogram showed that CCI increased ORL1 mRNA compared to untreated. Intrathecal ORL1 siRNA blocked mRNA increase. b Histogram showed that CCI increased ORL1 protein compared to untreated. Intrathecal ORL1 siRNA blocked protein increase. **p < 0.01, ***p < 0.001 vs. untreated group; #p < 0.05 vs. CCI group
ORL1 siRNA Blocked SCH221510 Analgesia
SCH221510 was intrathecally injected daily for 7 days starting from 1 day before CCI surgery. The effects of intrathecal ORL1 siRNA on CCI-induced thermal and mechanical hypersensitivity were tested on days 3, 7, 10, and 14. ORL1 siRNA did not change PWL and mechanical threshold on days 3, 7, 10, and 14 when compared with CCI group (p > 0.05 vs. CCI) (Fig. 3a, b).
Ten micrograms SCH221510 was intrathecally injected in CCI group and CCI rats treated with ORL1 siRNA group on day 7 after CCI. SCH221510 significantly increased PWL and 50% mechanical threshold of CCI rats when compared with control (CCI only) group (p < 0.01) (Fig. 4a, b). However, PWL and 50% mechanical threshold increases were blocked by ORL1 siRNA when compared with SCH2210510 treated group (p < 0.05) (Fig. 4a, b). There was no difference between SCH221510 plus ORL1 siRNA group and control (CCI only) group on both PWL and mechanical threshold, indicating that SCH221510 analgesia was abolished by ORL1 siRNA in CCI rats (p > 0.05) (Fig. 4a, b).
ORL1 siRNA blocked SCH221510 analgesia in CCI rats. All three groups had CCI surgery. Intrathecal 10 μg SCH221510 significantly increased PWL (a) and 50% mechanical threshold (b) when compared to control (CCI only) group. Intrathecal ORL1 siRNA blocked SCH221510 analgesia on CCI-induced thermal (a) and mechanical (b) hypersensitivity. SCH SCH221510. **p < 0.01 vs. control (CCI only) group; #p < 0.05 vs. CCI plus SCH221510 group
Discussion
The current study showed that intrathecal ORL1 agonist SCH221510 dose-dependently decreased thermal and mechanical hypersensitivity in hind paw induced by chronic constrictive injury to rat sciatic nerve. The analgesic effect was blocked by ORL1 antagonist [Nphe1]nociceptin(1-13)NH2. Intrathecal ORL1 siRNA decreased the spinal cord ORL1 mRNA and protein. ORL1 siRNA did not change CCI-induced thermal and mechanical hypersensitivity. SCH221510 analgesia was blocked with ORL1 siRNA pre-treatment. The results indicated that spinal ORL1 activation mediates SCH221510 analgesia on CCI-induced thermal and mechanical hypersensitivity in rats.
Neuropathic pain is usually caused by a lesion or disease of the somatosensory nervous system which impairs quality of life and is often poorly managed. Neuropathic pain animal models are usually caused by peripheral nerve injury through compression or transection to trigeminal nerve or sciatic nerve (Bennett & Xie, 1988; Decosterd & Woolf, 2000; Xu, Aita, & Chavkin, 2008). Chronic constrictive injury to sciatic nerve is one of the most used animal models to study neuropathic pain. Meanwhile, a variety of drug treatments have been recommended including antidepressants, Tramadol, and opioids but more effective treatments are still needed. Morphine was less effective in treating neuropathic pain shown in both clinics and animal studies. μ-Opioid receptor was downregulated and opioid receptor binding was reduced in the spinal cord after peripheral nerve-injury-induced neuropathic pain (deGroot, Coggeshall, & Carlton, 1997; Zajac, Lombard, Peschanski, Besson, & Roques, 1989). However, as a member of opioid receptor family, ORL1 mRNA and protein were found in the central nervous system (Houtani, et al., 2000; Pettersson, Sundler, & Danielsen, 2002), and the animal models of neuropathic pain increased ORL1 in brain and dorsal root ganglion (Chen & Sommer, 2006; Ma, Xie, Dong, Wang, & Wu, 2005). Spinal ORL1 mRNA increase shown by RT-PCR indicated that ORL1 was upregulated after CCI in rats (Briscini, Corradini, Ongini, & Bertorelli, 2002). Our results showed that both ORL1 mRNA and protein were increased in the spinal cord after CCI injury, suggesting that spinal ORL1 was modulated differently than μ-opioid receptor in neuropathic pain. However, thermal and mechanical hypersensitivity were not blocked when spinal ORL1 was not reduced in CCI rats. Our result showed that intrathecal injection of ORL1 siRNA significantly lowered CCI-induced ORL1 mRNA and protein increase in the spinal cord 7 days after injection. CCI-induced thermal and mechanical hypersensitivity were also not blocked by intrathecal ORL1 siRNA. Our result was agreed by another report that intrathecal injection of ORL1 antagonists alone did not affect CCI-induced thermal and mechanical hypersensitivity (Obara, et al., 2005). In addition, ORL1 deletion did not block CCI-induced thermal and mechanical hypersensitivity in mice (Bertorelli, et al., 2002; Nishi, et al., 1997). Along with the previous reports that ORL1 receptor agonists displayed antinociceptive effect in CCI-induced neuropathic pain (Courteix, et al., 2004; Hayashi, et al., 2010), the current study suggested that spinal ORL1 activation contributed to SCH221510 analgesia on thermal and mechanical hypersensitivity instead of ORL1 upregulation probably due to lack of activation by endogenous agonist. The mechanisms remain to be determined.
Numerous studies showed that ORL1 participated in pain process of different pain models in both rodents and primates (Chen & Sommer, 2007; Courteix, et al., 2004; Ko & Naughton, 2009). ORL1 activation inhibited windup and reduced glutamatergic transmission induced by sciatic nerve injury in the spinal cord, suggesting that ORL1 could be a novel molecule targeting neuropathic pain (Faber, Chambers, Evans, & Henderson, 1996; Stanfa, Chapman, Kerr, & Dickenson, 1996). ORL1 upregulation itself did not change CCI-induced hypersensitivity but provided increasing number of acting sites for ORL1 agonists to perform the analgesic effect in neuropathic pain (Obara, et al., 2005; Rizzi, et al., 2015; Sukhtankar, et al., 2013). Our results showed ORL1 mRNA and protein increase in the spinal cord but did not locate which compartments the increases were. ORL1 agonists bound to membrane ORL1 inhibited nociceptive neuron via extracellular signal-regulated kinase (ERK)-dependent non-genomic mechanisms and gated rectifying potassium channels (Ikeda, et al., 1997; Small, Nag, & Mokha, 2013). The mechanism of spinal ORL1 activation analgesia in neuropathic pain is to be determined.
Mounting ORL1 receptor agonists including peptide and non-peptide agonists have shown that the antinociceptive action at spinal level was through pharmacological activation of ORL1 (Hayashi, et al., 2010; Obara, et al., 2005). Hayashi et al. reported that a compound HPCOM, one of the ORL1 agonists, showed robust antinociceptive effect at spinal level with enhanced bio-pharmacological availability, suggesting ORL1 agonist as a potential systemically potent new-classic analgesic (Hayashi, et al., 2010). Another non-peptide ORL1 agonist, SCH221510, potentiated analgesic effect of μ-opioid receptor agonist in primate through systemic administration (Cremeans, et al., 2012). SCH221510 was orally active and showed its antinociceptive effect in visceral pain during treating gastrointestinal diseases, suggesting an easier administration drug for pain treatments (Sobczak, et al., 2014). Intrathecal injection of SCH221510 reduced thermal and mechanical hypersensitivity induced by nerve injury in mice and it also displayed the antinociceptive effect in primate (Sukhtankar, et al., 2013). Our results showed that intrathecal SCH221510 dose-dependently reduced CCI-induced thermal and mechanical hypersensitivity in rats which was blocked by intrathecal ORL1 antagonist or siRNA, suggesting that ORL1 activation mediates SCH221510 analgesia in neuropathic pain.
In conclusion, the present work characterizes a new ORL1 receptor agonist, SCH221510, in neuropathic pain. The study proves ORL1 expression increased at both mRNA and protein levels and utilizes siRNA technique to suppress ORL1 translation beside receptor antagonists.
Abbreviations
- ORL1 :
-
opioid receptor like 1
- CCI:
-
chronic constrictive injury
- N/OFQ:
-
nociceptin/orphanin FQ
- PWL:
-
paw withdrawal latency
- PB:
-
phosphate buffer
References
Baker MD, Chen YC, Shah SU, Okuse K (2011) In vitro and intrathecal siRNA mediated K(V)1.1 knock-down in primary sensory neurons. Mol Cell Neurosci 48:258–265
Bennett GJ, Xie YK (1988) A peripheral mononeuropathy in rat that produces disorders of pain sensation like those seen in man. Pain 33:87–107
Bertorelli R, Bastia E, Citterio F, Corradini L, Forlani A, Ongini E (2002) Lack of the nociceptin receptor does not affect acute or chronic nociception in mice. Peptides 23:1589–1596
Briscini L, Corradini L, Ongini E, Bertorelli R (2002) Up-regulation of ORL-1 receptors in spinal tissue of allodynic rats after sciatic nerve injury. Eur J Pharmacol 447:59–65
Chen Y, Sommer C (2006) Nociceptin and its receptor in rat dorsal root ganglion neurons in neuropathic and inflammatory pain models: implications on pain processing. J Peripher Nerv Syst 11:232–240
Chen Y, Sommer C (2007) Activation of the nociceptin opioid system in rat sensory neurons produces antinociceptive effects in inflammatory pain: involvement of inflammatory mediators. J Neurosci Res 85:1478–1488
Cohen SP, Mao J (2014) Neuropathic pain: mechanisms and their clinical implications. BMJ 348:f7656
Courteix C, Coudore-Civiale MA, Privat AM, Pelissier T, Eschalier A, Fialip J (2004) Evidence for an exclusive antinociceptive effect of nociceptin/orphanin FQ, an endogenous ligand for the ORL1 receptor, in two animal models of neuropathic pain. Pain 110:236–245
Cremeans CM, Gruley E, Kyle DJ, Ko MC (2012) Roles of mu-opioid receptors and nociceptin/orphanin FQ peptide receptors in buprenorphine-induced physiological responses in primates. J Pharmacol Exp Ther 343:72–81
Decosterd I, Woolf CJ (2000) Spared nerve injury: an animal model of persistent peripheral neuropathic pain. Pain 87:149–158
deGroot JF, Coggeshall RE, Carlton SM (1997) The reorganization of mu opioid receptors in the rat dorsal horn following peripheral axotomy. Neurosci Lett 233:113–116
Dowell D, Haegerich TM, Chou R (2016) CDC guideline for prescribing opioids for chronic pain - United States, 2016. MMWR Recomm Rep 65:1–49
Faber ES, Chambers JP, Evans RH, Henderson G (1996) Depression of glutamatergic transmission by nociceptin in the neonatal rat hemisected spinal cord preparation in vitro. Br J Pharmacol 119:189–190
Finnerup NB, Attal N, Haroutounian S, McNicol E, Baron R, Dworkin RH, Gilron I, Haanpaa M, Hansson P, Jensen TS, Kamerman PR, Lund K, Moore A, Raja SN, Rice AS, Rowbotham M, Sena E, Siddall P, Smith BH, Wallace M (2015) Pharmacotherapy for neuropathic pain in adults: a systematic review and meta-analysis. Lancet Neurol 14:162–173
Hayashi S, Nakata E, Morita A, Mizuno K, Yamamura K, Kato A, Ohashi K (2010) Discovery of {1-[4-(2-{hexahydropyrrolo[3,4-c]pyrrol-2(1H)-yl}-1H-benzimidazol-1-yl)piperidin-1-yl]cyclooctyl}methanol, systemically potent novel non-peptide agonist of nociceptin/orphanin FQ receptor as analgesic for the treatment of neuropathic pain: design, synthesis, and structure-activity relationships. Bioorg Med Chem 18:7675–7699
Houtani T, Nishi M, Takeshima H, Sato K, Sakuma S, Kakimoto S, Ueyama T, Noda T, Sugimoto T (2000) Distribution of nociceptin/orphanin FQ precursor protein and receptor in brain and spinal cord: a study using in situ hybridization and X-gal histochemistry in receptor-deficient mice. J Comp Neurol 424:489–508
Ikeda K, Kobayashi K, Kobayashi T, Ichikawa T, Kumanishi T, Kishida H, Yano R, Manabe T (1997) Functional coupling of the nociceptin/orphanin FQ receptor with the G-protein-activated K+ (GIRK) channel. Brain Res Mol Brain Res 45:117–126
Ko MC, Naughton NN (2009) Antinociceptive effects of nociceptin/orphanin FQ administered intrathecally in monkeys. J Pain 10:509–516
Ma F, Xie H, Dong ZQ, Wang YQ, Wu GC (2005) Expression of ORL1 mRNA in some brain nuclei in neuropathic pain rats. Brain Res 1043:214–217
Mogil JS, Grisel JE, Zhangs G, Belknap JK, Grandy DK (1996) Functional antagonism of mu-, delta- and kappa-opioid antinociception by orphanin FQ. Neurosci Lett 214:131–134
Mogil JS, Pasternak GW (2001) The molecular and behavioral pharmacology of the orphanin FQ/nociceptin peptide and receptor family. Pharmacol Rev 53:381–415
Nishi M, Houtani T, Noda Y, Mamiya T, Sato K, Doi T, Kuno J, Takeshima H, Nukada T, Nabeshima T, Yamashita T, Noda T, Sugimoto T (1997) Unrestrained nociceptive response and disregulation of hearing ability in mice lacking the nociceptin/orphaninFQ receptor. EMBO J 16:1858–1864
Obara I, Przewlocki R, Przewlocka B (2005) Spinal and local peripheral antiallodynic activity of Ro64-6198 in neuropathic pain in the rat. Pain 116:17–25
Pettersson LM, Sundler F, Danielsen N (2002) Expression of orphanin FQ/nociceptin and its receptor in rat peripheral ganglia and spinal cord. Brain Res 945:266–275
Rizzi A, Sukhtankar DD, Ding H, Hayashida K, Ruzza C, Guerrini R, Calo G, Ko MC (2015) Spinal antinociceptive effects of the novel NOP receptor agonist PWT2-nociceptin/orphanin FQ in mice and monkeys. Br J Pharmacol 172:3661–3670
Small KM, Nag S, Mokha SS (2013) Activation of membrane estrogen receptors attenuates opioid receptor-like1 receptor-mediated antinociception via an ERK-dependent non-genomic mechanism. Neuroscience 255:177–190
Sobczak M, Mokrowiecka A, Cygankiewicz AI, Zakrzewski PK, Salaga M, Storr M, Kordek R, Malecka-Panas E, Krajewska WM, Fichna J (2014) Anti-inflammatory and antinociceptive action of an orally available nociceptin receptor agonist SCH 221510 in a mouse model of inflammatory bowel diseases. J Pharmacol Exp Ther 348:401–409
Standifer KM, Rossi GC, Pasternak GW (1996) Differential blockade of opioid analgesia by antisense oligodeoxynucleotides directed against various G protein alpha subunits. Mol Pharmacol 50:293–298
Stanfa LC, Chapman V, Kerr N, Dickenson AH (1996) Inhibitory action of nociceptin on spinal dorsal horn neurones of the rat, in vivo. Br J Pharmacol 118:1875–1877
Sukhtankar DD, Zaveri NT, Husbands SM, Ko MC (2013) Effects of spinally administered bifunctional nociceptin/orphanin FQ peptide receptor/mu-opioid receptor ligands in mouse models of neuropathic and inflammatory pain. J Pharmacol Exp Ther 346:11–22
Tian JH, Xu W, Fang Y, Mogil JS, Grisel JE, Grandy DK, Han JS (1997) Bidirectional modulatory effect of orphanin FQ on morphine-induced analgesia: antagonism in brain and potentiation in spinal cord of the rat. Br J Pharmacol 120:676–680
Truini A (2017) A review of neuropathic pain: from diagnostic tests to mechanisms. Pain Ther 6:5–9
Varty GB, Lu SX, Morgan CA, Cohen-Williams ME, Hodgson RA, Smith-Torhan A, Zhang H, Fawzi AB, Graziano MP, Ho GD, Matasi J, Tulshian D, Coffin VL, Carey GJ (2008) The anxiolytic-like effects of the novel, orally active nociceptin opioid receptor agonist 8-[bis(2-methylphenyl)methyl]-3-phenyl-8-azabicyclo[3.2.1]octan-3-ol (SCH 221510). J Pharmacol Exp Ther 326:672–682
Wang JL, Zhu CB, Cao XD, Wu GC (1999) Distinct effect of intracerebroventricular and intrathecal injections of nociceptin/orphanin FQ in the rat formalin test. Regul Pept 79:159–163
Xu M, Aita M, Chavkin C (2008) Partial infraorbital nerve ligation as a model of trigeminal nerve injury in the mouse: behavioral, neural, and glial reactions. J Pain 9:1036–1048
Zajac JM, Lombard MC, Peschanski M, Besson JM, Roques BP (1989) Autoradiographic study of mu and delta opioid binding sites and neutral endopeptidase-24.11 in rat after dorsal root rhizotomy. Brain Res 477:400–403
Zimmermann M (1983) Ethical guidelines for investigations of experimental pain in conscious animals. Pain 16:109–110
Acknowledgements
Thanks Fei Liu for editing the manuscript.
Availability of Data and Materials
The authors will provide data upon request.
Funding
The study was funded by the Xinxiang Central Hospital Startup fund.
Author information
Authors and Affiliations
Contributions
QW designed the experiment, carried out the study, and drafted the manuscript. LL carried out the experiments.
Corresponding author
Ethics declarations
Ethics Approval
The experiment was approved by the Animals Care and Use Committee of Luoyang Medical College.
Consent for Publication
The authors have consent to publish the study.
Competing Interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Wu, Q., Liu, L. ORL1 Activation Mediates a Novel ORL1 Receptor Agonist SCH221510 Analgesia in Neuropathic Pain in Rats. J Mol Neurosci 66, 10–16 (2018). https://doi.org/10.1007/s12031-018-1140-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-018-1140-0