Abstract
Survival was examined from a Turkish liver transplant center of patients with HCC, to identify prognostic factors. Data from 215 patients who underwent predominantly live donor liver transplant for HCC at our institute over 12 years were included in the study and prospectively recorded. They were 152 patients within and 63 patients beyond Milan criteria. Patients beyond Milan criteria were divided into two groups according to presence or absence of tumor recurrence. Recurrence-associated factors were analyzed. These factors were then applied to the total cohort for survival analysis. We identified four factors, using multivariate analysis, that were significantly associated with tumor recurrence. These were maximum tumor diameter, degree of tumor differentiation, and serum AFP and GGT levels. A model that included all four of these factors was constructed, the ‘Malatya criteria.’ Using these Malatya criteria, we estimated DFS and cumulative survival, for patients within and beyond these criteria, and found statistically significant differences with improved survival in patients within Malatya criteria of 1, 5, and 10-year overall survival rates of 90.1%, 79.7%, and 72.8% respectively, which compared favorably with other extra-Milan extended criteria. Survival of our patients within the newly defined Malatya criteria compared favorably with other extra-Milan extended criteria and highlight the usefulness of serum AFP and GGT levels in decision-making.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hepatocellular cancer (HCC) is the fifth most common cancer and the second most common cause of cancer death worldwide [1]. Liver transplantation (LT) provides the only recurrence-free curative treatment option and the Milan criteria (MC) are adopted worldwide to select patients with HCC for LT. However, MC based on tumor morphological features are too strict and patients with favorable tumor biology who are beyond these criteria are excluded from LT and loose the opportunity for curative treatment [2]. University of California, San Francisco criteria (UCSF) [3], Barcelona Clinic Liver Cancer extended criteria (BCLC) [4], Up-to-Seven [5], Extended Toronto (ETC) [6], Hangzhou criteria (HC) [7], and similar extended criteria are defined to overcome limitations of MC. This study aims to examine the results of patients beyond Milan criteria who were transplanted at our institution. We evaluated post-transplant tumor recurrences and the factors associated with recurrence. Using these factors, we identified patients with HCC that would likely benefit long term from LT. We refer to these as the Malatya criteria. We found that alpha fetoprotein (AFP) and gamma glutamyl transferase (GGT) were important in identifying patients at risk for recurrence, in this retrospective study.
Materials and Methods
Patient Selection
Two hunderd fifteen patients underwent LT for HCC at our Liver Transplantation Institute, of whom 152 were within Milan criteria and 63 were beyond Milan criteria. Prospectively recorded data were analyzed retrospectively. This study has been approved by Inonu University Institutional Review Board (Approval no: 2018/1-9).
Study Design
This was a retrospective analysis of prospectively collected data. Age, gender, Child-Pugh score (CHILD), Model for End Stage Liver Disease (MELD) score, body mass index (BMI) (kg/m2), graft to recipient weight ratio (GRWR), AFP, histological tumor differentiation, microvascular invasion, total tumor size (TTS, cm), dominant or maximum tumor diameter (MTD, cm), number of nodules, MC, UCSF, Up-to-Seven, ETC, HC, neutrophil-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), platelets, alkaline phosphatase (ALKP), gamma glutamyl transferase (GGT), overall survival (OS) (days), and disease-free survival (DFS) (days) were analyzed.
Patients were divided into two groups, namely within MC (n = 152) and beyond MC (n = 63) for survival analysis, total = 215 (Fig. 1). Our initial aim was to identify parameters affecting tumor-free survival in patients with tumors beyond MC, using both univariate and multivariate analyses. The cut-off values which we used were defined from the receiver operating characteristics (ROC) analysis as follows: age (≤ 55 years), MELD (≤ 14), AFP (≤ 200 ng/mL), GGT (≤ 104 U/L), ALKP (≤ 135 U/L), TTS (≤ 8 cm), MTD (≤ 6 cm), NLR (≤ 2.4), PLR (≤ 113), platelets (≤ 125 109/L), and BMI (≤ 25 kg/m2) (Supplementary Fig. 1). Parameters with a p value < 0.05 in univariate analysis were included in the multivariate analysis model to determine any possible risk factor for tumor recurrence. Independent risk factors defined by this model were included in the Malatya criteria given below.
Definition of the Malatya Criteria
-
1.
Patients within MC have been also accepted as within Malatya criteria.
-
2.
Patients with tumors beyond the MC subgroup analysis revealed AFP (≤ 200 ng/mL), GGT (≤ 104 IU/L), differentiation grade (well/moderate), and MTD (≤ 6 cm) were independent risk factors for recurrence. These formed the basis of the Malatya criteria (Table 2), which were then applied to beyond-Milan HCC patients for survival analysis.
Preoperative Evaluation
In our institution prior to development of the Malatya criteria, patients were considered as eligble to live donor liver transplantation (LDLT) only if the disease was confined to liver and without any macrovascular invasion [8, 9]. Since 2016, the indication for LT is discussed in multidisciplinary medical committee that is constituted by transplant surgeons, medical oncologist, radiologist, nuclear medicine specialist, pathologist, and hepatologist. The law commisioned by the Turkish ministry of health on organ procurement and allocation allow deceased donor liver transplantation in patients with HCC that are within the MC. However, this does not apply to the recipients of the living donors. Therefore, patients with tumors beyond the Milan criteria can only receive LDLT.
Our preoperative evaluation includes liver function tests, complete blood counts, coagulation parameters, AFP levels, multislice computed tomography (MSCT) scans, magnetic resonance imaging (MRI), and some recently also had positron emission tomography/computerized tomography scan (PET/CT).
Post-Transplant Follow Up and Immunosuppressive Regimens
Surveillance of the AFP levels are perfomed monthly in the follow-up period. In the initial 2 years of the follow-up period, abdominal ultrasonography once in every 3 months and MSCT is performed once in every 6 months. In the follow-up period between postoperative second and fifth years, include annual MSCT. In patients with high AFP levels during the follow-up period, MSCT, MRI, and PET/CT are obtained. In patients with atypical nodules detected on MSCT with high AFP levels, a contrast-enhanced MRI was performed. In patients with high AFP levels and a typical nodule detected on MSCT is considered as having an HCC recurrence.
The immunosuppresive treatment protocol following LT for HCC includes routine initiation of tacrolimus (through level 6–10 ng/mL), mycophenolate mofetil, and corticosteroid for the first month. After the first month, low-dose tacrolimus (through level 5–7 ng/mL) and everolimus (through level 8–10 ng/mL), mycophenolate mofetil, and corticosteroid were given. Following the third month, low-dose tacrolimus + everolimus combined regimen is continued.
Statistical Analysis
Distribution of the parameters were evaluated with Shapiro-Wilk and Kolmogorov-Smirnov tests to show presence of normal distribution. Continuous (quantitative) variables were expressed as median (range), mean ± SD. Categorical (qualitative) variables were expressed as number and percentage. Comparisons between groups were analyzed with Mann-Whitney U test for continuous variables and with Pearson chi-square test, Yates corrected test, and Fisher’s exact tests for cathegorical variables. ROC analysis was performed to identify optimum cut-off values of continuous variables. A cut-off value for each variable was determined to obtain the most ideal sensitivity and specificity. Categorized variables were compared using univariate analysis methods (Pearson chi-square test, Fisher’s exact test, Yates corrected chi-square). Variables with a p value < 0.05 were taken into backward stepwise logistic regression model to define the independent risk factors. Hosmer and Lemeshow test was used for analysis of fit for logistic regression models. Kaplan-Meier survival estimate was used to determine overall survival and disease-free survival of the patients. Follow-up period was defined as the interval between LT until the date of last visit to the outpatient department for living patients or until the date of death of the patient. Time to disease recurrence was defined as the interval between the LT until the date a lesion that appeared to be a tumor was detected by biochemical (AFP) and radiological examination and/or a lesion diagnosed as HCC in another region of the patient. Statistical tests were considered significant when the corrensponding p value was less than 5%. All statistical analyses are peformed using Statistical Package for Sociak Sciences sofware version 25 (SPSS v25) (IBM, USA).
Results
Survival and recurrence analyzes were performed in patients within MC. The 5-year survival in patients with MC was 81.9%, and recurrence was found in only four patients (3.6%). The median survival of these four patients was 3.7 years (1343 ± 644.9 days). Then, we analyzed the survival of patients with MC, known as poor prognostic factors, with microvascular invasion positivity, poor differentiation, high AFP (AFP > 1000 ng/mL) (Supplementary Fig. 1). The mean survival of 33 patients with positive microvascular invasion within MC was 9.8 years (3554.1 ± 244.3 days); mean survival of 7 patients with poor differentiation within MC was 9.3 years (3349.6 ± 516.1 days); and the mean survival of 6 patients with AFP level > 1000 ng/mL within MC was 6 years (2191.7 ± 401.1 days). Given these long survival outcomes, we decided that no patient within MC should be excluded for liver transplantation. However, the ETC and Up-to-Seven criteria pushed some patients in MC out of liver transplant criteria. Thus, the new extended criteria to be established should directly cover patients within MC.
Extra-MC patients were analyzed next. A total of 63 patients with extra-Milan tumors, for whom there was follow-up data for at least 5 years, were studied in terms of tumor recurrence and non-recurrence. A ROC analysis was performed on all parameters mentioned in the ‘Materials and methods’ section (Supplementary Fig. 2). ROC analysis revealed the following cut-off values: age (≤ 55 years), MELD (≤ 14), AFP (≤ 200 ng/mL), GGT (≤ 104 IU/L), ALKP (≤ 135 IU/L), TTS (≤ 8 cm), MTD (≤ 6 cm), NLR (≤ 2.4), PLR (≤ 113), and platelets (≤ 125 109/L) were found as cut-off values.
The variables were then compared for the tumor recurrence and non-recurrence groups in all the extra-Milan patients. Parameters with a p value < 0.05 (Table 1) were then included in a subsequent multivariate analysis model. This multivariate analysis (Table 1) showed odds ratios (ORs) for recurrence of the following significant parameters: GGT (OR 5.87, p = 0.049), differentiation (OR 18.9, p = 0.013), AFP (OR 7.7, p = 0.035), and dominant tumor size (OR 12.4, p = 0.008). These 4 independent risk factors defined above in 41 patients who had tumors beyond MC were used to create the ‘Malatya criteria’ (Table 2, Supplementary Fig. 3).
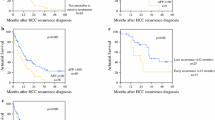
For patients who were within Malatya criteria (Fig. 1), OS rates at 1, 5, and 10 years were 90.1%, 79.7%, and 72.8%, respectively. For the 41 patients who were beyond MC but within Malatya criteria, OS survival rates were 94.7%, 71.9%, and 71.9% at 1, 5, and 10 years, respectvely. These survival rates were found to be similar to our 152 patients who were within MC (88.8%, 81.9%, 72.5% at 1, 5, and 10 years, respectively), as shown in Fig. 1 and Table 3. Figure 1 shows that the survival results for Malatya criteria (beyond Milan) were at least as good as the survival results for within Milan criteria, as well as for results of our patients using several extended (UCSF, Up-to-Seven, BCLC, ETC, Hangzhou) criteria to analyze our same patients (Table 4).
A multiple regression model showed the importance of serum levels of both AFP and GGT. To examine these two parameters further, we examined their relationship to survival in the total cohort, dichotomized by their ROC cut-off values (Fig. 2). For each parameter, there was a statistically significant survival difference between patients having above or below the serum cut-off values or 104 IU/mL for GGT and 200 ng/mL for AFP.
Discussion
Optimal patient selection criteria for LDLT in patients with HCC are still not clearly defined. MC enables 6–18% of HCC patients to undergo LT (10). Extended criteria enable LT for an additional 12–63% patients, compared with LTs performed in accordance with MC [10]. As previously suggested, patients would benefit from extended criteria in many ways where survival is the most important parameter [11]. However, expansion of selection criteria for HCC patients with decreased patient survival would result in only modest benefit in terms of the outcomes in patients with HCC. Nevertheless, any extended criteria should provide the patient with adequate benefit which is worth the donor undergoing a major abdominal surgery such as donor hepatectomy.
The criteria we have provided in the current work are associated with HCC patient post-transplant survival at 5- and 10-year overall survival with a rate of 79.7 and 72.8, respectively. At the same time, we offered a curative treatment option to an additional 27% patients to what could have been offered using MC alone, and achieved a favorable survival outcome by doing this. The results of the present study indicate that by using Malatya criteria, patients with HCC who have favorable outcomes can be effectively selected and LDLT can be safely performed.
As a center which performs the highest volume of LDLT in Turkey and Europe, we obtained 5-year survival rate of 81.9% to the HCC patients within MC, which was an expected outcome. However, our aim was to identify patients with a good prognosis who had HCCs that were beyond MC criteria, by using our Malatya criteria as developed from a multivariate regression analysis. The results of the present study show that with Malatya criteria, we were able to identify patients with tumors that were beyond Milan criteria, but with a favorable survival outcome which was better than other studies using current extended criteria and also similar to results from MC [3,4,5,6,7, 12,13,14,15,16]. In addition, poor outcomes of some patients within MC group have also been reported, some of which were patients with a single lesion greater than 3 cm, three separate lesions, unresponsive to loco-regional therapy (LRT), or with AFP > 20 ng/mL following LRT [17]. In our study, all of the patients with a tumor recurrence and who started within MC had AFP > 400 ng/mL (Inonu University Liver Transplant Institute unpublished data). However, these patients survived a median of 3.7 years. Most studies concerning patients within MC showed a 5-year survival rate of 70–80% following LT. Furthermore, HC, ETC, Toso, and Up-to-Seven criteria resulted in excluding a small group of patients within MC, while aiming to define good prognosis patients beyond MC [5,6,7, 14]. For this reason, we did not exclude any patients within MC, regardless of their AFP blood levels, as they had a good survival in our experience (Fig. 1 and Table 3). Our results show a 5-year OS rate of 81.9% in patients with tumors within MC. We had a group consisting 41 patients with tumors beyond MC but within Malatya, who have a 5-year OS 71.9% (Table 3). Ultimately, we obtained a 5-year OS rate of 79.7% for patients within Malatya criteria, likely because many of the patients were also within MC (n = 152). Other expanded criteria unfortunately did not provide this survival rate when those criteria were applied to the patients in our study (Table 4). Thus, we think expanded criteria should be applied to HCC patients beyond MC.
Another differentiating feature of Malatya criteria from other expanded criteria was in the use of results from levels of plasma GGT, which is a biochemical parameter. This enzyme level has been previously used in an HCC aggressiveness index [18,19,20]. A GGT level > 104 IU/mL was found to be related with poor outcomes (Table 1). Total GGT activity is increased in liver diseases and extrahepatic biliary tumors. GGT levels are at the highest level in embryonic liver and decrease to the lowest level in the postnatal period. However, GGT is re-expressed during the formation of HCC (onco-fetal). Blood GGT is divided into sub-fractions (I, II, and III). II is known to be hepatoma-specific GGT (HS-GGT) and has been used in diagnosis of HCC. GGT activity is elevated in be a parameter for poor survival following LT for HCC [21,22,23].
Another parameter is differentiation, which was found to be a poor prognostic factor in our study. This factor is also used in most of the expanded criteria [6, 7] and this contributes to the discussion concerning the necessity for liver biopsy before LT. However, it has also been reported that the grade of the differentiation can be evaluated with PET scan or can be deduced indirectly by tumor response to LRT [24,25,26].
High AFP levels have been consistently shown to predict poor prognosis after LT for HCC. Studies have shown that AFP levels associated with a greater risk of HCC recurrence or poor survival range from as low as 20 ng/mL to > 1000 ng/mL [7, 14, 27]. Microvascular invasion and poor differentiation were found to be prominent predictors of HCC recurrence. In the criteria we have identified, poor differentiation and AFP > 200 ng/mL were associated with increased tumor recurrences (Fig. 2).
The Malatya critera thus enabled us to extend LT to an additional 27% of patients more than MC. With this extension, in the present study, we were able to include patients within our Malatya criteria with resulting survival that was comparable to MC results.
Among the various extended criteria proposals, the highest 5- and 10-year survival rates included the Malatya criteria, as described here. We therefore propose an extension of the criteria for transplantation for HCC to tumors up to 6 cm maximum diameter, and especially to patients with low serum AFP and GGT levels.
In conclusion, Malatya criteria provide better long-time survival for HCC patients and contains plasma GGT levels as a new parameter and approach which is not present in the previous extended criteria.
Data Availability
The raw data used to support the findings of this study are available from the corresponding author upon request.
Change history
08 July 2020
The original version of this article unfortunately contained a mistake in the author group section.
Abbreviations
- AFP:
-
Alpha fetoprotein
- ALKP:
-
Alkaline phosphatase
- BCLC:
-
Barcelona Clinic Liver Cancer extended criteria
- BMI:
-
Body mass index
- CHILD:
-
Child-Pugh score
- DFS:
-
Disease-free survival
- ETC:
-
Extended Toronto criteria
- GGT:
-
Gamma glutamyl transferase
- GRWR:
-
Graft to recipient weight ratio
- HC:
-
Hagzhou criteria
- HCC:
-
Hepatocellular cancer
- LT:
-
Liver transplantation
- LDLT:
-
Live donor liver transplantation
- MC:
-
Milan criteria
- MELD:
-
Model for End Stage Liver Disease score
- MRI:
-
Magnetic resonance imaging
- MSCT:
-
Multislice computed tomography
- MTD:
-
Maximal tumor diameter
- NLR:
-
Neutrophil-lymphocyte ratio
- OS:
-
Overall survival
- OR:
-
Odds ratio
- PET/CT:
-
Positron emission tomography/computerized tomography scan
- PLR:
-
Platelet-to-lymphocyte ratio
- ROC:
-
Receiver operating characteristics
- TTS:
-
Total tumor size
- UCSF:
-
University of California, San Francisco criteria
References
World cancer report. http://publications.iarc.fr/Non-Series-Publications/World-Cancer-Reports/World-Cancer-Report-2014
Mazzaferro V, Regalia E, Doci R, Andreola S, Pulvirenti A, Bozzetti F, Montalto F, Ammatuna M, Morabito A, Gennari L. Liver transplantation for the treatment of small hepatocellular carcinomas in patients with cirrhosis. N Engl J Med. 1996;334:693–9.
Yao FY, Ferrell L, Bass NM, Watson JJ, Bacchetti P, Venook A, Ascher NL, Roberts JP. Liver transplantation for hepatocellular carcinoma: expansion of the tumor size limits does not adversely impact survival. Hepatology. 2001;33(6):1394–403.
Llovet JM, Pavel M, Rimola J, Diaz MA, Colmenero J, Saavedra-Perez D, Fondevila C, Ayuso C, Fuster J, Ginès P, Bruix J, Garcia-Valdecasas JC. Pilot study of living donor liver transplantation for patients with hepatocellular carcinoma exceeding Milan criteria (Barcelona clinic liver cancer extended criteria). Liver Transplant. 2018;24:369–79.
Mazzaferro V, Llovet JM, Miceli R, Bhoori S, Schiavo M, Mariani L, Camerini T, Roayaie S, Schwartz ME, Grazi GL, Adam R, Neuhaus P, Salizzoni M, Bruix J, Forner A, de Carlis L, Cillo U, Burroughs AK, Troisi R, Rossi M, Gerunda GE, Lerut J, Belghiti J, Boin I, Gugenheim J, Rochling F, van Hoek B, Majno P, Metroticket Investigator Study Group. Predicting survival after liver transplantation in patients with hepatocellular carcinoma beyond the Milan criteria: a retrospective, exploratory analysis. Lancet Oncol. 2009;10(1):35–43.
Sapisochin G, Goldaracena N, Laurence JM, Dib M, Barbas A, Ghanekar A, Cleary SP, Lilly L, Cattral MS, Marquez M, Selzner M, Renner E, Selzner N, McGilvray ID, Greig PD, Grant DR. The extended Toronto criteria for liver transplantation in patients with hepatocellular carcinoma: a prospective validation study. Hepatology. 2016;64(6):2077–88.
Zheng SS, Xu X, Wu J, Chen J, Wang WL, Zhang M, Liang TB, Wu LM. Liver transplantation for hepatocellular carcinoma: Hangzhou experiences. Transplantation. 2008;85(12):1726–32.
Isik B, Ince V, Karabulut K, Kayaalp C, Yilmaz S. Living donor liver transplantation for hepatocellular carcinoma. Transplant Proc. 2012;44(6):1713–6.
Kayaalp C, Ince V, Ersan V, Karakas S, Kahraman AS, Yilmaz S. Liver transplantation for hepatocellular carcinoma at Inonu University. J Gastrointest Cancer. 2017;48(3):268–71.
Toso C, Kneteman NM, James Shapiro AM, Bigam DL. The estimated number of patients with hepatocellular carcinoma selected for liver transplantation using expanded selection criteria. Transpl Int. 2009;22(9):869–75.
Mazzaferro V, Battiston C, Sposito C. Pro (with caution): extended oncologic indications in liver transplantation. Liver Transpl. 2018;24(1):98–103.
Patel SS, Arrington AK, McKenzie S, et al. Milan criteria and UCSF criteria: a preliminary comparative study of liver transplantation outcomes in the United States. Int J Hepatol. 2012;2012:253517.
Duffy JP, Vardanian A, Benjamin E, Watson M, Farmer DG, Ghobrial RM, Lipshutz G, Yersiz H, Lu DSK, Lassman C, Tong MJ, Hiatt JR, Busuttil RW. Liver transplantation criteria for hepatocellular carcinoma should be expanded: a 22-year experience with 467 patients at UCLA. Ann Surg. 2007;246(3):502–9.
Toso C, Meeberg G, Hernandez-Alejandro R, Dufour JF, Marotta P, Majno P, Kneteman NM. Total tumor volume and alpha-fetoprotein for selection of transplant candidates with hepatocellular carcinoma: a prospective validation. Hepatology. 2015;62(1):158–65.
Lee SG, Hwang S, Moon DB, Ahn CS, Kim KH, Sung KB, Ko GY, Park KM, Ha TY, Song GW. Expanded indication criteria of living donor liver transplantation for hepatocellular carcinoma at one large-volume center. Liver Transpl. 2008;14(7):935–45.
Ito T, Takada Y, Ueda M, Haga H, Maetani Y, Oike F, Ogawa K, Sakamoto S, Ogura Y, Egawa H, Tanaka K, Uemoto S. Expansion of selection criteria for patients with hepatocellular carcinoma in living donor liver transplantation. Liver Transpl. 2007;13(12):1637–44.
Mehta N, Dodge JL, Goel A, Roberts JP, Hirose R, Yao FY. Identification of liver transplant candidates with hepatocellular carcinoma and a very low dropout risk: implications for the current organ allocation policy. Liver Transpl. 2013;19(12):1343–53.
Carr BI, Guerra V, Giannini EG, et al. An HCC aggressiveness index and blood GTP, bilirubin and platelet levels. J Integr Oncol. 2016;5:172. https://doi.org/10.4172/2329-6771.1000172.
Carr BI, Guerra V, Giannini EG, et al. A liver index and its relationship to indices of HCC aggressiveness. J Integr Oncol. 2016;5(4):178.
Akkiz H, Carr BI, Yalçın KK, et al. Characteristics of hepatocellular carcinoma aggressiveness factors in Turkish patients. Oncology. 2018;94(2):116–24.
Wang NY, Zhang D, Zhao W, Fang GX, Shi YL, Duan MH. Clinical applicaton of an enzyme-linked immunosorbent assay detecting hepatoma-spesific gamma-glutamyltransferase. Hepatol Res. 2009;39:979–87.
Yao DF, Dong ZZ, Yao M. Specific molecular markers in hepatocellular carcinoma. Hepatobiliary Pancreat Dis Int. 2007;6(3):241–7.
Xia J, Song P, Sun Z, Sawakami T, Jia M, Wang Z. Advances of diagnostic and mechanistic studies of γ-glutamyl transpeptidase in hepatocellular carcinoma. Drug Discov Ther. 2016;10(4):181–7.
Lee SD, Kim SH. Role of positron emission tomography/computed tomography in living donor liver transplantation for hepatocellular carcinoma. Hepatobiliary Surg Nutr. 2016;5(5):408–14.
Lai Q, Avolio AW, Graziadei I, et al. Alpha-fetoprotein and modified response evaluation criteria in solid tumors progression after locoregional therapy as predictors of hepatocellular cancer recurrence and death after transplantation. Liver Transpl. 2013;19(10):1108–18.
Otto G, Herber S, Heise M, Lohse AW, Mönch C, Bittinger F, Hoppe-Lotichius M, Schuchmann M, Victor A, Pitton M. Response to transarterial chemoembolization as a biological selection criterion for liver transplantation in hepatocellular carcinoma. Liver Transpl. 2006;12(8):1260–7.
Hameed B, Mehta N, Sapisochin G, Roberts JP, Yao FY. Alpha-fetoprotein level > 1000 ng/mL as an exclusion criterion for liver transplantation in patients with hepatocellular carcinoma meeting the Milan criteria. Liver Transpl. 2014;20(8):945–51.
Acknowledgments
The authors declare that there is no funding used for the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original version of this article was revised: The original version of this article unfortunately contained a mistake in the author group section. The correct name of the second author is “Sami Akbulut”.
Rights and permissions
About this article
Cite this article
Ince, V., Akbulut, S., Otan, E. et al. Liver Transplantation for Hepatocellular Carcinoma: Malatya Experience and Proposals for Expanded Criteria. J Gastrointest Canc 51, 998–1005 (2020). https://doi.org/10.1007/s12029-020-00424-w
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-020-00424-w