Abstract
The functional outcome after peripheral nerve repair is often unpredictable for many reasons, e.g., the severity of neuronal death and scarring. Axonal degeneration significantly affects outcomes. Post-injury axonal degeneration in peripheral nerves is accompanied by myelin degradation initiated by Schwann cells (SCs), which activate autophagy, a ubiquitous cytoprotective process essential for degrading and recycling cellular constituents. Scar formation occurs concomitantly with nerve insult and axonal degeneration. The association between SC autophagy and the mechanisms of nerve scar formation is still unknown. A rat model of peripheral nerve lesions induced by sciatic nerve transection injuries was used to examine the function of autophagy in fibrosis reduction during the early phase of nerve repair. Rats were treated with rapamycin (autophagy inducer) or 3-methyladenine (autophagy inhibitor). One week after the nerve damage, fibrosis was potently inhibited in rapamycin-treated rats and, based on gait analysis, yielded a better functional outcome. Immunohistochemistry showed that the autophagic activity of SCs and the accumulation of neurofilaments were upregulated in rapamycin-treated rats. A deficiency of SC autophagic activity might be an early event in nerve scar formation, and modulating autophagy might be a powerful pharmacological approach for improving functional outcomes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Functional recovery and morphological regeneration after peripheral nerve injury are variable: they often leave patients with substantial sensory or motor deficits, and sometimes with chronic pain (Devor and Seltzer 1999). Technological advances in diagnostic imaging, neurosurgical instrumentation, and surgical microscopes have led to great improvements in diagnosing and repairing transected peripheral nerves; however, the functional outcome after nerve repair is often unpredictable (Robinson et al. 2000). This happens because of the degree of neuronal death (Lundborg and Danielsen 1991) and the formation of scarring and neuromas (aka “neurofibromas”) at the nerve injury site (Lane et al. 1978). Scar formation causes many clinical problems that affect function, growth, and appearance (McCallion and Ferguson 1996). Numerous investigators (Rubinsztein et al. 2005; Larsen and Sulzer 2002; Chu 2006) have studied scar formation after a peripheral nerve injury, and some have tried to modify these events to improve outcomes. However, no therapeutic measures designed to modify scar formation have been introduced into clinical practice.
A growing number of recent reports (Chong et al. 2012; Kim et al. 2013; Ravikumar et al. 2004; Malagelada et al. 2010) highlight the potential importance of autophagy-related processes for aggregating proteins that regulate cell death pathways and regenerate neurons. There are several excellent reviews (McCallion and Ferguson 1996; Rubinsztein et al. 2005; Larsen and Sulzer 2002; Chu 2006) of autophagy in neurons and nerve tissue, and they have inspired us to investigate whether there is any relationship between scar reduction and autophagy.
We chose rapamycin, a lipophilic macrolide antibiotic used in many studies (Chong et al. 2012; Kim et al. 2013; Ravikumar et al. 2004; Malagelada et al. 2010; Caccamo et al. 2010; Rangaraju et al. 2010; Abe et al. 2010; Marinelli et al. 2011), as our autophagy inducer. Rapamycin (aka “sirolimus”) inhibits the mammalian target of rapamycin complex 1 (mTORC1) (Chong et al. 2012), which senses nutrients and negatively regulates autophagy (Kim et al. 2013). Using rapamycin to activate autophagy positively affects Huntington’s (Ravikumar et al. 2004), Parkinson’s (Malagelada et al. 2010), and Alzheimer’s (Caccamo et al. 2010) diseases in animal models, and autophagy dependently improves myelination in neuropathic mouse Schwann cells (SCs) in culture medium (Rangaraju et al. 2010). Relatively few studies have focused on how autophagy is involved in neuronal injury. Gomez-Sanchez et al. (Gomez-Sanchez et al. 2015) reported that autophagy in SCs is crucial for clearing myelin debris during the first 5–7 post-nerve-injury days. Using rapamycin to pharmacologically activate autophagy reduced inflammation, induced analgesia, facilitated nerve regeneration, and prevented chronic pain (Marinelli et al. 2011). Abe et al. (Abe et al. 2010) showed that activating the mTOR pathway regenerated axons in peripheral nerve system neurons.
Although recent studies (McCallion and Ferguson 1996; Rubinsztein et al. 2005; Larsen and Sulzer 2002; Chu 2006; Abe et al. 2010; Marinelli et al. 2011; Gomez-Sanchez et al. 2015) have reported that autophagy benefits peripheral nerve regeneration, few studies (Abe et al. 2010; Marinelli et al. 2011; Gomez-Sanchez et al. 2015) mention whether autophagy is involved in scar reduction or whether the amount of scar tissue created is related to nerve function. Because of the paucity of information on this topic, we investigated in a rat model whether rapamycin is beneficial for myelination and scar modification at nerve repair sites.
Methods
Animals and Surgical Procedures
Eight-week-old male Sprague-Dawley rats (n = 42) (Biolasco Taiwan, Taipei) were used. They were housed under a 12/12-h light/dark cycle with food and water ad libitum. All procedures followed National Cheng Kung University’s Animal Use Protocol. A sciatic nerve repair model was used with the rats after they had been intramuscularly (i.m.) anesthetized with tiletamine hydrochloride and zolazepam hydrochloride (Zoletil® 50) (80 mg/kg) (Virbac, Carros, France) and premedicated with gentamycin (8 mg/kg [i.m.]) (Yung Shin Pharmaceutical Industrial Co., Taichung, Taiwan). Core temperatures were monitored using rectal probes connected to a multichannel thermometer (Portable Hybrid Recorder, model 3087; Yokogawa Hokushin Electric, Tokyo, Japan) and maintained at 37–38 °C using a heating pad and lamp. Using the gluteal muscle splitting method, the left sciatic nerve was exposed under a microscope. The rats underwent sciatic nerve transaction, and end-to-end epineural nerve repair with 10–0 nylon sutures was performed immediately after transection (Ethilon; Ethicon, Somerville, NJ, USA); the surgical wounds were closed in layers using 3–0 silk sutures.
Drugs
3-Methyladenine (3-MA; Calbiochem, Hessen, Germany) (500 mg), an autophagy inhibitor, was dissolved in saline (20 ml), and rapamycin (RAPA; Calbiochem) (20 mg) was dissolved in dimethylsulfoxide (DMSO) (20 ml). Immediately after surgery, and daily for 7 days thereafter, the rats were given an ipsilateral hind-paw intraplantar (ipl) injection of the drug (20 ml) assigned to their group. The same solution without RAPA was used as a vehicle control; thus, the control group was injected with DMSO (20 ml) only. As reported elsewhere (Marinelli et al. 2011), the dosage described above did not harm the rats.
Groups
Twenty-four rats were assigned to the behavioral test and nerve fibrosis assessment group. The remaining 18 rats were assigned to the immunohistochemical analysis group (Fig. 1). In the behavioral test and nerve fibrosis assessment group, the 24 rats were then randomly assigned to 1 of 4 groups (n = 6 in each group): [i] sham neurorrhaphy (control group, given a surgical incision but no sciatic nerve transection, and then injected [ipl] with DMSO); [ii] DMSO (sciatic nerve was transected, repaired, and then injected [ipl] with DMSO); [iii] RAPA (sciatic nerve transected, repaired, and then injected [ipl] with RAPA); and [iv] 3-MA (sciatic nerve transected, repaired, and then injected [ipl] with 3-MA). These 24 rats were killed after they finished the behavioral test to assess nerve fibrosis 56 days after the neurorrhaphy (Fig. 2). To check that the RAPA and 3-MA were really working, the other 18 rats undergoing sciatic nerve repair after transection were randomly assigned to 1 of 3 groups (n = 6 in each group): DMSO, RAPA, and 3-MA as described as above and killed 7 days after neurorrhaphy; their repaired nerves were harvested and then immunohistochemically analyzed.
Sciatic nerve function index (SFI) values in each experimental group. Function recovery was better in RAPA-treated rats than in DMSO- and 3-MA-treated rats. SFI ranged from 10 (normal) to 100 (severe injury). The error bars represent SD. [*] shows DMSO compared with RAPA, and [#] shows DMSO compared with 3-MA; *p < 0.05; **p < 0.01; ***p < 0.005; ****p < 0.001
Behavioral Test
The 24 rats underwent a walking-track analysis for evidence of neurological compromise 56 days after their neurorrhaphy and drug treatment. The hind-limb footprints of each rat were obtained using a walking track with a video-based system (Fig. 2). (Jen-I et al. 2012; Hsiao-Yu et al. 2012) The walkway is made of a Plexiglas chamber (80 cm long, 6 cm wide, 12 cm high) with a 45° tilting mirror placed under the walkway. The LED light was illuminated from the inferioranterior directions of the walkway. The tilted mirror reflects the soles on the track. The reflected footprints and lateral limb can be simultaneously recorded by the digital camera (EX-F1; Casio, Japan) positioned 1 m in front of and at the same level as the walkway. The lateral and plantar views of walking track corners were marked with seven red circles (5 mm in diameter) to represent the horizontal and vertical frames, respectively. The data were processed by a MATLAB program designed by our laboratory (MathWorks, Natick, MA). Following an initial pixels/mm calibration, the resolution was 0.18 mm in the 50-cm walking track. For all trials, the system was calibrated to calculate the pixel-to-distance ratio at any plane using red circle markers. The calibration was carried out on the sagittal and bottom views. The overall pixel to distance ratios were 0.18 and 0.21 mm/pixel for the sagittal and bottom views. The sciatic function index (SFI) (Bain et al. 1989) was calculated using paired measurements of the print length (PL), toe spread (TS) (first to fifth toe), and intermediary toe spread (IT) (second to fourth toe). The measurements of the control left foot (CPL, CTS, CIT) and of the corresponding right experimental foot (EPL, ETS, EIT) were recorded for each rat at each time point. The measurements were then incorporated into the SFI. The formula is as follows:
Sciatic Nerve Fibrosis Assessments and Immunohistochemistry
The sciatic nerve fibrosis assessment was done after the walking-track analysis had been completed, and then, the rats were anesthetized with an overdose of sodium pentobarbital (70 mg/kg) (Sigma-Aldrich, St. Louis, MO, USA). After they had been deeply anesthetized, the rats were perfused with 4% paraformaldehyde in phosphate-buffered saline (PBS) for 6 min and then with PBS-only for 6 min. Their sciatic nerves were collected and immersed in 4 °C paraformaldehyde overnight. The next day, after they had been washed with PBS three times for a total of 10 min, the samples were dehydrated with increasing percentages of ethanol (70, 95, and 100%; 1 h at each concentration). The tissue samples were then immersed in xylene, paraffin and an isometric of xylene, and then pure paraffin, in that order. Each nerve was then cut into five 50-mm samples, embedded in paraffin, and then sliced longitudinally into 5-mm-thick sections. Sample sections were deparaffinized using xylene and then rehydrated with decreasing percentages of alcohol (100, 95, and 70%) using a standard protocol (http://www.abcam.com/protocols/ihc-deparaffinization-protocol). Nerve sections were stained using a Masson trichrome stain kit (Sigma-Aldrich). Fibrous tissue turned bright blue. For trichrome staining, the hue value used for blue was measured in all slides, and the average hue from 155 to 175 was used to evaluate the slides. The default hue width was used to set an adequate threshold for measuring fibrosis. In this study, the color density was calculated in a 144′ 412-pixel photograph and then presented as pixel density/cm2. The pixel density was analyzed using Image J 1.46 (http://imagej.nih.gov/ij/) as a fibrosis index. For quantitative analysis, type I collagen staining was done in addition to trichrome staining. The slides were prepared using heat-induced antigen retrieval (http://www.abcam.com/protocols/ihc-antigen-retrieval-protocol) with 10-mM citric acid (pH 6.0) at 98 °C for 20 min. The slide was incubated with collagen I (EMD; Millipore, Billerica, MA, USA, AB755P; 1:50) antibody overnight at room temperature. After they had been washed, the nerve sections were incubated with goat anti-rabbit IgG antibody(Jackson immunoresearch, 111-035-144; 1:1000) for 1 h. Collagen I was visualized by incubating the sections with diaminobenzidine (DAB). To quantify the percentage of the collagen-I-positive stained area, four photographs of each group around the suture site were acquired and then analyzed using the Image J mark and count tool. Finally, the mean of the collagen-I-positive stained area in each group was calculated.
Seven days after neurorrhaphy, a double-immunofluorescence staining was performed to assess autophagy in specific cell. The sciatic nerve sections were blocked in 2.5% goat serum for 1 h at room temperature following incubation with S-100beta (Abcam, Cambridge, UK, ab212816; 2μg/ml) and neurofilament antibodies (EMD; Millipore, NE1017; 1:1000) overnight at 4 °C, and then washed three times with PBS. The slides were then incubated with light chain 3 (LC3) antiserum which was meant to visualize the ongoing autophagy (PM036; 1:500, MBL Medical & Biological Laboratories, Nagoya, Japan) overnight at 4 °C. After they had been washed, they were double-stained and incubated with Alexa Fluor®594-conjugated goat anti-rabbit IgG (111-585-144, 1:300; Jackson ImmunoResearch, West Grove, PA, USA) and Alexa Fluor®488-conjugated goat anti-mouse IgG (711-545-152, 1:300; Jackson ImmunoResearch, West Grove, PA, USA) for 1 h at room temperature. The slides were mounted (ProLong Gold Antifade Mountant with DAPI; Invitrogen, Waltham, MA, USA) after they had been washed.
All images were captured using fluorescence microscopy (BMI-4000B; Leica Microsystems CMS GmbH, Mannheim, Germany). Image J 1.46 was used to quantify the immunohistochemical and immunofluorescence assessment results. The number of immunofluorescent pixels was automatically counted (4 nerve sections/rat) using the Image J mark and count tool’s RGB (red, green, blue) method, which uses brightness values for the calculation, and then, the mean for each group of rats (n = 6/group) was calculated.
Statistical Analysis
One-way analysis of variance (ANOVA) was used to compare the SFI, fibrosis index, and immunohistochemical assessment with drug administration after neurorrhaphy. Post hoc comparisons were made using Tukey’s test. Significance was set at p < 0.05. All data are means ± standard error of the mean (SEM). Two researchers were not involved in this research and performed all analysis twice.
Results
SFI Outcome
The SFI ranges from − 10 (normal) to − 100 (severe injury) (Bain et al. 1989). The sham group SFI (− 10.23 ± 6.54) was unchanged after the rats had been injected (ipl) with DMSO. Rats injected (ipl) with RAPA to induce autophagy had a significantly higher level of hind-limb function (− 44.56 ± 5.86 vs. − 59.74 ± 5.11; p < 0.05) than did rats injected with DMSO. In contrast, the functional recovery of rats injected (ipl) with 3-MA was significantly inhibited (− 72.15 ± 15.84 vs. − 59.74 ± 5.11; p < 0.05) (compared with the DMSO group) (Fig. 2).
Measuring Nerve Fibrosis
To understand the effects of autophagy on sciatic nerve fibrosis, we investigated fibrotic tissue formation after the induction and inhibition of autophagy. Macroscopic observation showed that, 8 weeks after the sciatic nerve repair, the repair site was enlarged (Fig. 3c#) and opaquely dark yellow. The neoplastic (fibrotic) tissue was significantly less abundant in the RAPA group but more abundant in the 3-MA group. Microscopic observation of the fibrosis of the Masson’s trichrome-stained sciatic nerve sections showed that the suture site was surrounded by blue-stained fibrotic tissue (*) (Fig. 3a, b). Sciatic nerves in the DMSO group had significantly more fibrotic tissue around the nerve repair site than did those in the sham group (sham vs. DMSO: 0.012 ± 0.004 vs. 0.034 ± 0.005 pixels per cm2; p < 0.01) (Fig. 3a, b). Sciatic nerves in the RAPA group had significantly less fibrotic tissue around the nerve-repair site than did those in the DMSO group (RAPA vs. DMSO: 0.023 ± 0.003 vs. 0.034 ± 0.005 pixels per cm2; p < 0.05), and the sciatic nerves in the 3-MA group had significantly more fibrotic tissue than did those in the DMSO group (3-MA vs. DMSO: 0.049 ± 0.004 vs. 0.034 ± 0.005 pixels per cm2; p < 0.05) (Fig. 3d). Collagen I-stained sciatic nerves had a significantly larger distribution area in the 3-MA group and a significantly smaller one in the RAPA group (3-MA vs. DMSO: 38.49 ± 3.038 vs. 13.91 ± 2.583%; p < 0.005; RAPA vs. DMSO: 7.114 ± 1.909 vs. 13.91 ± 2.583%; p < 0.05) (Fig. 4).
The sciatic nerve fibrosis assessment at 2 months after neural repair in c gross observation, a, b Masson’s trichrome staining, d quantified using the pixel density of fibrotic tissue, and e photograph of microscopic magnification 4× and 40× from the suture area (a, b: □). f Enlargement of the magnification 40× from e, and arrowheads (△) indicate the Masson’s trichrome stained tissue. Autophagy induced by RAPA treatment resulted in greater fibrosis reduction than did DMSO and 3-MA treatment. The error bars represent SD. #suture site. [*] DMSO compared with RAPA; [#] DMSO compared with 3-MA; *p < 0.05; **p < 0.01; ***p < 0.005; ****p < 0.001. A rat injected with 3-MA shows severe tethering and a very thick scar tissue surrounding the nerve. A rat injected with RAPA shows minimal tethering and only a very thin membrane of scar tissue surrounding the nerve (e)
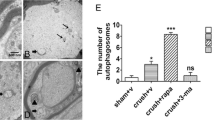
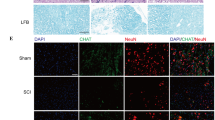
Sciatic Nerve Immunohistochemistry
Autophagy intensity can be modulated by RAPA or 3-MA (Chong et al. 2012; Kim et al. 2013; Ravikumar et al. 2004; Malagelada et al. 2010; Caccamo et al. 2010; Rangaraju et al. 2010; Abe et al. 2010). Therefore, we investigated whether RAPA increased and whether 3-MA decreased autophagy intensity in neurofilaments and SCs. Seven days after neurorrhaphy, we immunohistochemically analyzed LC3 expression (autophagy analysis) in the SC (stained with S-100) nerve repair site. SC ongoing autophagy (a merge of S-100 and LC3) in the RAPA group was compared with SC ongoing autophagy in the DMSO and 3-MA groups (Fig. 5a). The RAPA group showed a trend of increasing S-100, LC3, and merge staining. In contrast, the 3-MA group showed a trend of decreasing merge staining (RAPA vs. DMSO: 115.5 ± 11.56 vs. 28.5 ± 4.203 pixels per cm2, p < 0.001; 3-MA vs. DMSO: 10 ± 4.546 vs. 28.5 ± 4.203 pixels per cm2, p < 0.05). There was also a trend of increasing neurofilament, LC3, and merge staining in the RAPA group (Fig. 5b). The 3-MA group showed a decrease of merge staining, however (RAPA vs. DMSO: 282.6 ± 14.51 vs. 158.8 ± 30.82 pixels per cm2, p < 0.001; 3-MA vs. DMSO: 16.8 ± 11.12 vs. 158.8 ± 30.82 pixels per cm2, p < 0.001). In S100 and neurofilament stain samples only, the S100 pixel density (Fig. 5a) was greater in both the 3-MA group and the RAPA group (DMSO [57.0 ± 8.3] vs. 3-MA [84.5 ± 12.0] and RAPA [120.6 ± 10.5] pixels per cm2). The distribution sites of neurofilament pixel density (Fig. 5b) were not significantly different in the DMSO and the RAPA groups, but they were significantly lower after 3-MA treatment (DMSO vs. 3-MA: 678.5 ± 147.4 vs. 308.5 ± 95.0 pixels per cm2).
A longitudinal section of sciatic nerve immunofluorescence labeled for LC3 (red) with a S-100 (green) and b neurofilament (green) 7 days after sciatic nerve repair. Arrowheads (s) indicate double-positive stained cells. Effects of treatments on LC3 expression are shown in the graph; histograms show red pixels converted to brightness values. The autophagy intensity was higher in Schwann cells and neurofilaments after RAPA treatment. In contrast, autophagy was inhibited in 3-MA-treated Schwann cells and neurofilaments. Scale bar: 20 mm. [*] DMSO compared with RAPA; [#] DMSO compared with 3-MA; *p < 0.05; **p < 0.01; ***p < 0.005; ****p < 0.001
Discussion
We investigated the effects of autophagy on neuronal scarring in the first 8 weeks after peripheral nerve repair. In rats that had been injected with RAPA, (i) peripheral nerve function recovered more quickly, (ii) fibrosis was inhibited, and (iii) nerve regeneration was facilitated.
As with other conventional wound-healing processes, peripheral nerve regeneration involves an early inflammatory phase, a granulation phase, and, finally, a remodeling phase and scar formation. Thus, it inevitably results in intraneural scarring that impedes axonal regeneration and is a mechanical barrier to sprouting axons (Mathur et al. 1983). Multiple branched axonal terminals were found at the neuromas developed from these barriers (Lane et al. 1978; Sunderland 1978), and the ectopic neural discharge at these sites is important in neuropathic pain (Yates et al. 2000; Devor 2001). An experimental study (Eather et al. 1986) on rat sciatic nerves found that this was most prominent in nerve segments that were 2.5 mm proximal and distal to the injury site. Scar formation also occurred diffusely and distally within the transected nerve, which suggested that this process is not merely a reaction to local inflammation. Moreover, the amount of scar tissue formed depended upon the severity of the nerve trauma (Sunderland 1987). Sunderland’s Nerves and Nerve Injuries (Sunderland 1987) extensively highlights this scarring problem.
Our rat gait analyses showed that RAPA treatment yielded better functional recovery than did DMSO or 3-MA treatment. Thus, we hypothesized that functional recovery after sciatic nerve repair is associated with SC autophagy and scar reduction. Autopsies done 2 months after the nerve repair verified our hypothesis. The RAPA group had less scarring and better functional performance. Collagen and scar formation in the distal segment of a severed nerve are associated with the shrinking of endoneurial sheaths, which leads to the reduction of axonal diameter by as much as 80–90% (Sunderland 1987; Sunderland and Bradley 1959). This agreed with Bora’s (Bora 1967) report of a negative correlation between the degree of functional return and the amount of scar formation at the repair site.
Immunohistochemistry was used to determine the correlation between SC autophagy and nerve scar reduction. We found that, in the RAPA group, 7 days post-nerve repair, LC3 levels were substantially higher than in the DMSO and 3-MA groups. Co-localization of LC3 (autophagy analysis) protein and S-100 (Schwann cell analysis) was higher in the RAPA group, and these results showed that more SCs were engaged in autophagy in the RAPA group than in the other groups. The co-localization of neurofilaments and LC3 showed that autophagy is beneficial for nerve regeneration. The RAPA group also had more co-localization of neurofilaments and LC3 than did the other groups. Thus, RAPA, which induces autophagy, might facilitate nerve regeneration.
Many studies have investigated the effects of scar-suppressing drugs at a site of peripheral nerve injury. Topically applied triamcinolone acetate, a steroid, improved nerve regeneration in squirrels and monkeys (Graham et al. 1973), and triamcinolone hexacetonide had a similar effect in ferrets (Nachemson et al 1985). However, the collagen-formation inhibiting agents penicillamine (Bucko et al. 1981) and cis-hydroxyproline (Nachemson et al. 1985) had no apparent effect. Using collagenase (Wehling et al. 1992; Rydevik et al. 2002) and hyaluronic acid (Ozgenel 2003) has produced conflicting results. Other studies report positive results using a polymer gel (Peterson et al. 1996), hyaluronic acid-carboxymethyl cellulose membrane (Adanali et al. 2003), amniotic fluid (Ozgenel and Filiz 2003), low-dose external beam radiation (Gorgulu et al. 2003), tissue plasminogen activator (Zou et al. 2006), and various combinations of these (Ozgenel and Filiz 2004). Here, we tested RAPA, a widely used therapeutic compound that increases autophagy within neuropathic SCs, and that might improve their capacity to myelinate. Many research groups have used RAPA to investigate the effects of SC autophagy on central nervous system diseases like Huntington’s (Ravikumar et al. 2004), Parkinson’s (Malagelada et al. 2010), and Alzheimer’s (Caccamo et al. 2010) and have reported positive effects in animal models. Abe et al. (Abe et al. 2010) reported greater axonal regeneration in peripheral nerve system neurons after they had activated the mTOR pathway with RAPA. Our findings suggest that neural scarring can be reduced and that functional recovery can be increased in an animal model during healing by using RAPA in the first week after nerve repair. Using 3-MA, however, caused neural scarring and worsened functional recovery.
Because SCs respond robustly to RAPA, and because the peripheral nervous system is outside the blood-brain barrier, it is possible that peripheral nerves will respond to this compound more robustly than will nerves in the central nervous system. We showed that RAPA promoted functional recovery and was associated with scar reduction and autophagy. Significantly, RAPA improved the continuity and the neural function of neurofilaments. Our findings support the notion that peripheral nerve regeneration is crucially associated with autophagy and scar reduction.
This study has some limitations. First, we determined pixel density without cell counting. Cell size and staining consistency are the confounding factors for pixel density analysis. Second, although we found that RAPA promoted nerve regeneration and functional recovery, and that nerve regeneration was associated with SC autophagy and scar reduction, we are unable to conclude that autophagy causes nerve regeneration. Additional studies are required to clarify whether autophagy is merely correlated with nerve regeneration, or whether and how it is involved in nerve regeneration.
References
Abe N, Borson SH, Cavalli V et al (2010) Mammalian target of rapamycin (mTOR) activation increases axonal growth capacity of injured peripheral nerves. J Biol Chem 285(36):28034–28043
Adanali G, Verdi M, Tuncel A, Erdogan B, Kargi E (2003) Effects of hyaluronic acid-carboxymethylcellulose membrane on extraneural adhesion formation and peripheral nerve regeneration. J Reconstr Microsurg 19:29–36
Bain JR, Mackinnon SE, Hunter RT (1989) Functional evaluation of complete sciatic peroneal, and posterior tibial nerve lesions in the rat. Plast Reconstr Surg 83:129–138
Bora FJ (1967) Peripheral nerve repair in cats. The fascicular stitch. J Bone Joint Surg [Am] 49:659–666
Bucko CD, Joynt RL, Grabb WC (1981) Peripheral nerve regeneration in primates during D-penicillamine-induced lathyrism. Plast Reconstr Surg 67:23–30
Caccamo A, Majumder S, Richardson A, Strong R, Oddo S (2010) Molecular interplay between mammalian target of rapamycin (mTOR), amyloid-beta, and tau: effects on cognitive impairments. J Biol Chem 285:13107–13120
Chong ZZ, Shang YC, Wang S, Maiese K (2012) Shedding new light on neurodegenerative diseases through the mammalian target of rapamycin. Prog Neurobiol 99:128–148
Chu CT (2006) Autophagic stress in neuronal injury and disease. J Neuropathol Exp Neurol 65:423–432
Devor M (2001) Neuropathic pain: what do we do with all these theories? Acta Anaesthesiol Scand 45:1121–1127
Devor M, Seltzer Z (1999) Pathophysiology of damaged nerves in relation to chronic pain. In: Wall PD, Melzack R (eds) Textbook of pain. Churchill Livingstone, London, pp 129–164
Eather TF, Pollock M, Myers DB (1986) Proximal and distal changes in collagen content of peripheral nerve that follow transection and crush lesions. Exp Neurol 92:299–310
Gomez-Sanchez JA, Carty L, Iruarrizaga-Lejarreta M, Palomo-Irigoyen M, Varela-Rey M, Griffith M, Hantke J, Macias-Camara N, Azkargorta M, Aurrekoetxea I, de Juan VG, Jefferies HBJ, Aspichueta P, Elortza F, Aransay AM, Martínez-Chantar ML, Baas F, Mato JM, Mirsky R, Woodhoo A, Jessen KR (2015) Schwann cell autophagy, myelinophagy, initiates myelin clearance from injured nerves. J Cell Biol 210(1):153–168
Gorgulu A, Uzal C, Doganay L, Imer M, Eliuz K, Cobanoglu S (2003) The effect of low-dose external beam radiation on extraneural scarring after peripheral nerve surgery in rats. Neurosurgery 53:1389–1395
Graham W, Patakey P, Calabretta A, Munger B, Buda M (1973) Enhancement of peripheral nerve regeneration with triamcinolone after neurorrhaphy. Surg Forum 24:457–461
Hsiao-Yu L, Tsung-Hsun H, Jia-Jin JC et al (2012) Quantitative video-based gait pattern analysis for hemiparkinsonian rats. Med Biol Eng Comput 50:937–946
Jen-I L, Meng-Yi C, Ming-Long Y et al (2012) Video-based gait analysis for functional evaluation of healing Achilles tendon in rats. Ann Biomed Eng 40(12):2532–2540
Kim SG, Buel GR, Blenis J (2013) Nutrient regulation of the mTOR complex 1 signaling pathway. Mol Cells 35:463–473
Lane JM, Bora FW Jr, Pleasure D (1978) Neuroma scar formation in rats following peripheral nerve transection. J Bone Joint Surg Am 60:197–203
Larsen KE, Sulzer D (2002) Autophagy in neurons: a review. Histol Histopathol 17:897–908
Lundborg G, Danielsen N (1991) Injury, degeneration and regeneration. In: Gelberman RH (ed) Operative nerve repair and reconstruction, vol 1. JB Lippincott, Philadelphia, pp 109–131
Malagelada C, Jin ZH, Jackson-Lewis V, Przedborski S, Greene LA (2010) Rapamycin protects against neuron death in in vitro and in vivo models of Parkinson’s disease. J Neurosci 30:1166–1175
Marinelli S, Pavone F et al (2011) Schwann cell autophagy counteracts the onset and chronification. Pain 155:93–107
Mathur A, Merrell JC, Russell RC, Zook EG (1983) A scanning electron microscopy evaluation of peripheral nerve regeneration. Scan Electron Microsc 1983(Pt 2):975–981
McCallion RL, Ferguson MW (1996) Fetal wound healing and the development of antiscarring therapies for adult wound healing. In: Clark RA (ed) The molecular and cell biology of wound repair, 2nd edn. Plenum Press, New York, pp 561–599
Nachemson AK, Lundborg G, Myrhage R, Rank F (1985) Nerve regeneration after pharmacological suppression of the scar reaction at the suture site. An experimental study on the effect of estrogen-progesterone, methylprednisolone-acetate and cis-hydroxyproline in rat sciatic nerve. Scand J Plast Reconstr Surg 19:255–260
Ozgenel GY (2003) Effects of hyaluronic acid on peripheral nerve scarring and regeneration in rats. Microsurgery 23:575–581
Ozgenel GY, Filiz G (2003) Effects of human amniotic fluid on peripheral nerve scarring and regeneration in rats. J Neurosurg 98:371–377
Ozgenel GY, Filiz G (2004) Combined application of human amniotic membrane wrapping and hyaluronic acid injection in epineurectomized rat sciatic nerve. J Reconstr Microsurg 20:153–157
Peterson J, Russell L, Andrus K, Mackinnon M, Silver J, Kliot M (1996) Reduction of extraneural scarring by ADCON-T/N after surgical intervention. Neurosurgery 38:976–983
Rangaraju S, Verrier JD, Madorsky I, Nicks J, Dunn WA Jr, Notterpek L (2010) Rapamycin activates autophagy and improves myelination in explant cultures from neuropathic mice. J Neurosci 30:11388–11397
Ravikumar B, Vacher C, Berger Z, Davies JE, Luo S, Oroz LG, Scaravilli F, Easton DF, Duden R, O'Kane CJ, Rubinsztein DC (2004) Inhibition of mTOR induces autophagy and reduces toxicity of polyglutamine expansions in fly and mouse models of Huntington disease. Nat Genet 36:585–595
Robinson PP, Loescher AR, Smith KG (2000) A prospective, quantitative study on the clinical outcome of lingual nerve repair. Br J Oral Maxillofacial Surg 38:255–263
Rubinsztein DC, Difiglia M, Heintz N et al (2005) Autophagy and its possible roles in nervous system diseases, damage and repair. Autophagy 1:11–22
Rydevik M, Bergstrom F, Mitts C, Danielson N (2002) Locally applied collagenase and regeneration of transected and repaired rat sciatic nerves. Scand J Plast Reconstr Surg Hand Surg 36:193–196
Sunderland S (1978) Nerves and nerve injuries, 2nd edn. Churchill Livingstone, London, pp 188–200
Sunderland S (1987) Nerves and nerve injuries. Churchill Livingstone, New York, pp 173–176
Sunderland S, Bradley KC (1959) Endoneurial tube shrinkage in the distal segment of a severed nerve. J Comp Neurol 93:411–420
Wehling P, Pak M, Cleveland S, Nieper R (1992) The influence of bacterial collagenase on regeneration of severed rat sciatic nerves. Acta Neurochir 119:121–127
Yates JM, Smith KG, Robinson PP (2000) Ectopic neural activity from myelinated afferent fibres in the lingual nerve of the ferret following three types of injury. Brain Res 874:37–47
Yates JM, Smith KG, Robinson PP (2004) The effect of triamcinolone hexacetonide on the spontaneous and mechanically-induced ectopic discharge following lingual nerve injury in the ferret. Pain 111:261–269
Zou T, Ling C, Xiao Y, Tao X, Ma D, Chen ZL, Strickland S, Song H (2006) Exogenous tissue plasminogen activator enhances peripheral nerve regeneration and functional recovery after injury in mice. J Neuropath Exp Neurol 65:78–86
Acknowledgements
We are grateful to Kuen-Jer Tsai, PhD, Ms. I-Wen Shene, Ms. Shu Hsien Shih, and Ms. Ying-Chiu Lin for their excellent assistance. None of the authors has a commercial interest relevant to the manuscript.
Funding
This study was supported by grant NSC106-2314-B-006-004 from the National Science Council, Taiwan, grant EDAHP 106004 from the E-Da Hospital, Taiwan.
Author information
Authors and Affiliations
Contributions
Po-Yen Ko and Cheng-Chang Yang contributed equally to this work. Po-Yen Ko and Cheng-Chang Yang carried out the study design, acquiring and analyzing the data, and drafting of the articles; Yao-Lung Kuo, Tai-I Hsu participated in the critical revision of the article for important intellectual content, and technical or logical support; Fong-Chin Su, Yuan-Kun Tu, and I-Ming Jou participated in the final approval of the article provision of the study, obtaining of funding, provision of study materials, and critical revision of the article for important intellectual content. All authors have read and approved the final submitted manuscript.
Corresponding authors
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Ko, PY., Yang, CC., Kuo, YL. et al. Schwann-Cell Autophagy, Functional Recovery, and Scar Reduction After Peripheral Nerve Repair. J Mol Neurosci 64, 601–610 (2018). https://doi.org/10.1007/s12031-018-1056-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-018-1056-8