Abstract
Diabetic retinopathy (DR), a common complication of diabetes, remains a major cause of blindness among population. Considerable amounts of evidences suggest the involvement of inflammatory process in this pathology. Increased levels of proinflammatory cytokines, including interleukin-1β (IL-1β), were found in the vitreous of diabetic patients and in the retina of diabetic rats. However, in this context, no attention has been given to the other main IL-1 family members: IL-1α, two transmembrane receptors IL-1RI and IL-1RII and the natural antagonist receptor IL-1Ra. Despite that they actively participate in the IL-1-mediated inflammation process, their implication in DR has not been described. Thus, we investigated by Western blot and confocal laser scanning microscopy analysis the effect of hyperglycemia on expression of IL-1 family members in retinal layers, using an in vivo model of type 1 diabetes. It was induced in adult rats by intraperitoneal injection of streptozotocin (STZ). Exposure to hyperglycemia induces a significant increase in the protein expression of IL-1β, IL-1RI, IL-RII and IL-1Ra but not of IL-1α. Moreover, high glucose alters their distribution pattern in the rat’s retinal layers. Among these latter, the most compromised are the photoreceptor, the inner plexiform and ganglion cell layers. These findings support previous data demonstrating the involvement of inflammation in DR and suggest new pharmacological approaches for the treatment of this pathology.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Diabetic retinopathy (DR) is a major cause of visual impairment and acquired blindness among patients with type 1 and type 2 diabetes (Saydah et al. 2004; Hoerger et al. 2008). It has mainly been considered as a microvascular disease, caused by a range of hyperglycemia-linked pathways (Safi et al. 2014) and characterized by basement membrane thickening of retinal vessels, loss of pericytes and endothelial cells, blood–retinal barrier (BRB) breakdown (Cunha-Vaz 2004; Scuderi et al. 2013). However, some evidences suggest that neurodegenerative processes may occur before of any detectable microvascular alterations in the retina. Indeed, all retinal cell types are susceptible to hyperglycemia-induced biochemical alterations that lead to oxidative stress, apoptosis and inflammation (Lieth et al. 2000; Giunta et al. 2012). Inflammation has been recognized as a trigger element in the early and late stages of DR (Kern 2007; Feenstra et al. 2013). In fact, varieties of physiological and molecular abnormalities, consistent with inflammation, have been found in the retinas or vitreous humor of diabetic animals and patients. These include macroglial and microglial activation, leukostasis, increased vascular permeability, vasoactive peptides (Chakrabarti et al. 2000; Rungger-Brandle et al. 2000; Krady et al. 2005) and increased levels of inflammatory cytokines, such as interleukin-1beta (IL-1β) and tumor necrosis factor-α (TNF-α) (Abu el Asrar et al. 1992; Yuuki et al. 2001; Demircan et al. 2006; Bucolo et al. 2012). Interesting reports regarding a correlation between dysfunctional IL-1β signaling with the incidence of many pathologies, including DR (Carmo et al. 2000; Kowluru and Odenbach 2004; Krady et al. 2005), have led us to focus our attention to the other members of this family, to investigate their involvement during early phase of diabetes.
The IL-1’s family members include various ligands with agonist activity. Among these, the most studied are IL-1α and IL-1β, both pro-inflammatory cytokines, and the endogenous receptor antagonist IL-1Ra (Arend et al. 2008). All IL-1’s ligands are produced as pro-peptides, while IL-1β requires proteolytic cleavage for its activity; IL-1α possesses a limited activity prior to processing (Kim et al. 2013). The IL-1Ra is released by the cell, as an active molecule of 25 kDa without a requirement for processing. Once released and cleaved, IL-1 ligands elicit a multitude of effects on target cells, binding to two different types of transmembrane receptors: IL-1R type I and IL-1R type II (Sims and Dower 1994; Rothwell and Luheshi 2000). IL-1RII is a decoy receptor, which lacks the cytoplasmatic domain and cannot signal but binds to IL-1RI by limiting the biological availability of this latter. IL-1Ra competes either with IL-1α or β to bind IL-1 type I receptor thus inhibiting any signal transduction (Irikura et al. 2002). Although IL-1β has already been described in the literature as a mediator in DR, so far there are no data about the involvement of other IL-1’s family members in the early stages of retinal damage induced by hyperglycemia (Carmo et al. 2000; Kowluru and Odenbach 2004; Krady et al. 2005).
In the present paper, to characterize the involvement of these cytokines in early phases of hyperglycemia, it has been analyzed the expression of IL-1α, IL-1β, IL-1Ra and relative receptors in an in vivo model of DR, induced in rats following intraperitoneal injection of streptozotocin (STZ).
Our findings suggest that these cytokines play distinct roles in the context of retinal damage during DR. Although systemic glycemic control remains the most effective approach to control retinal degeneration, the better characterization of IL-1’s signaling system in DR might provide new insight for the development of a more targeted therapeutic approach.
Materials and Methods
Rats
Male Sprague–Dawley rats, 3 months old, weighing approximately 200 g each, obtained from Charles River (Calco, Italy) were used for the present study. All the animals were treated according to the Association for Research in Vision and Ophthalmology (ARVO) Statement for the Use of Animals in Ophthalmic and Vision Research. The animals were fed with standard laboratory chow and were allowed free access to water in an air-conditioned room with a 12 h light/12 h dark cycle. Final group sizes for all measurements were n = 6–9.
Induction of Diabetes
Diabetes was induced with a single intraperitoneal injection of STZ (Sigma-Aldrich, St. Louis, MO, USA) as previously described (Bucolo et al. 2012). Briefly, after 12 h of fasting, a group of animals received a single injection of STZ (60 mg/kg body weight) in 10 mM sodium citrate buffer, pH 4.5 (1 mL/kg dose volume). Nondiabetic animals were fasted and received citrate buffer alone. Twenty four hours post STZ injection, blood glucose levels were measured and rats showing blood glucose levels greater than 250 mg/dL were considered as diabetic (Sedaghat et al. 2011) and selected for the study. We monitored throughout the study the diabetic state by evaluating glycemia daily using a blood glucose meter (Accu-CheckActive; Roche Diagnostic, Milan, Italy) and by the weight loss. All experiments were performed 3 weeks after the induction of diabetes. For subsequent experiments, rats were killed with a lethal intraperitoneal (i.p.) dose of sodium pentobarbital. Retinas were immediately removed and homogenized in ice cold buffer for Western blot analysis, and others were fixed in 4 % paraformaldehyde for histological and immunohistochemical analysis.
Measurement of Blood–Retinal Barrier Breakdown
In a separate set of animals, the BRB breakdown was measured using Evans blue dye (Sigma-Aldrich, St. Louis, MO) 3 weeks post STZ injection as previously reported (Bucolo et al. 2009). Rats were killed, and the retinas were carefully dissected and thoroughly dried in a concentration/drying system (SpeedVac; Thermo Fisher Scientific, Milan, Italy). The dry weight was used to normalize the quantitation of Evans blue leakage. Evans blue was extracted from each retina and the samples used for spectrophotometric measurements. The background-subtracted absorbance was determined by measuring each sample at 620 nm (the maximum absorbance for Evans blue in formamide) and 740 nm (the minimum absorbance). The concentration of dye in the extracts was calculated from a standard curve of Evans blue in formamide. BRB breakdown was calculated using the following equation, with results being expressed in μL plasma × g retina dry weight−1 × h−1.
We expressed results as percentage of control.
Western Blot Analysis
Western blot analysis was performed to determine the relative levels of the interleukin-1 family ligands and receptors using specific antibodies. Analysis was performed as previously described by D’Amico et al. (2013). Briefly, proteins were extracted with buffer containing 20 mM Tris (pH 7.4), 2 mM EDTA, 0.5 mM EGTA, 50 mM mercaptoethanol, 0.32 mM sucrose and a protease inhibitor cocktail (Roche Diagnostics) using a Teflon-glass homogenizer and then sonicated twice for 20 s using an ultrasonic probe, followed by centrifugation at 10,000 g for 10 min at 4 °C. The Quant-iT Protein Assay Kit (Invitrogen) determined protein concentrations. Sample proteins (30 μg) were diluted in 2× Laemmli buffer (Invitrogen, Carlsbad, CA, USA), heated at 70 °C for 10 min and then separated on a Biorad Criterion XT 4–15 % Bis-tris gel (Bio-Rad) by electrophoresis and then transferred to a nitrocellulose membrane (Bio-Rad). Blots were blocked using the Odyssey Blocking Buffer (LI-COR Biosciences) and probed with appropriate antibodies: rabbit anti-β-tubulin (sc-9104, Santa Cruz Biotechnology; 1:500), rabbit anti-IL-1α (sc-7929, Santa Cruz Biotechnology; 1:200); goat anti-IL-1β (sc-1250, Santa Cruz Biotechnology; 1:200), rabbit anti-IL-1RI (sc-688, Santa Cruz Biotechnology; 1:200), rabbit anti-IL-1RII (sc-292522, Santa Cruz Biotechnology; 1:200) and mouse anti-IL-Ra (sc-376094, Santa Cruz Biotechnology; 1:200). The secondary antibody goat anti-rabbit IRDye 800CW (#926-32211; LI-COR Biosciences), donkey anti-goat IRDye 800CW (#926-32214 LI-COR) and goat anti-mouse IRDye 680CW (#926-68020D; LI-COR Biosciences) were used at 1:20,000.
Blots were scanned using an Odyssey Infrared Imaging System (Odyssey). Densitometric analysis of Western blot signals was performed at nonsaturating exposures and analyzed using the ImageJ software (NIH, Bethesda, MD; available at http://rsb.info.nih.gov/ij/index.html).
Immunolocalization
Eyes were enucleated and fixed overnight with 4 % paraformaldehyde in 0.1 M sodium phosphate (pH 7.6). Analysis was performed as previously described by (Giunta et al. 2012). Before immunofluorescence staining, paraffin-embedded retina sections (14 μm) mounted on glass slides were dewaxed in xylene and rehydrated through graded alcohols. Sections were put into Rodent Decloaker 1X retrieval solution (RD913, Biocare Medical) in a slide container and then incubated with the anti IL-1β, IL-1α, IL-1R type I and II, IL-1Ra primary antibodies. To establish signal specificity, in a preliminary experiment, each antibody was preincubated with an excess of antigen (blocking peptide). No signal was revealed in sections incubated with neutralized antibody. This confirmed that signal detected by each antibody was not an artifact (data not shown). Tissue sections were then incubated with Alexa Fluor 488 goat anti-rabbit and Alexa Fluor 488 donkey anti-goat secondary antibodies, respectively for 1.5 h at room temperature and shielded from light. Diamidino-2-phenylindole (DAPI) was used to stain nuclei (#940110 Vector Laboratories).
Images of the central retina were taken with a confocal laser scanning microscope (CLSM) (Zeiss LSM700 with a × 20, ×40, and × 63 objectives), as previously described (D’Amico et al. 2013) and analyzed using the ZEN 2011 software. Experiments were repeated at least three times to confirm results.
Statistical Analysis
Statistical analyses were performed using specific software GraphPad Prism 5. Paired t tests were used to determine whether differences were significant. The level of significance for all statistical tests was p ≤ 0.05.
Results
Changes in the Body Weight and Blood Glucose Levels After 3 weeks of STZ Administration
Table 1 shows the effects of STZ treatment on body weight and nonfasting blood glucose levels in rats after 3 weeks. Body weight and glycemia of rats before treatments were approximately 200 g and 100 mg/dL respectively. The statistical analysis revealed a significant decrease in body weight 3 weeks after STZ injection (p < 0.01 vs. nondiabetic control group). Three weeks after onset of diabetes, blood glucose values in diabetic rats were significantly (p < 0.01) higher than corresponding values in nondiabetic rats (391 ± 35 and 98 ± 18 mg/dL respectively).
Blood–Retinal Barrier Breakdown
Increased BRB permeability is an early event in rats with hyperglycemia. Evans blue permeability was measured 3 weeks after STZ diabetes induction. Figure 1 shows that Evans blue leakage from retinas of diabetic rats was twofold higher than that from nondiabetic rats (p < 0.01).
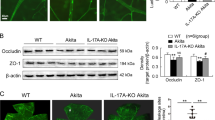
Effects of STZ-Induced Diabetes on IL-1 Family Member Protein Expression
Western blot analysis showed significantly higher expression of IL-1 receptor type I and IL-1β diabetic rat retinas compared to nondiabetic (***p < 0.001). Hyperglycemia resulted also in a small but significant induction of the IL-1 receptor type II and of the receptor antagonist IL-Ra (respectively *p < 0.05 and **p < 0.01 vs. retina from nondiabetic rats), but no effect had on the expression level of IL-1α (Fig. 2a, b). Results were quantified and are the mean ± SEM, percent of control (n = 6 animals; *p < 0.05, **p < 0.01 and ***p < 0.001 compared with control, Student’s t test).
Hyperglycemia increases the proinflammatory IL-1 signaling, in rat retina. Rats were injected with STZ (60 mg/kg, i.p.), and levels of interleukin-1 alpha (IL-1α), interleukin-1beta (IL-1β), interleukin-1 receptor antagonist (IL-1Ra), interleukin receptor type I (IL1-RI) and type II (IL1-RII) were determined by Western blot analysis. Levels of total IL-1α, IL-1β, IL-1Ra, IL1-RI and IL1-RII were determined to control (β-tubulin) for loading differences. a Representative Western blot images for each protein are shown. b Results were quantified and are the mean ± SEM, percent of control (n = 6 animals; *p < 0.05, **p < 0.01 and ***p < 0.001 compared with control, Student’s t test)
Regional Distribution of IL-1 Family Members
The distribution of the IL-1α, IL-1β, IL-1Ra, IL-1RI and IL-1RII was detected, using specific antibodies, in the retina of rats after 3 weeks of STZ injection.
The IL-1α is widely distributed in the retina (Fig. 3). IL-1α immunoreactivity was mostly found in the photoreceptor layer (layer 1), inner nuclear layer (layer 4), inner plexiform layer (layer 5) and ganglion cell layer (layer 6), but differences are not appreciable between groups, nondiabetic and diabetic retina (Fig. 3a, b). In a more detail, in the case of the photoreceptor layer, IL-1α is located in the more peripheral part of the outer cone/rod segments. Moreover, in the case of the inner nuclear layer, the fluorescent signals were also observed inside the nuclei of the some cells (Fig. 3c, d).
Distribution of IL-1α in the normal and diabetic rat retina. Representative images showing distribution of IL-1α in retinal layers of control (a), diabetic rats (b). Retinal distribution of IL-1α was detected using a rabbit anti-IL-1α primary antibody revealed with Alexa Fluor 488 goat anti-rabbit (green fluorescence). Cell nuclei were stained with DAPI (blue fluorescence). Images shown are representative results taken from different fields from randomly selected slides and scanned by CLSM. Retinal layers are indicated, on the left part of the figure, as follows: L1, photoreceptors outer and inner segment; L2, outer nuclear layer; L3, outer plexiform layer; L4, inner nuclear layer; L5, inner plexiform layer; L6, ganglion cell layer. c, d Cells from the inner nuclear layer (diabetic retina) where fluorescence signals are visible in some nuclei. Orthogonal vision of cells from the same layer is shown in d. Scale bars: 10 μm
The IL-1β expression and the distribution in retinal layers are different in the nondiabetic respect to the diabetic retina (Fig. 4). In the nondiabetic retina, IL-1β is prevalently located in the photoreceptor layer (layer 1) and in a lesser extent in the inner plexiform and in the ganglion cell layers (layers 5 and 6, respectively). In the diabetic retina, the fluorescent signals for IL-1β increased in all layers except in the outer nuclear layer (Fig. 4a, e). The hybridization signals observed in the photoreceptor layer (layer 1) are present in both inner and outer segments of the cone/rods, and the location seems to be along the cytoplasmic membrane (see Fig. 4b, f).
Distribution of IL-1β in the normal and diabetic rat retina. Representative images showing distribution of IL-1β in the retinal layers of control rats (a, b, c, d) and diabetic rats (e, f, g, h). IL-1β was detected using a rabbit anti-IL-1β primary antibody revealed with Alexa Fluor 488 mouse anti-goat (green fluorescence). Cell nuclei were stained with DAPI (blue fluorescence). Images shown are representative results taken from different fields from randomly selected slides and scanned by CLSM. Retinal layers are indicated, on the left of the figure, as follows: L1, photoreceptors outer and inner segment; L2, outer nuclear layer; L3, outer plexiform layer; L4, inner nuclear layer; L5, inner plexiform layer; L6, ganglion cell layer. b, c, d show the enlarged sectors indicated in a. f, g, h show the enlarged sectors indicated in e. Scale bars: 10 μm
IL-1Ra was observed only in the photoreceptor (layer 1) and in the outer plexiform (layer 5) layers, but an increased expression was detected in diabetic retina with respect to the nondiabetic one (Fig. 5a, e). In a more detail, in the plexiform layer (layer 5), we observed IL-1Ra immunoreactivity in the proximal area of the outer nuclear layer (see Fig. 5g).
Distribution of IL-1Ra in the normal and diabetic rat retina. Representative images showing distribution of IL-Ra in the retinal layers of control rats (a, b, c, d) and diabetic rats (e, f, g, h). IL-Ra was detected using a rabbit anti-IL-1β primary antibody revealed with Alexa Fluor 488 mouse anti-goat (green fluorescence). Cell nuclei were stained with DAPI (blue fluorescence). Images shown are representative results taken from different fields from randomly selected slides and scanned by CLSM. Retinal layers are indicated, on the left of the figure, as follows: L1, photoreceptors outer and inner segment; L2, outer nuclear layer; L3, outer plexiform layer; L4, inner nuclear layer; L5, inner plexiform layer; L6, ganglion cell layer. b, c, d show the enlarged sectors indicated in a. f, g, h show the enlarged sectors indicated in e. Scale bars: 10 μm
A different expression pattern is evident for the IL-1RI (Fig. 6a, b) and IL-1RII (Fig. 6c, d) in nondiabetic retina. IL-1RI labeling (Fig. 6a) is distributed in all retinal layers, being almost absent in the outer segment of the photoreceptor layer (layer 1). Instead, IL-1RII is particularly evident in the entire photoreceptor layer (layer 1), in the ganglion cell layer (layer 6) and in the region of the plexiform layer (layer 5) close to the inner nuclear layer (layer 4). The hyperglycemic condition induced by STZ determines an overall expression of both IL-1RI and IL-1RII in all the retina layers (Fig. 6b, d), with a larger amount of the former with respect to the second (see also Fig. 2a). In the case of IL-1RI, the increase is very evident in the outer nuclear layer (layer 2) on the contrary to that observed for IL-1RII whose increment in the outer nuclear layer (layer 2) is lesser massive than IL-1RI (Fig. 6b, d).
Distribution of IL-1RI and IL-1RII in the normal and diabetic rat retina. Representative images showing the distribution of IL-1RI (a, b) and IL-1RII (c, d), in the retinal layers of control rats (a, c) and diabetic rats (b, d) after 3 weeks of hyperglycemia. Retinal distribution of IL-1RI and IL-1RII was detected using a rabbit anti-IL-1RI and anti-IL-1RII primary antibody revealed with Alexa Fluor 488 goat anti-rabbit (green fluorescence). Cell nuclei were stained with DAPI (blue fluorescence). Images shown are representative results taken from different fields from randomly selected slides and scanned by CLSM. Retinal layers are indicated, on the left of the figure, as follows: L1, photoreceptors outer and inner segment; L2, outer nuclear layer; L3, outer plexiform layer; L4, inner nuclear layer; L5, inner plexiform layer; L6, ganglion cell layer. Scale bars: 10 μm
Discussion
Hyperglycemia is recognized as the main cause for neural and vascular inflammation in DR. During this condition, the excessive oxidative stress and the reduction of neutralizing mechanisms lead to activation of some proinflammatory cytokines, such as interleukin-1β (IL-1β). Indeed, previous papers have already described its involvement in ocular diseases including DR (Demircan et al. 2006; Brucklacher et al. 2008; Tang and Kern 2011). IL-1β has been described as a mediator of retinal damage in early phase of diabetes; however in this context, no attention has been given to the other members of IL-1’s family, whom all together participate and modulate inflammatory response (Carmo et al. 2000; Kowluru and Odenbach 2004; Krady et al. 2005).
In the present study, we focused our attention on some of these members. Results showed that hyperglycemia interferes with their expression. In particular, diabetic retinas showed a significant increase in the levels of IL-1β and IL-1RI (p < 0.001) and in lesser extent of IL-Ra and IL-1RII (p < 0.01 and p < 0.05 respectively) compared to nondiabetic ones (Fig. 1). These data suggest that the inflammatory process is mainly mediated by IL-1β, through interaction with its receptor IL-1RI. This cytokine, once released, triggers other inflammatory mediators and leads to tissutal damage (Rothwell and Luheshi 2000). Moreover, it is able to induce own synthesis via autocrine/paracrine autostimulation by generating an amplification of inflammatory process (Toda et al. 2002). This evidence is further supported by retinal upregulation of IL-1RI during diabetes, which is essential transduction element of IL-1β.
In our study, IL-1α levels were unchanged in retina of diabetic as compared to control. This data is consistent with other evidences demonstrating that the retinal inflammation is mediated in lesser extent by this cytokine as compared to IL-1β (Rider et al. 2013). IL-1α seems to have mainly a role in inflammatory events involving cell necrosis. It is present in cells as a precursor, and during the tissue damage, it is released in the microenvironment by triggering the inflammatory response against the dead cells. Therefore, this cytokine is exclusively released from necrotizing cells; instead in cells dying through apoptotic process, IL-1α is retained in the nucleus tightly linked to chromatin (Luheshi et al. 2009; Cohen et al. 2010; Lamacchia et al. 2013). This binding reduces mobility of IL-1α, which is not released from dying cells, and attenuates inflammation caused by cells expressing IL-1α (Luheshi et al. 2009; Cohen et al. 2010). According to this evidence, in our previous paper, we demonstrated that in the early phases of hyperglycemia, there is retinal neurodegeneration due to change in survival signaling pathways and overexpression of activated caspase 3 and p53, both genes involved in apoptotic cell death (Giunta et al. 2012; Scuderi et al. 2014).
Here, we also observed that to contrast the inflammatory process mediated by IL-1β in the diabetic retina, other mechanisms were involved. Indeed, during hyperglycemia, we detected a significant increase in the expression levels of IL-1 antagonist, IL-1Ra and IL-1RII. Since its discovery, IL-1Ra was considered the major natural inhibitor and an important in vivo regulator of IL-1 action (Garlanda et al. 2013). Furthermore, it protects retinal endothelial cells against the degeneration induced by nitric oxidative stress or glucose (Kowluru and Odenbach 2004). However, our results suggested that its levels are not sufficient to counteract the overwhelming effects of IL-1β. The concomitant overexpression of the receptor IL-1RII, even if it limits the IL-1RI biological action, fails to counter the devastating effects induced by IL-1β. These evidences are confirmed by immunofluorescent analysis.
This study provides also a detailed analysis, not described until now, about the distribution of above-mentioned IL-1 family members in the diabetic retina. All receptors examined (IL-1RI and IL-1RII) are present in the retina and show partially overlapping distribution between retinal layers. IL-1RI is almost absent in the outer segment of the photoreceptor layer where instead IL-1RII is particularly abundant. IL-1α is widely distributed in the retina, especially in the photoreceptor layer, inner nuclear layer, inner plexiform layer and ganglion cell layer, while IL-1β is prevalently located in the photoreceptor layer and in a lesser extent in the inner plexiform and in the ganglion cell layers. Hyperglycemia affects the regional distribution of these inflammatory elements. Indeed, in the diabetic retina, IL-1RI become detectable in the outer nuclear layer, and concomitantly, an increased expression of IL-1β in the same retinal layer has been observed. This highlights the hyperactivation of an important inflammatory pathway, in an anatomical region strictly connected with the BRB which is seriously compromised during DR. As previously described, we found also thinning of diabetic retina, especially in the ganglion cell layer, as compared to control (Fig. 3). This has been previously described in animal models of DR and clinically showing attenuation of some layers, i.e., ganglion cell layer, inner and outer nuclear layer, resulting from the inflammatory cascade (Martin et al. 2004; Cabrera DeBuc and Somfai 2010).
In a recent paper, it has been demonstrated the main role performed by Müller cells in inflammatory process in response to hyperglycemia. These cells are spanning the entire retinal thickness and are glial cells. They become activated in response to some pathological changes and produce various cytokines, such as IL-6 and IL-8, following exposure to different stimuli. Particularly, it has been observed that during hyperglycemic insult, IL-1β induces IL-6 production in these cells through the activation of P38 MAPK/NF-κB signaling pathway (Liu et al. 2015). This effect could likely be mediated by the interaction between this cytokine and its IL-1RI receptor expressed in Müller cells. In support of this hypothesis, we have observed, in diabetic rat’s retina, the increase IL-1RI immunoreactivity in the layers spanned by Müller cells, i.e., external granular layer, outer plexiform layer and inner granular layer. However, this hypothesis needs to be further validated by using specific cell markers.
Our study was limited to the analysis of some cytokines; however, it will be necessary to deepen this work by analyzing other molecules involved in inflammatory process during DR. However, the evidences reported here suggest a new therapeutic approach to protect the retina from diabetic degeneration.
Conclusions
To date, the maintenance of normal blood glucose levels represents the most effective approach to the prevention of DR. However, the depth characterization of the apoptotic and inflammatory pathway involved in this degenerative process could lead to the development of effective and targeted therapy.
References
Abu el Asrar AM, Maimone D, Morse PH, Gregory S, Reder AT (1992) Cytokines in the vitreous of patients with proliferative diabetic retinopathy. Am J Ophthalmol 114(6):731–736
Arend WP, Palmer G, Gabay C (2008) IL-1, IL-18, and IL-33 families of cytokines. Immunol Rev 223:20–38
Brucklacher RM, Patel KM, VanGuilder HD, Bixler GV, Barber AJ, Antonetti DA, Lin CM, LaNoue KF, Gardner TW, Bronson SK, Freeman WM (2008) Whole genome assessment of the retinal response to diabetes reveals a progressive neurovascular inflammatory response. BMC Med Genomics 1:26
Bucolo C, Leggio GM, Drago F, Salomone S (2012) Eriodictyol prevents early retinal and plasma abnormalities in streptozotocin-induced diabetic rats. Biochem Pharmacol 84(1):88–92
Bucolo C, Ward KW, Mazzon E, Cuzzocrea S, Drago F (2009) Protective effects of a coumarin derivative in diabetic rats. Invest Ophthalmol Vis Sci 50(8):3846–3852
Cabrera DeBuc D, Somfai GM (2010) Early detection of retinal thickness changes in diabetes using Optical Coherence Tomography. Med Sci Monit 16(3):15–21
Carmo A, Cunha-Vaz JG, Carvalho AP, Lopes MC (2000) Effect of cyclosporin-A on the blood–retinal barrier permeability in streptozotocin-induced diabetes. Mediators Inflamm 9(5):243–248
Chakrabarti S, Cukiernik M, Hileeto D, Evans T, Chen S (2000) Role of vasoactive factors in the pathogenesis of early changes in diabetic retinopathy. Diabetes Metab Res Rev 16(6):393–407
Cohen I, Rider P, Carmi Y, Braiman A, Dotan S, White MR, Voronov E, Martin MU, Dinarello CA, Apte RN (2010) Differential release of chromatin-bound IL-1alpha discriminates between necrotic and apoptotic cell death by the ability to induce sterile inflammation. Proc Natl Acad Sci U S A 107(6):2574–2579
Cunha-Vaz JG (2004) The blood-retinal barriers system. Basic concepts and clinical evaluation. Exp Eye Res 78(3):715–721
D'Amico AG, Scuderi S, Saccone S, Castorina A, Drago F, D'Agata V (2013) Antiproliferative effects of PACAP and VIP in serum-starved glioma cells. J Mol Neurosci 51(2):503–513
Demircan N, Safran BG, Soylu M, Ozcan AA, Sizmaz S (2006) Determination of vitreous interleukin-1 (IL-1) and tumour necrosis factor (TNF) levels in proliferative diabetic retinopathy. Eye (Lond) 20(12):1366–1369
Feenstra DJ, Yego EC, Mohr S (2013) Modes of retinal cell death in diabetic retinopathy. J Clin Exp Ophthalmol 4(5):298
Garlanda C, Dinarello CA, Mantovani A (2013) The interleukin-1 family: back to the future. Immunity 39(6):1003–1018
Giunta S, Castorina A, Bucolo C, Magro G, Drago F, D'Agata V (2012) Early changes in pituitary adenylate cyclase-activating peptide, vasoactive intestinal peptide and related receptors expression in retina of streptozotocin-induced diabetic rats. Peptides 37(1):32–39
Hoerger TJ, Segel JE, Gregg EW, Saaddine JB (2008) Is glycemic control improving in U.S. adults? Diabetes Care 31(1):81–86
Irikura VM, Lagraoui M, Hirsh D (2002) The epistatic interrelationships of IL-1, IL-1 receptor antagonist, and the type I IL-1 receptor. J Immunol 169(1):393–398
Kern TS (2007) Contributions of inflammatory processes to the development of the early stages of diabetic retinopathy. Exp Diabetes Res 2007:95103
Kim B, Lee Y, Kim E, Kwak A, Ryoo S, Bae SH, Azam T, Kim S, Dinarello CA (2013) The interleukin-1alpha precursor is biologically active and is likely a key alarmin in the IL-1 family of cytokines. Front Immunol 4:391
Kowluru RA, Odenbach S (2004) Role of interleukin-1beta in the development of retinopathy in rats: effect of antioxidants. Invest Ophthalmol Vis Sci 45(11):4161–4166
Krady JK, Basu A, Allen CM, Xu Y, LaNoue KF, Gardner TW, Levison SW (2005) Minocycline reduces proinflammatory cytokine expression, microglial activation, and caspase-3 activation in a rodent model of diabetic retinopathy. Diabetes 54(5):1559–1565
Lamacchia C, Rodriguez E, Palmer G, Gabay C (2013) Endogenous IL-1alpha is a chromatin-associated protein in mouse macrophages. Cytokine 63(2):135–144
Lieth E, Gardner TW, Barber AJ, Antonetti DA, Penn State Retina Research Group (2000) Retinal neurodegeneration: early pathology in diabetes. Clin Exp Ophthalmol 28(1):3–8
Liu X, Ye F, Xiong H, Hu DN, Limb GA, Xie T, Peng L, Zhang P, Wei Y, Zhang W, Wang J, Wu H, Lee P, Song E, Zhang DY (2015) IL-1beta Induces IL-6 production in retinal Muller cells predominantly through the activation of P38 MAPK/NF-kappaB signaling pathway. Exp Cell Res 331(1):223–231
Luheshi NM, McColl BW, Brough D (2009) Nuclear retention of IL-1 alpha by necrotic cells: a mechanism to dampen sterile inflammation. Eur J Immunol 39(11):2973–2980
Martin PM, Roon P, Van Ells TK, Ganapathy V, Smith S (2004) Death of retinal neurons in streptozotocininduced diabetic mice. Invest Ophthalmol Vis Sc. 45(9):3330–3336
Rider P, Carmi Y, Voronov E, Apte RN (2013) Interleukin-1alpha. Semin Immunol 25(6):430–438
Rothwell NJ, Luheshi GN (2000) Interleukin 1 in the brain: biology, pathology and therapeutic target. Trends Neurosci 23(12):618–625
Rungger-Brandle E, Dosso AA, Leuenberger PM (2000) Glial reactivity, an early feature of diabetic retinopathy. Invest Ophthalmol Vis Sci 41(7):1971–1980
Safi SZ, Qvist R, Kumar S, Batumalaie K, Ismail IS (2014) Molecular mechanisms of diabetic retinopathy, general preventive strategies, and novel therapeutic targets. Biomed Res Int 2014:801269
Saydah SH, Fradkin J, Cowie CC (2004) Poor control of risk factors for vascular disease among adults with previously diagnosed diabetes. JAMA 291(3):335–342
Scuderi S, D'Amico AG, Castorina A, Federico C, Marrazzo G, Drago F, Bucolo C, D'Agata V (2014) Davunetide (NAP) protects the retina against early diabetic injury by reducing apoptotic death. J Mol Neurosci
Scuderi S, D'Amico AG, Castorina A, Imbesi R, Carnazza ML, D'Agata V (2013) Ameliorative effect of PACAP and VIP against increased permeability in a model of outer blood retinal barrier dysfunction. Peptides 39:119–124
Sedaghat R, Roghani M, Ahmadi M, Ahmadi F (2011) Antihyperglycemic and antihyperlipidemic effect of Rumex patientia seed preparation in streptozotocin-diabetic rats. Pathophysiology 18(2):111–115
Sims JE, Dower SK (1994) Interleukin-1 receptors. Eur Cytokine Netw 5(6):539–546
Tang J, Kern TS (2011) Inflammation in diabetic retinopathy. Prog Retin Eye Res 30(5):343–358
Toda Y, Tsukada J, Misago M, Kominato Y, Auron PE, Tanaka Y (2002) Autocrine induction of the human pro-IL-1beta gene promoter by IL-1beta in monocytes. J Immunol 168(4):1984–1991
Yuuki T, Kanda T, Kimura Y, Kotajima N, Tamura J, Kobayashi I, Kishi S (2001) Inflammatory cytokines in vitreous fluid and serum of patients with diabetic vitreoretinopathy. J Diabetes Complicat 15(5):257–259
Acknowledgments
Dr. Soraya Scuderi was supported by the International PhD Program in Neuropharmacology, Medical School, University of Catania, Catania, Italy. The study was supported by Ministry of University and Research (MIUR), grant PRIN 2009BM7LJC_005 and grant PON 01–00110. These experiments were also accomplished using equipments provided in by the City Hall of Catania (ICT-E1 project).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Scuderi, S., D’amico, A.G., Federico, C. et al. Different Retinal Expression Patterns of IL-1α, IL-1β, and Their Receptors in a Rat Model of Type 1 STZ-Induced Diabetes. J Mol Neurosci 56, 431–439 (2015). https://doi.org/10.1007/s12031-015-0505-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-015-0505-x