Abstract
Pituitary adenylate cyclase-activating polypeptide (PACAP) is a neuropeptide originally isolated from ovine hypothalamus. Recently, we have shown that the PACAP receptor (PAC1-R) is expressed in reactive astrocytes following an in vivo stub wound brain injury. However, the functional role of PACAP has not yet been clarified. In order to investigate the effect of PACAP on the proliferation of reactive astrocytes, a scratch wound paradigm was applied to astrocytic monolayers. Following injury, there was an increase in PAC1-R and glial fibrillary acidic protein (GFAP) immunoreactivity in the astrocytes surrounding the scratch line. PACAP at concentrations of 10−15 to 10−7 M was applied immediately after scratching, and the proliferating astrocytes were visualized by multiple immunofluorescence labeling. The percentage of cells that colabeled for Ki67 (a marker of proliferating cells) and GFAP increased in the 10−11- and 10−13-M PACAP-treated groups. The proliferating astrocytes induced by PACAP treatment mainly occurred in the proximal wound area where many reactive astrocytes were observed. Pretreatment with the PACAP receptor antagonist PACAP6-38 significantly suppressed the PACAP-induced effects. These results strongly suggest that PACAP plays an important role in the proliferation of reactive astrocytes following nerve injury.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Astrocytes are a subtype of glial cells found in the brain and spinal cord. Astrocytes have various functions in the intact central nervous system (CNS), including structural support for neural elements, homeostatic maintenance of the extracellular ionic environment and pH, uptake of extracellular glutamate, regulation of energy metabolism, secretion of growth factors and cytokines, and interactions with endothelia to create and maintain the blood–brain barrier (Fields and Stevens-Graham 2002; Ransom et al. 2003; Volterra and Meldolesi 2005). In the injured CNS, reactive astrocytes form dense scar tissue, known as the glial scar, around the lesion site, which serves to compact inflammatory cells and reseal the blood–brain barrier after it has been breached by injury (Fawcett and Asher 1999; Milos and Michael 2005). However, although reactive astrocytes are prominent in the cellular response to nervous tissue injury, their role is not well understood.
Pituitary adenylate cyclase-activating polypeptide (PACAP) is a neuropeptide which was originally isolated from ovine hypothalamus (Miyata et al. 1989). PACAP-containing neurons are mainly found in the hypothalamus, and their fibers are widely distributed throughout the brain (Arimura and Shioda 1995; Shioda 2000; Watanabe et al. 2007). PACAP has a pleiotropic function in the CNS, as a neuroprotectant, neurite outgrowth factor, and inducer of neural stem cell differentiation into astrocytes (Nakamachi et al. 2010; Ohno et al. 2005; Ohtaki et al. 2006, 2008; Shioda et al. 2006; Somogyvari-Vigh and Reglodi 2004; Tamas et al. 2006; Watanabe et al. 2006a, b). PACAP has also been widely reported to act as a regulator of astrocytes in vitro (Gottschall et al. 1994; Tatsuno and Arimura 1994; Tatsuno et al. 1990, 1996). We have previously reported that immunoreactivity for the PACAP receptor, PAC1-receptor (PAC1-R), is observed in reactive astrocytes following a stub wound brain injury in vivo (Suzuki et al. 2003). However, the involvement of PACAP in reactive astrocytosis remains unclear. The aim of this study was therefore to investigate the effect of PACAP on the proliferation of reactive astrocytes induced by an in vitro scratch injury model.
Materials and Methods
Primary Culture of Astrocytes
Cerebral cortices were obtained from newborn ICR mice. The tissues were minced and treated with trypsin (0.025%, Invitrogen, Carlsbad, CA, USA) dissolved in phosphate-buffered saline (PBS) solution containing 0.02% l-cysteine monohydrate (Sigma-Aldrich, St. Louis, MO, USA), 0.5% glucose (Wako Pure Chemicals, Osaka, Japan), and 0.02% bovine serum albumin (Wako Pure Chemicals). After enzyme treatment at 37°C for 15 min, cells were dispersed by gentle agitation through a pipette and plated in a flask. One week after seeding in Dulbecco’s modified Eagle’s medium (DMEM; Invitrogen) supplemented with 10% heat-inactivated newborn calf serum (Invitrogen), 1% glucose, 10 U/mL penicillin, and 10 g/mL streptomycin in a humidified atmosphere of 95% air and 5% CO2 at 37°C, the flask was shaken at 150 rpm for 20 h at 37°C to remove nonastrocytic cells. The remaining cells were then seeded at a density of 105 cells/cm2 and maintained for 5–7 days.
Scratch Wound Model
The scratch wound model was initiated by scratching confluent monolayers in the secondary cultures with the tip of a sterile plastic pipette. Immediately following scratching, the culture medium was replaced with serum-free DMEM containing 1% glucose, 10 U/mL penicillin, 10 g/mL streptomycin, and G-5 supplement (Invitrogen). PACAP38 (Peptide Institute, Osaka, Japan) or the PACAP receptor antagonist PACAP6-38 (Peptide Institute) was also added to the medium at this time. Subsequent morphological changes were observed under a phase-contrast microscope (Eclipse TE2000, Nikon, Tokyo, Japan).
Immunocytochemistry
Cultured cells were washed three times in ice-cold PBS and fixed with 4% paraformaldehyde for 30 min on ice. The cells were pretreated with 0.3% Triton X-100 for 30 min and 5% normal horse serum for 1 h, after which they were incubated in primary antibody: rabbit polyclonal anti-PAC1-R antibody (1:500), mouse monoclonal antiglial fibrillary acidic protein (anti-GFAP) antibody (1:1000; Sigma-Aldrich), mouse monoclonal anti-NeuN antibody (1:1,000; Millipore, Billerica, MA, USA), rabbit polyclonal anti-Iba1 antibody (1:2,000; Wako Pure Chemicals), mouse monoclonal anti-GalC antibody (1:500; Millipore), or monoclonal anti-Ki67 antibody (1:1,000; Novocastra, Newcastle upon Tyne, UK). The rabbit polyclonal anti-PAC1-R antibody was raised by using the N-terminal residue as an antigen and affinity purified (Suzuki et al. 2003). After incubation, the sections were immersed in Alexa Fluor 350-, 488-, and 546-labeled antimouse or antirabbit IgG secondary antibodies (1:400; Invitrogen). At the end of the staining period, the sections were counterstained with DAPI. All of the above procedures were carried out on three to four brains per condition. Sections were observed with the aid of a fluorescence microscope (AXIO Imager Z1, Carl Zeiss, Germany). Cell counts were performed on eight to 12 fields (600,000 μm2 each) per dish, with more than four dishes being evaluated for each group. The percentage of proliferative astrocytes was calculated by determining the number of Ki67 and GFAP double-positive cells as a function of the total number of GFAP-positive cells. The proximal wound area was defined as lying within 500 μm of the scratch line, and the distal wound area was considered to be at least 5,000 μm from the scratch line.
Statistical Analysis
Data were expressed as the mean ± SEM. Multiple comparisons were made by ANOVA with Tukey–Kramer multiple-comparison tests. A P value of less than 0.05 was considered statistically significant for all analyses.
Results
Scratch Wound Model
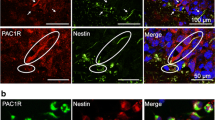
Primary cultures of newborn mouse brain were characterized by immunocytochemistry. The majority of cells (92.7%) were immunopositive for the astrocytic marker GFAP (Fig. 1), with only small numbers of cells being labeled for the oligodendrocyte marker GalC (0.4%), the microglia/macrophage marker Iba-1 (0.2%), or the neuronal marker NeuN (0.1%). The astrocytic monolayer was then scratched and observed for the following 7 days. Cells along the scratch line, which was approximately 200 μm in width, were initially removed by the wound. Three days later, however, astrocytes had begun to cover the injury site, and after 7 days, this process was almost complete (Fig. 2). The PAC1-R and GFAP immunoreactivity of the cultured astrocytes was determined before and after scratching in order to assess PAC1-R expression on both resting and reactive astrocytes. Slight PAC1-R immunoreactivity was observed immediately after the injury. However, 2 days later, there was a marked increase in PAC1-R and GFAP immunoreactivity in the reactive astrocytes along the scratch line (Fig. 3), and many hypertrophic cell processes, which were also double immunopositive for PAC1-R and GFAP, had migrated into the wound area.
Characterization of astrocytic monolayer cultures by immunocytochemistry. Cultured astrocytes were immunostained with antibodies against GFAP, GalC, Iba-1, and NeuN. a Fluorescence micrographs taken after immunostaining with specific cell markers. b Cell counts demonstrating the number of each immunopositive cell type expressed as a function of the total number of DAPI-positive cells
Morphological changes in cultured astrocytes following a scratch wound. a Illustration of the scratch injury created in astrocytic monolayers using the tip of a pipette. The boxed region is shown at higher magnification in b. b Phase-contrast micrographs of the injury site. The time period after scratching is indicated at the upper left of each picture
PAC1-R and GFAP immunoreactivity in scratch-induced reactive astrocytes. Fluorescence micrographs of astrocytes stained with anti-PAC1-R and anti-GFAP antibodies. Pictures were taken with the same exposure time 0 and 2 days after scratching. The dotted white line shows the border between the wound (left) and the astrocyte layer (right)
PACAP Treatment
To evaluate the effect of PACAP on reactive astrocytes induced by scratch injury, the cultures were treated with various concentrations of PACAP (10−7, 10−9, 10−11, 10−13, or 10−15 M). The proliferating astrocytes were visualized by multiple immunofluorescence staining 2 days after PACAP treatment. The percentage of cells in the vehicle-treated control that colabeled for the proliferative marker Ki67 and GFAP was 7.1% at 2 days. This value was significantly higher in the 10−11-M (12.3%) and 10−13-M (11.4%) PACAP-treated groups (Fig. 4b). In the group treated with 10−11 M PACAP, many astrocytic processes were observed migrating toward the injured area (Fig. 4a). However, no significant differences were noted in the groups treated with 10−7, 10−9, or 10−15 M PACAP compared to the control.
Effect of PACAP on the proliferation of scratch-induced reactive astrocytes. Cultured astrocytes were stained with anti-GFAP and anti-KI67 antibodies. a Typical pictures of control or 10−11 M PACAP-treated astrocytes showing GFAP immunoreactivity (green) and Ki67 immunoreactivity (red), as well as DAPI-positive nuclei (blue), 2 days after scratching. b Cell counts of the number of Ki67 and GFAP double-immunopositive cells expressed as a function of the total number of GFAP-immunopositive cells in the proximal injury area. PACAP was added at a final concentration of 10−15, 10−13, 10−11, 10−9, or 10−7 M
In order to evaluate the contribution of the PACAP receptor to the proliferative effect of PACAP, cultures were cotreated with 10−11 M PACAP and the PACAP receptor antagonist, PACAP 6-38. The percentage of Ki67-positive astrocytes was 8.5% in the control and 11.9% in the group treated with PACAP. The latter value significantly decreased to 7.5% in the group cotreated with both PACAP and PACAP 6-38 (Fig. 5). Treatment with PACAP 6-38 alone produced a value of 7.2%.
Effect of PACAP6-38 on the proliferation of reactive astrocytes induced by PACAP. PACAP (10−11 M) and the PACAP receptor antagonist, PACAP6-38 (10−9 M), were added to the astrocyte cultures immediately after scratching. The number of Ki67 and GFAP double-immunopositive cells was expressed as a function of the total number of GFAP-immunopositive cells in the proximal injury area 2 days after scratching
The percentages of Ki67-positive astrocytes within 500 µm of the scratch line (proximal area) in the control (8.5%) and PACAP-treated (11.1%) groups were significantly different (Fig. 6). In the distal area (over 5,000 µm beyond the scratch line), these values were 6.8% and 8.9%, respectively. This result was nonsignificant, although an increase was still observed in the PACAP-treated group.
Effect of PACAP on astrocytes proximal and distal to the wound. The number of Ki67 and GFAP double-immunopositive cells as a function of the number of GFAP-immunopositive cells distal (∼5,000 μm) and proximal (∼500 μm) to the wound site was determined 2 days after injury with or without 10−11 M PACAP treatment
Discussion
Scratch wound models have been used to characterize the astrocytic changes that occur after neural injury (Lanosa and Colombo 2007). To investigate the role of PACAP on proliferation of reactive astrocytes, we first established astrocytic monolayer cultures as previously described (Kato et al. 2006) and confirmed that the rate of contamination with other cell types was less than 1% (Fig. 1). GFAP and PAC1-R immunoreactivity increased in these cultures 2 days after injury (Fig. 3). GFAP is not only well known as a normal astrocytic marker but is also upregulated when these astrocytes become reactive (Lin et al. 1995). Furthermore, we have previously shown that reactive astrocytes induced by stub wound injury are immunoreactive for PAC1-R (Suzuki et al. 2003). These studies support the present findings which demonstrate that scratch injury in astrocytic monolayers induces reactive astrocytes and that PAC1-R is a novel marker for these cells. A number of growth factors and cytokines are also released from reactive astrocytes (Ridet et al. 1997), and it has been reported that PACAP administration induces the expression of neuroprotective proteins, such as ADNF and ADNP (Dejda et al. 2005; Nakamachi et al. 2006; Nakamachi et al. 2008) and cytokines (Gottschall et al. 1994; Tatsuno et al. 1996). Such PACAP-inducible factors could be additional candidates as markers of astrocytic activation.
PACAP at a concentration of 10−11 or 10−13 M significantly increased the number of proliferative astrocytes near the scratch area (Fig. 4). It also tended to increase the number of KI67-positive astrocytes distally as well as proximally (Fig. 6). Hashimoto and colleagues have reported that a 10−12-M concentration of PACAP can induce the proliferation of resting astrocytes via the cAMP pathway (Hashimoto et al. 2003). These results suggest either that PACAP is able to stimulate the proliferation of both resting and reactive astrocytes or that it induces a phenotypic change from quiescence to reactivity. In addition, the present results demonstrate that many astrocytes in the PACAP-treated groups extended processes toward the injury area (Fig. 5). It has previously been reported that PACAP stimulates the dose-dependent extension of projections from resting astrocytes derived from the rat hypothalamus (Ikeda et al. 2003), although how this occurs remains unclear. Moreover, astrocytes close to a wound display increased migratory potential and move toward the injury site to initiate repair (Kornyei et al. 2000). Further studies are required to fully elucidate the role of PACAP in the functional behavior of astrocytes and to characterize the underlying mechanism.
PACAP and vasoactive intestinal polypeptide (VIP) share three receptors: PAC1-R and the VPAC1 and VPAC2 receptors (VPAC1-R, VPAC2-R). The affinity of PAC1-R for PACAP is more than 1,000 times higher than its affinity for VIP, indicating that PAC1-R is a relatively specific receptor for PACAP (Arimura 1998). During the embryonic period, astrocytes express all three types of PACAP receptor, but by 0–7 days after birth, VPAC2-R and PAC1-R are the dominant astrocytic forms (Jaworski 2000), with PAC1-R and VPAC2-R expression also being shown to increase in the injured mouse brain (Furuta et al. 2007; Suzuki et al. 2003). In the present study, cotreatment with PACAP and PACAP6-38, an antagonist of the PAC1 and VPAC2 receptors (Gourlet et al. 1995), suppressed the PACAP-induced proliferation of reactive astrocytes (Fig. 6). This suggests that PACAP induces the proliferation of reactive astrocytes via PAC1-R or VPAC2-R. Further studies focusing on the contribution of these receptors to the PACAP-induced proliferation of reactive astrocytes is therefore warranted.
When the mammalian CNS is damaged, astrocytes undergo an injury response and become reactive, leading eventually to the formation of a dense glial scar network at the lesion site (Fawcett and Asher 1999). The glial scar not only serves to compact the injury site but also inhibits axonal regeneration through regions of scar formation. We conclude that PACAP plays an important role in the proliferation of reactive astrocytes after nerve injury, suggesting that it is associated with the glial scar formation that produces a barrier to axonal regeneration. Elucidating the underlying molecular mechanisms of these effects therefore has major implications for our understanding of functional brain recovery following trauma, ischemia, and neurodegenerative disease.
References
Arimura A (1998) Perspectives on pituitary adenylate cyclase activating polypeptide (PACAP) in the neuroendocrine, endocrine, and nervous systems. Jpn J Physiol 48(5):301–331
Arimura A, Shioda S (1995) Pituitary adenylate cyclase activating polypeptide (PACAP) and its receptors: neuroendocrine and endocrine interaction. Front Neuroendocrinol 16(1):53–88
Dejda A, Sokolowska P, Nowak JZ (2005) Neuroprotective potential of three neuropeptides PACAP, VIP and PHI. Pharmacol Rep 57(3):307–320
Fawcett JW, Asher RA (1999) The glial scar and central nervous system repair. Brain Res Bull 49(6):377
Fields RD, Stevens-Graham B (2002) NEUROSCIENCE: new insights into neuron–glia communication. Science 298(5593):556–562
Furuta A, Wada E, Wada K (2007) Function of glial G-protein coupled receptors. Brain Nerve 59(7):717–724
Gottschall PE, Tatsuno I, Arimura A (1994) Regulation of interleukin-6 (IL-6) secretion in primary cultured rat astrocytes: synergism of interleukin-1 (IL-1) and pituitary adenylate cyclase activating polypeptide (PACAP). Brain Res 637(1–2):197–203
Gourlet P, Vandermeers A, Vandermeers-Piret M-C, Rath J, De Neef P, Robberecht P (1995) Fragments of pituitary adenylate cyclase activating polypeptide discriminate between type I and II recombinant receptors. Eur J Pharmacol 287(1):7
Hashimoto H, Kunugi A, Arakawa N et al (2003) Possible involvement of a cyclic AMP-dependent mechanism in PACAP-induced proliferation and ERK activation in astrocytes. Biochem Biophys Res Commun 311(2):337–343
Ikeda T, Iijima N, Munekawa K, Ishihara A, Ibata Y, Tanaka M (2003) Functional retinal input stimulates expression of astroglial elements in the suprachiasmatic nucleus of postnatal developing rat. Neurosci Res 47(1):39–45
Jaworski DM (2000) Expression of pituitary adenylate cyclase-activating polypeptide (PACAP) and the PACAP-selective receptor in cultured rat astrocytes, human brain tumors, and in response to acute intracranial injury. Cell Tissue Res 300(2):219–230
Kato H, Narita M, Miyatake M, Yajima Y, Suzuki T (2006) Role of neuronal NR2B subunit-containing NMDA receptor-mediated Ca2+ influx and astrocytic activation in cultured mouse cortical neurons and astrocytes. Synapse 59(1):10–17
Kornyei Z, Czirok A, Vicsek T, Madarasz E (2000) Proliferative and migratory responses of astrocytes to in vitro injury. J Neurosci Res 61(4):421–429
Lanosa XA, Colombo JA (2007) Astroglial injury in an ex vivo model: contributions to its analysis in enriched cell cultures. In Vitro Cell Dev Biol Anim 43(5–6):186–195
Lin RCS, Matesic DF, Marvin M, McKay RDG, Brüstle O (1995) Re-expression of the intermediate filament nestin in reactive astrocytes. Neurobiol Dis 2(2):79
Milos P, Michael N (2005) Astrocyte activation and reactive gliosis. Glia 50(4):427–434
Miyata A, Arimura A, Dahl RR et al (1989) Isolation of a novel 38 residue-hypothalamic polypeptide which stimulates adenylate cyclase in pituitary cells. Biochem Biophys Res Commun 164(1):567–574
Nakamachi T, Li M, Shioda S, Arimura A (2006) Signaling involved in pituitary adenylate cyclase-activating polypeptide-stimulated ADNP expression. Peptides 27(7):1859–1864
Nakamachi T, Ohtaki H, Yofu S et al (2008) Pituitary adenylate cyclase-activating polypeptide (PACAP) type 1 receptor (PAC1R) co-localizes with activity-dependent neuroprotective protein (ADNP) in the mouse brains. Regul Pept 145(1–3):88–95
Nakamachi T, Ohtaki H, Yofu S et al (2010) Endogenous pituitary adenylate cyclase activating polypeptide is involved in suppression of edema in the ischemic brain. Acta Neurochir Suppl 106:43–46
Ohno F, Watanabe J, Sekihara H et al (2005) Pituitary adenylate cyclase-activating polypeptide promotes differentiation of mouse neural stem cells into astrocytes. Regul Pept 126(1–2):115–122
Ohtaki H, Nakamachi T, Dohi K et al (2006) Pituitary adenylate cyclase-activating polypeptide (PACAP) decreases ischemic neuronal cell death in association with IL-6. Proc Natl Acad Sci USA 103(19):7488–7493
Ohtaki H, Nakamachi T, Dohi K, Shioda S (2008) Role of PACAP in ischemic neural death. J Mol Neurosci 36(1–3):16–25
Ransom B, Behar T, Nedergaard M (2003) New roles for astrocytes (stars at last). Trends Neurosci 26(10):520
Ridet JL, Malhotra SK, Privat A, Gage FH (1997) Reactive astrocytes: cellular and molecular cues to biological function. Trends Neurosci 20(12):570–577
Shioda S (2000) Pituitary adenylate cyclase-activating polypeptide (PACAP) and its receptors in the brain. Kaibogaku Zasshi 75(6):487–507
Shioda S, Ohtaki H, Nakamachi T et al (2006) Pleiotropic functions of PACAP in the CNS: neuroprotection and neurodevelopment. Ann NY Acad Sci 1070:550–560
Somogyvari-Vigh A, Reglodi D (2004) Pituitary adenylate cyclase activating polypeptide: a potential neuroprotective peptide. Curr Pharm Des 10(23):2861–2889
Suzuki R, Arata S, Nakajo S, Ikenaka K, Kikuyama S, Shioda S (2003) Expression of the receptor for pituitary adenylate cyclase-activating polypeptide (PAC1-R) in reactive astrocytes. Brain Res Mol Brain Res 115(1):10–20
Tamas A, Zsombok A, Farkas O et al (2006) Postinjury administration of pituitary adenylate cyclase activating polypeptide (PACAP) attenuates traumatically induced axonal injury in rats. J Neurotrauma 23(5):686–695
Tatsuno I, Arimura A (1994) Pituitary adenylate cyclase-activating polypeptide (PACAP) mobilizes intracellular free calcium in cultured rat type-2, but not type-1, astrocytes. Brain Res 662(1–2):1–10
Tatsuno I, Gottschall PE, Koves K, Arimura A (1990) Demonstration of specific binding sites for pituitary adenylate cyclase activating polypeptide (PACAP) in rat astrocytes. Biochem Biophys Res Commun 168(3):1027–1033
Tatsuno I, Morio H, Tanaka T et al (1996) Pituitary adenylate cyclase-activating polypeptide (PACAP) is a regulator of astrocytes: PACAP stimulates proliferation and production of interleukin 6 (IL-6), but not nerve growth factor (NGF), in cultured rat astrocyte. Ann NY Acad Sci 805:482–488
Volterra A, Meldolesi J (2005) Astrocytes, from brain glue to communication elements: the revolution continues. Nat Rev Neurosci 6(8):626
Watanabe J, Nakamachi T, Matsuno R et al (2007) Localization, characterization and function of pituitary adenylate cyclase-activating polypeptide during brain development. Peptides 28(9):1713–1719
Watanabe J, Ohba M, Ohno F et al (2006a) Pituitary adenylate cyclase-activating polypeptide-induced differentiation of embryonic neural stem cells into astrocytes is mediated via the beta isoform of protein kinase C. J Neurosci Res 84(8):1645–1655
Watanabe J, Ohno F, Shioda S, Kikuyama S, Nakaya K, Nakajo S (2006b) Involvement of protein kinase C in the PACAP-induced differentiation of neural stem cells into astrocytes. Ann NY Acad Sci 1070:597–601
Acknowledgment
This work was supported in part by a Showa University Grant-in Aid for Innovative Collaborative Research Projects (S.S) and by a grant from Japan's Ministry of Education, Science, Sports and Culture (T.N, S.S) and Research on Health Sciences focusing on Drug Innovation from The Japan Health Sciences Foundation (S.S).
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the Yakushima2009 Symposium
Rights and permissions
About this article
Cite this article
Nakamachi, T., Nakamura, K., Oshida, K. et al. Pituitary Adenylate Cyclase-Activating Polypeptide (PACAP) Stimulates Proliferation of Reactive Astrocytes In Vitro. J Mol Neurosci 43, 16–21 (2011). https://doi.org/10.1007/s12031-010-9404-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12031-010-9404-3