Abstract
The tumor necrosis factor receptor-associated factor 6 (TRAF6) gene encodes a protein that acts downstream of the Toll-like receptor (TLR) pathway. TLRs activate inflammatory cascades and mediate inflammatory injury after cerebral ischemia. However, the role of TFAR6 gene polymorphisms in ischemic stroke (IS) remains unknown. This study aims to investigate the associations of TRAF6 gene polymorphisms with susceptibility to IS and IS-related quantitative traits in Southern Chinese Han population. A total of 816 IS cases and 816 age- and gender-matched controls were included. Two variants of the TRAF6 gene (rs5030411 and rs5030416) were genotyped using the Sequenom MassARRAY iPLEX platform. Our study showed that rs5030416 was significantly associated with increased susceptibility to IS in the additive model [ORadj 1.25(1.04–1.51), P adj = 0.019, P Bc = 0.038] and dominant model [ORadj 1.23(1.04–1.60), P adj = 0.021, P Bc = 0.042] after adjusting by age and sex and applying a Bonferroni correction. No significant association was found between rs5030411 and IS susceptibility (all P > 0.05). The haplotype rs5030416 (allele C)-rs5030411 (allele C) was significantly associated with IS susceptibility (P adj = 0.015). Moreover, a significant association of rs5030411 with TC levels in IS patients under the additive model [β 0.16(0.01–0.30), P adj = 0.034] and recessive model [β 0.45(0.12–0.78), P adj = 0.007] was observed after adjustment by age and sex. This association remained statistically significant under the recessive model (P Bc = 0.042) after Bonferroni correction. Our results suggest that TRAF6 gene polymorphisms may be involved in the pathogenesis of IS.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Stroke is one of the leading causes of premature death and disability-adjusted life years (DALY) worldwide (Bonita 1992; Lozano et al. 2012; Murray et al. 2012). In China, the annual incidence of stroke is over 2.5 million, and the number of stroke survivors who need long-term, costly care is seven million (Xue et al. 2009). The burden of stroke becomes more serious with the growing age of the world’s population, significantly affecting the economy and social stability, especially in Asian counties (Kim 2014). Stroke represents a complex clinical syndrome caused by the disruption of focal cerebral blood supply (Markus 2011). Approximately 20 % of strokes are hemorrhagic, while 80 % are ischemic (Feigin et al. 2003), mainly attributed to cerebral arterial occlusion resulting from atherosclerosis (Humphries and Morgan 2004). Ischemic stroke can lead to tissue hypoxia and metabolic disorders following irreversible brain damage (Dirnagl et al. 1999).
Many conventional risk factors contribute to stroke, such as hypertension, obesity, atrial fibrillation, diabetes, dyslipidemia, and smoking (Dichgans 2007). However, these factors cannot fully explain all stroke risks (Sacco et al. 1989). Twin studies and family history studies suggest an important role for genetic predisposition in stroke pathogenesis (Sacco et al. 1989; Brass et al. 1992; Bak et al. 2002; Jerrard-Dunne et al. 2003). Previous linkage studies and candidate gene association studies have found potential susceptibility chromosomal regions and genetic loci for stroke. A genome-wide association study (GWAS) is an important strategy for uncovering the genetic mechanisms of complex human diseases. Various genetic variants associated with neurological disorders, such as Alzheimer’s disease (Cruchaga et al. 2013) and Parkinson’s disease (Hill-Burns et al. 2014), have been successfully identified through this method. Currently, GWAS on stroke is relatively less common (http://www.ebi.ac.uk/gwas/), and no GWAS on stroke have been carried out in the Chinese population. Therefore, candidate gene studies are still important, and corresponding genes involved in the etiological hypothesis of stroke are noteworthy. It is necessary to identify susceptibility gene variants to further clarify the genetic mechanisms responsible for stroke.
The tumor necrosis factor receptor-associated factor 6 (TRAF6) gene is located on chromosome 11p12 (Namjou et al. 2012). The protein encoded by the TRAF6 gene is a 63 kDa molecule from the tumor necrosis factor receptor-associated factors (TRAFs) superfamily (Cao et al. 1996; Ishida et al. 1996), which consists of cytoplasmic adapter proteins that can recognize various pro-inflammatory cytokines [e.g., CD40L, tumor necrosis factor-α (TNF-α), interleukin-1β]. TRAF6 has important functions in regulating the development of some tissues, such as the central nervous system and lymph nodes, as well as various physiological processes including bone metabolism, innate immunity, and adaptive immunity (Bradley and Pober 2001). Unlike the other family members that are involved only in signal transduction from the tumor necrosis factor receptor (TNFR) superfamily, TRAF6 can also meditate signaling from the interleukin-1 (IL-1R)/Toll-like receptor (TLR) superfamily (Wu and Arron 2003). TLR family members, except for TLR3, signal through the myeloid differentiation factor 88 (MyD88)-dependent pathway (Wang et al. 2011), while TRAF6 is a crucial molecule in the MyD88-dependent pathway. When the Toll/IL-1R (TIR) domain interacts with the adaptor protein MyD88, TRAF6 is recruited along with IL-1R-associated kinase 1 (IRAK1) and IL-1R-associated kinase 4 (IRAK4), leading to translocation of transcription factor nuclear factor κB (NF-κB) and production of pro-inflammatory cytokines (Akira and Takeda 2004; Moghimpour Bijani et al. 2012). TLRs activate inflammatory cascades and mediate inflammatory injury in cerebral ischemia (Caso et al. 2007; Wang et al. 2011). Therefore, the crucial role of TRAF6 in the TLR downstream pathway may suggest its involvement in IS development.
Miyahara et al. (Miyahara et al. 2004) showed that TRAF6 participated in the formation of neointimal lesions through an inflammatory signaling pathway based on a rabbit carotid arterial injury model. Wu et al. (Wu et al. 2013) reported that the TRAF6 gene was upregulated in the peripheral blood of IS patients, and its role in the TLR downstream pathways during IS development was crucial. Furthermore, Yuan et al. (Yuan et al. 2013) reported that TRAF6 mRNA expression was upregulated in neuronal cells, and activated TRAF6 promoted the inflammatory process triggered by cerebral ischemia–reperfusion to mediate cell apoptosis in a rat cerebral ischemia–reperfusion model. This evidence suggested that TRAF6 may be involved in IS pathogenesis. However, to the best of our knowledge, no association studies on TRAF6 single nucleotide polymorphisms (SNPs) and IS susceptibility have been reported yet. According to the HapMap database, this gene has 13 common SNPs. Among these SNPs, rs5030411 is a transcript variant occurring in an intron, and rs5030416 is a sequence variant occurring in a non-coding transcript exon (http://asia.ensembl.org/index.html). Therefore, we performed the present study, which included 816 IS cases and 816 controls, to investigate the associations between two TRAF6 SNPs (rs5030411 and rs5030416) and susceptibility to IS, as well as IS-related quantitative traits, in Southern Chinese Han population.
Materials and Methods
Subjects
The present study was performed with prior approval from the Medical Ethics Committees of Guangxi University of Chinese Medicine. All subjects were declared to be unrelated Southern Chinese Han individuals and provided written informed consent. A total of 816 IS cases were recruited from inpatients admitted to the Neurology Department at the First Affiliated Hospital of Guangxi University of Chinese Medicine between July 2009 and July 2014. The diagnosis of IS was determined by two or more clinical neurologists according to the “diagnosis of cerebral vascular disease” criteria revised in the Fourth National Academic Conference of Cerebral Vascular Disease. All cases were confirmed with computed tomography (CT) and/or magnetic resonance imaging (MRI). We excluded patients with tumor, cardiogenic embolism, traumatic brain injury, transient ischemic attack (TIA), and intracranial vascular malformation. Cases complicated with systemic disease (inflammatory disease, collagenosis, severe cardiac dysfunction, severe hepatosis, and severe renal disorders) or presented poor compliance were also excluded. The control group consisted of 816 individuals matched for gender and age, randomly recruited from healthy individuals who attended physical examination. Orthopedic patients without serious illness and neurological disease were also enrolled in the control group. All controls were free of autoimmune disease and history of cardio-cerebrovascular diseases and did not accept hormone or immunosuppressive therapy during the enrollment period.
Demographics and Clinical Parameters
A uniform questionnaire survey was carried out among 1632 subjects for associated demographics, including gender, age, nationality, history of stroke, coronary heart disease, diabetes, hypertension and hyperlipidemia, and family history. Systolic blood pressure (SBP) and diastolic blood pressure (DBP) were measured with a mercury sphygmomanometer. Limosis peripheral blood (10 ml) was collected from each subject with anticoagulant and non-anticoagulant tubes. The total cholesterol (TC), triglyceride (TG), high-density lipoprotein cholesterol (HDL-C), and low-density lipoprotein cholesterin (LDL-C) were analyzed in non-anticoagulant blood using the Hitachi 7600 automated biochemistry analyzer based on standard laboratory procedures.
DNA Extraction and Genotyping
Anticoagulant blood samples were stored at 4 °C. Genomic DNA extraction was carried out using the TIANamp Blood DNA Kit (Tiangen Biotech, Beijing, China) based on the product manual within a week. Extracted DNA samples were preserved at −80 °C until analysis. Primer for rs5030411 and rs5030416 were designed using the Sequenom Assay Designer 3.1 software (Sequenom, San Diego, CA, USA); details are provided in Table S1. The Sequenom MassARRAY iPLEX platform was used for genotyping. Primer design, oligo synthesis, and SNP genotyping were completed by Bomiao Biological Co., Ltd., Beijing, China. All operators strictly followed a set of standard procedures and were blinded to the identity of the samples with regard to case and control status throughout the trial. Furthermore, we re-genotyped 5 % of the DNA samples selected randomly and achieved complete concordance.
Statistical Analysis
Differences in gender, age, and other demographic variables between groups were analyzed using SPSS for windows, version 16.0. Enumeration data were compared with the chi-square test and measurement data (normally distributed) by independent samples t test. The PLINK software (http://pngu.mgh.harvard.edu/∼purcell/plink/) was used to estimate any association between genotypes and phenotypes. Distributions of genotype were subjected to a chi-square goodness-of-fit test for deviations from the Hardy–Weinberg equilibrium (HWE) for the controls. The association between polymorphisms and IS was assessed by odds ratios (ORs) with 95 % confidence intervals (CIs) using multiple logistic regression analysis with adjustment of conventional confounding variables in four genetic models, namely, the additive, dominant, recessive, and allelic models. Haplotypes were also estimated using multiple logistic regression. Moreover, we determined the association between polymorphisms and IS-related quantitative traits with the linear regression analysis method. Bonferroni correction was used to adjust the P value for multiple comparisons. The test power was calculated using the Quanto software (http:// hydra.usc.edu/gxe). Corresponding parameters for power calculations were as follows: minor allele frequency of 0.21 for rs5030411 and 0.16 for rs5030416, odds ratio of 1.3, sample size for each group (case group and control group) of 816, and additive model and disease prevalence for IS of 0.019 (http://www.gov.cn/xinwen/2014-05/19/content_2682279.htm). All tests were set as two-tailed; P values less than 0.05 were considered statistically significant.
Results
Characteristics of Subjects
The test power for rs5030411 and rs5030416 was 88 and 82 %, respectively. A total of 816 IS patients (465 males and 351 females) and 816 controls (433 males and 383 females) were included in the present study. The mean age of the IS group was 65.97 ± 10.50 years, compared with 65.26 ± 10.87 years for the controls. No statistically significant difference was observed between the two groups with respect to gender (P = 0.11), age (P = 0.179), and TC (P = 0.202) or TG levels (P = 0.368), whereas the SBP (P < 0.001), DBP (P < 0.001), HDL (P < 0.001), and LDL levels (P = 0.020) were significantly different between the IS cases and the controls.
TRAF6 Gene Polymorphisms and Risk of IS
As shown in Table 1, the genotype distribution of rs5030416 and rs5030411 both conformed to the Hardy–Weinberg equilibrium among controls. A statistical association was observed between rs5030416 and elevated risk of IS (additive model: OR = 1.26, 95 % CI = 1.04–1.51, P = 0.016; dominant model: OR = 1.30, 95 % CI = 1.05–1.61, P = 0.017; and allelic model: OR = 1.26, 95 % CI = 1.05–1.53, P = 0.015). This association was also detected in the additive and dominant models after adjusting for covariates by age and sex and adjusting the P value with Bonferroni correction (additive model: ORadj = 1.25, 95 % CI = 1.04–1.51, P adj = 0.019, P Bc = 0.038; dominant model: ORadj = 1.23, 95 % CI = 1.04–1.60, P adj = 0.021, P Bc = 0.042). No statistical association was observed between rs5030411 and IS under any models (all P > 0.05) (Table 2).
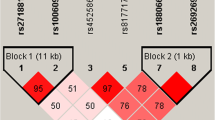
Haplotype and Risk of IS
We estimated IS and three common haplotypes constructed from rs5030416 and rs5030411. As shown in Table 3, a significant difference was observed in distribution of the haplotype rs5030416 (allele C)-rs5030411 (allele C) between cases and controls, suggesting that this haplotype may increase the risk of IS (OR = 1.27, P = 0.013). Adjustment by age did not alter the results.
TRAF6 Gene Polymorphisms and IS-Related Quantitative Traits
According to the linear regression analysis, the polymorphism rs5030411 showed a statistical association with TC levels in IS patients under the additive model [β 0.16(0.01–0.30), P adj = 0.034] and recessive model [β 0.45(0.12–0.78), P adj = 0.007] after adjusting by age and sex, but not the other IS-related quantitative traits (TG, HDL, LDL, SBP, or DBP levels) (Table 4). After a Bonferroni correction, the association between rs5030411 and TC levels in IS patients remained statistically significant under recessive model (P Bc = 0.042) (Table S2). Moreover, no statistically significant association was found between rs5030416 and any of the IS-related quantitative traits (Table 4).
Discussion
To the best of our knowledge, this study is the first to investigate the association between TRAF6 gene variants rs5030411 and rs5030416 with susceptibility to IS. We showed that rs5030416 was associated with increased susceptibility to IS, but no significant association was found between rs5030411 and IS. The haplotype rs5030416 (allele C)-rs5030411 (allele C) increased the susceptibility of IS. Moreover, polymorphism rs5030411 was associated with TC levels in IS patients. The test power in the present study was greater than 80 %.
TRAF6 acts as a convergence point for TNFR and TLR families (Song et al. 1997; Muzio et al. 1998; Ye et al. 2002). In signaling transduction by the TLR family, this protein is essential for activation of the MyD88-dependent pathway. When the Toll/IL-1R (TIR) domain, which is the cytoplasmic region shared by the TLR and IL-1R families, combines with the adaptor protein MyD88, IRAK4 and IRAK1 are recruited and form a heterotrimer. Phosphorylated IRAK1 separates from this heterotrimer and interacts with TRAF6, following the formation of lysine63-linked polyubiquitin chains. These chains can lead to transforming growth factor-activated kinase 1 (TAK1) phosphorylation. Phosphorylated TAK1 is associated with TAK1-binding protein 1 (TAB1), TAK1-binding protein 2 (TAB2), or TAK1-binding protein 3 (TAB3) and promotes activation of mitogen-activated protein kinase (MAPK) pathway and inhibition of the nuclear factor kappa-B kinase (IKK) complex, which results in the translocation of NF-κB and the production of pro-inflammatory cytokines such as TNF-ɑ, interleukin-1(IL-1), and interleukin-1 (IL-6) (Akira and Takeda 2004; Moghimpour Bijani et al. 2012). TLRs have been associated with the activation of various inflammatory cascades in cerebral ischemia and develop an important role in mediating cerebral ischemic injury. In addition, a previous study has suggested that the downregulation of TLR signaling through cerebral preconditioning reduces inflammatory injury after cerebral ischemia (Wang et al. 2011). Based on this evidence, we assumed that TRAF6, which serves as a crucial molecule in the TLR downstream pathway, may be involved in IS development. In this present study, the TRAF6 gene variant rs5030416 was found to increase IS susceptibility. TRAF6 had been demonstrated upregulated in neuronal cells in a rat cerebral ischemia–reperfusion model and in the peripheral blood of IS patients (Wu et al. 2013; Yuan et al. 2013). Furthermore, TRAF6 participates in the inflammation process induced by the TLR pathway, which may exert an important function in cerebral ischemia, as mentioned previously. Therefore, rs5030416 may have modified the expression of TRAF6, thereby promoting inflammatory injury and predisposition to IS. However, this hypothesis remains to be further elucidated.
In our study, the TRAF6 gene variant rs5030411 was found to be associated with elevated TC levels in IS patients. Increasing serum cholesterol was a definite risk factor for IS (Hankey 2006). Previous studies suggested a significant association of a number of genetic variants with TC levels. Lu et al. (Lu et al. 2014) found that the T allele of the ITGA2 C807T polymorphism appeared to increase the TC levels of IS patients. Song et al. (Song et al. 2014) reported that TC levels in IS patients who carried Ala/Thr and Thr/Thr of FABP2 gene were significantly higher than in those who carried Ala/Ala. Although no significant association was observed between the TRAF6 gene polymorphism rs5030411 and IS susceptibility in the present study, this SNP was significantly associated with TC levels in IS patients. However, the role of rs5030411 in lipid metabolism has not been reported to date, and how it influences TC levels needs to be clarified in further studies.
Currently, 16 GWASs on stroke were added to the catalog of published GWASs (http://www.ebi.ac.uk/gwas/). Some SNPs, such as rs556621 on chromosome 6p21.1 (Holliday et al. 2012), rs2107595 in HDAC9, and rs6843082 in PITX2 (Traylor et al. 2012), were identified as susceptibility loci for stroke. But no significant association was reported between TRAF6 SNPs and stroke susceptibility. At present, the majority of these GWASs were performed only in Caucasian. According to the international HapMap data, the minor allele frequency of rs5030411 and rs5030416 in Caucasian (HapMap-CEU) were 0.398 and 0.165, respectively, while they were 0.244 and 0.073 in Chinese (HapMap-CHB), respectively. These results suggest that there may be an ethnicity difference in distribution of the minor allele frequency of these two SNPs in Caucasian and Chinese. Since stroke-associated GWASs in Chinese have not been reported to date, larger GWASs performed in Chinese are required to confirm our findings.
The present study also has certain limitations. First, this study was only conducted among Chinese Han individuals. To reduce the influence of heterogeneity resulting from ethnicity, we explored the effects of gene polymorphisms on IS in a single ethnic population, similar to most studies (Zhao et al. 2012; Cui et al. 2013; Li et al. 2014). We found a significant association between rs5030416 and IS susceptibility; this association should be extrapolated to other ethnic groups with extreme caution. Second, IS is considered a clinically heterogeneous disease, and its pathological mechanisms differ among etiology subtypes (Markus 2011). We did not categorize the IS cases into different subtypes, which may impact on the outcomes of this association study. Further studies on the effects of TRAF6 gene polymorphisms on different IS subtypes are needed. Third, our study was based on a hospital population, so it was difficult to avoid selection bias. A multicenter study with more representative samples is warranted to reduce selection bias. Fourth, similar to reports from other association studies (Zhao et al. 2012; Cui et al. 2013; Luo et al. 2013), the controls in this study did not have a CT or MRI examination, unlike the patients. However, IS is a severe disease with obvious symptoms (Hachinski 2002; Vasiliadis and Zikic 2014), and most individuals clearly know whether they suffer from this disease or not. Thus, the possibility of misclassification bias in the present study was small. Finally, we did not explore the interaction of the gene and the environment, which may play a crucial role in IS development (Humphries and Morgan 2004; Markus et al. 2006). Further research needs to confirm the influence of the studied SNPs on IS based on the interaction with environmental factors.
The present study provides data for an association study on TRAF6 SNPs and IS susceptibility, as well as IS-related quantitative traits, among the Southern Chinese Han population. In summary, we reported that rs5030416 was associated with an increased susceptibility to IS, while rs5030411 was associated with elevated TC levels in IS patients. Subsequent research, including the mechanisms underlying gene–environment interaction, the effects of SNPs on different histological subtypes of IS, and republication in other ethnic groups, is required.
References
Akira S, Takeda K (2004) Toll-like receptor signalling. Nat Rev Immunol 4(7):499–511
Bak S, Gaist D, Sindrup SH, Skytthe A, Christensen K (2002) Genetic liability in stroke: a long-term follow-up study of Danish twins. Stroke 33(3):769–74
Bonita R (1992) Epidemiology of stroke. Lancet 339(8789):342–4
Bradley JR, Pober JS (2001) Tumor necrosis factor receptor-associated factors (TRAFs). Oncogene 20(44):6482–91
Brass LM, Isaacsohn JL, Merikangas KR, Robinette CD (1992) A study of twins and stroke. Stroke 23(2):221–3
Cao Z, Xiong J, Takeuchi M, Kurama T, Goeddel DV (1996) TRAF6 is a signal transducer for interleukin-1. Nature 383(6599):443–6
Caso JR, Pradillo JM, Hurtado O, Lorenzo P, Moro MA, Lizasoain I (2007) Toll-like receptor 4 is involved in brain damage and inflammation after experimental stroke. Circulation 115(12):1599–608
Cruchaga C, Kauwe JS, Harari O et al (2013) GWAS of cerebrospinal fluid tau levels identifies risk variants for Alzheimer’s disease. Neuron 78(2):256–68
Cui X, Chen H, Hou X, Wang S, Jayaram S, Zheng Z (2013) Polymorphism of the RAGE affects the serum inflammatory levels and risk of ischemic stroke in a Chinese population. Cell Physiol Biochem 32(4):986–96
Dichgans M (2007) Genetics of ischaemic stroke. Lancet Neurol 6(2):149–61
Dirnagl U, Iadecola C, Moskowitz MA (1999) Pathobiology of ischaemic stroke: an integrated view. Trends Neurosci 22(9):391–7
Feigin VL, Lawes CM, Bennett DA, Anderson CS (2003) Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol 2(1):43–53
Hachinski V (2002) Stroke: the next 30 years. Stroke 33(1):1–4
Hankey GJ (2006) Potential new risk factors for ischemic stroke: what is their potential? Stroke 37(8):2181–8
Hill-Burns EM, Wissemann WT, Hamza TH, Factor SA, Zabetian CP, Payami H (2014) Identification of a novel Parkinson’s disease locus via stratified genome-wide association study. BMC Genomics 15:118
Holliday EG, Maguire JM, Evans TJ et al (2012) Common variants at 6p21.1 are associated with large artery atherosclerotic stroke. Nat Genet 44(10):1147–51
Humphries SE, Morgan L (2004) Genetic risk factors for stroke and carotid atherosclerosis: insights into pathophysiology from candidate gene approaches. Lancet Neurol 3(4):227–35
Ishida T, Mizushima S, Azuma S et al (1996) Identification of TRAF6, a novel tumor necrosis factor receptor-associated factor protein that mediates signaling from an amino-terminal domain of the CD40 cytoplasmic region. J Biol Chem 271(46):28745–8
Jerrard-Dunne P, Cloud G, Hassan A, Markus HS (2003) Evaluating the genetic component of ischemic stroke subtypes: a family history study. Stroke 34(6):1364–9
Kim JS (2014) Stroke in Asia: a global disaster. Int J Stroke 9(7):856–7
Li Y, Cui LL, Li QQ et al (2014) Association between ADAM17 promoter polymorphisms and ischemic stroke in a Chinese population. J Atheroscler Thromb 21(8):878–93
Lozano R, Naghavi M, Foreman K et al (2012) Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2095–128
Lu JX, Lu ZQ, Zhang SL, Zhi J, Chen ZP, Wang WX (2014) Polymorphism in Integrin ITGA2 is Associated with Ischemic Stroke and Altered Serum Cholesterol in Chinese Individuals. Balkan Med J 31(1):55–9
Luo S, Wang F, Li Z, Deng J (2013) Effect of the +781C/T polymorphism in the interleukin-8 gene on atherosclerotic cerebral infarction, and its interaction with smoking and drinking. PLoS One 8(11):e80246
Markus HS, Labrum R, Bevan S et al (2006) Genetic and acquired inflammatory conditions are synergistically associated with early carotid atherosclerosis. Stroke 37(9):2253–9
Markus HS (2011) Stroke genetics. Hum Mol Genet 20(R2):R124–31
Miyahara T, Koyama H, Miyata T et al (2004) Inflammatory signaling pathway containing TRAF6 contributes to neointimal formation via diverse mechanisms. Cardiovasc Res 64(1):154–64
Moghimpour Bijani F, Vallejo JG, Rezaei N (2012) Toll-like receptor signaling pathways in cardiovascular diseases: challenges and opportunities. Int Rev Immunol 31(5):379–95
Murray CJ, Vos T, Lozano R et al (2012) Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859):2197–223
Muzio M, Natoli G, Saccani S, Levrero M, Mantovani A (1998) The human toll signaling pathway: divergence of nuclear factor kappaB and JNK/SAPK activation upstream of tumor necrosis factor receptor-associated factor 6 (TRAF6). J Exp Med 187(12):2097–101
Namjou B, Choi CB, Harley IT et al (2012) Evaluation of TRAF6 in a large multiancestral lupus cohort. Arthritis Rheum 64(6):1960–9
Sacco RL, Ellenberg JH, Mohr JP et al (1989) Infarcts of undetermined cause: the NINCDS Stroke Data Bank. Ann Neurol 25(4):382–90
Song HY, Regnier CH, Kirschning CJ, Goeddel DV, Rothe M (1997) Tumor necrosis factor (TNF)-mediated kinase cascades: bifurcation of nuclear factor-kappaB and c-jun N-terminal kinase (JNK/SAPK) pathways at TNF receptor-associated factor 2. Proc Natl Acad Sci U S A 94(18):9792–6
Song Y, Long Y, Long L, Zhang N, Liu Y (2014) Polymorphism Ala54Thr of fatty acid-binding protein 2 gene is not associated with stroke risk in Han population of Hunan China. Med Sci Monit 20:1751–7
Traylor M, Farrall M, Holliday EG et al (2012) Genetic risk factors for ischaemic stroke and its subtypes (the METASTROKE collaboration): a meta-analysis of genome-wide association studies. Lancet Neurol 11(11):951–62
Vasiliadis AV, Zikic M (2014) Current status of stroke epidemiology in Greece: a panorama. Neurol Neurochir Pol 48(6):449–457
Wang YC, Lin S, Yang QW (2011) Toll-like receptors in cerebral ischemic inflammatory injury. J Neuroinflammation 8:134
Wu D, Lee YC, Liu HC et al (2013) Identification of TLR downstream pathways in stroke patients. Clin Biochem 46(12):1058–64
Wu H, Arron JR (2003) TRAF6, a molecular bridge spanning adaptive immunity, innate immunity and osteoimmunology. Bioessays 25(11):1096–105
Xue H, Wang H, Song X et al (2009) Phosphodiesterase 4D gene polymorphism is associated with ischaemic and haemorrhagic stroke. Clin Sci (Lond) 116(4):335–40
Ye H, Arron JR, Lamothe B et al (2002) Distinct molecular mechanism for initiating TRAF6 signalling. Nature 418(6896):443–7
Yuan P, Liu Z, Liu M, Huang J, Li X, Zhou X (2013) Up-regulated tumor necrosis factor-associated factor 6 level is correlated with apoptosis in the rat cerebral ischemia and reperfusion. Neurol Sci 34(7):1133–8
Zhao N, Liu X, Wang Y et al (2012) Association of inflammatory gene polymorphisms with ischemic stroke in a Chinese Han population. J Neuroinflammation 9:162
Acknowledgments
Our study is supported by grants from the National Natural Science Foundation of China (Grant Nos. 81473670 and 81260594), the Guangxi National Natural Science Foundation (Grant No. 2013GXNSFAA019145), and the Scientific Research Foundation of the Guangxi Health Department (Grant No. 2012047).
Conflict of Interest
None declared.
Author information
Authors and Affiliations
Corresponding author
Additional information
Li Su, Ziwen Chen, and Yan Yan were the first coauthors.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 41 kb)
Rights and permissions
About this article
Cite this article
Su, L., Chen, Z., Yan, Y. et al. Association Between TRAF6 Gene Polymorphisms and Susceptibility of Ischemic Stroke in Southern Chinese Han Population. J Mol Neurosci 57, 386–392 (2015). https://doi.org/10.1007/s12031-015-0580-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-015-0580-z