Abstract
Bipolar disorder (BD) is a chronic psychiatric illness with an unknown etiology. Lithium is considered the cornerstone in the management of BD, though about 50–60 % of patients do not respond sufficiently to chronic treatment. Insulin-like growth factor 1 (IGF1) has been identified as a candidate gene for BD susceptibility, and its low expression has been suggested as a putative biomarker for lithium unresponsiveness. In this study, we examined the in vitro effects of insulin-like growth factor 1 (IGF-1) on lithium sensitivity in lymphoblastoid cell lines (LCLs) from lithium responder (R) and non-responder (NR) bipolar patients. Moreover, we evaluated levels of microRNA let-7c, a small RNA predicted to target IGF1. We found that exogenous IGF-1 added to serum-free media increased lithium sensitivity selectively in LCLs from NR BD patients. However, no significant differences were observed when comparing let-7c expression in LCLs from R vs. NR BD patients. Our data support a key role for IGF-1 in lithium resistance/response in the treatment of bipolar disorder.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bipolar disorder (BD) is a severe and debilitating illness that is among the leading contributors to morbidity and lost productivity in developed countries, with a prevalence of 0.8–1.2 % in the general population (Merikangas et al. 2007). Despite consistent evidence from genetic studies supporting a role of specific genes in BD etiology, the molecular bases of this disorder remain to be elucidated. Lithium salts are a well-established treatment in the management of BD; however, about 50–60 % of patients do not respond sufficiently and require a change to another mood stabilizing drug such as valproate or carbamazepine (Yildiz et al. 2011). Therefore, the neurobiological mechanisms underlying variation in therapeutic response to lithium remain a topic requiring urgent further investigation.
A number of studies have suggested a potential role of insulin-like growth factor 1 (IGF-1, also called somatomedin C) in bipolar disorder and lithium response. IGF-1 is a member of a family of hormones involved in growth and development. The protein consists of a single chain, 70 amino acids peptide, similar to insulin in structure and function. IGF-1 binds with high affinity to the IGF-1 receptor (IGF-1R) and the hybrid receptors IGF-1R/insulin receptor (IR-A) and IGF-1R/IR-B, whereas it binds with low affinity to IR-A, IR-B, and hybrid receptors IR-A/IR-B (Sciacca et al. 2012). The IGFs may affect brain function by either local tissue expression or by peripheral circulating peptides crossing the blood–brain barrier. Brain uptake of circulating IGFs involves the IGF-1R receptor (encoded by IGF1R) and the low-density lipoprotein receptor-related protein 1 (LRP1). Thus, peripheral IGFs can reach the cerebrospinal fluid as well as the hypothalamus and hippocampus, playing a role in regulation of brain function (Werner and Leroith 2014).
IGF1 has been identified as a candidate gene for susceptibility to BD (Pereira et al. 2011). In addition, studies have reported that peripheral IGF-1 mediates neurotrophic and antidepressant effects (Åberg et al. 2000), whereas this effect was inhibited by anti-IGF-I antiserum in a mice neurodegeneration model (Carro et al. 2001). In addition, decreased expression of IGFBP2, the major IGF-1 binding protein in the brain, was found in postmortem prefrontal cortex tissues of bipolar disorder patients compared with matched controls (Bezchlibnyk et al. 2007).
In a recent study comparing genome-wide mRNA expression profiles of lymphoblastoid cell lines (LCLs) from 10 lithium responder (R) and 10 lithium non-responder (NR) BD patients, we reported that IGF1 was significantly over-expressed (fold difference = 2.21; p = 0.005) in LCLs from lithium responder BD patients compared to non-responder patients (Squassina et al. 2013). In addition, recent studies showed that serum IGF-1 levels were elevated in BD patients (Palomino et al. 2013) (Liu et al. 2014). These studies suggest that IGF1 expression may serve as biomarker for lithium responsiveness in BD patients, and that IGF-1 may be implicated in lithium’s therapeutic efficacy via a yet unknown mechanism (Kim et al. 2013).
MicroRNAs (miRNAs) are short (20–24 nt) non-coding RNAs that are involved in post-transcriptional regulation of gene expression in multicellular organisms by affecting both the stability and translation of mRNAs (Ambros 2004). MiRNAs affect cellular functions, among these developmental processes (Hornstein and Shomron 2006) and drug response (Rukov and Shomron 2011). Alterations in miRNA expression have been observed in neuropsychiatric conditions, including BD (Maffioletti et al. 2014).
Interestingly, animal studies have shown that chronic lithium treatment reduced let-7c expression in the rat hippocampus (Zhou et al. 2009) and IGF-1-treated human breast adenocarcinoma cells (MCF-7) also showed decreased let-7c expression (Martin et al. 2012). These studies suggest that IGF-1 may be implicated in lithium responsiveness and that lithium and IGF-1 may converge via reducing let-7c expression.
Let-7, the first known human miRNA, and its family members are highly conserved across animal species (Roush and Slack 2008) and are upregulated during mouse brain development (Wulczyn et al. 2007). Interestingly, myMIR, a bioinformatic tool that collects the results of the most widely used miRNA target predictions algorithms (miRanda, TargetScan, RNA-hybrid, PicTar 4-way, DIANA-microT, and PITA) and ranks them through a novel consensus strategy (Corrada et al. 2011), identifies IGF1, IGFBP1, IGFBP2, and IGFBP3 as predicted targets of let-7c.
Therefore, to further investigate the involvement of IGF-1 and let-7c in lithium response in BD, we explored the role of IGF-1 in modulating in vitro lithium sensitivity in the cohort of lymphoblastoid cell lines from responder and non-responder BD patients used in our genome-wide expression study (Squassina et al. 2013), and measured let-7c expression in correlation with IGF-1 mRNA levels in the same cohort.
Materials and Methods
Patients and Cell Cultures
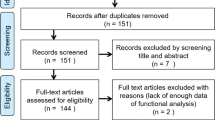
For the study on the effects of IGF-1 on lithium sensitivity, we used LCLs of 17 female patients with a diagnosis of BD type I (BDI), arbitrarily selected from an existing collection recruited at the Lithium Clinic of the Clinical Psychopharmacology Centre of the University Hospital of Cagliari, Italy. Of the 17 patients included in this study, eight were lithium responders (R) and nine were non-responders (NR), based on the Retrospective Criteria of Long-Term Treatment Response in Research Subjects with Bipolar Disorder’ scale (Grof et al. 2002).
Expression of let-7c was measured in the same LCLs as in Squassina et al. (2013), in order to be able to test the correlation between levels of IGF1 mRNA and let-7c. Samples included LCLs from ten bipolar subjects R to lithium and ten bipolar NR. Methods to establish these cell lines were described elsewhere (Squassina et al. 2013). At the time of enrollment, all participants signed written informed consent. The research protocol followed the principles of the Declaration of Helsinki and was approved by the local Ethics Committees.
Cell Proliferation Assays
Growth inhibition of LCLs was examined by exposure to 10 mM lithium (chloride salt) for 3 days in RPMI-1640 medium supplemented with either 10 % fetal bovine serum (FBS), 2 % FBS, or 4 % of albumin-free serum replacement (Biogro-2, Biological Industries, Beth-Haemek, Israel; (Orengo et al. 2014). Testing lithium in a range of 1–15 mM in standard growing conditions (RPMI-1640 with 10 % FBS) revealed that the IC50 of lithium-mediated growth inhibition was 10 mM (Fig. 1a). A concentration of 10 mM lithium and an exposure period of 3 days were chosen for the phenotypic comparisons, as this concentration is close to the IC50 where assay accuracy is highest, and 3 days exposure allows accurate measurements of effects on cell growth (Morag et al. 2010; Oved et al. 2013). Growth inhibition of LCLs was also examined by exposure to paroxetine (an antidepressant drug) for 3 days in RPMI-1640 medium supplemented with either 10 % FBS or 4 % of Biogro-2. The 10 μM paroxetine concentration was chosen according to Morag et al. (2011).
a Growth inhibition by various lithium concentrations in an individual LCL (72 h in vitro exposure, see “Materials and Methods”). Lithium’s IC50 values were 10, 12, and >15 mM in media containing 10 % FBS, 2 % FBS, or 4 % serum-free Biogro-2 supplement, respectively. b Growth inhibition induced by 10 mM lithium (72 h) in 4 % Biogro-2, 2 % FBS, and 10 % FBS media in a representative sample of eight LCLs. More than four independent experiments were conducted on these representative samples. Bars indicate the average ± SD of three replicates
Cells under optimal growth conditions were counted with a microscope slide, diluted to a concentration of 250,000 cells/ml and incubated in 96-well plates (Costar ®, Sigma-Aldrich) in a volume of 100 μl for 3 days, with lithium added in a volume of 10 μl phosphate-buffered saline (PBS) in three replicate wells, and six replicates for the controls (10 μl PBS). In the other three replicate wells, 200 ng/ml IGF-1 (PeproTech Ltd, Rocky Hill, NJ, USA) was added in combination with 10 mM lithium in serum-free (4 % Biogro-2) medium. The edges of the plates were not used for experiments and contained RPMI-1640 medium without cells for ensuring appropriate humidity. On the third day, activated XTT reagent (Biological Industries, Israel; Catalog number: 20-30-1000A; volume of 50 μl) was added to each well (including blank wells containing RPMI-1640 medium alone). Following 6 h of further incubation, absorption was measured using an ELISA reader (Bio-Rad microplate reader model 680; Bio-Rad Laboratories, CA, USA) at a wavelength of 450 nm and a reference absorbance of 655 nm. As previously demonstrated, color generation by the XTT method is a reliable reflection of cell numbers compared with direct cell counting (Morag et al. 2010).
Quantitative Real-Time PCR
Let-7 reverse transcription was carried out using Applied BiosystemsTaqMan® microRNA assays. Individual TaqMan® MicroRNA Assays were performed with TaqMan Universal Master Mix no UNG, using hsa-let-7c (000379) assay and U6 snRNA (001973) as endogenous control. Quantitative real-time PCRs (qRT-PCRs) were performed according to the manufacturer’s instructions with all samples run in duplicates. Replicates were omitted if threshold cycle (Ct) standard deviation was greater than 1. Fold differences were obtained by using the formula 2-∆∆Ct.
Quantification of IGF-1 in Conditioned Medium
IGF-1 levels were measured by an ELISA method using the human IGF-1 Kit (R&D System, MN, USA), according to the manufacturer’s instructions. LCLs proliferated well for 14 days in serum-free RPMI medium supplemented with 4 % Biogro-2. Samples of the conditioned media (after removal of cells by centrifugation) were concentrated up to 18-fold by Vivaspin 2 ultrafiltration tubes with 5 kDa cutoff (Sartorious Stedim Biotech, Goettingen, Germany) according to the manufacturer’s protocol. All IGF-1 measurements were performed in duplicate.
Results
Lithium Sensitivity in LCLs from Responders and Non-responders
The growth inhibition induced by lithium (in the range of 1–15 mM; 72 h) was tested under three different experimental conditions (RPMI-1640 media containing 10 % FBS, 2 % FBS, or serum-free medium supplemented with 4 % Biogro-2) (Fig. 1a, b). No differences in lithium sensitivity between LCLs responder (R) and non-responder (NR) patients were observed in either of these media (p = 0.41, p = 0.66, p = 0.42, respectively. Fig. 2). However, in both R and NR LCLs, we observed a significantly higher lithium sensitivity in media containing 10 % FBS compared with serum-free media. Intermediate lithium sensitivity levels were observed in media containing 2 % FBS (Figs. 1b and 2). To test the hypothesis that proteins contained in FBS interact with cell proteins involved in lithium’s pathway, we compared the sensitivity of LCLs to 10 uM paroxetine in the same media compositions. We observed an opposite effect: sensitivity was higher in serum-free medium compared with 10 % FBS (20.7 and 46.1 % in serum-free and serum-containing media, respectively; p = 1.9 E-8) (Supplementary Fig S1).
Effect of IGF-1 on Lithium Sensitivity
IGF-1 is present in FBS at an estimated concentration of 30 μg/L (Honegger and Humbler 1986) but not in serum-free supplements. We therefore compared lithium sensitivity (10 mM, 72 h) of LCLs from R and NR patients in the presence or absence of IGF-1 (200 ng/ml, equal to 0.026 uM) in serum-free medium (containing 4 % Biogro-2) (Fig. 3a). Human serum has been reported to contain high concentration of IGF-1, and the estimated normal range in adults is ~200 ng/ml (Singh and Armstrong 1997).
a Growth inhibition (%) induced by 10 mM lithium and 10 mM lithium + 200 ng/ml IGF-1 in medium containing 4 % Biogro-2 in LCLs from R and NR BD patients. Bars indicate the average ± SD of the percentage of growth inhibition of three replicates. b Average of growth inhibition in NR induced by 10 mM lithium and 10 mM lithium + IGF1 200 ng/ml. Bars indicate the average ± SD of the growth inhibition (%)
Collectively, when using serum-free conditions, exogenous IGF-1 enhanced lithium sensitivity in NR (p = 0.01; Fig. 3b) but not in R LCLs (p = 0.5). As expected, no effects of exogenous IGF-1 were observed when LCLs were exposed to lithium in FBS-containing media. To quantify the effect of IGF-1, Delta values were calculated for each cell line (Delta 1 = effect of 10 % FBS on Li sensitivity; Delta 2 = effect of IGF1 on Li sensitivity (72 h) measured in the absence of FBS) (Delta1 = %GI in 10 % FBS- %GI in 4 % Biogro-2; Delta2 = %GI in 4 % Biogro-2 + IGF1- %GI in 4 % Biogro-2). We found that the addition of exogenous IGF-1 to serum-free medium affected the lithium-mediated growth inhibition to a larger degree in LCLs from NR compared to R BD patients (p = 0.009) (Fig. 4a). In contrast, no difference in lithium-mediated growth inhibition for NR and R LCLs was observed upon addition of 10 % FBS to culture media (p = 0.1) (Supplementary Fig. S2). Moreover, in the presence of IGF-1, NR LCLs exhibited higher lithium sensitivity compared with R LCLs (p = 0.034; Fig. 4b). No such differences were observed in the absence of IGF-1 in either serum-containing or serum-free media.
a Effect of IGF-1 on lithium sensitivity in serum-free media: bars indicate the average ± SD of Delta 2 in R and NR BD patients. b Bars indicate the average ± SD of growth inhibition percent induced by 10 mM lithium + 200 ng IGF-1 in serum-free medium containing 4 % Biogro-2 in LCLs from R and NR BD patients
In a recent genome-wide expression study, we reported higher IGF1 expression levels in LCLs from lithium responder BD patients compared with non-responders (Squassina et al. 2013). As the previous study included LCLs from 10 BD responders and non-responders each, while the current study compared LCLs from 8 responders and 9 non-responders, the IGF1 expression levels from the current cohort are presented in Fig. S3. As shown, IGF1 expression levels were higher (1.4-fold, p = 0.008 Z = −2.64) in the lithium responder LCLs.
MiRNA let-7c Levels and IGF1 mRNA Levels Correlation
We observed a trend for higher let-7c expression in LCLs from NR compared to R BD patients (FC = 1.6). However, the difference did not reach the significance threshold (p = 0.1) (Fig. S4). Lithium treatment did not affect let-7c expression in any LCL group (HC FC = 1.03 p = 0.2; R FC = 1.15 p = 0.88; and NR FC = 1.06 p = 0.8). Moreover, we observed a trend toward negative correlation between let-7c and IGF-1 mRNA levels (Pearson, r = −0.3682, p = 0.054). There was no difference in this correlation between R and NR.
IGF-1 Levels in Conditioned Media
We could not detect IGF-1 in medium conditioned by the BD LCLs from either R or NR BD patients. When assayed by a commercial human IGF-1 ELISA kit (see “Materials and Methods”), even 18-fold concentrated conditioned medium samples gave OD readings below the lowest standard of 94 pg/ml. We can therefore conclude that IGF-1 levels in media conditioned by LCLs using our experimental conditions are probably below 5 pg/ml.
Discussion
Several studies have implicated IGF1 and its encoded protein in the biology of BD (Palomino et al. 2013; Kim et al. 2013; Liu et al. 2014), in antidepressant response (Åberg et al. 2000) and lithium response (Squassina et al. 2013). In this study, we aimed to further investigate the role of IGF-1 in lithium response in BD patients. To this aim, LCLs from lithium R and NR BD patients were exposed to 10 mM lithium for 3 days under three different media conditions (containing different amounts of insulin and IGF1) and the in vitro lithium sensitivity was evaluated by measuring its effect on LCLs growth. The estimated amount of insulin in different media conditions were 0.68 uM in 4 % Biogro-2, 1.3 uM in 2 % FBS; and 6.9 uM in 10 % FBS. We did not find differences in lithium sensitivity between R and NR LCLs in either of these media; however, we observed a significantly higher lithium sensitivity in media containing 10 % FBS compared with serum-free media, whereas intermediate sensitivity levels were observed in media with 2 % FBS (Figs. 1 and 2). To test the hypothesis that component(s) present in FBS interact with lithium’s cellular pathway, thereby affecting its growth inhibition capacity, we compared the sensitivity of LCLs to 10 μM paroxetine (an antidepressant drug) in the same media compositions and observed an opposite effect (Fig. S1). The latter finding is not surprising, as cells are expected to show higher growth inhibition sensitivity for tested drugs in the absence of the growth-promoting protein and lipid hormones present in FBS. Moreover, many hydrophobic drugs bind to serum albumin so that their free concentrations are reduced in FBS-containing media. Thus, the lower sensitivity of LCLs to lithium in serum-free conditions was surprising. Due to the suggested involvement of IGF-1 in BD pathophysiology, and considering that IGF-1 is present in FBS but not in serum-free media supplements, we tested the in vitro effect of 200 ng/ml IGF-1 on lithium sensitivity of LCLs from R and NR BD patients. We observed that when added to serum-free medium, IGF-1 significantly enhanced lithium sensitivity in NR but not in R BD LCLs. This effect, as expected, was not observed in FBS-containing medium.
Using hypothesis-free genome-wide expression microarray experiments, Squassina and collaborators (Squassina et al. 2013) showed that IGF1 mRNA levels were on average 2.21-fold lower in LCLs from lithium NR BD patients compared to R patients. Together with the results presented in the current study, it seems that the in vitro addition of exogenous IGF-1 affects lithium sensitivity only in LCLs from NR BD patients that express less IGF1. We assume that in LCLs from R patients endogenous IGF-1 levels are constitutively optimal, therefore masking the effect of exogenously added IGF-1. Thus, our findings support a role for IGF-1 in lithium resistance/response in the treatment of BD, and possibly, in the therapeutic pathway of lithium as a mood-stabilizer drug.
Of note, IGF-1 is a key player in cancer, including breast and endometrial cancers (Sarkissyan et al. 2014; Werner and Leroith 2014), as it acts as a mitogen to augment tumorigenesis through the regulation of MAPK and AKT signaling pathways. Of interest, both of these pathways are inhibited by lithium. Specific miRNAs regulating IGF-1 signaling in the estrogen receptor positive MCF-7 breast cancer cell line have been identified, and it was demonstrated that IGF-1 decreased let-7c expression (Martin et al. 2012). To test if the lower endogenous levels of IGF1 mRNA expression observed by Squassina et al. (2013) in LCLs from R BD patients were correlated with higher let-7c levels, we measured miRNA let-7c expression and observed a trend of higher let-7c expression in LCLs from NR BD patients (FC = 1.6; p = 0.1; Supplementary Fig. S4). Moreover, our data showed a trend for an inverse correlation between let-7c and IGF-1 expression, though there was no difference between R and NR. Lithium appeared not to influence expression of let-7c in any of the tested groups.
The study is based on a small cohort of LCLs from 17 BD patients (8 lithium responders and 9 non-responders). Our findings thus need to be reproduced by a larger replication cohort. Yet, it should be noted that all cell lines are from female BD patients with identical ethnicity (Sardinian) and recruited and diagnosed by the same clinic (see “Materials and Methods”). Moreover, the lithium response used for the current study was evaluated with the Alda scale (Manchia et al. 2013), a standardized and validated tool that we also used in a previous study reporting potential SNP markers for lithium response (Squassina et al. 2011).
In conclusion, we demonstrate that exogenous IGF-1 added to serum-free media increases lithium sensitivity selectively in LCLs from NR BD patients, supporting a key role of IGF-1 in lithium resistance/response in the treatment of bipolar disorder. Further studies in independent samples and using further molecular tools are warranted to confirm the role of IGF-1 in lithium’s therapeutic action.
Abbreviations
- BD:
-
Bipolar disorder
- IGF-1:
-
Insulin-like growth factor 1
- LCLs:
-
Lymphoblastoid cell lines
- R:
-
Responders
- NR:
-
Non-responders
- IGF1R :
-
IGF-1 receptor
- IR:
-
Insulin receptor
- LRP1:
-
Receptor-related protein 1
- IGFBP2 :
-
Insulin-like growth factor binding protein 2
- miRNAs:
-
MicroRNAs
- IGFBP1 :
-
Insulin-like growth factor binding protein 1
- IGFBP3 :
-
Insulin-like growth factor binding protein 3
- qRT-PCR:
-
Quantitative real-time-PCR
References
Åberg MAI, Åberg ND, Hedba H et al (2000) Peripheral infusion of IGF-I selectively induces neurogenesis in the adult rat hippocampus. Endocrinology 20:2896–2903
Ambros V (2004) The functions of animal microRNAs. Nature 431:350–355
Bezchlibnyk YB, Xu L, Wang J-F, Young LT (2007) Decreased expression of insulin-like growth factor binding protein 2 in the prefrontal cortex of subjects with bipolar disorder and its regulation by lithium treatment. Brain Res 1147:213–217. doi:10.1016/j.brainres.2007.01.147
Carro E, Trejo JL, Busiguina S, Torres-aleman I (2001) Circulating insulin-like growth factor I mediates the protective effects of physical exercise against brain insults of different etiology and anatomy. J Neurosci 21:5678–5684
Corrada D, Viti F, Merelli I et al (2011) myMIR: a genome-wide microRNA targets identification and annotation tool. Brief Bioinform 12:588–600. doi:10.1093/bib/bbr062
Grof P, Ph D, Duffy A et al (2002) Is response to prophylactic lithium a familial trait? J Clin Psychiatry 63:942–947
Honegger A, Humbel RE (1986) Insulin-like growth factors I and II in fetal and adult bovine serum. Purification, primary structures, and immunological cross-reactivities. J Biol Chem 261:569–575
Hornstein E, Shomron N (2006) Canalization of development by microRNAs. Nat Genet 38(Suppl):S20–S24. doi:10.1038/ng1803
Kim Y-K, Na K-S, Hwang J-A et al (2013) High insulin-like growth factor-1 in patients with bipolar I disorder: a trait marker? J Affect Disord 151:738–743. doi:10.1016/j.jad.2013.07.041
Liu X, Zhang T, He S et al (2014) Elevated serum levels of FGF-2, NGF and IGF-1 in patients with manic episode of bipolar disorder. Psychiatry Res 218:54–60. doi:10.1016/j.psychres.2014.03.042
Maffioletti E, Tardito D, Gennarelli M, Bocchio-Chiavetto L (2014) Micro spies from the brain to the periphery: new clues from studies on microRNAs in neuropsychiatric disorders. Front Cell Neurosci 8:75. doi:10.3389/fncel.2014.00075
Manchia M, Adli M, Akula N et al (2013) Assessment of response to lithium maintenance treatment in bipolar disorder: a Consortium on Lithium Genetics (ConLiGen) Report. PLoS One 8(6):e65636
Martin EC, Bratton MR, Zhu Y et al (2012) Insulin-like growth factor-1 signaling regulates miRNA expression in MCF-7 breast cancer cell line. PLoS One 7:e49067. doi:10.1371/journal.pone.0049067
Merikangas KR, Akiskal HS, Angst J et al (2007) Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey replication. Arch Gen Psychiatry 64:543–552. doi:10.1001/archpsyc.64.5.543
Morag A, Kirchheiner J, Rehavi M, Gurwitz D (2010) Human lymphoblastoid cell line panels: novel tools for assessing shared drug pathways. Pharmacogenomics 11:327–340
Morag A, Pasmanik-Chor M, Oron-Karni V (2011) Genome-wide expression profiling of human lymphoblastoid cell lines identifies CHL1 as a putative SSRI antidepressant response biomarker. Pharmacogenomics 171–184
Orengo AM, Di Carlo E, Comes A et al (2014) Tumor cells engineered with IL-12 and IL-15 genes induce protective antibody responses in nude mice. J Immunol 171:569–575. doi:10.4049/jimmunol.171.2.569
Oved K, Morag A, Pasmanik-Chor M et al (2013) Genome-wide expression profiling of human lymphoblastoid cell lines implicates integrin beta-3 in the mode of action of antidepressants. Transl Psychiatry 3:e313. doi:10.1038/tp.2013.86
Palomino A, González-pinto A, Martinez-cengotitabengoa M et al (2013) Progress in neuro-psychopharmacology & biological psychiatry relationship between negative symptoms and plasma levels of insulin-like growth factor 1 in first-episode schizophrenia and bipolar disorder patients. Prog Neuropsychopharmacol Biol Psychiatry 44:29–33. doi:10.1016/j.pnpbp.2013.01.008
Pereira ACP, McQuillin A, Puri V et al (2011) Genetic association and sequencing of the insulin-like growth factor 1 gene in bipolar affective disorder. Am J Med Genet B Neuropsychiatr Genet 156:177–187. doi:10.1002/ajmg.b.31153
Roush S, Slack FJ (2008) The let-7 family of microRNAs. Trends Cell Biol 18:505–516. doi:10.1016/j.tcb.2008.07.007
Rukov JL, Shomron N (2011) MicroRNA pharmacogenomics: post-transcriptional regulation of drug response. Trends Mol Med 17:412–423. doi:10.1016/j.molmed.2011.04.003
Sarkissyan S, Sarkissyan M, Wu Y et al (2014) IGF-1 regulates Cyr61 induced breast cancer cell proliferation and invasion. PLoS One 9:e103534. doi:10.1371/journal.pone.0103534
Sciacca L, Le Moli R, Vigneri R (2012) Insulin analogs and cancer. Front Endocrinol (Lausanne) 3:21. doi:10.3389/fendo.2012.00021
Singh B, Armstrong DT (1997) Insulin-like growth factor-1, a component of serum that enables porcine cumulus cells to expand in response to follicle-stimulating hormone in vitro. Biol Reprod 1375:1370–1375
Squassina A, Manchia M, Borg J et al (2011) Evidence for association of an ACCN1 gene variant with response to lithium treatment in Sardinian patients with bipolar disorder. Pharmacogenomics 12:1559–1569
Squassina A, Costa M, Congiu D et al (2013) Insulin-like growth factor 1 (IGF-1) expression is up-regulated in lymphoblastoid cell lines of lithium responsive bipolar disorder patients. Pharmacol Res 73:1–7. doi:10.1016/j.phrs.2013.04.004
Werner H, Leroith D (2014) Insulin and insulin-like growth factor receptors in the brain: Physiological and pathological aspects. Eur Neuropsychopharmacol 1–7. doi: 10.1016/j.euroneuro.2014.01.020
Wulczyn FG, Smirnova L, Rybak A et al (2007) Post-transcriptional regulation of the let-7 microRNA during neural cell specification. FASEB J 21:415–426. doi:10.1096/fj.06-6130com
Yildiz A, Vieta E, Leucht S, Baldessarini RJ (2011) Efficacy of antimanic treatments: meta-analysis of randomized, controlled trials. Neuropsychopharmacology 36:375–389. doi:10.1038/npp.2010.192
Zhou R, Yuan P, Wang Y et al (2009) NIH Public Access 34:1395–1405. doi:10.1038/npp.2008.131.Evidence
Acknowledgments
The authors thank the patients involved in the study for the generous collaboration. This study was supported by the US Israel Binational Science Foundation (BSF) Grant No. 2013223 (to DG). DG is supported by the Shalom and Varda Yoran Institute for Human Genome Research at Tel Aviv University. Elena Milanesi is a post-doctoral fellow supported by the Shabbetai Donnolo Fellowships between Italy and Israel. MG and Elisabetta Maffioletti are supported by grants from the Italian Ministry of Health (Ricerca Corrente). AS is a post-doctoral fellow funded by a grant from the Sardinia Regional Government (P.O.R. Sardegna F.S.E. Operational Program of the Autonomous Region of Sardinia, European Social Fund 2007-2013–Axis IV Human Resources, Objective l.3, Line of Activity l.3.1.).
Author information
Authors and Affiliations
Corresponding authors
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Fig. S1
(A) Growth inhibition (%) induced by 10 μM paroxetine (72 h) in media containing 10 % FBS or 4 % Biogro-2. Bars indicate the average ± SD of the growth inhibition of three replicates. (B) Average of growth inhibition induced by 10 μM paroxetine in 4 % Biogro-2 and 10 % FBS media. Bars indicate the average ± SD of the growth inhibition. (DOCX 63 kb)
Fig. S2
Effect of 10 % FBS on lithium sensitivity, Bars indicate the average of Delta 1 ± SD in R and NR BD patients. (DOCX 22 kb)
Fig. S3
Relative expression levels of IGF-1. Relative expression levels were measured by means of the comparative Ct method (ΔΔ Ct) using GAPDH as endogenous control. Fold change of the difference between R and NR was calculated with 2 − ΔΔCt equation. Differences between R and NR were analyzed with the Mann–Whitney U test. (For more details see Squassina et al., 2013) (DOCX 40 kb)
Fig. S4
Expression of let-7c in LCLs from 10 healthy controls, 10 R BD and 10 NR BD patients. U6 assay was used as endogenous control. Bars represent the fold difference compared with healthy controls ± SD. (DOCX 21 kb)
Rights and permissions
About this article
Cite this article
Milanesi, E., Hadar, A., Maffioletti, E. et al. Insulin-like Growth Factor 1 Differentially Affects Lithium Sensitivity of Lymphoblastoid Cell Lines from Lithium Responder and Non-responder Bipolar Disorder Patients. J Mol Neurosci 56, 681–687 (2015). https://doi.org/10.1007/s12031-015-0523-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-015-0523-8