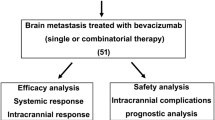
Abstract
Background
Brain metastases are rare in patients with colorectal cancer, but the incidence is expected to rise due to prolonged survival resulting from more effective regimens including anti-EGF-receptor and anti-angiogenic antibodies. Because of the potential fear of intracranial hemorrhage, patients with colorectal brain metastases have been excluded from clinical trials involving bevacizumab or aflibercept.
Patients
Five patients with colorectal brain metastases treated with bevacizumab-containing chemotherapy regimen following either neurosurgery, radiosurgery, or whole-brain radiotherapy were identified between 2009 and 2014. The clinicopathological data and outcomes for these patients were reviewed.
Results
Mean time to disease progression concerning brain metastases was 14.8 months (range 5–25). Overall survival was 26.2 months (range 7–42 months) and overall survival since diagnosis of brain metastases was 20.6 month (7–42). Best response was a partial response in two and a stable disease in three patients. Treatment-related adverse events were mild hypertension (grade 1), diarrhea (grade 1), and fatigue (grade 1). No intracranial hemorrhage was observed.
Conclusion
Bevacizumab in combination with chemotherapy is a feasible option for palliative treatment of patients with colorectal brain metastasis with a good safety profile.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is one of the most common cancers in Europe and one of the main causes for cancer-related deaths worldwide with 212,000 deaths reported for Europe in 2008 [1]. Up to 25 % of patients have synchronous metastatic disease and another 25 % develop metachronous metastases involving the liver in up to 80 % of all patients [2].
Median survival of patients with metastatic colorectal carcinoma improved significantly over the last two decades from approximately 10 months up to 3 years currently [3, 4]. The main reason for this improvement is the combination of fluorouracil with irinotecan and oxaliplatin and since 2004 in combination with targeted therapies. The current chemotherapy regimens for metastatic disease are combinations of fluorouracil with irinotecan (FOLFIRI), oxaliplatin (FOLFOX) combined with an antiangiogenic antibody (bevacizumab or more recently aflibercept), or an EGFR antibody (cetuximab or panitumumab) [5–7].
Brain metastases from CRC are a rare phenomenon. In a large population-based study involving 720 CRC patients, an estimated cumulative incidence of 1.2 % was reported [8]. In general, brain metastases are linked to a dismal prognosis with survival times of less than 6 months [9]. Since survival in metastatic CRC patients has steadily improved over the last decade, the risk of developing metachronous brain metastases might also rise.
Vascular endothelial growth factor A (VEGF-A) is part of a ligand family together with VEGF-B, VEGF-C, VEGF-D, and PLGF. VEGF-A signaling is essential for the regulation of angiogenesis and vascular hemostasis. The roles and functions of VEGF-A are multiple such as stimulation of endothelial cell growth in the artery, venules, and lymph vessels [10]. VEGF-A acts as a survival factor for endothelial cells and inhibits apoptosis [11]. Furthermore, VEGF-A can increase vascular permeability and is thereby an important factor of vessel homeostasis [12, 13].
It is well documented that vessel supply is essential for tumor growth [14] and that VEGF mRNA is highly upregulated in multiple human cancers [10, 12]. Tumor vessels show an aberrant phenotype with increased vascular permeability, decreased pericytic coverage, and higher fluid pressure due to pathological angiogenesis caused by the hypoxic tumor environment [14].
Bevacizumab is a selective monoclonal antibody inhibitor of VEGF-A. It was FDA approved for metastatic colorectal cancer in 2005, after showing efficacy in combination with a 5-FU-based therapy. Hurwitz et al. combined bevacizumab with fluorouracil and irinotecan first line in metastatic disease and were able to improve median survival from 15.5 to 20.3 months [15]. In another phase III trial (NO16966), bevacizumab was combined with an oxaliplatin regimen (FOLFOX, XELOX) and increased PFS from 8 to 9.4 months [16]. Second-line bevacizumab combined with oxaliplatin following progress under irinotecan regimen was tested in the E3200 trail [17] showing improved response rates from 8.6 to 22.7 % and improved median survival from 10.8 to 12.9 months. The results of the TML trial [18] proved the efficacy of maintaining bevacizumab in the second line after progression under the first-line regimen by increasing the median survival from 9.8 to 11.2 months.
Based on the occurrence of intracerebral bleeding in a patient with hepatocellular carcinoma and occult brain metastases, treated with bevacizumab in a pharmacokinetic trial [19], patients with brain metastasis were excluded from further clinical trials with bevacizumab [15, 17, 20, 21]. However, in daily clinical practice, no increased risk of intracerebral bleeding in patients with occult cerebral metastasis treated with bevacizumab-containing regimen vs. not receiving bevacizumab was reported [22, 23].
Therefore, the experience of bevacizumab in patients with known brain metastases is still limited. Here, we present the clinical outcome of five patients with brain metastases from colorectal cancer treated with bevacizumab-containing chemotherapy regimens following either neurosurgery, radiosurgery, or whole-brain radiotherapy.
Patients and Methods
Between 2009 and 2014, five patients were retrospectively identified in our outpatient clinic with brain metastasis and colorectal cancer, which were treated with bevacizumab-containing chemotherapy regimen. All patients received bevacizumab 7.5 mg/kg every 3 weeks intravenously combined with concomitant chemotherapy or as single agent as maintenance therapy. Concomitant chemotherapy was dependent on previously administered regimen and was given according to current guidelines. Tumor response was measured by CT or MRI scans every 8–12 weeks. Progressive disease, stable disease, or regressive disease was diagnosed according to RECIST criteria [24, 25]. Progressive disease was determined if new lesions were present or tumor volume increased above 20 %. Physical examinations, number of treatment cycles, blood results, and toxicity were evaluated every time chemotherapy was administered. Toxicity was graded along the CTCAE 3.0. All patients were followed until April 2014 or death.
Results
Patients’ Characteristics
All patients were male and the mean age was 65.8 years. Eastern Oncology Group performance status was 1 or 2. UICC stages were II–IV at time of first diagnosis (Table 1 in the Appendix). Histopathologically, all tumors were adenocarcinomas of the colon. All patients underwent initial surgery of the primary tumor and received at least one line of chemotherapy before bevacizumab was administered. Median time to diagnosis of brain metastasis since the time of initial tumor diagnosis was 29 months (range 0–58). Number of lesions was 1 (n = 4) or 2 (n = 1). Peritumoral edema was present in four patients, and one showed no edema. Three patients underwent initial R0 neurosurgical resection. Three patients received whole-brain radiation and four patients underwent gamma knife therapy, two as primary treatment and two during the further course.
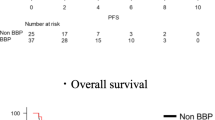
Efficacy
The mean time patients received bevacizumab was 14.2 months (5–25). In two patients, a partial response was documented. In one of those, an improvement of visual disturbance was achieved after the start of bevacizumab treatment. In the remaining three patients, a stable disease was documented. Mean time to disease progression concerning brain metastases was 14.8 months (5–25). Overall survival was 26.2 months (7–42 month), and overall survival since diagnosis of brain disease was 20.6 month (7–42). In April 2014 (data cut off), one patient was still alive. Cause of death was progressive systemic disease; in one patient, clinical findings suggested rapid progress of brain metastasis and consecutive death after stopping treatment due to patients’ will.
Safety Profile
No patient needed dose reduction or a change of chemotherapy protocol due to side effects related to bevacizumab. Observed toxicities were mild hypertension (n = 1), mild diarrhea (n = 5), and fatigue (n = 1). All were grade 1 according to CTCAE 3.0. One patient showed acute renal failure one time, possibly due to exsiccosis, and recovered fully.
No clinical signs and imaging results suggestive of intracranial hemorrhage were observed in any patient at any time.
Discussion
We presented five cases of patients treated in our outpatient clinic between 2009 and April 2014 with diagnosed colorectal cancer and brain metastasis. All patients received bevacizumab in combination with chemotherapy or alone as maintenance therapy (three patients in the further course). The patient’s overall survival ranged from 7 to 42 months and no severe side effects of bevacizumab were observed.
Patients with central nervous system disease were excluded from clinical trials with bevacizumab because of a single case of intracerebral bleeding in a phase I study [19]. Until 2009, more than 600,000 patients received bevacizumab [26]. Based on these datasets, more evidence on the safety profile of bevacizumab in patients with brain metastasis, mostly patients with non-small cell lung cancer (NSCLC), became available. In the phase IV Safety of Avastin in Lung (SaiL) trial, 281 patients were diagnosed with central nervous system (CNS) disease and 5 patients (2 %) experienced intracerebral bleeding during treatment. Overall the incidence of ≥grade 3 intracerebral bleeding in the intention to treat (ITT) population (n = 2212) was 1 % (n = 2) [27]. In the PASSPORT trial, 1/115 (0.8 %) patients treated with bevacizumab suffered from grade 1 intracerebral bleeding. In this trial, concomitant use of anticoagulants was allowed [22].
Besse and colleagues conducted a retrospective exploratory analysis with safety data from different randomized controlled phase II/III trials using bevacizumab [26]. They identified 8433 patients in randomized control trials (RCTs) (cancer types were CRC, NSCLC, breast, and other); 187 patients (2.2 %) suffered from CNS metastasis, and 91 patients (1.9 %) received bevacizumab. CRC was the underlying tumor in 34 patients, and of those, 16 were treated with a bevacizumab combination. In the bevacizumab group, three patients out of 91 patients (3.3 %) suffered from intracerebral hemorrhage; in the non-bevacizumab group, there was one (1.0 %) event of intracerebral bleeding. None of the bevacizumab-treated patients with intracerebral hemorrhage died due to the bleeding. The authors concluded no elevated risk for intracerebral bleeding in bevacizumab-treated patients with brain metastases.
Carden and colleagues addressed the question if any of the available anti-VEGF strategy (bevacizumab, sunitinib, sorafenib) might raise the risk for cerebral hemorrhage in patients with brain metastasis. They found a negligible rate of intracerebral bleeding (<1 %) even in the presence of cerebral metastasis and concluded that there is no evidence that anti-VEGF therapy yields an increased risk of intracranial bleeding [28].
To our knowledge, only one trial so far addressed the efficacy and safety of bevacizumab treatment in patients with known brain metastases (NCT00800202-BRAIN trail). The trial evaluated the efficacy and safety of bevacizumab in combination with etoposide or carboplatin/paclitaxel in patients with NSCLC and untreated brain metastasis. Only one patient out of 91 treated patients suffered from grade 1 intracerebral bleeding [29].
In contrast to NSCLC, cerebral metastasis is a rare event in patients suffering from metastatic colon cancer (mCRC), developing in 2–4 % of individuals. Most of the metastases (55 %) are located in the cerebellum [30–32]. The median time to diagnosis of brain disease ranges from 22 to 28 months [30, 33]. Without treatment, the median survival is just around 4–6 weeks in such patients [34, 35]. Positive prognostic factors in patients with cerebral CRC metastases are of young age (<65 years), solitary metastasis, absence of neurological deficits, and low general tumor burden [34].
For brain metastases, different treatment options apart from systemic chemotherapy are established, e.g., neurosurgical resection, stereotactic surgery (Gamma Knife, Cyber Knife), or whole-brain radiotherapy (WBRT) [36]. The mostly used approach is surgical resection followed by WBRT with significant improvement in overall survival [34]. WBRT alone or the addition to a surgical approach is of arguable benefit, but with stereotactical surgery, a relatively new approach is established as an efficient treatment option [37–40].
In recurrent glioblastoma, bevacizumab in combination with chemotherapy might result in prolonged progression-free survival [41–43]. However, no improvement in overall survival was found in two phase III trials evaluating the use of bevacizumab in first-line treatment of glioblastoma [44, 45]. Moreover, there is preclinical evidence that anti-VEGF treatment can promote an invasive phenotype in glioblastoma [46], which might be one reason for lacking survival benefit in this disease.
The advances in the treatment of mCRC such as aggressive surgical resection of limited metastatic disease, RAS testing, sequential treatment options, and others have yielded to mean survival times of 2–3 years. Therefore, it seems likely that more patients with mCRC will develop brain metastasis in the future. In this report, we show that multimodal treatment with bevacizumab-containing chemotherapy regimen following either neurosurgery, radiosurgery, or whole-brain radiotherapy is safe and might result in a prolonged survival in this prognostic unfavorable group of patients (Figs 1, 2, and 3).
Timeline of patients’ treatment course since diagnosis of brain disease. SD/PD or RD just applies to the metastatic brain disease, not systemic disease. FD first diagnosis of cancer, BD first diagnosis of brain disease, S surgical resection of brain metastasis, GK gamma knife treatment of brain metastasis, WBRT whole-brain radiation therapy, Cap capecitabin, Iri irinotecan, Ox oxaliplatin, Cet cetuximab, SD stable disease, PD progressive disease, RD regressive disease
Abbreviations
- CRC:
-
Colorectal cancer
- OS:
-
Overall survival
- CRP:
-
C-reactive protein
- EGF:
-
Epidermal growth factor
- FDA:
-
Food and Drug Administration
- VEGF:
-
Vascular endothelial growth factor
- CT:
-
Computed tomography
- NSCLC:
-
Non-small cell lung cancer
- MRI:
-
Magnetic resonance imaging
- CTCAE:
-
Common terminology criteria for adverse events
- CNS:
-
Central nervous system
- ITT:
-
Intention to treat
- RCT:
-
Randomized control trial
- ICH:
-
Intracerebral hemorrhage
- WBRT:
-
Whole-brain radiotherapy
References
Ferlay J, Shin HR, et al. Estimates of worldwide burden of cancer in 2008: GLOBOCAN 2008. Int J Cancer. 2008;127(12):2893–917.
Van der Pool AE, Damhuis RA, et al. Trends in incidence, treatment and survival of patients with stage IV colorectal cancer: a population based series. Color Dis. 2012;14(1):56–61.
Kopetz S, Chang GJ, et al. Improved survival in metastatic colorectal cancer is associated with adoption of hepatic resection and improved chemotherapy. J Clin Oncol. 2009;27(22):3677–83.
Heinemann V, Fischer von Weikersthal L, Decker T, et al. Randomized comparison of FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab as first-line treatment of KRAS wild-type metastatic colorectal cancer: German AIO study KRK-0306 (FIRE-3). J Clin Oncol. 2013;31:2013 (suppl; abstr LBA3506).
Van Cutsem E, Peeters M, Siena S, Humblet Y, Hendlisz A, et al. Open label phase III trial of panitumumab plus best supportive care compared with best supportive care alone in patients with chemotherapy refractory metastatic colorectal cancer. J Clin Oncol. 2007;25(13):1658–64.
Van Cutsem E, Tabernero J, Lakomy R, et al. Addition of aflibercept to fluorouracil, leucovorin, and irinotecan improves survival in a phase III randomized trial in patients with metastatic colorectal cancer previously treated with an oxaliplatin-based regimen. J Clin Oncol. 2012;30:3499–506.
Cunningham D, Atkin W, Lenz HJ, Lynch HT, et al. Colorectal cancer. Lancet. 2010;375:1030–47.
Schouten LJ, Rutten J, Huveneers HA, et al. Incidence of brain metastases in a cohort of patients with carcinoma of the breast, colon, kidney, and lung and melanoma. Cancer. 2002;94:2698–705.
Jung M, Ahn JB, Chang JH, Suh CO, Hong S, et al. Brain metastases from colorectal carcinoma: prognostic factors and outcome. J Neuro-Oncol. 2011;101(1):49–55.
Ferrara N, Davis-Smyth T. The biology of vascular endothelial growth factor. Endocr Rev. 1997;18:4–25.
Gerber HP, Dixit V, Ferrara N, et al. Vascular endothelial growth factor induces expression of the antiapoptotic proteins Bcl-2 and A1 in vascular endothelial cells. J Biol Chem. 1998;273:13313–6.
Dvorak HF, Brown LF, Detmar M, Dvorak AM, et al. Vascular permeability factor/vascular endothelial growth factor, microvascular hyperpermeability, and angiogenesis. Am J Pathol. 1995;146:1029–39.
Senger DR, Galli SJ, Dvorak AM, Perruzzi CA, Harvey VS, Dvorak HF. Tumor cells secrete a vascular permeability factor that promotes accumulation of ascites fluid. Science. 1983;219:983–5.
Folkman J. Tumor angiogenesis: therapeutic implications. NEJM. 1971;285:1182–6.
Hurwitz H, Fehrenbacher L, Novotny W, et al. Bevacizumab plus irinotecan, fluorouracil, and leucovorin for metastatic colorectal cancer. NEJM. 2004;350:2335–42.
Saltz LB, Clarke S, Diaz-Rubio E, Scheithauer A, Figer R, et al. Bevacizumab in combination with oxaliplatin-based chemotherapy as first-line therapy in metastatic colorectal cancer: a randomized phase III study. J Clin Oncol. 2008;26(12):2013–9.
Giantano BJ, Catalano PJ, Meropol NJ, O’Dwyer PJ, et al. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer, results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007;25(12):1539–44.
Bennouna J, Sastre J, Arnold D, Österlund P, et al. Continuation of bevacizumab after first progression in metastatic colorectal cancer (ML18147): a randomised phase 3 trial. Lancet Oncol. 2013;14(1):29–37.
Gordon MS, Margolin K, Talpaz M, et al. Phase I safety and pharmacokinetic study of recombinant human anti-vascular endothelial growth factor in patients with advanced cancer. J Clin Oncol. 2001;19:843–50.
Sandler A, Gray R, Perry MC, et al. Paclitaxel–carboplatin alone or with bevacizumab for non–small-cell lung cancer. NEJM. 2006;355:2542–50.
Escudier B, Pluzanska A, Koralewski P, et al. Bevacizumab plus interferon alfa-2a for treatment of metastatic renal cell carcinoma: a randomised, double-blind phase III trial. Lancet. 2007;370:2103–11.
Socinski MA, Langer CJ, Huang JE, et al. Safety of bevacizumab in patients with non-small-cell lung cancer and brain metastases. J Clin Oncol. 2009;27:5255–61.
Archer V, Reck M, Sandler AB, et al. Risk of symptomatic central nervous system (CNS) progression and secondary hemorrhage in patients with non-squamous non-small cell lung cancer (NSCLC) receiving bevacizumab (BV)-based first-line therapy. J Clin Oncol. 2008;26:15. abstr 8114.
Therasse P, Arbuck SG, et al. New guidelines to evaluate the response to treatment in solid tumors. J Natl Cancer Inst. 2000;92(3):205–16.
Eisenhauer EA, Therasse P, Bogaerts J, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45(2):228–47.
Besse B, Lasserre SF, Compton P, Huang J, Augustus S, Rohr UP, et al. Bevacizumab safety in patients with central nervous system metastases. Clin Cancer Res. 2010;16(1):269–78.
Crinò L, Dansin E, Garrido P, et al. Safety and efficacy of first-line bevacizumab-based therapy in advanced non-squamous non-small-cell lung cancer (SAiL, MO19390): a phase 4 study. Lancet. 2010;11:733–40.
Carden CP, Larkin JM, Rosenthal MA. What is the risk of intracranial bleeding during anti-VEGF therapy? Neuro Oncol. 2008;10:624–30.
Besse B, Le Moulec S, Senellart H, et al. Final overall survival (OS) results of a non comparative phase II study of bevacizumab (B) plus first-line chemotherapy or second-line erlotinib (E) in nonsquamous NSCLC patients with asymptomatic untreated brain metastases (BM)(BRAIN). J Clin Oncol. 2013; 31, (suppl; abstr 8059); ASCO Anual Meeting 2013; Abstract Number: 8059.
Go PH, Klaassen Z, Meadows MC, Chamberlain R, et al. Gastrointestinal cancer and brain metastasis—a rare and omnious sign. Cancer. 2011;117(16):3630–40.
Cascino TL, Leavengood JM, Kemeny N, Posner JB. Brain metastases from colon cancer. J Neuro-Oncol. 1983;1:203–9.
Wronski M, Arbit E. Resection of brain metastases from colorectal carcinoma in 73 patients. Cancer. 1998;85:1677–85.
Bartelt S, Momm F, Weissenberger C, Lutterbach J, et al. Patients with brain metastases from gastrointestinal tract cancer treated with whole brain radiation therapy: prognostic factors and survival. World J Gastroenterol. 2004;10:3345–8.
Farnell GF, Buckner JC, Cascino TL, O’Connell MJ, et al. Brain metastases from colorectal carcinoma. The long term survivors. Cancer. 1996;78:711–6.
Hammoud MA, McCutcheon IE, Elsouki R, Schoppa D, et al. Colorectal carcinoma and brain metastasis: distribution, treatment, and survival. Ann Surg Oncol. 1996;3:453–63.
Suzuki Y, Yamaguchi T, Matsumoto H, Nakano D, et al. Prognostic factors and treatment effects in patients with curatively resected brain metastasis from colorectal cancer. Dis Colon Rectum. 2014;57(1):56–63.
Tsao MN, Lloyd N, Wong RK, Chow E, Rakovitch E, Laperriere N. Whole brain radiotherapy for the treatment of newly diagnosed multiple brain metastases. Cochrane Database Syst Rev. 2012; 4:CD003869. doi:10.1002/14651858.CD003869.pub3.
Patil CG, Pricola K, Sarmiento JM, Garg SK, Bryant A, Black Kl, et al. Whole brain radiation therapy (WBRt) alone versus WBRt and radiosurgery for the treatment of brain metastases. Cochrane Database Syst Rev. 2012; 9.
O’Neill BP, Iturria NJ, Link MJ, Pollock BE, Ballman KV, O’Fallon JR, et al. A comparison of surgical resection and stereotactic radiosurgery in the treatment of solitary brain metastases. Int J Radiat Oncol Biol Phys. 2003;55:1169–76.
Kondziolka D, Patel A, Lunsford LD, Kassam A, Flickinger JC, et al. Stereotactic radiosurgery plus whole brain radiotherapy versus radiotherapy alone for patients with multiple brain metastases. Int J Radiat Oncol Biol Phys. 1999;45:427–34.
Poulsen NHS, Grunnet K, Sorensen M, Olsen P, et al. Bevacizumab plus irinotecan in the treatment patients with progressive recurrent malignant brain tumours. Acta Oncol. 2009;48:52–8.
Vredenburg JJ, Desjardins A, Hernon JE, Dowell JM, et al. Phase II trial of bevacizumab and irinotecan in recurrent malignant glioma. Clin Cancer Res. 2007;13:1253–9.
Friedman HS, Prados MD, Wen PY, Mikkelsen T, Schiff D, Abrey LE, et al. Bevacizumab alone and in combination with irinotecan in recurrent glioblastoma. J Clin Oncol. 2009;27(28):4733–40.
Gilbert MR, Dignam JJ, Armstrong TS, Wefel JS, Blumenthal DT, et al. A randomized trial of bevacizumab for newly diagnosed glioblastoma. NEJM. 2014;370(8):699–708.
Chinot OL, Wick W, Mason W, Henriksson R, Saran F, et al. Bevacizumab plus radiotherapy-temozolomide for newly diagnosed glioblastoma. NEJM. 2014;370(8):709–22.
Paez-Ribes M, Allen E, Hudock J, Takeda T, Okuyama H, et al. Antiangiogenic therapy elicits malignant progression of tumors to increased local invasion and distant metastasis. Cancer Cell. 2009;15:220–31.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
O. Waidmann received a travel grant from Roche, and O. Bähr received consulting fees and travel grants from Roche. S. Zeuzem and J. Trojan received consulting fees from Roche.
Financial Support
Nothing to declare
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
ESM 1
(DOC 41 kb)
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Finkelmeier, F., You, SJ., Waidmann, O. et al. Bevacizumab in Combination with Chemotherapy for Colorectal Brain Metastasis. J Gastrointest Canc 47, 82–88 (2016). https://doi.org/10.1007/s12029-015-9795-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12029-015-9795-z