Abstract
Follicular growth, ovulation, and luteinization are influenced by interactions of peptide and steroid hormone-signaling cascades in the ovary. Pituitary adenylate cyclase-activating polypeptide (PACAP) plays an important role in the regulation of several endocrine processes and is present in ovarian follicular fluid (FF). However, little is known about PACAP in FF with regard to maturation, ovulation, fertilization, and successful pregnancy. The aim of this pilot study was to investigate whether there is a correlation between PACAP concentration in FF and ovarian response to superovulation treatment in infertile women, performed in volunteers (n = 132; aged between 20 and 35). After treatment, the number of harvested oocytes was recorded and PACAP immunoreactivity in FF was measured by radioimmunoassay. All the corresponding PACAP concentrations were below 290 fmol/ml in cases when the number of harvested oocytes exceeded 14 per patient, while in all cases above 290 fmol/ml, the number of oocytes was below 14. Using these cutoff values, we determined three study groups: high-PACAP concentration, high-oocyte number, and low-PACAP concentration–low-oocyte number groups. Median values of PACAP concentration in these groups were 411.2, 106.5, and 101.0 fmol/ml, respectively, while the median values of harvested oocytes were 5.5, 19.0, and 5.0, respectively. Differences were significant, indicating a correlation between concentration of PACAP in FF and the number of recruited oocytes. Higher concentrations of PACAP in FF might be associated with lower number of developing oocytes, while low concentrations of PACAP might correlate with a markedly higher number of ova retrieved, thus predicting a higher chance for ovarian hyperstimulation. Our present study is among the first few human clinical studies with direct conclusions drawn for possible clinical impact of PACAP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Follicular growth, ovulation, and luteinization are influenced by interactions of peptide and steroid hormone-signaling cascades in the ovary. Although the pituitary gonadotropins follicle-stimulating hormone (FSH) and luteinizing hormone (LH) play critical regulatory roles in follicular maturation, steroidogenesis, and ovulation, their actions are also dependent on other peptidergic and non-peptidergic signaling pathways (Bodis et al. 2001, 2002; Koppan et al. 2004; Kornya et al. 2001; Richards et al. 2002). Pituitary adenylate cyclase-activating polypeptide (PACAP) was originally isolated from the hypothalamus and was named after its cAMP-increasing effect in pituitary cells (Arimura 2007; Miyata et al. 1989). It is found in two amino acid forms, PACAP38 and PACAP27, with the 38 amino acids form being predominant in human tissues (Arimura 2007; Brubel et al. 2010; Miyata et al. 1989; Sherwood et al. 2007). Although during the last two decades it has been revealed that PACAP is much more than a hypothalamo/hypophyseal neuropeptide, its involvement in functions of the endocrine system is still aimed by extensive research (Brubel et al. 2010; Sherwood et al. 2000; Vaudry et al. 2009). PACAP has been shown to play an important role in the regulation of several different endocrine processes, such as gonadotropin secretion (Koves et al. 2003; Sherwood et al. 2000; Szabo et al. 2004), fertility, receptivity, implantation, reproductive behavior (Apostolakis et al. 2004; 2005; Sherwood et al. 2007), and placental functions (Reglodi et al. 2008). Furthermore, in gonadal regulation, PACAP delays puberty (Szabo et al. 2002) and reduces follicular apoptosis in the ovary (Lee et al. 1999). Also, PACAP has been shown to have several functions in follicular development. In the rat, PACAP is stage-specifically expressed in the granulosa cells of large mature follicles before ovulation, while weaker expression has been shown in immature antral and pre-antral follicles (Gras et al. 1996; 2005; Park et al. 2001). Furthermore, PACAP is thought to play a role in primordial germ cell proliferation (Pesce et al. 1996), cyclic recruitment of immature follicles (Gras et al. 2005), follicular apoptosis (Lee et al. 1999; Vaccari et al. 2006), as well as ovarian hormone and enzyme production in human, rat, and bovine (Apa et al. 1997; 2002; Sayasith et al. 2007; Zhong and Kasson 1994). Since PACAP is known to be a trophic factor in the development of nearly all organs and since the follicular fluid is a culture medium for the maturing oocyte and its cellular environment, we hypothesize that PACAP might play a regulatory role in the follicular fluid (Sherwood et al. 2000; Vaudry et al. 2009). As a first step, we provided evidence that PACAP occurs in the human ovarian follicular fluid (FF) after superovulation treatment, using mass spectrometry analysis (Brubel et al. 2011). However, little is known about PACAP levels in FF with regard to follicular maturation, ovulation, fertilization, and successful pregnancy. Thus, the aim of this present pilot study was to investigate whether there is any correlation between PACAP concentration in FF and ovarian response to superovulation treatment in infertile women.
Materials and Methods
Patients and Treatments
Superovulation treatment was performed in female volunteers by follicular puncture after controlled ovarian hyperstimulation during the in vitro fertilization procedure (n = 132; aged between 20 and 35). All the necessary examinations, such as cervical sample, serum hormone measuring (FSH, LH, prolactin, estradiol, progesterone, testosterone, and TSH) on the 3rd and on the 21st day of the unstimulated cycle, HIV and HBsG screening, andrological examination, and hysteroscopy were performed before sample collection.
Gonadotropin-releasing hormone agonist triptorelin (0.05 mg, Decapeptyl; Ferring) was used in a long (from the 21st day of the previous cycle) or short (from the first day of the cycle) protocol. Stimulation was performed with individual dosages of human recombinant gonadotropin (Gonal-F; Serono or Puregon; Organon), varying from 100 to 200 IU from the 3rd day of the cycle. Follicular development was detected by ultrasound every second day from day 6 of the cycle onward, along with monitoring serum LH and estradiol levels. We changed the gonadotropin amount administered individually based on the size of the maturing follicles. Ovulation was induced by injection of 250 μg (7,500 IU) human recombinant chorionic gonadotropin (Ovitrelle; Serono). Clinical outcome data for the short term after in vitro fertilization (IVF) were recorded in all patient files and later compared with biochemical and ultrasound data.
Sample Collection
Follicular fluid was collected at 36 h after ovulation induction by ultrasound-guided vaginal puncture, and sample collection for the study was performed according to a protocol approved by the institutional ethics committee (PTE AOK no. 3117/2008, 3610/2009). FF from all follicles of one individual patient was pooled and then processed as one sample, determining PACAP concentrations on a per patient basis. Patients provided written approval of the sample collection in all cases. Peptidase inhibitor aprotinin was added to all samples (30 μl/ml). The number of harvested oocytes was recorded to all individual patient files.
Radioimmunoassay
The samples were weighed and centrifuged (12,000 rpm, 4°C, 30 min), and the supernatant was further processed for radioimmunoassay (RIA) analysis of PACAP38-like immunoreactivity, as previously described (Borzsei et al. 2009). Briefly, antiserum PACAP38 “88 111-3” was a kind gift of Prof. A. Arimura, New Orleans; working dilution was 1:10,000). The tracer mono-125I-labeled ovine PACAP24-38 was prepared in our laboratory (5,000 cpm/tube). Ovine PACAP38 was used as an RIA standard ranging from 0 to 1,000 fmol/ml, while the assay was prepared in 1 ml of 0.05 mol/l (pH 7.4) phosphate buffer containing 0.1 mol/l sodium chloride, 0.25 % (w/v) BSA, and 0.05 % (w/v) sodium azide. Incubation time was 48–72 h at 4°C. Separation solution was charcoal/dextran/milk powder (10/1/0.5 g in 100 ml distilled water).
Statistical Analysis
A number of harvested oocytes and PACAP concentrations in FF samples were analyzed and expressed as mean ± standard deviation (SD). We created cutoff values for the PACAP concentration and the number of harvested oocytes above mean ± SD for PACAP and number of oocytes, thus creating three groups of data as follows: high-PACAP concentration (hP), high number of oocytes (hO), and low-PACAP concentration–low-number of oocytes (lP-lO) groups. Raw data of the groups were then processed by Kruskal–Wallis one-way analysis of variance on ranks. To isolate the group or groups differing from the others in case of statistical significance, the analysis was completed by pairwise multiple comparison procedure (Dunn's method). Results are expressed as median + 1st and 3rd quartile (1st quartile—25 % of point below; 3rd quartile—75 % of points below).
Results
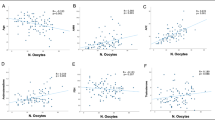
The mean number of oocytes harvested was 8.08 ± 6.02, ranging between 0 and 30 with a median value of 6.5 (Fig. 1 and Table 1). PACAP was detected in all FF samples with a mean value of 143.58 ± 110.78 fmol/ml, ranging between 28.0 and 690.0 fmol/ml with a median value of 107.75 fmol/ml (Fig. 2 and Table 1).
PACAP Concentrations
Using a cutoff value of 290 fmol/ml for PACAP concentration and 14 oocytes/patient for the number of harvested oocytes, the median values of PACAP concentration in hP (n = 12), hO (n = 17), and lP-lO (n = 103) groups were 411.2 fmol/ml (312.5–492.0 fmol/ml), 106.5 fmol/ml (61.0–180.5 fmol/ml), and 101.0 fmol/ml (72.7–139.0 fmol/ml), respectively. The differences in the median values among the groups were statistically significant (Fig. 3 and Tables 1 and 2).
Scatter plot showing number of harvested oocytes along with the corresponding concentration of PACAP in follicular fluid. Vertical dashed line represents the cutoff value of 290 fmol/ml for the PACAP concentration. Horizontal dashed line represents the cutoff value of 14 oocytes/patient for the number of harvested oocytes. Filled circles high-PACAP concentration group. Empty circles high number of oocytes group. Inverted triangle low-PACAP concentration–low-number of oocytes group
Number of Harvested Oocytes
Using the same cutoff values and groups as above, the median values of harvested oocytes per patient in the hP (n = 12), hO (n = 17), and lP-lO (n = 103) groups were 5.5 (4.0–10.0), 19.0 (15.0–21.7), and 5.0 (3.0–10.0), respectively. The differences in the median values among the groups were statistically significant (Fig. 3 and Tables 1 and 2).
Clinical Outcome Data
Within this cohort of patients, we encountered three cases of mild ovarian hyperstimulation syndrome (OHSS). In these three cases, PACAP concentrations in FF and number of oocytes retrieved were as follows: (1) 109 fmol/ml, 6/patient; (2) 312 fmol/ml, 8/patient; and (3) 79 fmol/ml, 20/patient. The median + 1st and 3rd quartile results for the data of these three patients are 109.0 fmol/ml (86.5–261.25 fmol/ml) for the PACAP and 8.0 (6.5–17.0) for the number of oocytes/patient.
Discussion
The present study provided evidence that PACAP occurs at different concentrations in human ovarian follicular fluid after superovulation treatment. Furthermore, PACAP38 was present at a detectable level without exception in all samples examined. This is in accord with our previous finding, where we showed the presence of PACAP with mass spectroscopy in all samples from a series of 40 FF of patients after the superovulation treatment (Brubel et al. 2011). The fact that PACAP occurs in all of the ovarian follicular fluid samples indicates an important biological role for PACAP in this culture medium for the developing oocyte. However, our earlier study provided no data whether PACAP concentration in FF and ovarian response to gonadotropins are related to each other. All data were obtained from the patients after superovulation treatment. Since there is no worldwide accepted research protocol covered by institutional ethical permission for sample collection under general anesthesia using transvaginal puncture of spontaneously cycling female volunteers, we have not had the chance to investigate follicular fluid samples of such individuals to compare PACAP concentrations with that of controlled hyperstimulated subjects. However, to our knowledge, the present pilot study is the first aiming to find a correlation between oocyte number and PACAP concentration in the follicular fluid. A recent study pointed out the possible correlation between the PACAP levels and post-traumatic stress syndrome in serum of human subjects suffering from this disease (Ressler et al. 2011). Thus, it is an emerging field in PACAP research to find a correlation between physiologic/pathologic conditions and PACAP levels in the blood and other biological fluids.
It is well known that FF serves as a culture medium for the developing oocyte, thus providing an important milieu for germ cell development. PACAP has been shown to play an important role in follicular maturation. This neuropeptide is expressed in a stage-specific manner in the granulosa cells of large mature follicles before ovulation, and, although in a weaker manner, expression has also been shown in the wall of premature antral and pre-antral follicles (Gras et al. 1996; 2005; Park et al. 2001). Also, receptors for PACAP have been demonstrated in developing follicles (Barberi et al. 2007; Vaccari et al. 2006). Moreover, both PACAP and PAC1 receptors have been found in the corpus luteum of the rat (Kotani et al. 1997). The peptide is thought to play a role in primordial germ cell proliferation (Pesce et al. 1996), cyclic recruitment of immature follicles (Gras et al. 2005), follicular apoptosis (Lee et al. 1999; Vaccari et al. 2006), and ovarian hormone and enzyme production (Apa et al. 1997; 2002; Sayasith et al. 2007; Zhong and Kasson 1994). These data are in line with our previous and current findings about the presence of the neuropeptide in human FF.
In the present pilot study, we found two important cutoff values, one for PACAP concentration in FF and the other one for the number of developing follicles. In all cases when the number of harvested oocytes exceeded 14/patient, all the corresponding PACAP concentrations were below 290 fmol/ml, with a median value of 106.5 fmol/ml. Beyond that, in all cases when PACAP concentrations were above 290 fmol/ml (with a median value of 411.2 fmol/ml), the number of harvested oocytes was below 14/patient. The difference between PACAP concentrations of these two groups, as well as between the number of harvested oocytes proved to be statistically significant. The reason for presenting our data as separate subgroups below PACAP concentrations of 290 fmol/ml (i.e., low-PACAP/low-oocyte and high-oocyte groups) is that low-PACAP concentrations do not seem to correlate with the oocyte numbers: both low and high values occur. However, high-PACAP concentrations are always correlated to low-oocyte numbers. Thus, we conclude that below the threshold value of PACAP, the neuropeptide may not have a significant impact on the number of developing oocytes. However, above that value, it may override other intraovarian regulatory mechanisms lowering the final number of oocytes retrieved.
This finding might draw attention, especially in the light of the pathomechanism, to the OHSS. This is an iatrogenic and potentially life-threatening condition resulting from excessive ovarian stimulation with a varying incidence between 1 and 10 % of IVF cycles (D'Angelo et al. 2011). It has been previously shown that patients were more likely to develop OHSS after superovulation treatment when they had significantly more follicles on the day of human chorionic gonadotropin (hCG) administration compared with patients without the syndrome (Jayaprakasan et al. 2007; Navot et al. 1992). A prospective study demonstrated that the cutoff number of follicles on the day of hCG administration for developing OHSS is 13 follicles (Papanikolaou et al. 2006). This cutoff value is in the range with ours, where we found a significant decrease in PACAP concentrations of the FF. This could mean that higher concentrations of PACAP in FF might be an indicator for a well-regulated follicular development in the ovary, while decreased PACAP concentrations would demonstrate a condition in favor of developing OHSS. The link between follicle number and FF concentration of PACAP is unclear. In our study, only very limited data were available for analyzing the examined variables in OHSS patients. That is why we cannot draw firm conclusion from them. However, it can be recognized that two of the OHSS patients had low-PACAP concentrations, and in the 3rd one, the concentration was in the first quartile of the group (312 fmol/ml). The overall significance of these observations promising predictive value of PACAP concentration in controlled superovulation treatment is to predict the potentially life-threatening OHSS.
In summary, our present data show, for the first time, a correlation between the concentration of PACAP in FF and the number of recruited and retrieved oocytes. The exact physiological role of PACAP in this scenario is unclear. However, based on the known effects of PACAP in oogenesis, as well as in ovarian hormonal secretion, the peptide in FF might play a role in oocyte recruitment and follicular development. Based on our present results, one might conclude that higher concentrations of PACAP in FF are associated with lower number of developing oocytes, while low concentrations of PACAP might correlate with a markedly higher number of ova retrieved, thus predicting a higher chance for ovarian hyperstimulation. Our present study is among the first few human clinical studies with direct conclusions drawn for possible clinical impact of PACAP.
References
Apa R, Lanzone A, Mastrandrea M, Miceli F, Caruso A et al (1997) Control of human luteal steroidogenesis: role of growth hormone-releasing hormone, vasoactive intestinal peptide, and pituitary adenylate cyclase-activating peptide. Fertil Steril 68:1097–1102
Apa R, Lanzone A, Miceli F, Vaccari S, Macchione E, Stefanini M et al (2002) Pituitary adenylate cyclase-activating polypeptide modulates plasminogen activator expression in rat granulosa cell. Biol Reprod 66:830–835
Apostolakis EM, Lanz R, O'Malley BW (2004) Pituitary adenylate cyclase-activating peptide: a pivotal modulator of steroid-induced reproductive behavior in female rodents. Mol Endocrinol 18:173–183
Apostolakis EM, Riherd DN, O'Malley BW (2005) PAC1 receptors mediate pituitary adenylate cyclase-activating polypeptide- and progesterone-facilitated receptivity in female rats. Mol Endocrinol 19:2798–2811
Arimura A (2007) PACAP: the road to discovery. Peptides 28:1617–1619
Barberi M, Muciaccia B, Morelli MB, Stefanini M, Cecconi S, Canipari R (2007) Expression localisation and functional activity of pituitary adenylate cyclase-activating polypeptide, vasoactive intestinal polypeptide and their receptors in mouse ovary. Reproduction 134:281–292
Bodis J, Koppan M, Kornya L, Tinneberg HR, Torok A (2001) Influence of melatonin on basal and gonadotropin-stimulated progesterone and estradiol secretion of cultured human granulosa cells and in the superfused granulosa cell system. Gynecol Obstet Invest 52:198–202
Bodis J, Koppan M, Kornya L, Tinneberg HR, Torok A (2002) The effect of catecholamines, acetylcholine and histamine on progesterone release by human granulosa cells in a granulosa cell superfusion system. Gynecol Endocrinol 16:259–264
Borzsei R, Mark L, Tamas A, Bagoly T, Bay C, Csanaky K et al (2009) Presence of pituitary adenylate cyclase activating polypeptide-38 in human plasma and milk. Eur J Endocrinol 160:561–565
Brubel R, Boronkai A, Reglodi D, Racz B, Nemeth J, Kiss P et al (2010) Changes in the expression of pituitary adenylate cyclase-activating polypeptide in the human placenta during pregnancy and its effects on the survival of JAR choriocarcinoma cells. J Mol Neurosci 42:450–458
Brubel R, Reglodi D, Jambor E, Koppan M, Varnagy A, Biro Z et al (2011) Investigation of pituitary adenylate cyclase activating polypeptide in human gynecological and other biological fluids by using MALDI TOF mass spectrometry. J Mass Spectrom 46:189–194
D'Angelo A, Brown J, Amso NN (2011) Coasting (withholding gonadotrophins) for preventing ovarian hyperstimulation syndrome. Cochrane Database Syst Rev 2:CD002811
Gras S, Hannibal J, Georg B, Fahrenkrug J (1996) Transient periovulatory expression of pituitary adenylate cyclase activating peptide in rat ovarian cells. Endocrinology 137:4779–4785
Gras S, Host E, Fahrenkrug J (2005) Role of pituitary adenylate cyclase-activating peptide (PACAP) in the cyclic recruitment of immature follicles in the rat ovary. Regul Pept 128:69–74
Jayaprakasan K, Herbert M, Moody E, Stewart JA, Murdoch AP (2007) Estimating the risks of ovarian hyperstimulation syndrome (OHSS): implications for egg donation for research. Hum Fertil (Camb) 10:183–187
Koppan M, Bodis J, Verzar Z, Tinneberg HR, Torok A (2004) Serotonin may alter the pattern of gonadotropin-induced progesterone release of human granulosa cells in superfusion system. Endocrine 24:155–159
Kornya L, Bodis J, Koppan M, Tinneberg HR, Torok A (2001) Modulatory effect of acetylcholine on gonadotropin-stimulated human granulosa cell steroid secretion. Gynecol Obstet Invest 52:104–107
Kotani E, Usuki S, Kubo T (1997) Rat corpus luteum expresses both PACAP and PACAP type IA receptor mRNAs. Peptides 18:1453–1455
Koves K, Kantor O, Molnar J, Heinzlmann A, Szabo E, Szabo F et al (2003) The role of PACAP in gonadotropic hormone secretion at hypothalamic and pituitary levels. J Mol Neurosci 20:141–152
Lee J, Park HJ, Choi HS, Kwon HB, Arimura A, Lee BJ et al (1999) Gonadotropin stimulation of pituitary adenylate cyclase-activating polypeptide (PACAP) messenger ribonucleic acid in the rat ovary and the role of PACAP as a follicle survival factor. Endocrinology 140:818–826
Miyata A, Arimura A, Dahl RR, Minamino N, Uehara A, Jiang L et al (1989) Isolation of a novel 38 residue-hypothalamic polypeptide which stimulates adenylate cyclase in pituitary cells. Biochem Biophys Res Commun 164:567–574
Navot D, Bergh PA, Laufer N (1992) Ovarian hyperstimulation syndrome in novel reproductive technologies: prevention and treatment. Fertil Steril 58:249–261
Papanikolaou EG, Pozzobon C, Kolibianakis EM, Camus M, Tournaye H, Fatemi HM et al (2006) Incidence and prediction of ovarian hyperstimulation syndrome in women undergoing gonadotropin-releasing hormone antagonist in vitro fertilization cycles. Fertil Steril 85:112–120
Park JY, Park JH, Park HJ, Lee JY, Lee YI, Lee K et al (2001) Stage-dependent regulation of ovarian pituitary adenylate cyclase-activating polypeptide mRNA levels by GnRH in cultured rat granulosa cells. Endocrinology 142:3828–3835
Pesce M, Canipari R, Ferri GL, Siracusa G, De FM (1996) Pituitary adenylate cyclase-activating polypeptide (PACAP) stimulates adenylate cyclase and promotes proliferation of mouse primordial germ cells. Development 122:215–221
Reglodi D, Borzsei R, Bagoly T, Boronkai A, Racz B, Tamas A et al (2008) Agonistic behavior of PACAP6-38 on sensory nerve terminals and cytotrophoblast cells. J Mol Neurosci 36:270–278
Ressler KJ, Mercer KB, Bradley B, Jovanovic T, Mahan A, Kerley K et al (2011) Post-traumatic stress disorder is associated with PACAP and the PAC1 receptor. Nature 470:492–497
Richards JS, Russell DL, Ochsner S, Hsieh M, Doyle KH, Falender AE et al (2002) Novel signaling pathways that control ovarian follicular development, ovulation, and luteinization. Recent Prog Horm Res 57:195–220
Sayasith K, Brown KA, Sirois J (2007) Gonadotropin-dependent regulation of bovine pituitary adenylate cyclase-activating polypeptide in ovarian follicles prior to ovulation. Reproduction 133:441–453
Sherwood NM, Krueckl SL, McRory JE (2000) The origin and function of the pituitary adenylate cyclase-activating polypeptide (PACAP)/glucagon superfamily. Endocr Rev 21:619–670
Sherwood NM, Adams BA, Isaac ER, Wu S, Fradinger EA (2007) Knocked down and out: PACAP in development, reproduction and feeding. Peptides 28:1680–1687
Szabo F, Horvath J, Heinzlmann A, Arimura A, Koves K (2002) Neonatal PACAP administration in rats delays puberty through the influence of the LHRH neuronal system. Regul Pept 109:49–55
Szabo E, Nemeskeri A, Arimura A, Koves K (2004) Effect of PACAP on LH release studied by cell immunoblot assay depends on the gender, on the time of day and in female rats on the day of the estrous cycle. Regul Pept 123:139–145
Vaccari S, Latini S, Barberi M, Teti A, Stefanini M, Canipari R (2006) Characterization and expression of different pituitary adenylate cyclase-activating polypeptide/vasoactive intestinal polypeptide receptors in rat ovarian follicles. J Endocrinol 191:287–299
Vaudry D, Falluel-Morel A, Bourgault S, Basille M, Burel D, Wurtz O et al (2009) Pituitary adenylate cyclase-activating polypeptide and its receptors: 20 years after the discovery. Pharmacol Rev 61:283–357
Zhong Y, Kasson BG (1994) Pituitary adenylate cyclase-activating polypeptide stimulates steroidogenesis and adenosine 3',5'-monophosphate accumulation in cultured rat granulosa cells. Endocrinology 135:207–213
Acknowledgments
This work was supported by Hungarian National Scientific Grants (OTKA, K72592, and CNK78480), Momentum Program of the Hungarian Academy of Sciences, SROP 4.1.2.B-10/2/KONV-20/0-0002, SROP-4.2.2/B-10/1-2010-0029, Bolyai Scholarship, and University of Pecs Medical School Research Grant 2010.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Koppan, M., Varnagy, A., Reglodi, D. et al. Correlation Between Oocyte Number and Follicular Fluid Concentration of Pituitary Adenylate Cyclase-Activating Polypeptide (PACAP) in Women After Superovulation Treatment. J Mol Neurosci 48, 617–622 (2012). https://doi.org/10.1007/s12031-012-9743-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-012-9743-3