Abstract
Differential expressions of immune molecules have been shown in the thymi with pathological results, including myasthenia gravis (MG). CD25 is an activation marker expressed on T cells. CXCL13 mediates the homing and motility of B cells in secondary lymphoid tissues. Herein, we investigated the expressions of CD25 and CXCL13 in the thymi of thymic hyperplasia patients with MG or with non-MG. A total of 34 thymic hyperplasia patients with MG (20 generalized MG (GMG) and 14 ocular MG (OMG) and six thymic hyperplasia patients without MG were enrolled and analyzed using immunohistochemical staining and real-time polymerase chain reaction for CD25 and CXCL13. Our study demonstrated a higher expression of both CD25 and CXCL13 in hyperplastic thymi with OMG or GMG compared to those with non-MG. According to the immunohistochemical results, we observed that CD25 expression was significantly lower in atrophic thymi and non-MG hyperplastic thymi, compared with that in infant thymi (P = 0.002 and 0.005, respectively). In contrast to CD25 expression, we did not observe differential expression of CXCL13 among three control groups. And a similar CD25 mRNA expression was found in real-time polymerase chain reaction (PCR) results. We observed that both hyperplastic thymi with OMG or GMG expressed significantly higher levels of CD25 than those with non-MG (P = 0.007 and 0.001, respectively). And an increase of CD25 expression was observed in hyperplastic thymi with GMG compared to those with OMG (P = 0.030). Similarly, CXCL13 expression was significantly higher in hyperplastic thymi with GMG or with OMG than those with non-MG (P = 0.001 and 0.050, respectively). No significant CXCL13 expression difference was found between hyperplastic thymi with GMG and those with OMG (P > 0.05). The real-time PCR results showed a similar tendency of CD25 mRNA expression among the thymi of non-MG, OMG, and GMG patients, but the difference did not reach significance (P > 0.05). An obvious increased expression of CXCL13 was found in hyperplastic thymi with GMG patients, compared to those with non-MG and OMG patients (P = 0.003 and 0.071, respectively). There was no difference found between hyperplastic thymi with non-MG and with OMG. Regression analysis showed a positive correlation between thymic CD25 level and MG symptom severity (F = 28.240; P = 0.000, r = 0.523). Similarly, a positive correlation was found between thymic CXCL13 expression and MG disease severity (F = 36.093; P = 0.000, r = 0.671). Taken together, our findings suggest CD25 and CXCL13 participate in the pathogenesis of MG and may influence the clinical symptoms of MG.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Myasthenia gravis (MG) is an autoimmune disorder characterized by the presence of antibodies against the skeletal muscle acetylcholine receptors (AChR) at the neuromuscular junction and by the failure of neuromuscular transmission (Vincent et al. 2001). Typically, MG is divided into ocular MG (OMG) and generalized MG (GMG). OMG involves the extraocular muscles and manifests with fluctuating extraocular muscular weakness. GMG is potentially life-threatening where dysphagia or dyspnea is attributed to the involvement of medulla oblongata as the primary cause of death. About 85 % of MG patients initially present with OMG, and 80 % of OMG patients develop into GMG in the first year and then 90 % in 3 years (Bever et al. 1983). In contrast, only 50 % of Asian MG patients present with purely ocular manifestations during their lifetime (Zhang et al. 2007). Finally, 80–90 % of MG patients suffer thymus dysfunction including thymic hyperplasia and thymoma (Onodera 2005).
IL-2 receptor α chain (CD25) is known as an activation marker expressed on T cells. CD4+CD25+ regulatory T cells (CD4+CD25+ Tregs) play an important role in promoting peripheral self-tolerance and regulating immune responses. Studies on the changes of circulating and thymic CD4+CD25+ Tregs in MG patients have been extensively performed, but controversial views were obtained. Some studies show lower CD4+CD25+ Treg in peripheral blood in MG patients (Balandina et al. 2005; Fattorossi et al. 2005; Sun et al. 2004). Other research shows no significant change in CD4+CD25+ Tregs in MG patients (Huang et al. 2004). In addition to CD4+CD25+ Tregs, CD8+ regulatory T cells exert a negative immunomodulatory function and are receiving more research attention. Importantly, this cell population has also demonstrated CD25 expression (Correale and Villa 2010; Cosmi et al. 2003). To some extent, CD25 expression may represent CD4+ and CD8+ regulatory T cells.
CXC chemokine ligand 13 (CXCL13) is known to mediate the homing and motility of B cells in secondary lymphoid tissues (Carlsen et al. 2002; Legler et al. 1998; Luther et al. 2003). Mice lacking CXCL13, or the CXCL13 receptor CXCR5, fail to form lymphoid follicles (Ansel et al. 2000). Lymphoid follicles are locations where abnormally responsive AChR antibodies (AChR Ab) are formed. These AChR Abs pathologically affect the transmission of nerve impulses in MG (Garcia et al. 2003; Roxanis et al. 2002). Several studies have shown that serum CXCL13 expression is associated with the severity of MG symptoms (Meraouna et al. 2006; Shiao et al. 2010), but it still remains unclear whether a similar correlation between thymic CXCL13 expression and MG disease severity exists. The aim of the present study was to explore possible correlations between expression levels of the two molecules CD25 and CXCL13 and the severity of MG symptoms in the thymi to clarify the difference between OMG and GMG. We collected thymic tissue samples from all thymic hyperplasia patients who underwent thymectomy in Tangdu Hospital between 2006 and 2010 to evaluate CD25 and CXCL13 expressions in MG patients with thymic hyperplasia.
Subjects and Methods
Subjects
A total of 52 thymic hyperplasia patients underwent thymectomy from 2006 to 2010 at the Department of Thoracic Surgery of Tangdu Hospital. The diagnosis of MG was based on the typical clinical symptoms, positive response to cholinesterase inhibitors, anti-AchR antibody assay, and abnormal results on repeat nerve electric stimulation. OMG or GMG was identified and classified according to the Myasthenia Gravis Foundation of America (MGFA) (Jaretzki et al. 2000). Three control groups were used to reduce bias. Control 1 (thymic hyperplasia with non-MG) was used to remove the influence by thymic hyperplasia. Control 2 (atrophic thymi from adult patients suffering from lung or esophageal cancer), and control 3 (infant thymi of less than 1 year who underwent surgical intervention for congenital heart disease) were used to determine whether aging is related to thymi associated with different molecular expression and why thymic hyperplasia was in high risk of MG. The infant thymi were obtained when thymus tissue must be removed to expose the surgical field. Exclusion criteria were (1) treatment with immunosuppressive drugs, such as corticosteroids, azathioprine, and with plasma exchange or intravenous immunoglobulin; (2) pregnancy; (3) other autoimmune or inflammatory diseases; and (4) diagnosis with thymoma. All adult patients gave written informed consent, and thymus tissues were used only for research purposes. The informed consents for infants were signed by their guardian. The study protocol was approved by the Ethics Committee of Tangdu Hospital. The clinical data of all the subjects are shown in Table 1.
Immunohistochemical Staining and Scoring
All thymus tissues were fixed with 10 % (v/v) formalin, embedded in paraffin, and cut into 2-μm-thick sections. Before staining, antigen retrieval was carried out by 10 mM citric acid buffer (pH 6.0), and endogenous peroxidase activity was quenched by 3 % (v/v) hydrogen peroxide–methanol solution. Nonspecific binding was blocked by incubation in a drop of 10 % (v/v) goat nonimmune serum (CD25) or of 10 % (v/v) rabbit nonimmune serum (CXCL13) for 30 min. Sections were then incubated at 4 °C overnight in the primary antibody, goat anti-human CXCL13 (Maixin, Fuzhou, China; clone number GAB-0616), or mouse anti-human CD25 monoclonal antibody (1:50 in PBS; Maixin, Fuzhou, China; clone number MAB-0209). The sections were rinsed three times with PBS and incubated at 37 °C for 20 min in biotinylated second antibodies. After rinsing three times with PBS, the sections were incubated at 37 °C for 20 min in streptavidin/horseradish peroxidase (Invitrogen, UK; catalog number 85–9043). Color development was performed by commercially available DAB Substrate Kit (Sigma-Aldrich, D8001; USA).
Immunohistochemical (IHC) staining was scored as described previously (Zhang et al. 2012). Briefly, the proportion of positive staining cells are as follows (S1): <5 % scored 0, 6–25 % scored 1, 26–50 % scored 2, 51–75 % scored 3, and >75 % scored 4; staining intensity (S2): colorless scored 0, flavescent scored 1, yellow scored 2, and brown scored 3. S1 was multiplied by S2 to obtain an estimate of the total IHC score for each molecule.
Real-Time Polymerase Chain Reaction
The mRNA expressions of CD25 and CXCL13 were analyzed by real-time polymerase chain reaction (PCR) using the 7500 fast equipment (Applied Biosystems, USA). The experiments were always done in quadruplicate, and samples were normalized using adults’ atrophic thymi as controls. The primer used for amplification of the CXCL13 sense was CTCTGCTTCTCATGCTGCTG and anti-sense was TGAGGGTCCACACACACAAT. The primer of the CD25 sense was ACCAAGGCGGGAGCATCT and the anti-sense was GCAACAGCACCTGGGAAT. All the results were expressed relative to GAPDH, and this gene sense primer was AGGTCCACCACTGACACGTT, and the anti-sense was GCCTCAAGATCATCAGCAAT. The relative expression of both genes studied was calculated according to formula 2−(Rt−Et)−(Rn−En).
Statistical Analysis
Data on the IHC scores are expressed as means ± sem (standard error of mean) and were analyzed by one-way analysis of variance (ANOVA). The results of CD25 and CXCL13 expressions from real-time PCR were relative to the adults’ atrophic thymi. Linear regression analysis was done to determine the correlations between thymic CD25 or CXCL13 expression, respectively, and classification of MG (MGFA). All statistical analyses were performed using SPSS13.0 software, and a value of P < 0.05 was considered significantly.
Results
Clinical Characteristics of Thymic Hyperplasia Patients with OMG, GMG, and Non-MG
A total of 34 thymic hyperplasia patients with MG were selected, 20 identified as GMG and 14 as OMG. We collected six thymic hyperplasia patient samples with non-MG with the mean age of undergoing thymectomy at 25.17 ± 6.35 years (mean ± standard deviation). The mean onset age of MG was 25.29 ± 6.44 years for OMG and 31.00 ± 6.21 years for GMG. The mean duration of MG before thymectomy was 13.50 ± 9.85 months for OMG and 11.40 ± 6.45 months for GMG. We did not observe significant differences between the two groups in the mean onset age (P = 0.154) and in the mean duration (P = 0.583).
Expressions of CD25 and CXCL13 Protein and mRNA in Infant, Atrophic, and Hyperplastic Thymi with Non-MG Groups
According to the IHC results, we observed that CD25 expression was significantly lower in atrophic thymi compared with that in infant thymi (P = 0.002). Also, a significantly lower CD25 expression was observed in non-MG hyperplastic thymi than that in infant thymi (P = 0.005). Similar CD25 expression was seen between atrophic thymi and non-MG hyperplastic thymi. In contrast to CD25 expression, we did not observe differential expression of CXCL13 among three control groups (Fig. 1). Similar significance levels of CD25 mRNA expression were found in real-time PCR among atrophic, infant, and non-MG hyperplastic thymi (Fig. 2). Although the CXCL13 mRNA level was lower in atrophic thymi, and higher in non-MG hyperplastic thymi than in infant thymi, the difference did not reach significance (P = 0.099 and 0.074, respectively). The representative micrographs for CD25 and CXCL13 staining in these groups are shown in Fig. 3.
Different expressions of CD25 and CXCL13 in infant thymi, adult atrophic thymi, and adult hyperplastic thymi with non-MG. Bars represent the mean IHC scores for the two molecules in each group. Data are shown as means ± sem and were analyzed by one-way ANOVA. The asterisk indicates P < 0.05 versus infant normal thymi
Quantitative analysis of CD25 and CXCL13 mRNA expression in thymus. The mRNA expression of CD25 and CXCL13 in thymus from infant adult and hyperplastic thymi with non-MG patients was performed by real-time polymerase chain reaction. Expression level of each group was shown relative to adult atrophic thymus. The bars showed means ± sem, and the results were analyzed by ANOVA. The asterisk indicates P < 0.05 versus adult atrophic thymi
Expressions of CD25 and CXCL13 Protein and mRNA in Hyperplastic Thymi with Non-MG, OMG, and GMG
We observed that both hyperplastic thymi with OMG or GMG expressed significantly higher levels of CD25 protein than those with non-MG (P = 0.007 and 0.001, respectively). And an increase of CD25 expression was observed in hyperplastic thymi with GMG compared to those with OMG (P = 0.030). Similarly, CXCL13 protein expression was significantly higher in hyperplastic thymi with GMG or with OMG than those with non-MG (P = 0.001 and 0.050, respectively). No significant difference was found in the CXCL13 expression between hyperplastic thymi with GMG and those with OMG (P = 0.069) (Fig. 4). The representative micrographs are shown in Fig. 3.
Different expressions of CD25 and CXCL13 in hyperplastic thymi with non-MG, OMG, and GMG. Bars represent the mean IHC scores for the two molecules in each group. Data are shown as means ± sem and were analyzed by ANOVA. The asterisk indicates P < 0.05 versus hyperplastic thymi with non-MG, and the number sign indicates P < 0.05 versus hyperplastic thymi with OMG
The real-time PCR showed a similar mRNA expression of CD25 among the thymi of non-MG, OMG, and GMG patients, with the difference not reaching statistical significance (P > 0.05). An obvious increased expression of CXCL13 mRNA was found in hyperplastic thymi with GMG patients, compared to those with non-MG and OMG patients (P = 0.003 and 0.071, respectively); however, there was no difference found between the latter groups (Fig. 5).
Quantitative analysis of CD25 and CXCL13 mRNA expression in thymic hyperplasia. The mRNA expression of CD25 and CXCL13 in hyperplastic thymi from non-MG, OMG, and GMG patients was performed by real-time polymerase chain reaction. Expression level of each group was shown relative to adult atrophic thymus. Data are shown as means ± sem and were analyzed by ANOVA. The asterisk indicates P < 0.05 versus hyperplastic thymi with non-MG
Correlations Between Expression Level and Severity of MG Symptoms in Thymic Hyperplasia Patients
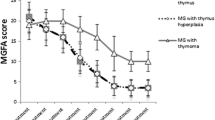
Regression analysis showed a positive correlation between thymic CD25 level and MG symptom severity (F = 28.240; P = 0.000, r = 0.523). Similarly, a positive correlation was found between thymic CXCL13 expression and MG disease severity (F = 36.093; P = 0.000, r = 0.671) (Fig. 6).
Correlation between CD25 and CXCL13 expression with the severity of MG. The y-axis shows the mean IHC score for the two molecules in each clinical symptom of MG. The x-axis shows each clinical symptom of MG valued from MGFA. a Correlation between CD25 expression and the severity of MG. b Correlation between CXCL13 expression and the severity of MG
Discussion
There is increasing evidence for Treg participation in MG. Tregs express a highly constitutive surface marker CD25. Although CD4+CD25+ Tregs are the main focus, a subset of CD8+ T cells, performing similar functions as CD4+CD25+ Tregs, have been gaining notice. Interestingly, these CD8+ T cells also express high levels of CD25. Thus, we detected CD25 expression to reflect the change of the two types of Tregs in different thymi.
Aging-related thymic degeneration leads to a prominent inability to produce new T cells (Berzins et al. 2002; Goronzy and Weyand 2005). Given that Tregs are generated in the thymus, it is conceivable that thymic output of Tregs decreases during aging (Dejaco et al. 2006). And this notion is confirmed by our observation of a significant decrease of CD25 expression in atrophic thymi compared to that in infant thymi. Theoretically, a higher expression of CD25 should result in milder clinical symptoms based on the known suppressive role of Tregs in autoimmune diseases (Sun et al. 2004; Talpur et al. 2006; van Roon et al. 2010; Viglietta et al. 2004). However, our comparison of CD25 expressions in hyperplastic thymi unexpectedly found significantly elevated levels of CD25 in the OMG samples, and most notably in the GMG group, compared to those in the non-MG. Such a phenomenon is presumed to be involved with the functional defect of these CD25+ Tregs in MG patients, and a similar result has been published in an early report (Balandina et al. 2005). And the CD25 excess can be explained by an alleviative cholonergic blockade on T cells, since massive increases in acetylcholinesterase levels have been observed in MG (Brenner et al. 2003; Gilboa-Geffen et al. 2007). Moreover, a positive correlation between CD25 expression and MG disease severity has been revealed by our study. All the findings suggest that CD25 in hyperplastic thymi may participate in the pathogenesis of MG and might be used as an index of disease severity and prognosis of MG.
Chemokine CXCL13 plays a critical role in the formation of germinal center-like follicles in autoimmune diseases. Ectopic thymic expression of CXCL13 is associated with aberrant B cell trafficking to the thymus of MG (Shiao et al. 2010) and is the key molecule in autoimmune malfunction in MG (Meraouna et al. 2006). In the present study, we observed an increased expression of CXCL13 in thymic hyperplasia in both OMG and GMG compared with that in non-MG. Increased CXCL13 expression was observed in thymic hyperplasia with MG compared to that with non-MG, which might be interpreted by the fact that the thymus of MG patients contains the germinal center-like follicles (Okumura et al. 2003). The similar CXCL13 expression level in thymic hyperplasia with non-MG, adult atrophic thymi, and infant normal thymi is likely due to an observed absence of germinal centers in the thymi of all three types. Similar to CD25, several studies have shown that serum CXCL13 level is associated with the severity of MG symptoms (Meraouna et al. 2006; Shiao et al. 2010) and positively correlates with the MGFA subtypes of GMG in thymic hyperplasia patients (Shiao et al. 2010). Similarly, we found a higher level of CXCL13 in thymic hyperplasia with GMG than with OMG, and linear regression analysis revealed a positive correlation of CXCL13 expression with the severity of MG symptoms. Combined with the previous report that the CXCL13 gene can be inhibited by glucocorticoids (Roxanis et al. 2002), we presume that a high thymic CXCL13 level might hint at poor MG prognosis, and strategies targeting CXCL13 could offer treatment options.
It is to be noted that there were different significance levels of IHC and RT-PCR tests. The technical issues should be avoided because the thymus tissues had been sliced and stained by skilled technicists blind to the grouping according to the same methodology. Given the known posttranscriptional regulatory functions of microRNAs (miRNAs) (Krol et al. 2010), further studies should be performed to clarify the potential involvement of miRNAs in the difference between protein and mRNA levels of CD25 and CXCL13. Besides, this study has several limitations that might influence the efficacy, such as small numbers of volunteers, far-removed control thymi that had been resected attributed to different causes. Further studies enrolling more thymic hyperplasia patients with or without MG and control groups with the same cause are needed.
In conclusion, this study demonstrates for the first time that an elevation of thymic CD25 expression positively correlates with severity of MG symptoms in thymic hyperplasia patients. An aging-related CD25 expression decrease is also revealed. Furthermore, we observed significantly higher thymic CXCL13 levels in both OMG and GMG with thymic hyperplasia, and a positive correlation between CXCL13 expression and severity of MG symptoms. These findings provide insight into the development of Tregs underlying thymic degeneration as well as in the pathogenesis of MG. Furthermore, we suggest that CD25 and CXCL13 participate in the pathogenesis of MG and may influence the clinical symptoms of MG.
References
Ansel KM, Ngo VN, Hyman PL, Luther SA, Forster R, Sedgwick JD, Browning JL, Lipp M, Cyster JG (2000) A chemokine-driven positive feedback loop organizes lymphoid follicles. Nature 406:309–314
Balandina A, Lecart S, Dartevelle P, Saoudi A, Berrih-Aknin S (2005) Functional defect of regulatory CD4(+)CD25+ T cells in the thymus of patients with autoimmune myasthenia gravis. Blood 105:735–741
Berzins SP, Uldrich AP, Sutherland JS, Gill J, Miller JF, Godfrey DI, Boyd RL (2002) Thymic regeneration: teaching an old immune system new tricks. Trends Mol Med 8:469–476
Bever CJ, Aquino AV, Penn AS, Lovelace RE, Rowland LP (1983) Prognosis of ocular myasthenia. Ann Neurol 14:516–519
Brenner T, Hamra-Amitay Y, Evron T, Boneva N, Seidman S, Soreq H (2003) The role of readthrough acetylcholinesterase in the pathophysiology of myasthenia gravis. FASEB J 17:214–222
Carlsen HS, Baekkevold ES, Johansen FE, Haraldsen G, Brandtzaeg P (2002) B cell attracting chemokine 1 (CXCL13) and its receptor CXCR5 are expressed in normal and aberrant gut associated lymphoid tissue. Gut 51:364–371
Correale J, Villa A (2010) Role of CD8+ CD25+ Foxp3+ regulatory T cells in multiple sclerosis. Ann Neurol 67:625–638
Cosmi L, Liotta F, Lazzeri E, Francalanci M, Angeli R, Mazzinghi B, Santarlasci V, Manetti R, Vanini V, Romagnani P, Maggi E, Romagnani S, Annunziato F (2003) Human CD8+CD25+ thymocytes share phenotypic and functional features with CD4+CD25+ regulatory thymocytes. Blood 102:4107–4114
Dejaco C, Duftner C, Schirmer M (2006) Are regulatory T-cells linked with aging? Exp Gerontol 41:339–345
Fattorossi A, Battaglia A, Buzzonetti A, Ciaraffa F, Scambia G, Evoli A (2005) Circulating and thymic CD4 CD25 T regulatory cells in myasthenia gravis: effect of immunosuppressive treatment. Immunology 116:134–141
Garcia YR, Pothitakis JC, Krolick KA (2003) Myocyte production of nitric oxide in response to AChR-reactive antibodies in two inbred rat strains may influence disease outcome in experimental myasthenia gravis. Clin Immunol 106:116–126
Gilboa-Geffen A, Lacoste PP, Soreq L, Cizeron-Clairac G, Le Panse R, Truffault F, Shaked I, Soreq H, Berrih-Aknin S (2007) The thymic theme of acetylcholinesterase splice variants in myasthenia gravis. Blood 109:4383–4391
Goronzy JJ, Weyand CM (2005) T cell development and receptor diversity during aging. Curr Opin Immunol 17:468–475
Huang YM, Pirskanen R, Giscombe R, Link H, Lefvert AK (2004) Circulating CD4+CD25+ and CD4+CD25+ T cells in myasthenia gravis and in relation to thymectomy. Scand J Immunol 59:408–414
Jaretzki AR, Barohn RJ, Ernstoff RM, Kaminski HJ, Keesey JC, Penn AS, Sanders DB (2000) Myasthenia gravis: recommendations for clinical research standards. Task Force of the Medical Scientific Advisory Board of the Myasthenia Gravis Foundation of America. Ann Thorac Surg 70:327–334
Krol J, Loedige I, Filipowicz W (2010) The widespread regulation of microRNA biogenesis, function and decay. Nat Rev Genet 11:597–610
Legler DF, Loetscher M, Roos RS, Clark-Lewis I, Baggiolini M, Moser B (1998) B cell-attracting chemokine 1, a human CXC chemokine expressed in lymphoid tissues, selectively attracts B lymphocytes via BLR1/CXCR5. J Exp Med 187:655–660
Luther SA, Ansel KM, Cyster JG (2003) Overlapping roles of CXCL13, interleukin 7 receptor alpha, and CCR7 ligands in lymph node development. J Exp Med 197:1191–1198
Meraouna A, Cizeron-Clairac G, Panse RL, Bismuth J, Truffault F, Tallaksen C, Berrih-Aknin S (2006) The chemokine CXCL13 is a key molecule in autoimmune myasthenia gravis. Blood 108:432–440
Okumura M, Ohta M, Takeuchi Y, Shiono H, Inoue M, Fukuhara K, Kadota Y, Miyoshi S, Fujii Y, Matsuda H (2003) The immunologic role of thymectomy in the treatment of myasthenia gravis: implication of thymus-associated B-lymphocyte subset in reduction of the anti-acetylcholine receptor antibody titer. J Thorac Cardiovasc Surg 126:1922–1928
Onodera H (2005) The role of the thymus in the pathogenesis of myasthenia gravis. Tohoku J Exp Med 207:87–98
Roxanis I, Micklem K, McConville J, Newsom-Davis J, Willcox N (2002) Thymic myoid cells and germinal center formation in myasthenia gravis; possible roles in pathogenesis. J Neuroimmunol 125:185–197
Shiao YM, Lee CC, Hsu YH, Huang SF, Lin CY, Li LH, Fann CS, Tsai CY, Tsai SF, Chiu HC (2010) Ectopic and high CXCL13 chemokine expression in myasthenia gravis with thymic lymphoid hyperplasia. J Neuroimmunol 221:101–106
Sun Y, Qiao J, Lu CZ, Zhao CB, Zhu XM, Xiao BG (2004) Increase of circulating CD4+CD25+ T cells in myasthenia gravis patients with stability and thymectomy. Clin Immunol 112:284–289
Talpur R, Jones DM, Alencar AJ, Apisarnthanarax N, Herne KL, Yang Y, Duvic M (2006) CD25 expression is correlated with histological grade and response to denileukin diftitox in cutaneous T-cell lymphoma. J Investig Dermatol 126:575–583
van Roon JA, Hartgring SA, van der Wurff-Jacobs KM, Bijlsma JW, Lafeber FP (2010) Numbers of CD25+Foxp3+ T cells that lack the IL-7 receptor are increased intra-articularly and have impaired suppressive function in RA patients. Rheumatology (Oxford) 49:2084–2089
Viglietta V, Baecher-Allan C, Weiner HL, Hafler DA (2004) Loss of functional suppression by CD4+CD25+ regulatory T cells in patients with multiple sclerosis. J Exp Med 199:971–979
Vincent A, Palace J, Hilton-Jones D (2001) Myasthenia gravis. Lancet 357:2122–2128
Zhang X, Yang M, Xu J, Zhang M, Lang B, Wang W, Vincent A (2007) Clinical and serological study of myasthenia gravis in HuBei Province, China. J Neurol Neurosurg Psychiatry 78:386–390
Zhang M, Li H, Guo J, Zhou Y, Gong L, Wang X, Li Z, Zhang W (2012) Different molecular expression in thymoma with ocular or generalized myasthenia gravis. J Neurol Sci 313:27–31
Acknowledgments
This work was supported by the National Natural Science Foundation of China (nos. 31270952 and 31200665).
Conflicts of interest
The authors declare no financial conflict of interest.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Min Zhang, Jun Guo, and Hongzeng Li equally contributed to the present paper.
Rights and permissions
About this article
Cite this article
Zhang, M., Guo, J., Li, H. et al. Expression of Immune Molecules CD25 and CXCL13 Correlated with Clinical Severity of Myasthenia Gravis. J Mol Neurosci 50, 317–323 (2013). https://doi.org/10.1007/s12031-013-9976-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-013-9976-9