Abstract
Silver nanoparticles, which are being used increasingly as antimicrobial agents, may extend its antibacterial application to methicillin-resistant Staphylococcus aureus (MRSA), the main cause of nosocomial infections worldwide. To explore the antibacterial properties of silver nanoparticles against MRSA, the present work includes an analysis of the relation between nanosilver effect and MRSA’s resistance mechanisms, a study of the size dependence of the bactericidal activity of nanosilver and a toxicity assessment of nanoparticles against epithelial human cells. Minimum inhibitory concentration (MIC), minimum bactericidal concentration (MBC), and MBC/MIC ratio of silver nanoparticles were quantified by using a luciferase-based assay. The cytotoxic effect (CC50 and CC90) of three different nanosilver sizes (10, 30–40, and 100 nm) were assessed in HeLa cells by a similar method. The therapeutic index was used as an indicator of nanosilver overall efficacy and safety. Silver nanoparticles inhibited bacterial growth of both MRSA and non-MR S. aureus in a bactericidal rather than a bacteriostatic manner (MBC/MIC ratio ≤ 4). Silver nanoparticle’s therapeutic index varied when nanoparticle’s size diminished. At the same dose range, 10 nm nanoparticles were the most effective since they did not affect HeLa’s cell viability while inhibiting a considerable percentage of MRSA growth. Silver nanoparticles are effective bactericidal agents that are not affected by drug-resistant mechanisms of MRSA. Nanosilver size mediates MRSA inhibition and the cytotoxicity to human cells, being smaller nanoparticles the ones with a better antibacterial activity and nontoxic effect.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Methicillin resistant Staphylococcus aureus (MRSA) is an important pathogen in the healthcare sector that has not been eliminated from the hospital nor community environment. In humans, S. aureus causes superficial lesions in the skin and localized abscesses, central nervous system infections, osteomyelitis, invasive endocarditis, septic arthritis, septicemia, pneumonia, and urinary tract infections [1]. A bacteremia caused by S. aureus produces between 25% and 63% of mortality [2].
In 1960, the first strain of MRSA was isolated in the UK, just 1 year after methicillin started to be used as an alternative to penicillin. Nowadays, MRSA strains have a wide range of drug resistances, including to more than 16 types of antibiotics. Resistance to methicillin is related to the gen mecA, which codifies the protein PBP2a that has low affinity to methicillin and to all β-lactamics [2].
MRSA’s medical importance is attributed to the high mortality and morbidity rate of its infections and for being the main cause of nosocomial infections worldwide [2]. According to the World Health Organization, in some Asian countries, the incidence of MRSA has reached 70% to 80% of all the S. aureus isolates [3]. The National Nosocomial Infectious Surveillance System determined that in hospitalized patients, the prevalence of MRSA strains raised from 4% in 1980 to 60.7% in 2004 in the USA [2]. The Centers for Disease Control estimated for 2005 that invasive MRSA caused 94,360 infections and 18,650 associated deaths. Of these infections, about 86% are healthcare-associated and 14% are community-associated [4].
Investigations focused in the search of other alternatives for the treatment of MRSA infections are continuously being held. Among the range of compounds whose bactericidal activity is being investigated, silver nanoparticles rise as a promising new antibacterial agent that could be helpful to confront this and other drug-resistant bacteria.
Antibacterial properties of silver are documented since 1000 B.C., when silver vessels were used to preserve water. The first scientific papers describing the medical use of silver report the prevention of eye infection in neonates in 1881 and internal antisepsis in 1901. After this, silver nitrate and silver sulfadiazine have been widely used for the treatment of superficial and deep dermal burns of wounds and for the removal of warts [5]. Silver’s mode of action is presumed to be dependent on Ag+ ions, which strongly inhibit bacterial growth through suppression of respiratory enzymes and electron transport components and through interference with DNA functions [6].
Silver in a nanometric scale (less than 100 nm) has different catalytical properties compared with those attributed to the bulk form of the noble metal, like surface Plasmon resonance, large effective scattering cross section of individual silver nanoparticles, and strong toxicity to a wide range of microorganisms [7].
Different studies have established the bactericidal effect of nanosilver in Gram negative and Gram positive bacteria, but the bactericidal mechanism of this compound has not been clearly elucidated. Morones et al. [8] defined the antibacterial activity of silver nanoparticles in four types of Gram negative bacteria: Escherichia coli, Vibrio cholera, Pseudomonas aeruginosa, and Salmonella tiphy and suggested that silver nanoparticles attach to the surface of the cell membrane and disturb its function, penetrate bacteria, and release silver ions [9]. Other groups determined a similar antibacterial activity in Gram positive bacteria, such as Bacillus subtilis [8], S. aureus [10], and Enterococcus faecalis [11]. Silver nanoparticles have also been found to exert antibacterial activity against some drug-resistant bacteria [12, 13].
Furthermore, the antiviral capability of silver nanoparticles against the human immunodeficiency virus type 1 [7] and hepatitis B virus [14] has been established. Current applications of silver nanoparticles include antimicrobial bandages for burns [15], water filters [16], and others.
Toxicity of silver nanoparticles has been studied in different mammalian cell systems, including rat liver cells [17], human keratinocytes and fibroblasts cultures [18], and human spermatogonial stem cells [19]. In vitro, an elevated dose of nanosilver induces oxidative stress (liberation of reactive oxygen species) as a mechanism of cytotoxicity [20]. But, what happens at nanosilver concentrations that are nontoxic? Can they be used for a therapeutic purpose? At an innocuous concentration range, silver nanoparticles have been described to exert anti-inflammatory effects as: acceleration of wound healing [21], modulation of cytokine production and induction of peripheral blood mononuclear cells proliferation [22], inhibition of allergic contact dermatitis in mice, suppression of the expression of TNF-α and IL-12, and induction of apoptosis of inflammatory cells [23].
In this research, a comparison of nanosilver’s efficacy and safety was determined by analyzing, for the first time, the antibacterial potency of noncytotoxic nanosilver concentrations against MRSA. We report the effect of three nanoparticle sizes (10, 30–40, and 100 nm) against MRSA and HeLa cells. We explored (1) if the mechanisms that give MRSA its drug-resistance status influence its response to silver nanoparticles, (2) the MRSA size-dependent response to nanosilver, and (3) nanosilver toxicity to human cells at concentrations defined as antibacterial.
Materials and Methods
Silver Nanoparticles Formulation
Silver nanoparticles of ∼100 nm were obtained from Sigma–Aldrich (No. 576832, Sigma Aldrich, St. Louis, MO, USA) and 10 and 30–40 nm from Nanoamor (Stock No. 0478YD and 0477YD, Houston, TX, USA) in powder presentation. A solution was prepared in RPMI-1640 (No. R8758, Sigma Aldrich, St. Louis, MO, USA) culture media enriched with 10% fetal calf serum (FCS) and following dilutions were made in culture media.
Bacterial Strains
MRSA was obtained from the Department of Infectology of the University Hospital of the UANL, Monterrey, Mexico. The nonmethicillin-resistant (non-MR) S. aureus was obtained from the Microbiology and Immunology Department of the Biological Sciences Faculty of the UANL. Bacteria were cultured at 35ºC in Mueller Hinton agar (Code 211667, BD Bioxon, Mexico).
MRSA was typed with the latex agglutination assay Slidex MRSA Detection (No. 73117, Biomerieux, Marcy l'Etoile, France) and by using a cefoxitin disk [24]. Besides, a resistance profile was determined for both strains using the Kirby–Bauer test with multidisc (Bio-Rad, DF, Mexico) and NCCLS parameters.
MIC and MBC Determination
The minimal inhibitory concentration (MIC) and the minimal bactericidal concentration (MBC) were determined by a microdilution method, using LB broth (Sigma–Aldrich) and final inocula of 105 and 106 CFU/ml. Bacteria were incubated with serial twofold dilutions of silver nanoparticles, and the effect on cell viability was measured after a 24-h period of incubation. The MIC99 and MIC90 value corresponded to the doses that inhibited 99% and 90% of bacterial growth and, the MBC value, to the silver nanoparticles doses where 100% of the bacterial growth was inhibited compared with the positive control (no treatment).
Bacterial cell viability was measured with the BacTiter-Glo™ Microbial Cell Viability Assay (Cat. G8230, Promega, Madison, WI, USA), a luciferase based assay that quantifies ATP produced by metabolically active cells. Light generated during the process was registered in a Veritas Microplate Luminometer from Turner Biosystems (Model 9100-002).
MBC was also done by using a colony-forming capacity assay in blood agar [25]. All the assays were run in parallel with a negative and a positive control.
The experimental process was done at the Biosafety Laboratory Level 3 (BSL-3) of the Immunology and Virology Laboratory of the UANL, Mexico.
HeLa Cells Cytotoxicity Assay
HeLa-CD4-LTR-β-gal cells (human epithelial cells) were obtained from the AIDS Research and Reference Reagent Program, Division of AIDS, NIAID, NIH from Dr. Michael Emerman. HeLa-CD4-LTR-β-gal were cultured in Dulbecco's Modified Eagle Medium (DMEM) (1×) liquid without sodium phosphate and sodium pyruvate. The medium contained 4,500 mg/L d-glucose and l-glutamine (Sigma–Aldrich), with 10% FCS and 0.2 mg/ml geneticin (G418).
The 50% cytotoxic concentration (CC50) and the 90% cytotoxic concentration (CC90) were determined by a microdilution method, using DMEM culture media and 5 × 104 HeLa-CD4-LTR-β-gal cells/well.
A stock solution of the silver nanoparticles was twofold diluted to desired concentrations in growth medium and subsequently added into 96-plate wells with HeLa-CD4-LTR-β-gal cells. Microtitre plates were incubated at 37°C in a 5% CO2 air-humidified atmosphere for further 2 days. All the assays were run in parallel with a negative and a positive control. Assessments of the cell viability were carried out by using a CellTiter-Glo® Luminescent Cell Viability Assay (Promega). A Veritas Microplate Luminometer from Turner Biosystems was used. Cytotoxicity was evaluated based on the percentage cell survival in a dose-dependent manner relative to the positive control. The CC90 and CC50 value corresponded to the cytotoxic concentration that inhibited 90% and 50% of cellular viability compared with the positive control (no treatment).
Statistical Analysis
MIC and MBC results were expressed as the mean ± the standard error of the mean. A Student t test was used to compare these results. P values lower than 0.05 were considered significant.
Results
Resistance Profile
The presence of PBP2a protein was confirmed by a latex agglutination assay in the MRSA strain and in the non-MR S. aureus was not found. Besides, the MRSA isolate differed from non-MR S. aureus in its response to cefuroxime, gentamicin, pefloxacine, trimethoprim–sulfamethoxazole, and vancomycin (Table 1). According to the Kirby Bauer test, this MRSA strain could be a vancomycin-intermediate S. aureus, but further assays should be done to establish this status.
Bactericidal Activity of Silver Nanoparticles Against MRSA and non-MR S. aureus
MRSA and a non-MR S. aureus isolate were challenged with twofold 100 nm nanosilver serial dilutions for 24 h. Silver nanoparticles affected bacterial cellular viability in a dose-dependent manner. Both MRSA (Fig. 1a) and non-MR S. aureus (Fig. 1b) were inhibited at concentrations over 1.35 mg/ml for the 105-CFU/ml inoculum and over 2.7 mg/ml for the 106-CFU/ml inoculum. As expected, the antibacterial effect of 100 nm nanosilver was inversely related to the amount of bacteria, since the best performance was achieved at 105 CFU/ml than 106 CFU/ml, even though the latter is 1,000 times higher than the standard for susceptibility tests. Performance was defined as the capacity to inhibit bacterial growth under these conditions.
Silver nanoparticles inhibition of bacterial growth (MIC) of MRSA and non-MR S. aureus. a 105 CFU/ml and b 106 CFU/ml of MRSA and non-MR S. aureus were challenged against serial twofold dilutions of 100 nm nanosilver. After a 24-h incubation period cell viability was assessed with a luciferase-based assay and the MIC was defined. The assay was performed in triplicate; the error bars indicate the SEM.
The bactericidal effect of 100 nm nanosilver was also assessed by a colony-forming capacity assay (Fig. 2). The value defined as MBC was the nanosilver concentration that completely inhibited visible colony growth in the blood agar. The MBC values obtained by the colony-forming capacity method were smaller than those obtained by the luciferase-based assay for the 106 CFU/ml. This difference can be attributed to bacteria that are not visible in the agar plate but are still alive and have lost its growth capacity for the nanosilver exposure. The luciferase method quantifies ATP produced during metabolic activity, making it a more sensitive method. MBC results from the luciferase-based assay were the ones used to obtain the MBC/MIC ratio.
Bactericidal effect (MBC) of silver nanoparticles against MRSA and non-MR S. aureus. A colony-forming capacity assay was used to define the MBC of silver nanoparticles against MRSA (a, b) and non-MR S. aureus (c, d). After a 24-h challenge with serial twofold dilutions of 100 nm nanosilver, bacteria were grown in blood agar, and colony growth was recorded after 24 h of incubation. PC positive control, NC negative control.
MRSA and HeLa Cells: Size Matters
Silver nanoparticles of 100, 30–40, and 10 nm were assayed do determine their antibacterial properties against MRSA and cytotoxic effect against HeLa cells. Smaller nanosilver sizes were chosen because the decrease in volume will increase surface area and antibacterial activity.
The three nanosilver sizes exerted a bactericidal rather than a bacteriostatic effect, since MBC/MIC ratio values were lower than 4 (Table 2). However, each size had a distinct behavior against MRSA. Silver nanoparticles of 100 nm were the least effective against this bacteria, because a larger dose is needed to reach a bactericidal effect (MBC) compared to the dose needed to inhibit 99% of the population (MIC99). Furthermore, the comparison among the CC50’s reflects that 100 nm nanosilver particles were the most cytotoxic to HeLa epithelial cells.
The therapeutic index (TI) relates nanosilver therapeutic effect (antibacterial concentrations, MIC90) to its toxic effect (cytotoxic concentrations, CC90). A high therapeutic index, used as an indicator of overall nanosilver efficacy, corresponds to a situation in which one would need nontoxic concentrations of nanoparticles to inhibit MRSA growth. As seen in Table 2, TI is inversely proportional to silver nanoparticles size: the smaller ones (10 nm) were the most effective considering its anti-MRSA activity and noncytotoxic effect.
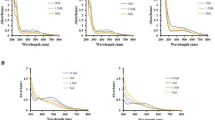
A direct comparison of the three nanosilver sizes under the same dose range (Fig. 3) showed that size does matter. Nanosilver of 100 nm did not inhibit MRSA at doses that did not affect HeLa cell viability (≤0.34 mg/ml); besides, antibacterial doses were cytotoxic (Fig. 3a). Noncytotoxic concentrations of 30–40 nm nanosilver (≤0.67 mg/ml) interfered with a ∼30% of MRSA growth, and mild cytotoxic concentrations (1.35 mg/ml) inhibited ∼50% (Fig. 3b). Finally, 10 nm silver nanoparticles effectively inhibited MRSA growth and kept HeLa cells viable at the same dose range (Fig. 3c). For example, at a 1.35-mg/ml dose, MRSA is almost eliminated without affecting HeLa cells viability.
Toxicity assessment of silver nanoparticles compared with MRSA growth inhibition activity. MRSA (106 CFU/ml) and HeLa cells (5 × 104 cells/well) were challenged with twofold serial dilutions of 100 nm (a), 30–40 nm (b), and 10 nm (c) silver nanoparticles. Cell viability assessment of both bacteria and human cells was done with a luciferase-based assay 24 h after nanosilver exposure. Percentage values are relative to the positive control (no treatment). The assay was performed in triplicate; the error bars indicate the SEM.
Discussion
A wide variety of synthetic compounds exert antibacterial effect, but just some of them can be used as biocides to develop drugs or coatings. The primary impediment for their use is their toxicity compared with their bactericidal effect; some of them are so toxic for eukaryotic cells that cannot be proposed as antibiotics. Among these materials, silver compounds (salts and colloids) raise as potent bactericidal agents whose application is restricted to topical creams used to reduce the risk of wound infection and to treat infected wounds. In order to challenge silver nanoparticles as novel antimicrobial agents, the principal aim of this research was to assess, by in vitro assays, the bactericidal properties of silver nanoparticles against a clinical isolate of MRSA. These bacteria were chosen because of its importance in the hospital environment and its growing appearance in the community.
The MBC/MIC ratio is a parameter that reflects the bactericidal capacity of a compound by relating both values. A ratio with a value superior to 1 (MBC>>MIC) indicates that a great amount of compound is needed to reach the bactericidal effect and that this compound could be considered a bacteriostatic agent. Besides, the MBC/MIC ratio can reflect if the bacteria are susceptible, tolerant, or resistant to the agent that is being challenged. The results show that silver nanoparticles inhibited bacterial growth of both MRSA and non-MR S. aureus in a bactericidal rather than a bacteriostatic manner (MBC/MIC ratio ≤4).
There was no significant difference between the effect of silver nanoparticles on MRSA and non-MR S. aureus, demonstrating that nanosilver activity was not affected by those resistant mechanisms that differentiate these strains. As seen in Table 1, MRSA expresses several resistant mechanisms that are not present in the non-MR S. aureus, including (1) the PBP2a protein for β-lactamic resistance, (2) the acetyltransferase and phosphotransferase for aminoglycoside resistance, (3) a mutated girase subunit A and topoisomerase IV for quinolone resistance, (4) reduced affinity in dihydrofolate reductase for trimethoprim-sulfamethoxazole resistance [2], and (5) abnormal thickened cell walls for vancomycin resistance [26]. PBP2a protein, for example, has low affinity for β-lactam antibiotics and, therefore, is capable of substituting the biosynthetic functions of the normal PBPs even in the presence of the β-lactams, thereby preventing cell lysis [26]. Apparently, silver nanoparticles do not act by directly inhibiting the expression or the activity of the PBP2a protein, since both drug-resistant and susceptible strains were inhibited in the same manner. Therefore, it can be said that silver nanoparticles are broad spectrum agents whose performance is not blocked by the drug-resistant mechanisms mentioned above.
These data also indicates that silver nanoparticles’ mode of action is not the same as the mode of action exerted by the mentioned antibiotics (β-lactamics, quinolones, aminoglycosides, trimethoprim-sulfamethoxazole, and vancomycin). Silver ions are known to bind to sulfhydryl groups, which lead to protein denaturation by the reduction of disulfide bonds (S–S → S–H + H–S) [27]. Besides, silver ions can complex with electron donor groups containing sulfur, oxygen, or nitrogen that are normally present as thiols or phosphates on amino acids and nucleic acids [28]. Thus, silver nanoparticles would not bind to specific proteins or structures of the bacterial cell of both MRSA and non-MR S. aureus but to a broad spectrum of targets that would include membrane and cytoplasmic proteins and genomic or plasmid DNA. Indeed, silver nanoparticles have been found to attach to the surface of the cell membrane and disturb its function, penetrate bacteria, and release silver ions [29]. Sondi et al. and Lok et al. also found that nano-Ag target the bacterial membrane, leading to a dissipation of the proton motive force [29, 30].
The TI was used as an indicator of silver nanoparticles overall efficacy and safety. A high therapeutic index is preferable since it corresponds to a situation in which a lower dose of silver nanoparticles is needed elicit the therapeutic effect (measured as the antibacterial activity) than the one needed to reach the toxic threshold for human cells. After evaluating silver nanoparticles of 100, 30–40, and 10 nm, it was observed that the TI improved when nanoparticle’s size diminished. At 0.67 mg/ml (Fig. 3), 100 nm particles were toxic for both MRSA and HeLa cells, 30–40 nm particles kept HeLa alive but partially inhibited MRSA, and 10 nm nanoparticles did not affect HeLa’s cell viability while inhibiting a considerable percentage of MRSA growth.
Discoveries in the past have demonstrated that physicochemical properties of noble metal nanocrystals are influenced by size [31]. Other researches also defined that the bactericidal and antiviral properties of silver nanoparticles are size dependent and that the only nanoparticles that present a direct interaction with the bacteria or virus preferentially have a diameter of ∼1–10 nm [7, 9]. A smaller size implies the ability to reach structures that otherwise is not available for bigger nanoparticles.
But, why do 10-nm silver nanoparticles eliminate bacteria while keeping human cells alive? As mentioned before, silver compounds are not specific and have several targets that can be present in both eukaryotic and bacterial cells. However, bacteria have a larger surface area-to-volume ratio than eukaryotic cells, which allows for rapid uptake and intracellular distribution of nutrients and excretion of wastes. This characteristic is achieved by having a rigid cell wall composed of peptidoglycan [32]. For that reason, at the same concentration, silver nanoparticles would be preferentially absorbed and accumulated by bacteria, thus exerting its antibacterial effect without significantly damaging human cells. In addition, as mentioned before, silver nanoparticles have been found to bound and disturb bacterial cell membrane activity [30]. Considering that the bacterial plasma membrane is the site of active transport, respiratory chain components, energy-transducing systems, membrane stages in the biosynthesis of phospholipids, peptidoglycan, LPS and capsular polysaccharides, and the anchoring for DNA [33], an alteration of the membrane’s integrity would have a great impact in bacterial growth.
From these studies, it can be concluded that silver-based nanoparticles of approximately 10 nm inhibit MRSA growth in vitro at noncytotoxic concentrations, supporting their potential use as antibacterial agents with a wide number of biomedical and therapeutic applications. Since drug resistance does not interfere with the bactericidal effect of nanosilver, they may prove useful in manufacturing pharmaceutical products and medical devices that may help to prevent the transmission of drug-resistant pathogens, but toxicological limitations for eukaryotic cells should be taken in account since nanosilver is not a target-specific antibacterial agent.
The data presented here are novel in that they prove that silver nanoparticles are effective bactericidal agents against MRSA regardless of the resistance mechanisms that confer importance to these bacteria as an emergent pathogen. Besides, it is the first time that the efficacy and safety of nanosilver in different sizes is determined for MRSA and human cells in vitro.
References
Velazquez-Meza ME. [Staphylococcus aureus methicillin-resistant: emergence and dissemination]. Salud Publica Mex. 2005;47:381–7.
Bustos-Martinez JA, Hamdan-Partida A, Gutierrez-Cardenas M. Staphylococcus aureus: la reemergencia de un patógeno en la comunidad. Rev Biomed. 2006;17:287–305.
World Health Organization. Monitoring of Antimicrobial Resistance. Report of an Intercountry Workshop; 2003 Oct 14–17; Tamil Nadu, India. 2004.
Klevens RM, Morrison MA, Nadle J, Petit S, Gershman K, Ray S, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298:1763–71.
Rai M, Yadav A, Gade A. Silver nanoparticles as a new generation of antimicrobials. Biotechnol Adv. 2009;27:76–83.
Li Y, Leung P, Yao L, Song QW, Newton E. Antimicrobial effect of surgical masks coated with nanoparticles. J Hosp Infect. 2006;62:58–63.
Elechiguerra JL, Burt JL, Morones JR, Camacho-Bragado A, Gao X, Lara HH, et al. Interaction of silver nanoparticles with HIV-1. J Nanobiotechnology. 2005;3:6.
Yoon KY, Byeon JH, Park JH, Ji JH, Bae GN, Hwang J. Antimicrobial Characteristics of Silver Aerosol Nanoparticles against Bacillus subtilis Bioaerosols. Environ Eng Sci. 2008;25:289–93.
Morones JR, Elechiguerra JL, Camacho A, Holt K, Kouri JB, Tapia J, et al. The bactericidal effect of silver nanoparticles. Nanotechnology. 2005;16:2346–53.
Shrivastava S, Bera T, Roy A, Singh G, Ramachandrarao P, Dash D. Characterization of enhanced antibacterial effects of novel silver nanoparticles. Nanotechnology. 2007;18:1–9.
Panacek A, Kvitek L, Prucek R, Kolar M, Vecerova R, Pizurova N, et al. Silver colloid nanoparticles: synthesis, characterization, and their antibacterial activity. J Phys Chem B. 2006;110:16248–53.
Birla SS, Tiwari VV, Gade AK, Ingle AP, Yadav AP, Rai MK. Fabrication of silver nanoparticles by Phoma glomerata and its combined effect against Escherichia coli, Pseudomonas aeruginosa and Staphylococcus aureus. Lett Appl Microbiol. 2009;48:173–9.
Inoue Y, Uota M, Torikai T, Watari T, Noda I, Hotokebuchi T, et al. Antibacterial properties of nanostructured silver titanate thin films formed on a titanium plate. J Biomed Mater Res A. 2009.
Lut L, Sun RW, Chen R, Hui CK, Ho CM, Luk JM, et al. Silver nanoparticles inhibit hepatitis B virus replication. Antivir Ther. 2008;13:253–62.
Tredget EE, Shankowsky HA, Groeneveld A, Burrell R. A matched-pair, randomized study evaluating the efficacy and safety of Acticoat silver-coated dressing for the treatment of burn wounds. J Burn Care Rehabil. 1998;19:531–7.
Jain P, Pradeep T. Potential of silver nanoparticle-coated polyurethane foam as an antibacterial water filter. Biotechnol Bioeng. 2005;90:59–63.
Hussain SM, Hess KL, Gearhart JM, Geiss KT, Schlager JJ. In vitro toxicity of nanoparticles in BRL 3A rat liver cells. Toxicol In Vitro. 2005;19:975–83.
Burd A, Kwok CH, Hung SC, Chan HS, Gu H, Lam WK, et al. A comparative study of the cytotoxicity of silver-based dressings in monolayer cell, tissue explant, and animal models. Wound Repair Regen. 2007;15:94–104.
Braydich-Stolle L, Hussain S, Schlager JJ, Hofmann MC. In vitro cytotoxicity of nanoparticles in mammalian germline stem cells. Toxicol Sci. 2005;88:412–9.
Arora S, Jain J, Rajwade JM, Paknikar KM. Cellular responses induced by silver nanoparticles: In vitro studies. Toxicol Lett. 2008;179:93–100.
Tian J, Wong KK, Ho CM, Lok CN, Yu WY, Che CM, et al. Topical delivery of silver nanoparticles promotes wound healing. Chem Med Chem. 2007;2:129–36.
Shin SH, Ye MK, Kim HS, Kang HS. The effects of nano-silver on the proliferation and cytokine expression by peripheral blood mononuclear cells. Int Immunopharmacol. 2007;7:1813–8.
Bhol KC, Schechter PJ. Topical nanocrystalline silver cream suppresses inflammatory cytokines and induces apoptosis of inflammatory cells in a murine model of allergic contact dermatitis. Br J Dermatol. 2005;152:1235–42.
Department of Health and Human Services, Centers for Disease Control. Detection of: Oxacillin/Methicillin-resistant Staphylococcus aureus. URL: http://www.cdc.gov/ncidod/dhqp/ar_lab_mrsa.html. Access date: Apr./14/2008.
Cleusix V, Lacroix C, Vollenweider S, Duboux M, Le Blay G. Inhibitory activity spectrum of reuterin produced by Lactobacillus reuteri against intestinal bacteria. BMC Microbiol. 2007;7:101.
Palavecino E. Clinical, Epidemiological, and Laboratory Aspects of Methicillin-Resistant Staphylococcus aureus (MRSA) Infections. In: Yinduo J, editor. Methicillin-Resistant Staphylococcus aureus (MRSA) Protocols. Humana Press; 2007. pp. 3–4.
McDonnell GE. Chemical Disinfection. In: Antisepsis, disinfection, and sterilization. 2007;111–5.
Starodub ME, Trevors JT. Silver resistance in Escherichia coli R1. J Med Microbiol. 1989;29:101–10.
Lok CN, Ho CM, Chen R, He QY, Yu WY, Sun H, et al. Proteomic analysis of the mode of antibacterial action of silver nanoparticles. J Proteome Res. 2006;5:916–24.
Sondi I, Salopek-Sondi B. Silver nanoparticles as antimicrobial agent: a case study on E. coli as a model for Gram-negative bacteria. J Colloid Interface Sci. 2004;275:177–82.
Pal S, Tak YK, Song JM. Does the antibacterial activity of silver nanoparticles depend on the shape of the nanoparticle? A study of the Gram-negative bacterium Escherichia coli. Appl Environ Microbiol. 2007;73:1712–20.
Murray PR, Rosenthal KS, Kobayashi GS, Pfaller MA. Medical Microbiology. In: MMII Mosby, Inc.: Spain; 2005. pp. 12–3.
Salton MRJ, Kim KS. Structure. In: Baron S, editor. Medical Microbiology. 2009.
Acknowledgments
This project was done with the economical support of the Programa de Apoyo a la Investigacion Cientifica y Tecnologica (PAICyT) of the Universidad Autonoma de Nuevo Leon, Mexico.
Author information
Authors and Affiliations
Corresponding author
Additional information
NV Ayala and HH Lara made equal contributions to this study.
Rights and permissions
About this article
Cite this article
Ayala-Núñez, N.V., Lara Villegas, H.H., del Carmen Ixtepan Turrent, L. et al. Silver Nanoparticles Toxicity and Bactericidal Effect Against Methicillin-Resistant Staphylococcus aureus: Nanoscale Does Matter. Nanobiotechnol 5, 2–9 (2009). https://doi.org/10.1007/s12030-009-9029-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12030-009-9029-1