Abstract
Oxidative stress is known to be one of the major factors underlying Parkinson’s disease (PD). One of the consequences of oxidative stress is lipid peroxidation. A toxic product of lipid peroxidation, (±)-4-hydroxy-2E-nonenal (HNE) leads to membrane disruption and formation of HNE–protein adducts and such adducts have been detected in PD brain tissues. Aldehyde dehydrogenases (ALDHs) are involved in metabolizing HNE and other endogenous aldehydes. Interestingly, the cytosolic aldehyde dehydrogenase 1A1 (ALDH1A1) has been reported to be down-regulated in brain tissues affected in PD which could result in enhancement of HNE toxicity. We sought to first establish the role of ALDH1A1 in mediating HNE toxicity in PC12 cells by overexpressing ALDH1A1 and by using disulfiram, an ALDH inhibitor. Overexpression and inhibition of ALDH1A1 activity resulted in reduced and increased HNE toxicity, respectively. We then established conditions for detecting HNE–protein adducts following HNE treatment and showed that overexpression and inhibition of ALDH activity resulted in reduced and increased formation of HNE–protein adducts, respectively. We also show that 6-methyl-2-(phenylazo)-3-pyridinol, previously identified as an activator of ALDH1A1, can protect PC12 cells against HNE-mediated toxicity and can cause a small but significant decrease in levels of HNE–protein adducts. Our results should encourage identification of more potent ALDH activators and their testing in the PC12–HNE model. Such cytoprotective compounds could then be tested for their neuroprotective activity in in vivo models of oxidative stress-induced PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The pathological factor underlying Parkinson’s disease (PD) is thought to be the degeneration of dopaminergic neurons in the substantia nigra (Samii et al. 2004). The causes of this neurodegeneration are mitochondrial dysfunction, oxidative stress, excitotoxicity, apoptosis, and inflammation (Bossy-Wetzel et al. 2004; Samii et al. 2004). A pathological hallmark in the surviving neurons is the presence of Lewy bodies (Samii et al. 2004). Additionally, (±)-4-hydroxy-2E-nonenal (HNE)–protein adducts have been detected in nigral neurons in PD as well as other neurodegenerative diseases such as Alzheimer’s disease (Yoritaka et al. 1996; Sayre et al. 1997). In addition to forming adducts with proteins, HNE can also react with other cellular components such as phospholipids and nucleic acids (Schaur 2003). Protein–HNE adducts can intercalate cell membranes and change membrane fluidity (Chen and Yu 1994; Subramaniam et al. 1997). The formation of these adducts is driven by the accumulation of HNE that is itself driven through the formation of high levels of alkoxyl radicals that degenerate into saturated and unsaturated aldehydes such as HNE by a process referred to as lipid peroxidation (Siems and Grune 2003). Lipid peroxidation is the result of interaction of membrane lipids with reactive oxygen species produced under oxidative stress conditions, and oxidative stress is among the many important causes of neurodegeneration (Bossy-Wetzel et al. 2004; Samii et al. 2004). In addition to forming adducts, HNE is a pleiotropic molecule capable of acting as a signaling molecule and eliciting a variety of cellular processes such as apoptosis, differentiation, and proliferation (Yang et al. 2003).
There are at least three mechanisms to detoxify HNE to less reactive metabolites (Siems and Grune 2003) that are mediated by glutathione-S-transferases, aldose reductase, and aldehyde dehydrogenases. The aldehyde dehydrogenase superfamily includes NAD(P)+-dependent enzymes that catalyze the oxidation of a wide spectrum of aldehydes to their corresponding carboxylic acids (Black and Vasiliou 2009). Endogenous aldehydes are formed during metabolism of alcohols, amino acids, biogenic amines, vitamins, steroids, and lipids. Two such endogenous biogenic aldehydes, 3,4-dihydroxyphenylacetaldehyde (DOPAL) and HNE are metabolized by ALDHs. A number of reports and our own observations indicate that a cytosolic aldehyde dehydrogenase, ALDH1A1, is significantly down-regulated in the substantia nigra tissue of PD patients at both the RNA and protein levels (Galter et al. 2003; Mandel et al. 2005; Werner et al. 2008). Given that HNE–protein adducts have been detected in PD nigral neurons, we hypothesized the HNE metabolism might be impaired in these neurons due to the reduced ALDH1A1 activity thereby leading to accumulation of HNE–protein adducts. In this paper, we provide evidence that suggests that ALDH1A1 is involved in HNE metabolism in PC12 cells, a neuronal cell line. Specifically, we show that modulation of ALDH1A1 activity affects HNE toxicity as well as HNE–protein adduct levels in PC12 cells. Importantly, we show that a previously identified activator of ALDH1A1 activity can protect PC12 cells against HNE toxicity.
Materials and Methods
Cell Culture and Reagents
PC12 cells were cultured in DMEM medium containing 15% horse serum and 5% fetal bovine serum. Cultures were maintained at 37°C in 5% CO2 at 95% relative humidity. 6-Methyl-2-(phenylazo)-3-pyridinol referred to as S9186 in this paper (Cat# S9186) and disulfiram (Cat# 86720) were purchased from Sigma; HNE (Cat# 32100) was purchased from Cayman Chemical.
Cloning of ALDH1A1 cDNA Sequences into pcDNA3.1zeo(+) Vector
ALDH1A1 cDNA was obtained by digesting pCMV6-XL5-ALDH1A1 (Origene, SC119729) with EcoRI–XbaI and subcloned into EcoRI–XbaI-digested pcDNA3.1zeo(+) (Invitrogen) to obtain ALDH1A1-pcDNA3.1zeo(+).
Creation of PC12-ALDH1A1 Cell Line
PC12 cells were transfected with ALDH1A1-pcDNA3.1zeo(+) using GeneJammer® Reagent (Stratagene) as per manufacturer’s protocol. A stable ALDH1A1-overexpressing PC12 cell clone was selected after screening with 200 μg/ml of Zeocin for 10 days. This clone was expanded to obtain PC12-ALDH1A1 cell line.
Western Blotting
PC12 cells or stable PC12-ALDH1A1 cells in 100-mm culture dish were washed with ice-cold PBS and lysed by incubation on ice in lysis buffer containing 10 mM Tris–HCl (pH 7.4), 1% Triton X-100, 150 mM NaCl, 5 mM EDTA, 1 mM PMSF, 1 mM DTT, and 1× protease inhibitor cocktail (P8340, Sigma). Lysates were centrifuged at 14,000 rpm for 10 min at 4°C. Protein concentration of the supernatant was measured using Bradford reagent and 20 μg of total protein was used for western blotting. ALDH1A1 protein was detected using a 1:100 dilution of polyclonal anti-ALDH1A1 antibody (Abcam, ab63026), and GAPDH protein was detected using a 1:10,000 dilution of polyclonal anti-GAPDH antibody (Abcam, ab22555) as internal control.
Cell Lysate ALDH Activity Assay
PC12 cells or stable PC12-ALDH1A1 cells in 100-mm culture dish were washed with ice-cold PBS and harvested by scraping. Cell pellets were lysed using M-PER Mammalian Protein Extraction Reagent (Thermo Scientific, Product# 78503) supplemented with protease inhibitors (Roche, Catalog #: 11836170001). Cell lysates were centrifuged at 15,000 rpm at 4°C for 15 min. Protein concentration of the supernatants was measured using Bradford reagent and 78 μg of total protein from both the PC12 and PC12-ALDH1A1 cells was used in the ALDH activity assay. The activity of ALDHs in supernatants was determined by monitoring the reductive reaction of NAD+ to NADH at λ = 460 nm. The assay was performed at room temperature in 50 mM HEPES buffer pH 7.5 containing 0.01% Tween-20 and 1 mM NAD+ and 1 mM propionaldehyde as the substrate. The fluorescence signal at 460 nm was measured in three replicate reactions over 1.5 h using VICTOR 3 multilabel counter (PerkinElmer) and expressed as background subtracted fluorescence reading.
Cell Viability Assay
The proliferation and cell viability of PC12 cells and PC12-ALDH1A1 cells in Optilux 96-well plates (BD Biosciences) were evaluated using ATPliteTM 1step Luminescence ATP Detection Assay System (PerkinElmer) as per manufacturer’s protocol. The luminescence signal was measured using VICTOR 3 multilabel counter (PerkinElmer). Results are normalized using corresponding reading from nontreated cells and expressed as fraction of cell viability. For HNE treatments, 1.5 × 104 PC12 cells/well and 5 × 103 PC12-ALDH1A1 cells/well (fewer PC12-ALDH1A1 cells were seeded because these cells were larger than PC12 cells) were seeded in Optilux 96-well plate. After culture for 48 h, cells were treated with HNE for 1 h. Then cells were incubated in culture medium for 23 h and cell viability was evaluated as described above. For disulfiram ± HNE treatment, 1.5 × 104 PC12 cells/well were seeded in Optilux 96-well plate. After culture for 48 h, cells were pretreated with disulfiram for 1 h, then treated with HNE in combination with disulfiram for 1 h. After treatment, PC12 cells were incubated in culture medium for 23 h and cell viability was evaluated as described above. For ALDH1A1 activator ± HNE treatment, 1.5 × 104 PC12 cells/well were seeded in Optilux 96-well plate. After culture for 48 h, cells were treated with HNE in combination with ALDH1A1 activator S9186 for 1 h, followed by S9186 alone for 2 h. Following treatment, PC12 cells were incubated in culture medium for an additional 21 h and cell viability was evaluated as described above.
HNE–Protein Adducts Level Measurement
In 100-mm culture dishes, 3.6 × 106 PC12 or PC12-ALDH1A1 cells/dish were plated. After culture for 48 h, they were treated with HNE for 2 h and the cells were harvested for HNE–protein adducts measurement as described below. For disulfiram treatments, 3.6 × 106 PC12 cells/dish in 100-mm culture dish were plated. Cells were pretreated with disulfiram for 1 h, then treated with HNE in combination with disulfiram for 2 h. After treatment, PC12 cells were incubated in culture medium for 22 h and HNE adduct level was measured as described below. For S9186 treatments, 3.6 × 106 PC12 cells/dish in 100-mm culture dish were plated. Cells were co-treated with S9186 and HNE for 2 h. After treatment, PC12 cells were incubated in culture medium for 22 h and HNE adducts were measured as described below. In all experiments, cells were harvested by scraping and pelleted by centrifugation. Cell pellets were then washed with 1× PBS, resuspended in 1× PBS, and lysed by sonication. HNE–protein level was measured using OxiSelect™ HNE-His Adduct ELISA Kit (Cell Biolabs, Inc., Catalog #: STA-334) as per manufacturer’s protocol. In a modified protocol, cells were harvested immediately following 2 h of HNE treatment described above and processed as described above for measurement of HNE adduct level.
Statistical Analysis
Data are presented as means ± SE of four replicates each from two to four independent experiments. Statistical analysis was performed using Student’s t test in KaleidaGraph version 3.6 (Synergy Software).
Results
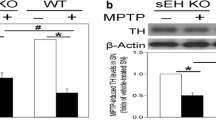
HNE is one of the major end products of lipid peroxidation and contributes to oxidative stress-related pathogenesis (Awasthi et al. 2005). To investigate the role of ALDH1A1 in the detoxification of HNE, we created a stable PC12-ALDH1A1 cell line. The overexpression of ALDH1A1 protein in stable PC12-ALDH1A1 cell line was confirmed by western blot (Fig. 1a) and resulted in significantly increased ALDH activity in this cell lysate compared to PC12 cell lysate (Fig. 1b). Then we examined the role of ALDH1A1 in the detoxification of HNE by comparing the viability of PC12 and PC12-ALDH1A1 cells after HNE treatment. Between 2.5 and 50 μM of HNE, PC12-ALDH1A1 cells are significantly more resistant to HNE-induced decrease in viability (Fig. 2). To further confirm the role of ALDH1A1 in the detoxification of HNE, modulators of ALDH activity were tested in combination with HNE. Pretreatment with 10 μM of disulfiram, an ALDH inhibitor enhanced HNE-induced decrease in cell viability by 41% to 46% (Fig. 3a). Co-treatment of HNE and S9186, an activator of ALDH1A1, protected PC12 cells against HNE-induced decrease in cell viability. S9186 at 50 μM increased viability by 36% of 10 μM HNE-treated PC12 cells and by 46% in 50 μM HNE-treated cells. S9186 at 80 μM increased cell viability by 46% in 10 μM of HNE-treated cells and by 58% in 50 μM HNE-treated cells compared to the corresponding HNE-treated cells (Fig. 3b). S9186 at 80 μM almost completely reversed the decreased viability observed in 10 μM of HNE-treated cells (Fig. 3b). We then tried to correlate the decrease in viability following HNE treatment with formation of HNE–protein adducts, using an ELISA-based method to quantify adduct levels. We first attempted to measure adduct levels using the treatment protocol that we used to follow the decrease in cell viability caused by HNE treatment. Under this protocol as described in “Materials and Methods”, we treated cells with HNE for 1 h and then placed the cells in medium only for 23 h. In these conditions, HNE–protein adduct level in HNE-treated PC12 cells was not significantly different from that in untreated cells (Fig. 4a). However, as observed previously, cell viability of HNE-treated PC12 cells was significantly decreased in a dose-dependent manner (Fig. 4b). We then measured adduct levels immediately following 2 h of HNE treatment. Surprisingly, HNE–protein adduct level in PC12 cells treated for 2 h was significantly increased in a dose-dependent manner (Fig. 4c), but no significant decrease in viability was detected at this time point (Fig. 4d). Our results suggest that there is a temporal disconnect between HNE adduct formation and decrease in cell viability in PC12 cells under the conditions described here. While HNE–protein adduct formation in treated cells is an early event, HNE-induced decrease in cell viability is detectable only as a later event. Since PC12-ALDH1A1 cells are more resistant to HNE-induced decrease in viability, we were interested in determining whether this resistance is also manifested as a difference in HNE–protein adduct levels. As shown in Fig. 5, at low HNE concentration (≤10 μM), there is no significant difference in the HNE–protein adduct levels between PC12 and PC12-ALDH1A1 cells. However, at 20 and 30 μM of HNE, HNE–protein adduct levels were significantly higher in PC12 cells compared to PC12-ALDH1A1 cells treated with the same concentration of HNE. This result could be due to an increased capacity in PC12-ALDH1A1 cells to metabolize HNE presumably due to higher ALDH1A1 activity. We next tried to determine whether the effect of modulators of ALDH1A1 activity on cell viability following HNE treatment is also manifested in adduct levels. HNE–protein adduct level in the cell lysates of PC12 cells treated with HNE in combination with either disulfiram or S9186 was measured. In 10 μM disulfiram-pretreated PC12 cells, HNE–protein adduct levels were increased by 153% and 63%, respectively, after 10 or 25 μM of HNE treatment for 2 h (Fig. 6a). In 50 μM S9186 co-treated PC12 cells, HNE–protein adduct levels were decreased by 24% and 20%, respectively, after 25 or 50 μM of HNE treatment for 2 h (Fig. 6b). This result is consistent with our findings in Fig. 5 and again offers the strong possibility that enhancement or inhibition of ALDH1A1 activity leads to decreased or increased levels of HNE–protein adduct levels with a corresponding effect on cell viability.
Overexpression of ALDH1A1 in PC12 cells. a Western blot analysis of ALDH1A1 expression in PC12-ALDH1A1 cells. The intensity of GAPDH band served as a control for loading equivalent amount of protein in lanes 3 and 4. Lane 1: magic marker. Lane 2: purified recombinant ALDH1A1 protein. Lane 3: PC12-ALDH1A1 cells. Lane 4: PC12 cells. b ALDH enzyme activity in wild-type PC12 cells and PC12-ALDH1A1 cells. ALDH enzyme activity is significantly higher in PC12-ALDH1A1 cells compared to PC12 cells. *p value < 0.001 comparing the difference of ALDH enzyme activity between PC12 and PC12-ALDH1A1 cell lysates. Statistical analysis was performed using one-tailed Student’s t test
Overexpression of ALDH1A1 protects PC12 cells from HNE-induced reduction in cell viability. Data are presented as means ± SE of two independent experiments. *p < 0.05 comparing the difference of cell viability between PC12 cells and ALDH1A1-PC12 cells. Statistical analysis was performed using Student’s t test
Effects of disulfiram and S9186 on HNE-induced reduction in cell viability. a Disulfiram enhances HNE-induced reduction in cell viability. *p < 0.01 comparing the difference in cell viability between 0 μM disulfiram pretreated PC12 cells and 10 μM of disulfiram pretreated PC12 cells at each HNE concentration. Statistical analysis was performed using one-tailed Student’s t test. b S9186 protects against HNE-induced reduction in cell viability. Data are presented as means ± SE of two independent experiments. *p < 0.05 comparing the difference of cell viability between 0 μM S9186 co-treated PC12 cells and S9186 co-treated PC12 cells at each HNE concentration. Statistical analysis was performed using one-tailed Student’s t test
HNE-induced reduction in cell viability and HNE–protein adduct formation are temporally separated. a HNE–protein adduct level in PC12 cells measured after 23 h of incubation in media following a 1-h treatment with 25 and 50 μM HNE was nearly unchanged from that of untreated cells, although the difference of HNE–protein adduct level between control and 50 μM of HNE-treated PC12 cells is still statistically significant. Data are presented as means ± SE of two independent experiments. *p < 0.05 comparing the difference of HNE–protein adduct level between 0 μM HNE-treated PC 12 cells and HNE-treated PC12 cells. b Cell viability measured after 23 h of incubation in media following a 1-h treatment with 25 and 50 μM HNE was significantly decreased. Data are presented as means ± SE of four replicates. *p < 0.001 comparing the difference of cell viability between untreated and HNE-treated PC12 cells. c HNE–protein adduct level increased in a dose-dependent manner in PC12 cells after 2 h of HNE treatment. Data are presented as means ± SE of two independent experiments. *p < 0.01 comparing the difference of HNE–protein adduct level between untreated and HNE-treated PC12 cells. d Cell viability was unchanged in PC12 cells after 2 h of 25 to 50 μM HNE treatment. Data are presented as means ± SE of four replicates. Statistical analysis was performed using Student’s t test
HNE–protein adduct level in HNE-treated PC12 cells and ALDH1A1-PC12 cells. HNE–protein adduct level was significantly lower in ALDH1A1-PC12 cells after 2 h of HNE treatment. Data are presented as means ± SE of two independent experiments. *p < 0.01 comparing the difference of HNE–protein adduct level between HNE-treated PC12 cells and HNE-treated ALDH1A1-PC12 cells. Statistical analysis was performed using one-tailed Student’s t test
Effects of disulfiram and S9186 on HNE–protein adduct level in PC12 cells. a Disulfiram increased HNE–protein adduct level in PC12 cells after 2 h of HNE treatment. Data are presented as means ± SE of two independent experiments. *p < 0.05 comparing the difference of HNE–protein adduct level between 10 μM disulfiram pretreated PC12 cells and 0 μM disulfiram pretreated PC12 cells. b S9186 decreased HNE–protein adduct level slightly in PC12 cells after 2 h of HNE treatment. Data are presented as means ± SE of two independent experiments. *p < 0.05 comparing the difference of HNE–protein adduct level between 50 μM S9186 co-treated PC12 cells and 0 μM S9186 co-treated PC12 cells. Statistical analysis was performed using one-tailed Student’s t test
Discussion
Rat PC12 pheochromocytoma cells have been widely used to investigate oxidative stress-mediated neuronal damage. More pertinently, they express the three major HNE detoxification mechanisms—glutathione-S-transferase (Raza and John 2006; Omata et al. 2008), aldose reductase (Lamensdorf et al. 2000a, b), and the aldehyde dehydrogenase, ALDH1A1 (Fig. 1). Thus, these cells are suitable for studying the effects of modulating ALDH1A1 activity on HNE toxicity in the context of the other two HNE detoxification mechanisms.
ALDH1A1 has been reported to be down-regulated in a number of PD-related reports. For example, ALDH1A1 was down-regulated threefold in a gene expression study of substantia nigra tissues from six Parkinsonian patients and six age-matched controls (Mandel et al. 2005). In another study, cytosolic aldehyde dehydrogenase mRNA levels were found to be lower in substantia nigra tissue in PD (n = 13) compared to controls (n = 14) using in situ hybridization (Galter et al. 2003). In addition, a proteomic analysis of human substantia nigra in PD revealed that ALDH1 was among the proteins whose level was lower in PD substantia nigra (Werner et al. 2008). These observations make it likely that ALDH1 activity is decreased in PD tissues which could lead to accumulation of endogenous aldehydes such as DOPAL and HNE. In fact, DOPAL accumulation has been observed in PC12 cells upon oxidative stress through complex I inhibition (Lamensdorf et al. 2000a, b), and we have found that ALDH1A1 mRNA is down-regulated in differentiated PC12 cells upon rotenone (a complex I inhibitor) treatment (data not shown). To our knowledge, there is no evidence in the literature for DOPAL accumulation in PD brains but HNE–protein adducts have been detected in nigral neurons in Parkinson disease as well as other neurodegenerative disorders such as ALS (Yoritaka et al. 1996). Hence, we decided to focus on HNE-induced cytotoxicity and HNE–protein adduct formation in PC12 cells.
We first tested the effect of overexpressing ALDH1A1 in PC12 cells and found that the resulting increased enzyme activity led to decreased HNE-induced cytotoxicity (Fig. 2). Similarly, overexpression of ALDH1A1 in the neuroblastoma-derived SH-SY5Y cells has been shown to reduce formation of HNE–protein adducts and activation of caspase-3 in these cells (Zhang et al. 2010). These results indicate that ALDH1A1 plays an important role in HNE detoxification in both of these cell lines of neuronal origin. We did attempt to test whether knocking down ALDH1A1 mRNA would have the opposite effect of increased sensitivity towards HNE. We were able to knock-down endogenous transcript levels in PC12 cells but this did not lead to reduced protein level indicating that the ALDH1A1 protein is quite stable in these cells (data not shown).
We next tested whether ALDH1A1 modulation, using compounds with inhibitory and activation properties, could affect HNE toxicity. Disulfiram is an irreversible inhibitor of both ALDH1A1 and ALDH2 with higher potency for ALDH1A1 (Lam et al. 1997). Disulfiram has been shown to inhibit ALDH activity in SH-SY5Y cells resulting in accumulation of DOPAL (Legros et al. 2004). It should be noted that disulfiram itself was toxic to PC12 cells at the concentrations tested here (data not shown). After normalization for disulfiram toxicity, disulfiram had a significant effect on enhancing HNE toxicity in PC12 (Fig. 3a). This enhancement is possibly due to inhibition of ALDH1A1 activity endogenous to PC12 cells resulting in reduced clearance of HNE. The clinical relevance of ALDH inhibition to PD is provided by a clinical report of disulfiram-induced Parkinsonism (Laplane et al. 1992).
While searching for modulators of ALDH1A1 activity, we came across PubChem data from a Quantitative High-Throughput Screen (PubChem Assay ID 1030) for inhibitors of ALDH1A1 in an in vitro assay. Ten of the 216,907 compounds tested in this screen were classified as activators because they increased the activity of ALDH1A1. We selected two compounds from among the activators based on their maximum activity, potency, and commercial availability. In the screen, S9186 (PubChem CID 6304902) was reported to have a potency of 1.12 μM with maximum activity of 29% over control reaction and P6500 (PubChem CID 5917) was reported to have a potency of 1.12 μM with maximum activity of 65% over control reaction. We found that co-treatment of S9186 and HNE for 1 h followed by treatment with 80 μM S9186 alone for 2 h led to nearly complete protection against HNE-induced decrease in cell viability (Fig. 3b). S9186 by itself had no effect on the viability of PC12 cells. On the other hand, P6500 was completely inactive in this assay (data not shown). The reason for this lack of activity is unclear because both compounds were reported to have similar effect (30–40% increased activity over control at 11.4 μM) in activating ALDH1A1 in the PubChem screen. It is possible that due to its greater hydrophilicity, P6500 is less cell-permeable compared to S9186. It is also possible that the mechanism of protection by S9186 is not through activation of ALDH1A1 activity but through inhibition of HNE toxicity. Further experiments are needed to delineate the mechanism of S9186 protection against HNE toxicity in PC12 cells. Other compounds have been reported to protect PC12 cells against HNE-induced toxicity but none of them were reported to act via ALDH1A1 (Cho et al. 2009; Jang et al. 2009, 2011).
We next sought to correlate decreased cell viability with intracellular fate of HNE in PC12 cells by measuring HNE–protein adduct levels following HNE treatment. Protein–HNE adducts can intercalate cell membranes and change membrane fluidity (Chen and Yu 1994; Subramaniam et al. 1997), and it has been reported that HNE interferes with the activities of various signal kinases to regulate cellular processes such as apoptosis mainly through the formation of HNE–protein adducts (Leonarduzzi et al. 2004). Our results indicate that there is a temporal disconnect between the formation of HNE–protein adducts and observable decrease in cell viability (Fig. 4). We first encountered this disconnect when we attempted to test whether there is reduced levels of adducts in PC12-ALDH1A1 cells compared to PC12 cells. Under the conditions (1 h HNE treatment followed by 23 h medium) in which reduced cell viability was observed following HNE treatment (Fig. 4b), adducts were slightly higher in the 50-μM HNE-treated PC12 cells and were unchanged in the 25-μM HNE-treated cells (Fig. 4a). In contrast, a much larger increase in adducts was observed in both 25 and 50 μM HNE-treated cells within 2 h of HNE treatment as shown in Fig. 4c. However, there was no decrease in cell viability at this time point (Fig. 4d).
The reasons for this temporal disconnect are unclear at this point. It is possible that the HNE–protein adducts are targeted to the proteosome where they are degraded and hence undetectable 22 h later. But before they are degraded, the adducts might cause membrane disruption which may manifest slowly as cytotoxicity (Chen and Yu 1994; Subramaniam et al. 1997). HNE has been shown to be capable of regulating activity of critical enzymes involved in apoptosis pathways which might also lead to gradual loss of cell viability (Leonarduzzi et al. 2004). Alternatively, it is possible that decrease in cell viability is independent of adduct formation and the temporally disconnected correlation we observed is coincidental. For instance, HNE itself has been shown to be a signaling molecule capable of initiating apoptosis (Yang et al. 2003; Leonarduzzi et al. 2004). Similar to our protocols, different treatment periods were used to detect adducts versus cytotoxicity and caspase activation in SH-SY5Y cells (Zhang et al. 2010) following HNE and H2O2 treatment. In this report, cytotoxicity was measured after 12 h of 20 μM HNE and 200 μM H2O2 treatment, adducts were measured after 8 h of treatment with 20 μM HNE and 200 μM H2O2 and caspase activation was observed 16 h following treatment with 200 μM H2O2. In all these instances, the cells were exposed continuously with HNE for the time periods indicated. In the report cited above, no explanation was provided for using different time points for observing these end points. We have done a more systematic comparison to show the temporal disconnect for the first time but more work is needed to understand the basis for this disconnect. It would also be interesting to determine if the temporal disconnect can be observed in markers of apoptotic process as well. In light of this temporal disconnect, different conditions were used to detect cytotoxicity and adducts in subsequent experiments. Reduced adduct levels were observed in PC12-ALDH1A1 cells upon HNE treatment (Fig. 5), indicating that the increased resistance to HNE toxicity exhibited by these cells also correlates with reduced formation of HNE–protein adducts. Both these observations are consistent with the understanding that increased ALDH1A1 activity results in increased clearance of HNE. Also, this suggests that measuring protein–HNE adduct levels is a useful indicator of the intracellular fate of HNE leading up to delayed reduction in cell viability.
We next tested whether compounds that modulate ALDH1A1 activity also affect HNE–protein adduct levels. As expected, the inhibitor disulfiram significantly increased adduct levels whereas the S9186 activator reduced adduct levels but by a lower amount relative to disulfiram (Fig. 6a, b). It is possible that in addition to activating ALDH1A1, S9186 may mediate additional nonspecific cytoprotective effects against HNE through pathways that do not involve reduction of HNE–protein adduct levels. For example, it is possible that S9186 promotes ALDH1A1-mediated HNE metabolism thereby reducing HNE concentration inside the cell to a level that actually promotes cell proliferation. As an example of this, HNE at low concentrations (1.0 and 2.5 μM) has been shown to cause cell proliferation of rat aortic smooth muscle cells (Ruef et al. 1998). It remains to be tested whether S9186 treatment for a longer period post-HNE treatment can result in greater reduction of adducts.
Further studies are needed to better understand the mechanisms by which S9186 protects against HNE toxicity. Pretreatment for 30 min with 5 or 10 μM kaempferol has been reported to protect against apoptosis caused by subsequent treatment for 24 h with 20 μM HNE in PC12 cells (Jang et al. 2011). In this case, kaempferol significantly inhibited HNE-induced activation of NADPH oxidase (NOX). This NOX activation appears to be an early pro-apoptotic signaling event—observed within 5 min of HNE treatment. In this report, adduct formation was not monitored but rather direct apoptotic signaling initiated by HNE was examined. Because S9186 can offer protection under a co-treatment regimen with HNE, the mechanism by which it confers protection warrants further studies.
It is clear that there are multiple pathways by which HNE toxicity is manifested, and consequently, multiple ways through which protection against this toxicity can be conferred (Cho et al. 2009; Jang et al. 2009, 2011). We focused on adducts and the ALDH1A1 enzyme because HNE–protein adducts have been detected in PD brains and because this enzyme is highly down-regulated in PD. This suggested that the formation of adducts and the role of ALDH1A1 in the formation of these adducts are potentially relevant to PD. The cell-based assay described here can be used to screen for additional ALDH1A1 modulator compounds for HNE detoxification with S9186 as the positive control. Alternatively, potent ALDH1A1 activators can be first identified in vitro and then tested for their ability to protect against HNE toxicity using this cell model. Such compounds may ultimately have potential in the treatment of PD.
References
Awasthi YC, Ansari GA, Awasthi S (2005) Regulation of 4-hydroxynonenal mediated signaling by glutathione S-transferases. Methods Enzymol 401:379–407
Black W, Vasiliou V (2009) The aldehyde dehydrogenase gene superfamily resource center. Hum Genomics 4:136–142
Bossy-Wetzel E, Schwarzenbacher R, Lipton SA (2004) Molecular pathways to neurodegeneration. Nat Med 10(Suppl):S2–S9
Chen JJ, Yu BP (1994) Alterations in mitochondrial membrane fluidity by lipid peroxidation products. Free Radic Biol Med 17:411–418
Cho ES, Jang YJ, Kang NJ et al (2009) Cocoa procyanidins attenuate 4-hydroxynonenal-induced apoptosis of PC12 cells by directly inhibiting mitogen-activated protein kinase kinase 4 activity. Free Radic Biol Med 46:1319–1327
Galter D, Buervenich S, Carmine A, Anvret M, Olson L (2003) ALDH1 mRNA: presence in human dopamine neurons and decreases in substantia nigra in Parkinson’s disease and in the ventral tegmental area in schizophrenia. Neurobiol Dis 14:637–647
Jang YJ, Kim JE, Kang NJ, Lee KW, Lee HJ (2009) Piceatannol attenuates 4-hydroxynonenal-induced apoptosis of PC12 cells by blocking activation of c-Jun N-terminal kinase. Ann N Y Acad Sci 1171:176–182
Jang YJ, Kim J, Shim J et al (2011) Kaempferol attenuates 4-hydroxynonenal-induced apoptosis in PC12 cells by directly inhibiting NADPH oxidase. J Pharmacol Exp Ther 337:747–754
Lam JP, Mays DC, Lipsky JJ (1997) Inhibition of recombinant human mitochondrial and cytosolic aldehyde dehydrogenases by two candidates for the active metabolites of disulfiram. Biochemistry 36:13748–13754
Lamensdorf I, Eisenhofer G, Harvey-White J, Hayakawa Y, Kirk K, Kopin IJ (2000a) Metabolic stress in PC12 cells induces the formation of the endogenous dopaminergic neurotoxin, 3,4-dihydroxyphenylacetaldehyde. J Neurosci Res 60:552–558
Lamensdorf I, Eisenhofer G, Harvey-White J, Nechustan A, Kirk K, Kopin IJ (2000b) 3,4-Dihydroxyphenylacetaldehyde potentiates the toxic effects of metabolic stress in PC12 cells. Brain Res 868:191–201
Laplane D, Attal N, Sauron B, de Billy A, Dubois B (1992) Lesions of basal ganglia due to disulfiram neurotoxicity. J Neurol Neurosurg Psychiatry 55:925–929
Legros H, Dingeval MG, Janin F, Costentin J, Bonnet JJ (2004) Toxicity of a treatment associating dopamine and disulfiram for catecholaminergic neuroblastoma SH-SY5Y cells: relationships with 3,4-dihydroxyphenylacetaldehyde formation. Neurotoxicology 25:365–375
Leonarduzzi G, Robbesyn F, Poli G (2004) Signaling kinases modulated by 4-hydroxynonenal. Free Radic Biol Med 37:1694–1702
Mandel S, Grunblatt E, Riederer P et al (2005) Gene expression profiling of sporadic Parkinson’s disease substantia nigra pars compacta reveals impairment of ubiquitin-proteasome subunits, SKP1A, aldehyde dehydrogenase, and chaperone HSC-70. Ann N Y Acad Sci 1053:356–375
Omata Y, Saito Y, Fujita K et al (2008) Induction of adaptive response and enhancement of PC12 cell tolerance by lipopolysaccharide primarily through the upregulation of glutathione S-transferase A3 via Nrf2 activation. Free Radic Biol Med 45:1437–1445
Raza H, John A (2006) 4-Hydroxynonenal induces mitochondrial oxidative stress, apoptosis and expression of glutathione S-transferase A4-4 and cytochrome P450 2E1 in PC12 cells. Toxicol Appl Pharmacol 216:309–318
Ruef J, Rao GN, Li F et al (1998) Induction of rat aortic smooth muscle cell growth by the lipid peroxidation product 4-hydroxy-2-nonenal. Circulation 97:1071–1078
Samii A, Nutt JG, Ransom BR (2004) Parkinson’s disease. Lancet 363:1783–1793
Sayre LM, Zelasko DA, Harris PL, Perry G, Salomon RG, Smith MA (1997) 4-Hydroxynonenal-derived advanced lipid peroxidation end products are increased in Alzheimer’s disease. J Neurochem 68:2092–2097
Schaur RJ (2003) Basic aspects of the biochemical reactivity of 4-hydroxynonenal. Mol Aspects Med 24:149–159
Siems W, Grune T (2003) Intracellular metabolism of 4-hydroxynonenal. Mol Aspects Med 24:167–175
Subramaniam R, Roediger F, Jordan B et al (1997) The lipid peroxidation product, 4-hydroxy-2-trans-nonenal, alters the conformation of cortical synaptosomal membrane proteins. J Neurochem 69:1161–1169
Werner CJ, Heyny-von HR, Mall G, Wolf S (2008) Proteome analysis of human substantia nigra in Parkinson’s disease. Proteome Sci 6:8
Yang Y, Sharma R, Sharma A, Awasthi S, Awasthi YC (2003) Lipid peroxidation and cell cycle signaling: 4-hydroxynonenal, a key molecule in stress mediated signaling. Acta Biochim Pol 50:319–336
Yoritaka A, Hattori N, Uchida K, Tanaka M, Stadtman ER, Mizuno Y (1996) Immunohistochemical detection of 4-hydroxynonenal protein adducts in Parkinson disease. Proc Natl Acad Sci U S A 93:2696–2701
Zhang M, Shoeb M, Goswamy J et al (2010) Overexpression of aldehyde dehydrogenase 1A1 reduces oxidation-induced toxicity in SH-SY5Y neuroblastoma cells. J Neurosci Res 88:686–694
Acknowledgments
The authors wish to thank Drs. Matthew Pando, Florence Mahe, and John Donello for their critical reading of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kong, D., Kotraiah, V. Modulation of Aldehyde Dehydrogenase Activity Affects (±)-4-Hydroxy-2E-nonenal (HNE) Toxicity and HNE–Protein Adduct Levels in PC12 Cells. J Mol Neurosci 47, 595–603 (2012). https://doi.org/10.1007/s12031-011-9688-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-011-9688-y