Abstract
Glial cell line-derived neurotrophic factor (GDNF) is a potent neurotrophic factor for midbrain dopamine (DA) neurons, while the DA neurons in the ventral tegmental area (VTA) is a crucial part of the neural circuits associated with drug addiction. Recently, more and more evidence suggests that GDNF plays an important role in negatively regulating the neuroadaptations induced by chronic exposure to drugs, which was thought to be the neurobiological basis of drug addiction, but the underlying mechanism is still unknown. More recently, the neural cell adhesion molecule (NCAM), which plays an important role in the process of neural plasticity, has been identified as an alternative signaling receptor for GDNF. The purpose of this study was to investigate whether NCAM was involved in the effects of GDNF on the neuroadaptations induced by chronic morphine exposure. Immunostaining results showed that NCAM was widely expressed in the VTA of rats, including all the DA neurons. The results also showed that the phosphorylation of NCAM-associated FAK, but not the total NCAM, was upregulated by GDNF, and this upregulation was inhibited by pre-treatment with the NCAM function-blocking antibody. Moreover, pre-treatment with the antibody could antagonize the effect of GDNF on inhibiting the neuroadaptations induced by chronic morphine exposure, including the decreases of the number and length of neurites and the size of cell bodies of VTA dopamine neurons, as well as the increase of tyrosine hydroxylase in the VTA dopamine neurons. These results suggest that NCAM signaling is involved in the negative regulatory effects of GDNF on chronic morphine-induced neuroadaptations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Drug addiction is a chronic relapsing disease of the brain, which is characterized by compulsive drug use in spite of adverse consequences (Ghitza et al. 2010). Despite decades of research, the availability of treatment for drug addiction is still extremely limited in clinical practice. Results from many animal experiments indicate that neuronal activity in mesocorticolimbic dopamine (DA) system underlies drug reward (Pierce and Kumaresan 2006) and relapse (Kalivas and McFarland 2003). This dopamine system, which consists of DA neurons in the ventral tegmental area (VTA) of the midbrain and their projections to the nucleus accumbens and other limbic regions in the forebrain, is a major substrate for motivated behavior and responses to natural reinforcers (Di Chiara and North 1992; Kelley and Berridge 2002). A current influential hypothesis is that the formation of drug addiction is due to drug-induced neuroadaptations in the mesocorticolimbic DA system and glutamatergic corticolimbic circuitry in which the DA projections are embedded (Kalivas and O'Brien 2008; Kalivas and Volkow 2005; Maldonado 2003). This drug-induced neuroadaptation hypothesis opens the door for work on the role of neurotrophic factors which have been implicated in many forms of plasticity within the adult nervous system (Alzoubi et al. 2013; Gong et al. 2009; Smith-Swintosky et al. 2005) in the formation of drug addiction. Among many neurotrophic factors, glial cell line-derived neurotrophic factor (GDNF) became the focus of research for its more potent and specific nutritional effect on midbrain DA neurons than any other neurotrophins (Lin et al. 1993), while the DA neurons in the VTA of the midbrain is a critical part of the neural circuits associated with drug addiction. More recently, accumulating experimental results suggest that GDNF plays an important role in negatively regulating the neuroadaptations induced by long-term exposure to drugs, which was thought to be the neurobiological basis of the formation of drug addiction. Nevertheless, the underlying mechanism remains obscure.
GDNF is a secreted protein, which is essential for the maintenance and survival of adult DA neurons (Pascual et al. 2008). As a soluble extracellular substance, GDNF exerts its effects on DA neurons via a receptor complex formed by a ligand-binding subunit termed GDNF family receptor-alpha1 (GFRa1) and a signal-transducing subunit termed RET receptor tyrosine kinase (Durbec et al. 1996; Treanor et al. 1996). Recently, the neural cell adhesion molecule-140 (NCAM-140) has been identified as an alternative signaling receptor for GDNF (Paratcha et al. 2003).
NCAM, a prominent cell adhesion molecule expressed on the surface of most neural cells, has been shown to participate in many developmental and plastic processes of the nervous system (Cox et al. 2009; Markram et al. 2007). Given that the ability of drugs of abuse to cause addiction can be viewed as a form of neural plasticity, we speculated that NCAM might be involved in some way in the formation of drug addiction. In fact, several recent studies support this speculation. For example, low prefrontal polysialylated NCAM has been demonstrated to confer risk for alcoholism-related behavior (Barker et al. 2012). In addition, another recent research has indicated that cocaine administration may modify constitutive synaptic plasticity in the medial prefrontal cortex (mPFC) by increasing the NCAM polysialylation in the mPFC of rats (Mackowiak et al. 2011). Based on the cited findings and the fact that NCAM could influence developmental events through both its adhesive as well as its signaling properties (Maness et al. 1996; Saffell et al. 1995), we postulate in the present study that GDNF may regulate negatively the neuroadaptations induced by chronic morphine exposure via altering the expression of NCAM or its signaling level. Our results showed that the phosphorylation of NCAM-associated focal adhesion kinase (FAK), but not the total NCAM levels, was upregulated with GDNF treatment, and this upregulation was inhibited by pre-treatment with the NCAM function-blocking antibody. Moreover, pre-treatment with the antibody, which decreased the phosphorylation of NCAM-associated FAK, but had no influence on the expression of NCAM, could abolish the effect of GDNF on inhibiting the neuroadaptations induced by chronic morphine exposure. These results suggest that NCAM signaling mediates the negative regulatory effects of GDNF on chronic morphine-induced neuroadaptations.
Materials and Methods
Animals
Adult male Sprague–Dawley rats (200–250 g) and neonatal Sprague–Dawley rats used in the present study were provided by the Experimental Animal Center of Xuzhou Medical College, Jiangsu. The adult animals were housed in a temperature- and humidity-controlled animal room with a 12/12-h light/dark cycle and food and water ad libitum. All animal procedures in this report were conducted in accordance with the Declaration of the National Institutes of Health Guide for Care and Use of Laboratory Animals.
Chronic Morphine Treatment
Adult rats were allowed to acclimatize to their environment for a week prior to drug administration. Then, they were injected subcutaneously with morphine hydrochloride (bid, for 5 days). The dose for each injection was 10 mg/kg on day 1 and increased by 10 mg/kg each day. An equal volume of saline (0.9 % NaCl) was injected subcutaneously in the control group. The rats receiving chronic morphine treatment were divided into three groups: morphine 1d, 3d, and 5d group, which were injected subcutaneously with morphine hydrochloride for 1, 3, and 5 days, respectively. Animals were sacrificed 12 h after the last injection.
Primary neuron culture was established from the VTA tissues of neonatal rats. At DIV 5, cultures were treated with morphine hydrochloride at a concentration of 10 μM for 5 days. This period of time and the concentration of morphine were considered as chronic morphine administration that might be suitable for studying drug dependence at the molecular level (Suder et al. 2003; Vlaskovska et al. 1999).
VTA Neuron Culture
Primary neuron culture was established from the VTA of neonatal (postnatal day 0) rats according to Inoue et al. (2007), with some modifications. Briefly, newborn Sprague–Dawley rat pups were decapitated, and their brains were removed from the skull and placed in ice-cold Dulbecco’s modified Eagle’s medium (DMEM)-F12 medium (Gibco). Coronal brain slices containing the VTA were made, and then the VTA tissues were dissected with tweezers and minced into small pieces. Tissues were enzymatically dissociated for 15 min at 37 °C with 0.25 % trypsin and 0.02 % EDTA solution; single-cell suspensions were made by gentle trituration through edge-narrowed Pasteur pipettes. After centrifugation, cell pellets were resuspended in the culture medium (DMEM/F12 1:1, containing 10 % fetal bovine serum and 4 mmol/l glutamine) and passed through a 200-mesh sieve. The cells were plated at a density of 1 × 105 cells/ml onto 24-well plates which contained poly-l-lysine-coated glass coverslips and plated at a density of 1 × 106 cells/ml onto 25-cm2 culture flasks pre-coated with poly-l-lysine. Cultures were incubated in a humidified 5 % CO2/95 % air atmosphere at 37 °C. After 24 h in vitro (1 DIV), the medium was replaced with NeurobasalTM medium (Gibco) containing 2 % B27 supplement (Gibco) and 4 mmol/l glutamine. Half of the medium was changed every 2 days. Neuronal cultures were used for experiments at DIV 5.
GDNF and NCAM Antibody Treatment
In order to explore the GDNF/NCAM interaction in vitro, at DIV 5, GDNF (Sigma, St. Louis, MO, USA) and NCAM antibody (Chemicon International, Inc., CA, USA) were administered for five consecutive days to the neuronal cultures which were exposed to morphine. It was reported that the NCAM Ab could block functionally the extacelluar domain of NCAM (Chao et al. 2003; Paratcha et al. 2003). Cultures were divided into five groups: PBS group, which was treated with PBS; morphine group, which was treated with morphine (10 μmol/L); morphine + GDNF group, which was treated with morphine (10 μmol/L) and GDNF (100 ng/ml); morphine + GDNF + NCAM Ab group, which was treated with morphine (10 μmol/L) and NCAM Ab (5 μg/ml), with GDNF (100 ng/ml) then added to the cultures at 30 min later; and morphine + NCAM Ab group, which was treated with morphine (10 μmol/L) and NCAM Ab (5 μg/ml). Subsequently, every 2 days, half of the medium was replaced and treated as described earlier until immunostaining or Western blotting was carried out.
Immunostaining
Rats were perfused through the ascending aorta with 200 ml of normal saline followed by 200 ml of 0.1 M phosphate buffer (PB, pH 7.4) containing 4 % paraformaldehyde under deep anesthesia with 10 % chloral hydrate (400 mg/kg, i.p.). After the perfusion, the brainstem was removed immediately, post-fixed overnight, and then cryoprotected for 24–48 h at 4 °C in 0.1 M PB containing 30 % sucrose. Frozen coronal sections (35 μm in thickness) were cut in a cryostat and collected the level of VTA in 0.01 M phosphate-buffered saline (PBS, pH 7.4). Sections were rinsed in 0.01 M PBS (pH 7.4) for three times (10 min each), blocked with 10 % donkey serum in 0.01 M PBS containing 0.3 % Triton X-100 for 2 h at room temperature (RT), and then used for immunofluorescent staining. The sections were incubated overnight at 4 °C with the primary antibodies: mouse anti-tyrosine hydroxylase (TH) (1:300; Millipore) mixed with rabbit anti-NCAM (1:100; Abcam). After that, the sections were washed for three times in 0.01 M PBS (10 min each) and then incubated for 2 h at RT with the corresponding secondary antibody: FITC-conjugated donkey anti-mouse IgG (1:200; Abcam) and TRITC-conjugated donkey anti-rabbit IgG (1:200; Abcam). Images were obtained using a confocal laser microscope (FV1000; Olympus, Tokyo, Japan), and digital images were captured with Fluoview 1000 (Olympus).
At DIV 10, the primary cultures were fixed with 4 % paraformaldehyde for 20 min at RT. After three washes with PBS, the cells were permeabilized with 0.01 M PBS containing 0.3 % Triton X-100 for 20 min and then blocked with 10 % donkey serum in PBS for 30 min. Other procedures were the same as those described earlier.
Western Blotting and Co-immunoprecipitation
To detect the expression level of NCAM in the VTA in vivo and in vitro, bilateral VTA tissues of rats were punched out on ice and then mechanically lysed in RIPA Lysis Buffer (Beyotime Institute of Biotechnology) containing 50 mM Tris (pH 7.4), 150 mM NaCl, 1 % Triton X-100, 1 % sodium deoxycholate, 0.1 % SDS, sodium orthovanadate, and 1 mM phenylmethylsulfonyl fluoride. The tissues were homogenized for 30 s and then centrifuged at 12,000 × g for 15 min at 4 °C. After centrifugation, the supernatants were retained and stored at −80 °C and were thawed once. The cultured VTA cells were washed with ice-cold PBS for three times. After lysing in ice-cold RIPA Lysis Buffer for 10 min, cell proteins were harvested with a cell scraper and stored at −80 °C. The concentration of proteins was determined by the bicinchoninic acid protein assay. Equal amounts of sample extract (60 μg) were subjected to 8 % SDS-PAGE gels and then transferred to a PVDF membrane by semi-dry transfer method. The membrane was blocked with 3 % bovine serum albumin for 2 h at RT and then incubated overnight at 4 °C with rabbit anti-NCAM antibody (1:500, Santa Cruz). After the membrane was washed 5 min for three times in wash buffer, it was incubated in the appropriate alkali phosphatase-conjugated goat anti-rabbit IgG (1:1,000, ZSGB-BIO) for 2 h at room temperature. Then, the protein band was visualized by the BCIP/NBT Alkaline Phosphatase Color Development Kit. Developed films were digitized using an Epson Perfection 2480 scanner (Seiko Corp., Nagano, Japan). Optical densities of detected proteins were obtained using Image J. For the standardization of the total protein content in each lane, membrane was incubated with a mouse primary antibody against β-actin (1:1,000; ZSGB-BIO). Other procedures were the same as described previously. In addition, to detect the expression level of TH in vitro, western blotting of TH was carried out similarly.
To detect the phosphorylation level of FAK associated with NCAM, the tissue proteins and cell proteins of VTA were obtained as described earlier. After that, 400 μl of IP buffer (50 mM HEPES, 10 % glycerol, 150 mM NaCl, 1.5 mM MgCl2, 1 mM ZnCl2, 1 mM EDTA, 1 mM EGTA, 50 mM NaF, 20 mM NaPPi, 20 mM β-phosphoglycerol, 1 mM PNPP, 1 mM Na3VO4, 0.5 % Nonidet P-40 (NP-40), 1 % Triton-X100, benzamidine (100 μg/ml), phenylmethylsulfonyl fluoride (5 μg/ml), pepstatin A (5 μg/ml), leupeptin (5 μg/ml), aprotinin (5 μg/ml)) was added to the extracts containing 500 μg protein, and then the mixture was incubated with rabbit anti-rat NCAM antibody (10 μl, Santa Cruz) for 6 h at 4 °C. Immune complex was collected by incubation (2 h, 4 °C) with protein A/G PLUS-Agarose (20 μl, Santa Cruz). After an extensive wash with IP buffer, immunoprecipitated proteins were dissolved in 8 % SDS-PAGE and analyzed by Western blotting with phosphorylated FAK antibody (Tyr397, 1:1,000, Epitomics).
Measurement of the Size of Cell Bodies and Neurite Outgrowth of DA Neuron
Effects of morphine, GDNF, and NCAM Ab on the size of cell bodies and neurite outgrowth of DA neurons were measured and quantified. All TH-positive neurons were included for measurement. The average lengths of the maximum and the minimum diameter of cell body per TH-positive neuron were used as indices of the cell bodies’ size of DA neurons, and the average number and lengths of neurites per TH-positive neuron were used as indices of DA neurite outgrowth. A neurite was defined as the neuronal process which extends directly from the soma. The branches from such processes were also included for quantification and values were added together. When the length of a neurite was shorter than the diameter of the soma of a given neurons, this neurite was not included for quantification. The lengths of neurites and cell body’s diameter per TH-positive neuron were measured by the Image-Pro Plus v.6.0 software.
Statistical Analysis
Values were expressed as means ± S.E.M. All statistical tests were undertaken in SPSS v.16.0 software. Statistical differences among more than three groups were determined using a one-way analysis of variance (ANOVA), followed by Student–Newman–Keuls (SNK) test. The minimal level of significance accepted was set at P < 0.05 level.
Results
Co-expression of TH with NCAM in the VTA of Rats
NCAM has been shown to be involved in the formation of drug addiction (Barker et al. 2012; Mackowiak et al. 2011), while the VTA, especially the DA neurons, is an important part of the neural circuits associated with drug addiction. It has been shown that chronic morphine treatment significantly decreases the size and caliber of dendrites and cell bodies of VTA dopamine neurons, an effect not seen for the non-dopaminergic neurons of the VTA (Sklair-Tavron et al. 1996). If NCAM is involved in the formation of drug addiction, we predicted that NCAM might well be expressed in the VTA, including the DA neurons. To examine this, we performed immunofluorescent double-labeling in the VTA of rats. Double-labeling studies revealed that NCAM was widely expressed in the VTA of rats, including all tyrosine hydroxylase (a marker of DA neurons)-positive neurons (Fig. 1), supporting our hypothesis that NCAM might be involved in the formation of morphine addiction.
Co-expression of TH with NCAM in the VTA of rats. Shown is dual-channel immunofluorescence for NCAM (red), tyrosine hydroxylase (green), and merged (yellow). a Images of VTA area (scale bar 500 μm). b Enlarged images of VTA area. The arrowheads point to cells immunostained both for NCAM and TH (scale bar 40 μm)
Chronic Morphine Treatment Down-Regulated the NCAM Signaling in the VTA In Vivo and In Vitro, but Not the Expression of NCAM
NCAM is a prominent cell adhesion molecule in the nervous system, where it has been shown to participate in a number of developmental processes including cell migration, neurite outgrowth, and synaptic plasticity. The ability of NCAM to influence developmental events can result both from its adhesive as well as its signaling properties (Saffell et al. 1995). Alternative splicing of NCAM mRNA generates three major protein isoforms as follows: transmembrane forms of 140 and 180 kDa, and a 120-kDa glycophosphatidylinositol-linked isoform (Hinsby et al. 2004). The cytoplasmic domains of the transmembrane isoforms may mediate interactions with intracellular cytoskeletal and signaling molecules. It has been demonstrated that the intracellular domain of NCAM was associated with Fyn, a member of Src family tyrosine kinases. Fyn becomes rapidly and transiently activated upon NCAM ligation, leading to recruitment and activation of the FAK, a nonreceptor tyrosine kinase known to participate in cytoskeletal rearrangements, and FAK has been shown to co-immunoprecipitate with Fyn and NCAM in COS and B35 cells upon NCAM stimulation (Beggs et al. 1997). Accordingly, NCAM-mediated neurite outgrowth has been reported to be abolished in PC12 cells that express a dominantly negative FAK (Kolkova et al. 2000).
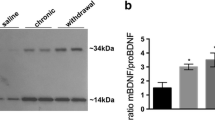
In the present study, it was investigated whether chronic morphine treatment affected the expression of NCAM or the phosphorylation of NCAM-associated FAK in the VTA in vivo and in vitro. At 12 h after the last injection with morphine or saline, bilateral VTA tissues of rats were punched out, and the cultured VTA cells treated with morphine or PBS were harvested at DIV 10; then, they were subjected to an immunoblotting or co-immunoprecipitation assay. The results in vivo and in vitro showed that the phosphorylated FAK in NCAM immunoprecipitates decreased dramatically in a time-dependent manner with morphine exposure, but the expression of NCAM has no significant change (Fig. 2), indicating that the down-regulation of NCAM signaling might be involved in the formation of morphine addiction.
Chronic morphine treatment down-regulated the phosphorylation level of NCAM-associated FAK in the VTA, but not the expression of NCAM in vivo and in vitro. a Quantitative analysis for levels of NCAM and NCAM-associated phosphorylated FAK (Tyr397) in the VTA of rats after repeated morphine or saline injection. b Quantitative analysis for levels of NCAM and NCAM-associated phosphorylated FAK (Tyr397) in primary cultured VTA cells with chronic morphine or PBS treatment. Statistical significance was evaluated by ANOVA followed by Student–Newman–Keuls test. Statistical analyses revealed that chronic morphine treatment had no effect on the expression of NCAM but decreased markedly the phosphorylation of NCAM-associated FAK in the VTA of rats in vivo and in vitro (*P < 0.05 vs. saline/PBS; n = 3). Data are presented as the mean integrated density value of three separate experiments
GDNF Up-Regulated the NCAM Signaling in Cultured VTA Cells but Had No Effect on the Expression of NCAM
The above results revealed that NCAM signaling might be involved in the formation of morphine addiction. However, these results do not tell whether NCAM signaling is involved in the negative regulatory effects of GDNF on morphine addiction.
In the present study, it was investigated whether GDNF was able to regulate the expression of NCAM or the NCAM signaling in cultured VTA cells. At DIV 10, cultures were harvested and subjected to a western blotting and co-immunoprecipitation assay. Statistical analysis revealed that GDNF had no effect on the expression of NCAM but markedly up-regulated the phosphorylation of NCAM-associated FAK (Fig. 3). Moreover, pre-treatment with NCAM Ab abolished the up-regulation of phosphorylated FAK induced by GDNF.
GDNF increased the phosphorylation of NCAM-associated FAK in primary cultured cells derived from newborn (postnatal day 0) rat VTA but had no effect on the expression of NCAM. Quantitative analysis for levels of a NCAM and b NCAM-associated phosphorylated FAK (Tyr397) in primary cultured cells derived from the VTA of newborn (postnatal day 0) rats. Cultures were treated as described in “Materials and Methods”. Cellular proteins were obtained at DIV 10 and then subjected to Western blotting and co-immunoprecipitate. The results showed that GDNF had no effect on the expression of NCAM but increased dramatically the phosphorylation of NCAM-associated FAK, and this effect could be antagonized by NCAM Ab (# P < 0.05 vs. PBS; *P < 0.05 vs. morphine; ※ P < 0.05 vs. morphine + GDNF). Data are presented as the mean integrated density value of three separate experiments
NCAM Signaling Mediated the Effect of GDNF on the Morphine-Induced Morphological Changes of VTA Dopamine Neurons
Although the above results demonstrated that GDNF significantly up-regulated the NCAM signaling in cultured VTA cells, we do not know whether this up-regulation of NCAM signaling actually mediates the effects of GDNF on the morphine-induced morphological changes of VTA dopamine neurons, including the decreases of the number and length of neurites and the size of cell bodies of DA neurons. The present experiment was designed to address this issue. Function-blocking anti-NCAM Ab was used. Immunofluorescence results showed that there was a visible decrease in the number and length of neurites and the size of cell bodies of TH-positive neurons treated with morphine (Fig. 4b), which was consistent with the results of previous studies (Sklair-Tavron et al. 1996), and this decrease was reversed by GDNF (Fig. 4c). Additionally, NCAM Ab alone did not markedly affect the size of cell bodies and neurite outgrowth of TH-positive neurons (Fig. 4e), but it significantly antagonized the effect of GDNF on this measure (Fig. 4d). The quantitative results are shown in Fig. 4f–h. These results indicated that NCAM signaling was involved in the effect of GDNF on the morphological changes of VTA dopamine neurons induced by chronic morphine.
Effect of GDNF and NCAM Ab on the morphology of primary cultured DA neurons derived from the VTA of newborn (postnatal day 0) rat. a TH-positive neurons in the control group. b Chronic morphine exposure markedly decreased the number and length of neurites and the size of cell bodies of TH-positive neurons. c Extensive neurite outgrowth and increased cell bodies of TH-positive neuron treated with GDNF was shown when compared with the morphine group (b). d NCAM Ab abolished the effect of GDNF on the cell bodies’ size and neurite outgrowth of TH-positive neuron. e NCAM Ab alone did not affect the cell bodies’ size and neurite outgrowth of TH-positive neuron (scale bar 40 μm). Quantitative analysis of the size of cell bodies of DA neurons was expressed as f the average lengths of the maximum and the minimum diameter of cell body per TH-positive neuron, and neurite outgrowth of DA neurons was expressed as g the average number of neurites per TH-positive neuron and h the average length of neurites per TH-positive neuron. Statistical significance was done by ANOVA followed by the Student–Newman–Keuls test (# P < 0.05 vs. PBS; *P < 0.05 vs. morphine; ※ P < 0.05 vs. morphine + GDNF). Cultures were treated as described in “Materials and Methods” and stained for TH at DIV 10. The number of cells ranged from 30 to 38 in each group. Experiments were repeated in three independent batches of cultures
NCAM Signaling Mediated the Effect of GDNF on the Morphine-Induced Increase of TH in the VTA Dopamine Neurons
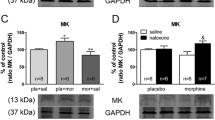
To investigate whether NCAM signaling was also involved in the effects of GDNF on the morphine-induced increase of TH in the VTA dopamine neurons, NCAM Ab was used to functionally block the extracellular domain of NCAM, and western blotting of TH was carried out. The results showed that chronic morphine increased dramatically the TH level, and GDNF reversed this increase. Prior administration of NCAM Ab partially but significantly antagonized the effect of GDNF on TH level (Fig. 5), indicating that NCAM signaling was involved in the effect of GDNF on the morphine-induced increase of TH in the VTA dopamine neurons.
NCAM signaling was involved in the effect of GDNF on the increased TH expression induced by chronic morphine treatment in vitro. Cultures were treated as described in “Materials and Methods”, and the level of TH protein in 60 μg of cytosol extract was determined by Western blot analysis at DIV 10. Statistical analysis revealed that chronic morphine increased dramatically the TH level, and GDNF reversed this increase. NCAM Ab pre-treatment alone did not markedly affect the TH level, but it significantly antagonized the effect of GDNF on TH level. Data are presented as the mean integrated density value of three separate experiments. Statistical significance difference was set at p < 0.05 (# P < 0.05 vs. PBS; *P < 0.05 vs. morphine; ※ P < 0.05 vs. morphine + GDNF)
Discussion
Addiction is a neuropsychiatric disorder for which effective treatments remain inadequate for those who are afflicted by the illness. More recently, a growing number of studies have demonstrated that GDNF plays a unique role in negatively regulating the drug- and alcohol-induced neural and behavioral plasticity related to addiction (Carnicella and Ron 2009; Ghitza et al. 2010). Although several mechanisms of GDNF in regulating alcohol addiction have been described, such as through reversing an alcohol-induced allostatic DA deficiency in the mesolimbic system (Barak et al. 2011b), positive-autoregulating its own mRNA and protein levels in an autocrine manner (Barak et al. 2011a), and inhibiting the interaction of TH with heat shock protein 90 (He and Ron 2008), those underlying the effect of GDNF on drug addiction remain unclear.
NCAM, which is considered as a mediator of cell–cell adhesion, as well as a signaling receptor that responds to both homophilic and heterophilic cues, has been demonstrated to participate in a number of plastic processes including learning, memory (Cremer et al. 1998), and cocaine and alcohol addiction (Barker et al. 2012; Mackowiak et al. 2011). NCAM can influence plastic processes through both its adhesive as well as its signaling properties. Furthermore, Paratcha et al. (2003) demonstrated that NCAM could function as a signaling receptor for GDNF. Based on the said evidence, we speculated that GDNF might regulate negatively the drug-induced neural and behavioral plasticity related to addiction via altering the expression of NCAM or its signaling levels. In the present study, immunostaining results showed that NCAM is widely expressed in the VTA of rats, a brain region that is a critical component of the neural circuitry related to drug addiction. In addition, the results of Western blotting and co-immunoprecipitation in vivo and in vitro showed that chronic morphine treatment had no effect on the expression of NCAM but down-regulated markedly the phosphorylation of NCAM-associated FAK. These results suggested that down-regulation of NCAM signaling in the VTA might be involved in the formation of morphine addiction. Amazingly, our results also showed that NCAM-associated phosphorylated FAK, but not the total NCAM, was up-regulated after GDNF administration in vitro, supporting our speculation that GDNF might regulate negatively the drug-induced neural and behavioral plasticity related to addiction via altering the expression of NCAM or its signaling levels.
To further confirm whether NCAM signaling actually mediates the effects of GDNF on morphine-induced neuroadaptations, which was thought to underlie morphine-induced behavioral plasticity (Nestler 2001; Sklair-Tavron et al. 1996), the NCAM Ab was administrated prior to GDNF. The results showed that chronic morphine exposure visibly decreased the number and length of neurites and the size of cell bodies of DA neurons in VTA cultures, which were consistent with the findings of Sklair-Tavron et al. (1996). Furthermore, our present study firstly showed that these morphine-induced morphological changes of VTA dopamine neurons could be prevented by GDNF. However, this effect of GDNF was antagonized by NCAM Ab, suggesting that NCAM signaling mediated the effect of GDNF on the morphological changes of VTA dopamine neurons induced by chronic morphine.
Another striking morphine-induced adaptation in the VTA is the increase of TH, the rate-limiting enzyme in the biosynthesis of dopamine. Our results revealed that GDNF could prevent the morphine-induced increase of TH level in the VTA cultures, which has been demonstrated by in vivo experiment (Messer et al. 2000). Prior administration of NCAM Ab did not affect TH level alone, partially, but significantly antagonized the effect of GDNF on TH level, indicating that NCAM signaling was involved in the effect of GDNF on the morphine-induced increase of TH level in the VTA.
By virtue of all the above findings, we are entitled to conclude that NCAM signaling mediates the effects of GDNF on some of morphine-induced neuroadaptations, including the morphological changes of DA neurons and the increase of TH level in the VTA. Moreover, our results also support a hypothesis that some of the morphine-induced neuroadaptations in the VTA might be due to morphine perturbation of GDNF signaling pathway (Messer et al. 2000). Together with the evidence that another neurotrophin, brain-derived neurotrophic factor (BDNF), has the same effects on the morphine-induced morphological changes of DA neurons and the induction of TH in the VTA as GDNF (Berhow et al. 1996; Sklair-Tavron et al. 1996), we speculated that some of the morphine-induced neuroadaptations in the VTA might be achieved via morphine perturbation of GDNF and BDNF shared signaling cascades. Correspondingly, it has been demonstrated that chronic morphine administration increased the phosphorylation state and activity of extracellular signal regulated kinase (ERK), a major effector of GDNF and BDNF, selectively in the VTA (Berhow et al. 1996), and direct evidence has been obtained to implicate such regulation of ERK in chronic morphine induction of TH in the VTA. Interestingly, Nicole et al. (2001) demonstrated that the neuroprotective effect of GDNF was achieved via activating the ERK pathway as well. These two conclusions appear to be contradictory, and a similar phenomenon also occurs in BDNF (Berhow et al. 1996). How to explain this so-called contradiction? The results from Berhow et al. (1996) suggested that chronic BDNF elicited a compensatory increase in the phosphorylation of the remaining ERK molecules and thereby prevents any additional increase in response to morphine exposure. This may also be the mechanism of action of GDNF on morphine-induced neuroadaptations, although direct evidence has not yet been put forward. Given this, in combination with our results, one possible signaling pathway of GDNF regulation of the morphine-induced neuroadaptations in the VTA is the GDNF–NCAM–FAK–ERK pathway, while additional work is clearly needed to directly demonstrate it.
In conclusion, the present results suggested that NCAM signaling was involved in the effects of GDNF on morphine-induced neuroadaptations, including the morphological changes of DA neurons and the increase of TH level in the VTA in vitro. However, subsequent steps in this signaling pathway have not been established; clearly, more work is needed to determine the postreceptor signaling pathways by which GDNF produces its physiological effects on morphine-induced neuroadaptations. Moreover, it will be essential in future studies to further confirm whether NCAM signaling mediates the effects of GDNF on morphine-induced behavioral plasticity. It should also be emphasized that activation of NCAM signaling is likely just one of several mechanisms by which GDNF regulate chronic morphine-induced neuroadaptations in the VTA. As just one example, the integrins, another kind of cell adhesion molecule, were also shown to be involved in the effect of GDNF on DA neurons (Chao et al. 2003). Nevertheless, the present results demonstrated that NCAM signaling mediated the effects of GDNF on some of morphine-induced neuroadaptations. Although GDNF has been proven to be a possible target to treat addiction, it is unlikely that GDNF itself could be used as a therapeutic agent because they are often labile and their delivery to the target is complicated by the fact that they do not cross the blood–brain barrier (Kastin et al. 2003). Therefore, the finding of small molecules that can be applied systemically to activate the receptors and the postreceptor signaling pathways of GDNF may have important clinical significance for addiction treatment. The finding in the present study that NCAM signaling mediated the effects of GDNF on some of morphine-induced neuroadaptations probably opens a new and promising avenue for the development of therapeutic approaches to treat addiction.
Abbreviations
- GDNF:
-
Glial cell line-derived neurotrophic factor
- NCAM:
-
Neural cell adhesion molecule
- FAK:
-
Focal adhesion kinase
- VTA:
-
Ventral tegmental area
- DA:
-
Dopamine
- TH:
-
Tyrosine hydroxylase
References
Alzoubi KH, Srivareerat M, Aleisa AM, Alkadhi KA (2013) Chronic caffeine treatment prevents stress-induced LTP impairment: the critical role of phosphorylated CaMKII and BDNF. J Mol Neurosci 49:11–20
Barak S, Ahmadiantehrani S, Kharazia V, Ron D (2011a) Positive autoregulation of GDNF levels in the ventral tegmental area mediates long-lasting inhibition of excessive alcohol consumption. Transl Psychiatry 1
Barak S, Carnicella S, Yowell QV, Ron D (2011b) Glial cell line-derived neurotrophic factor reverses alcohol-induced allostasis of the mesolimbic dopaminergic system: implications for alcohol reward and seeking. J Neurosci 31:9885–9894
Barker JM, Torregrossa MM, Taylor JR (2012) Low prefrontal PSA-NCAM confers risk for alcoholism-related behavior. Nat Neurosci 15:1356–1358
Beggs HE, Baragona SC, Hemperly JJ, Maness PF (1997) NCAM140 interacts with the focal adhesion kinase p125(fak) and the SRC-related tyrosine kinase p59(fyn). J Biol Chem 272:8310–8319
Berhow MT, Hiroi N, Nestler EJ (1996) Regulation of ERK (extracellular signal regulated kinase), part of the neurotrophin signal transduction cascade, in the rat mesolimbic dopamine system by chronic exposure to morphine or cocaine. J Neurosci 16:4707–4715
Carnicella S, Ron D (2009) GDNF—a potential target to treat addiction. Pharmacol Ther 122:9–18
Chao CC, Ma YL, Chu KY, Lee EH (2003) Integrin alphav and NCAM mediate the effects of GDNF on DA neuron survival, outgrowth, DA turnover and motor activity in rats. Neurobiol Aging 24:105–116
Cox ET, Brennaman LH, Gable KL, Hamer RM, Glantz LA, Lamantia AS, Lieberman JA, Gilmore JH, Maness PF, Jarskog LF (2009) Developmental regulation of neural cell adhesion molecule in human prefrontal cortex. Neuroscience 162:96–105
Cremer H, Chazal G, Carleton A, Goridis C, Vincent JD, Lledo PM (1998) Long-term but not short-term plasticity at mossy fiber synapses is impaired in neural cell adhesion molecule-deficient mice. Proc Natl Acad Sci U S A 95:13242–13247
Di Chiara G, North RA (1992) Neurobiology of opiate abuse. Trends Pharmacol Sci 13:185–193
Durbec P, Marcos-Gutierrez CV, Kilkenny C, Grigoriou M, Wartiowaara K, Suvanto P, Smith D, Ponder B, Costantini F, Saarma M et al (1996) GDNF signalling through the Ret receptor tyrosine kinase. Nature 381:789–793
Ghitza UE, Zhai H, Wu P, Airavaara M, Shaham Y, Lu L (2010) Role of BDNF and GDNF in drug reward and relapse: a review. Neurosci Biobehav Rev 35:157–171
Gong P, Zheng A, Chen D, Ge W, Lv C, Zhang K, Gao X, Zhang F (2009) Effect of BDNF Val66Met polymorphism on digital working memory and spatial localization in a healthy Chinese Han population. J Mol Neurosci 38:250–256
He DY, Ron D (2008) Glial cell line-derived neurotrophic factor reverses ethanol-mediated increases in tyrosine hydroxylase immunoreactivity via altering the activity of heat shock protein 90. J Biol Chem 283:12811–12818
Hinsby AM, Berezin V, Bock E (2004) Molecular mechanisms of NCAM function. Front Biosci 9:2227–2244
Inoue Y, Yao L, Hopf FW, Fan P, Jiang Z, Bonci A, Diamond I (2007) Nicotine and ethanol activate protein kinase A synergistically via G(i) betagamma subunits in nucleus accumbens/ventral tegmental cocultures: the role of dopamine D(1)/D(2) and adenosine A(2A) receptors. J Pharmacol Exp Ther 322:23–29
Kalivas PW, McFarland K (2003) Brain circuitry and the reinstatement of cocaine-seeking behavior. Psychopharmacol (Berl) 168:44–56
Kalivas PW, O'Brien C (2008) Drug addiction as a pathology of staged neuroplasticity. Neuropsychopharmacology 33:166–180
Kalivas PW, Volkow ND (2005) The neural basis of addiction: a pathology of motivation and choice. Am J Psychiatry 162:1403–1413
Kastin AJ, Akerstrom V, Pan W (2003) Glial cell line-derived neurotrophic factor does not enter normal mouse brain. Neurosci Lett 340:239–241
Kelley AE, Berridge KC (2002) The neuroscience of natural rewards: relevance to addictive drugs. J Neurosci 22:3306–3311
Kolkova K, Novitskaya V, Pedersen N, Berezin V, Bock E (2000) Neural cell adhesion molecule-stimulated neurite outgrowth depends on activation of protein kinase C and the Ras-mitogen-activated protein kinase pathway. J Neurosci 20:2238–2246
Lin LF, Doherty DH, Lile JD, Bektesh S, Collins F (1993) GDNF: a glial cell line-derived neurotrophic factor for midbrain dopaminergic neurons. Science 260:1130–1132
Mackowiak M, Mordalska P, Dudys D, Korostynski M, Bator E, Wedzony K (2011) Cocaine enhances ST8SiaII mRNA expression and neural cell adhesion molecule polysialylation in the rat medial prefrontal cortex. Neuroscience 186:21–31
Maldonado R (2003) The neurobiology of addiction. J Neural Transm Suppl 1–14
Maness PF, Beggs HE, Klinz SG, Morse WR (1996) Selective neural cell adhesion molecule signaling by Src family tyrosine kinases and tyrosine phosphatases. Perspect Dev Neurobiol 4:169–181
Markram K, Gerardy-Schahn R, Sandi C (2007) Selective learning and memory impairments in mice deficient for polysialylated NCAM in adulthood. Neuroscience 144:788–796
Messer CJ, Eisch AJ, Carlezon WA Jr, Whisler K, Shen L, Wolf DH, Westphal H, Collins F, Russell DS, Nestler EJ (2000) Role for GDNF in biochemical and behavioral adaptations to drugs of abuse. Neuron 26:247–257
Nestler EJ (2001) Molecular basis of long-term plasticity underlying addiction. Nat Rev Neurosci 2:119–128
Nicole O, Ali C, Docagne F, Plawinski L, MacKenzie ET, Vivien D, Buisson A (2001) Neuroprotection mediated by glial cell line-derived neurotrophic factor: involvement of a reduction of NMDA-induced calcium influx by the mitogen-activated protein kinase pathway. J Neurosci 21:3024–3033
Paratcha G, Ledda F, Ibanez CF (2003) The neural cell adhesion molecule NCAM is an alternative signaling receptor for GDNF family ligands. Cell 113:867–879
Pascual A, Hidalgo-Figueroa M, Piruat JI, Pintado CO, Gomez-Diaz R, Lopez-Barneo J (2008) Absolute requirement of GDNF for adult catecholaminergic neuron survival. Nat Neurosci 11:755–761
Pierce RC, Kumaresan V (2006) The mesolimbic dopamine system: the final common pathway for the reinforcing effect of drugs of abuse? Neurosci Biobehav Rev 30:215–238
Saffell JL, Doherty P, Tiveron MC, Morris RJ, Walsh FS (1995) NCAM requires a cytoplasmic domain to function as a neurite outgrowth-promoting neuronal receptor. Mol Cell Neurosci 6:521–531
Sklair-Tavron L, Shi WX, Lane SB, Harris HW, Bunney BS, Nestler EJ (1996) Chronic morphine induces visible changes in the morphology of mesolimbic dopamine neurons. Proc Natl Acad Sci U S A 93:11202–11207
Smith-Swintosky VL, Gozes I, Brenneman DE, D'Andrea MR, Plata-Salaman CR (2005) Activity-dependent neurotrophic factor-9 and NAP promote neurite outgrowth in rat hippocampal and cortical cultures. J Mol Neurosci 25:225–238
Suder P, Bogusiewicz A, Rolka K, Laidler P, Kotlinska J, Silberring J (2003) Rat neuronal cells in primary culture as a model for nociceptin/orphanin FQ metabolism. Neurosci Lett 348:167–170
Treanor JJ, Goodman L, de Sauvage F, Stone DM, Poulsen KT, Beck CD, Gray C, Armanini MP, Pollock RA, Hefti F, Phillips HS, Goddard A, Moore MW, Buj-Bello A, Davies AM, Asai N, Takahashi M, Vandlen R, Henderson CE, Rosenthal A (1996) Characterization of a multicomponent receptor for GDNF. Nature 382:80–83
Vlaskovska M, Kasakov L, Suder P, Silberring J, Terenius L (1999) Biotransformation of nociceptin/orphanin FQ by enzyme activity from morphine-naive and morphine-treated cell cultures. Brain Res 818:212–220
Acknowledgments
This project was supported by grants from the National Natural Science of China (30900417 and 30901402) and the Educational Department Science Research Foundation of Jiangsu Province (08KJB180011 and 09KJD320008). The authors declare no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Li Li Junping Cao, and Suming Zhang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Li, L., Cao, J., Zhang, S. et al. NCAM Signaling Mediates the Effects of GDNF on Chronic Morphine-Induced Neuroadaptations. J Mol Neurosci 53, 580–589 (2014). https://doi.org/10.1007/s12031-013-0224-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-013-0224-0