Abstract
Background
Acute muscle wasting is common in critically ill patients, and this can lead to unfavorable clinical outcomes. The aim of this study was to identify factors associated with muscle wasting and to investigate the association between skeletal muscle wasting and prolonged hospital stay in critically ill patients with acute brain injury.
Methods
This single-center prospective observational study was conducted in critically ill patients with acute brain injury who stayed in the intensive care unit for at least 1 week. The rectus femoris cross-sectional area was measured via ultrasound at baseline and a week after the first assessment. Univariate and multivariate logistic regression analyses were performed to identify factors that predicted prolonged hospital stay.
Results
A total of 86 patients were included in the study. Their mean age was 49.4 ± 16.9 years, 57% were male, and 46.5% had an admission diagnosis of subarachnoid hemorrhage. The percentage change in the rectus femoris cross-sectional area was 15.8% (95% confidence interval [CI] − 19.8% to − 12.0%; p < 0.001), and 57% of all patients had acute muscle wasting. According to the univariate analysis, there was a significant association between prolonged hospital stay and acute muscle wasting (odds ratio [OR] 3.677; 95% CI 1.487–9.043; p = 0.005), mechanical ventilation status (OR 3.600; 95% CI 1.455–8.904; p = 0.006), and Glasgow Coma Scale score (OR 0.888; 95% CI 0.808–0.976; p = 0.014) at intensive care unit admission. The multivariate analysis demonstrated that acute muscle wasting (OR 3.449; 95% CI 1.344–8.853; p = 0.010) was an independent risk factor for prolonged hospital stay.
Conclusions
There was considerable muscle wasting in critically ill patients with brain injuries over a 1-week period. Acute muscle wasting was associated with prolonged hospital stay in critically ill patients with acute brain injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
An acute brain injury is defined as an acute cerebral disorder consequent to trauma or to a cerebrovascular event with high morbidity and mortality [1,2,3]. Critically ill patients with acute brain injury suffer a hypercatabolic state caused by stress-related and proinflammatory cytokines and hormones that can contribute to protein catabolism in skeletal muscles and muscle wasting [4, 5]. Muscle wasting begins early during critical illness, and patients can lose nearly 2% of skeletal muscle per day during the first week [6]. Although the pathophysiology of skeletal muscle wasting is related to several physiological processes, including insulin resistance, inflammation, oxidative stress, and mitochondrial damage, it is not fully understood [7]. Critically ill patients with brain injury have a high severity of illness requiring prolonged immobilization, mechanical ventilation, and higher doses of sedative medications, all of which are independent risk factors for muscle wasting [7, 8]. Moreover, brain injury causes an increase in catabolism, and this may lead to inadequate nutrition [9]. Therefore, patients with brain injury may be more susceptible to the risk of muscle wasting, but there are limited data on this condition [10,11,12].
To diagnose muscle wasting and weakness, ideally, clinical measurement of muscle strength should be performed. However, for this to be implemented, patients must be awake and cooperative and must understand the assessor’s instructions. Because patients are often unconscious or uncooperative, such an evaluation is often not possible, particularly with the diagnosis of muscle wasting in critically ill patients with brain injury [13]. However, various imaging methods are available for the evaluation of skeletal muscle, each with advantages and disadvantages [14, 15]. Of these methods, muscle ultrasound is being discussed with growing interest as a noninvasive tool to assess and track changes in the muscles of critically ill patients. The quadriceps is the most commonly measured region to assess muscle loss via ultrasound in these patients [16,17,18]. Previous studies have reported quadriceps muscle ultrasound as a potential tool for prediction of clinical outcomes of critical illness [19, 20]. However, whether the diagnosis of muscle wasting based on skeletal muscle ultrasound measurement is associated with clinical outcomes requires further investigation.
The aim of in the present study was to assess the association between acute muscle wasting and prolonged hospital stay in critically ill patients with acute brain injury. The secondary aim was to investigate clinical and nutritional parameters associated with acute muscle wasting and prolonged hospital stay.
Methods
Study Design and Patients
This prospective observational study was conducted in the adult intensive care unit (ICU) of a tertiary care university hospital between January 2020 and June 2022. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement was used to organize and report the results [21]. The study protocol was approved by the Ethics Committee of Karadeniz Technical University. The procedures were in agreement with the Declaration of Helsinki, and written informed consent was obtained from all the participants or their relatives.
Adult critically ill patients with an acute brain injury defined as an acute cerebral disorder consequent to trauma or to a cerebrovascular event (subarachnoid hemorrhage, intracerebral hemorrhage, traumatic brain injury, acute ischemic stroke) and expected to stay in the ICU for at least 7 days were included. The exclusion criteria were based on identifying acute muscle wasting in the ICU and were aimed to exclude potential patient who had experienced or may experience muscle loss due to different mechanisms. The exclusion criteria were as follows: age < 18 years and > 90 years; other critically ill neurological populations (e.g., brain tumor, status epilepticus, anoxic-ischemic brain injury); expected to die or decision taken for withdrawal of life-sustaining therapy; pregnancy; body mass index > 35 kg/m2; the presence of diseases that may lead to chronic mobility impairment or muscle wasting at baseline, such as a prior disabling cerebrovascular event or primary systemic neuromuscular disease; amputated lower limbs; burn injury; malignancy; kidney failure with dialysis dependence; severe chronic liver disease or acute liver failure; history of ICU admission within the previous 6 months; a transfer record from an ICU and palliative care unit; and enrollment in an intervention study affecting the usual care process.
Data Collection
The demographic and clinical characteristics, including the patients’ age, sex, type of brain injury, comorbidity status and Charlson Comorbidity Index score [22], Acute Physiology and Chronic Health Evaluation II score [23], Sequential Organ Failure Assessment score [24], and Glasgow Coma Scale (GCS) [25] score, were recorded. The modified Nutrition Risk in the Critically Ill score (in which a score of > 4 is high nutrition risk) was calculated to assess nutritional risk [26]. Daily cumulative doses of analgesic, sedative, and neuromuscular blocking agents were collected using drug administration records, and they were converted to equivalents [27]. Clinical outcomes were assessed based on the duration of mechanical ventilation, the length of the ICU and hospital stay, and ICU mortality. The length of hospital stay was defined as the period from admission to the ICU until discharge to home or the palliative care unit or until death.
Dietary Assessment
Daily caloric and protein intake was recorded from all sources, including total parenteral nutrition, enteral nutrition, and oral nutrition, for a week. Intravenous energy was received from parenteral nutrition as well as from nonnutritional energy sources (dextrose solutions or propofol). Daily oral intake was evaluated with dietary recalls. The software Nutrition Knowledge System [28] was used to calculate daily energy and protein intakes from the total food and fluids consumed. Energy requirements were calculated using the Harris–Benedict equation [29]. Protein requirements were calculated according to the European Society for Clinical Nutrition and Metabolism guidelines for ICU patients [30]. Daily energy and protein adequacy (percentage) was calculated as follows: (daily amount delivered)/(daily estimated requirements) × 100. Adequacy over the study period was calculated as the total adequacy divided by the number of study days. Mean energy and protein delivered per kilogram of actual body weight averaged per study day were recorded.
Muscle and Anthropometric Measurements
All muscle and anthropometric measurements were conducted on the right side of the body when possible, as per International Standards for Anthropometric Assessment, at baseline (within 48 h of ICU admission) and on study day 7. When this was not possible, the left side of the body was used for measurements. Body weight was measured using the weighing scales of the ICU beds. Height and body weight were used to calculate the body mass index. Mid-arm circumference (cm) was measured with the aid of an inelastic tape by marking the midpoint between the acromion and olecranon protrusion of the patient. Calf circumference (cm) was measured at the largest circumference of the leg. The mean of three consecutive measurements was recorded. The rectus femoris cross-sectional area (RFCSA) (cm2) was measured by B-mode ultrasonography (Esaote MyLab) using a variable-band linear array 13–4 MHz probe with 50 mm (Esaote LA523) by a single intensive care physician. Validation of muscle ultrasound measurements by the intensive care physician was compared with that by a radiology physician. The RFCSAs of 20 critically ill adult patients were separately measured by both physicians blinded to patient information. The interobserver reliability analysis was high (r = 0.942; p < 0.001). The measurement was performed in accordance with the protocols previously described in the ICU setting [31]. Ultrasound measurements were obtained with the transducer placed perpendicular to the long axis of the thigh at the upper two thirds of the length between the anterior superior iliac spine and the upper pole of the patella. Measurements were performed by applying minimal compression to the ultrasound probe. The inner echogenic line of the rectus femoris was traced manually on a frozen image, and the RFCSA was calculated. A decrease in the RFCSA of ≥ 10% was considered to define muscle wasting in accordance with previous studies in critically ill patients [32, 33].
Statistical Analyses
There were no data on muscle wasting and clinical outcomes in critically ill patients with acute brain injury. Therefore, our sample size calculation was based on acute muscle loss. Previous studies of changes in the RFCSA over 1 week in critically ill patients have reported a wide range of effect sizes, from 0.2 to 0.8 [34,35,36]. We calculated the sample size as 84 patients using the software G*Power [37], with an α value of 0.05, a power of 0.95, and an effect size of 0.4. All statistical analyses were performed using SPSS (version 21; IBM). Categorical data were presented as count (percentage), and continuous data were reported as mean ± standard deviation or median (interquartile range [IQR]) as appropriate. Normality was assessed using the Kolmogorov–Smirnov test and confirmed by visual inspection of the histogram. For the comparison between measurements performed in the first and second assessments, a paired t-test was used. Normally distributed data were analyzed using Student’s t-test, and nonnormally distributed data were analyzed using the Mann–Whitney U-test. Logistic regression analysis was used to identify independent risk factors for prolonged stay. Variables with a p value lower than 0.2 in the univariate analysis were included in the multivariable regression analysis. All statistical tests were considered statistically significant at a two-tailed p value < 0.05.
Results
Clinical and Demographic Characteristics of the Patients
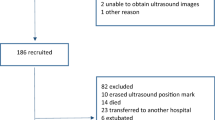
A total of 1,270 patients were screened, and 126 patients were included in the study; 40 patients were excluded because of death, discharge, or protocol violation, leaving a total of 86 patients (Fig. 1). The patient demographics and clinical characteristics are presented in Table 1. The mean age was 49.4 ± 16.9 years, and 57% were male. The GCS score on admission to the ICU was 10 (5–15), and the most common admission diagnosis was subarachnoid hemorrhage (46.5%). The median (IQR) durations of mechanical ventilation and ICU and hospital stay were 4 (0–20), 16 (12–23), and 23 (15–31.7) days, respectively.
Association Between Muscle Wasting, Prolonged Hospital Stay, and Clinical Parameters
Time to baseline ultrasound measurement was a median (IQR) of 1 (1–1) day following ICU admission. The RFCSA decreased significantly from study days 1 to 7 (15.8%; 95% confidence interval [CI] − 19.8% to − 12.0%; p < 0.001). A decrease in the RFCSA of ≥ 10% was seen in 57% of all patients. Patients with a lower median GCS score at admission to the ICU had a longer hospital stay (p = 0.006). There was no difference in age, sex, comorbidity, type of brain injury, and Acute Physiology and Chronic Health Evaluation II, Sequential Organ Failure Assessment, and modified Nutrition Risk in the Critically Ill scores between the groups. The sedative or analgesia agent taken (at least one time) most frequently by the patients was opiates (67.4%), followed by dexmedetomidine (50%), benzodiazepines (39.5%), and propofol (9.3%), and 5.8% of the patients took a neuromuscular blocking agent. The median dexmedetomidine dose (μg) was significantly higher in the muscle wasting group (p = 0.017).
Association Between Muscle Wasting, Prolonged Hospital Stay, and Nutritional Parameters
The mean energy delivered was 1,115 ± 440 kcal/d (15.5 ± 6.7 kcal/kg/d), with 53% ± 24% energy adequacy. The mean protein delivered was 71.2 ± 31.4 g/d (1 ± 0.5 g/kg/d), with 75.9% ± 35.2% protein adequacy. There was no difference in energy/protein intake or adequacy between the groups. The patients with muscle wasting had higher percentages of change in calf circumference (p = 0.025) (Table 2).
Factors Associated with Prolonged Hospital Stay from the Univariate and Multivariate Regression Analyses
Univariate and multivariate logistic regression analyses were used to identify the factors influencing prolonged hospital stay in critically ill patients with acute brain injury. In the univariate analyses, a significant association was found between prolonged hospital stay and acute muscle wasting (odds ratio [OR] 3.677; 95% CI 1.487–9.043; p = 0.005), mechanical ventilation status (OR 3.600; 95% CI 1.455–8.904; p = 0.006), and GCS score (OR 0.888; 95% CI 0.808–0.976; p = 0.014) at ICU admission. The multivariate analyses demonstrated that muscle wasting (OR 3.449; 95% CI 1.344–8.853; p = 0.010) was an independent risk factor for prolonged hospital stay (Table 3).
Discussion
Our results demonstrated a significant decrease in the RFCSA within a week, and 57% of the patients had muscle wasting. Further, acute muscle wasting increases the risk of prolonged hospital stay in critically ill patients with acute brain injury.
In critically ill patients, the greatest loss of muscle mass occurs during the first week in the ICU [38]. Similar to our results, studies have reported a 12.5–23.2% decrease in the RFCSA from baseline in the first week [32, 39]. In line with other studies conducted with critically ill patients [40], in the present study, there was a high rate of muscle wasting in critically ill patients with acute brain injury. The mechanisms of muscle wasting in patients with acute brain injury have not been elucidated, and further studies are needed to determine the relationship between muscle wasting in the critical care period and sarcopenia during post-acute care.
There is increasing evidence that sedative, analgesic, and neuromuscular blocking agents affect neuromusculoskeletal function and are associated with the risk of ICU-acquired weakness, but there is not enough evidence to definitively establish the effect of these agents [41,42,43]. In the present study, we found that higher doses of dexmedetomidine were associated with acute muscle wasting, but other sedative and analgesic agents were not. Previous studies have mostly focused on the effect of drugs on the risk of ICU-acquired weakness, and it is known that one of the most important risk factors associated with ICU-acquired weakness is the length of stay in the ICU [44]. However, further studies are needed to determine the relationship between drugs and muscle wasting that occurs during the 7-to 10-day period, which is the acute period.
To date, few researchers have either reported nutrition intake or examined the effect of medical nutrition therapy on the maintenance of skeletal muscle during critical illness. Thus, how the adequacy of protein and energy intake affects muscle loss in intensive care populations remains unclear. Although energy and/or protein intake may seem to be associated with muscle loss [45, 46], there are also data reporting no impact on the loss of skeletal muscle [47, 48], as in the present study. Interestingly, two recent meta-analyses reported conflicting results on the relationship between protein intake and muscle wasting in critically ill patients [49, 50]. On the other hand, Gungor et al. [51] reported that higher calorie or protein intake was negatively correlated with the magnitude of reduction in cross-sectional muscle area, as evaluated by computed tomography in patients with acute dysphagic ischemic stroke. Future studies on this topic with a specific emphasis on personalized nutritional care, taking into account the patient population, disease severity, and being in a vulnerable population in terms of muscle loss, would be of importance to understand the nutritional interventions for improvement of clinical outcomes in critically ill patients.
Sarcopenia at ICU admission is associated with unfavorable outcomes, including longer mechanical ventilation, longer ICU and hospital stay, and increased risk of mortality [52, 53]. However, only a few studies have been reported on the effect of loss of muscle mass on clinical outcomes, and none of these studies were conducted in critically ill patients with acute brain injury. For instance, it was reported that the change in quadriceps muscle layer thickness, but not RFCSA, over the first week of critical illness was a predictor of 60-day mortality in mechanically ventilated critically ill patients [34]. Sabatino et al. [54] found a relationship between severity of quadriceps muscle thickness loss in the first 5 days of ICU stay and discharge status in critically ill patients with acute kidney injury. On the other hand, in other studies, no relationship was reported between acute muscle loss and clinical outcomes in critically ill patients [35, 55]. In the present study, muscle loss was assessed using ultrasound as a decrease in the RFCSA of ≥ 10% to define muscle wasting, and muscle wasting was predictive of prolonged hospital stay in critically ill patients with acute brain injury. Comparison of study results is difficult because there is no consensus on the optimal measurement protocol for muscle ultrasound, and image quality can be affected by factors related to the practitioner and the patient [56]. To more precisely characterize skeletal muscle wasting, integration of different parameters may be necessary. Surprisingly, the multivariate regression analyses in our study showed that mechanical ventilation status was not associated with prolonged hospital stay. However, this may have been due to the fact that we showed the mechanical ventilation status of our patients between the time points when we evaluated muscle loss.
The present study has some limitations. First, our arbitrary definition of prolonged hospital stay and our single-institution patient population may limit the generalizability of our findings to other settings and institutions. Second, energy requirements were determined using the Harris–Benedict equation, which is recommended for use in the absence of indirect calorimetry in intensive care patient populations. Third, the potential for selection bias should be considered, as primary patient selection was based on the investigator’s subjective assessment of which patients were likely to remain in the ICU for longer than a week. Finally, the observational nature of the present study does not allow any inference about causality to be made.
Conclusions
In conclusion, muscle wasting occurs early and rapidly within the first 7 days of ICU stay in critically ill patients with acute brain injury. Muscle wasting appears to be related to unfavorable outcome in critically ill patients with acute brain injury. Future studies are required to further confirm these findings and determine an optimal strategy to specifically target modifiable risk factors to prevent muscle wasting.
References
Robba C, Poole D, McNett M, Asehnoune K, Bösel J, Bruder N, et al. Mechanical ventilation in patients with acute brain injury: recommendations of the European Society of Intensive Care Medicine consensus. Intensive Care Med. 2020;46(12):2397–410.
Roozenbeek B, Maas AI, Menon DK. Changing patterns in the epidemiology of traumatic brain injury. Nat Rev Neurol. 2013;9(4):231–6.
Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. 2009;373(9675):1632–44.
Abdelmalik PA, Dempsey S, Ziai W. Nutritional and bioenergetic considerations in critically ill patients with acute neurological injury. Neurocrit Care. 2017;27(2):276–86.
Sharma K, Mogensen KM, Robinson MK. Pathophysiology of critical illness and role of nutrition. Nutr Clin Pract. 2019;34(1):12–22.
Fazzini B, Märkl T, Costas C, Blobner M, Schaller SJ, Prowle J, et al. The rate and assessment of muscle wasting during critical illness: a systematic review and meta-analysis. Crit Care. 2023;27(1):2.
Duan K, Gao X, Zhu D. The clinical relevance and mechanism of skeletal muscle wasting. Clin Nutr. 2021;40(1):27–37.
Latronico N, Herridge M, Hopkins RO, Angus D, Hart N, Hermans G, et al. The ICM research agenda on intensive care unit-acquired weakness. Intensive Care Med. 2017;43(9):1270–81.
Lee HY, Oh BM. Nutrition management in patients with traumatic brain injury: a narrative review. Brain Neurorehabil. 2022;15(1): e4.
García-Martínez MÁ, MontejoGonzález JC, García-de-Lorenzo Y Mateos A, Teijeira S. Muscle weakness: understanding the principles of myopathy and neuropathy in the critically ill patient and the management options. Clin Nutr. 2020;39(5):1331–44.
Silva PE, Maldaner V, Vieira L, de Carvalho KL, Gomes H, Melo P, et al. Neuromuscular electrophysiological disorders and muscle atrophy in mechanically-ventilated traumatic brain injury patients: new insights from a prospective observational study. J Crit Care. 2018;44:87–94. Erratum in: J Crit Care. 2019;50:316.
Kofler M, Reitmeir P, Glodny B, Rass V, Lindner A, Ianosi BA, et al. The loss of temporal muscle volume is associated with poor outcome in patients with subarachnoid hemorrhage: an observational cohort study. Neurocrit Care. 2023;39(1):198–206.
Vanhorebeek I, Latronico N, Van den Berghe G. ICU-acquired weakness. Intensive Care Med. 2020;46(4):637–53.
Looijaard WG, Molinger J, Weijs PJ. Measuring and monitoring lean body mass in critical illness. Curr Opin Crit Care. 2018;24(4):241–7.
Mundi MS, Patel JJ, Martindale R. Body composition technology: implications for the ICU. Nutr Clin Pract. 2019;34(1):48–58.
Mourtzakis M, Parry S, Connolly B, Puthucheary Z. Skeletal muscle ultrasound in critical care: a tool in need of translation. Ann Am Thorac Soc. 2017;14(10):1495–503.
Palakshappa JA, Bakhru RN. Bedside ultrasonography can and should be used in the intensive care unit to evaluate muscle atrophy. Ann Am Thorac Soc. 2019;16(9):1107–11.
Lima J, Foletto E, Cardoso RC, Garbelotto C, Frenzel AP, Carneiro JU, et al. Ultrasound for measurement of skeletal muscle mass quantity and muscle composition/architecture in critically ill patients: a scoping review on studies’ aims, methods, and findings. Clin Nutr. 2024;43(1):95–110.
Mueller N, Murthy S, Tainter CR, Lee J, Riddell K, Fintelmann FJ, et al. Can sarcopenia quantified by ultrasound of the rectus femoris muscle predict adverse outcome of surgical intensive care unit patients as well as frailty? A prospective, observational cohort study. Ann Surg. 2016;264(6):1116–24.
Toledo DO, Freitas BJ, Dib R, Pfeilsticker FJ, Santos DM, Gomes BC, et al. Peripheral muscular ultrasound as outcome assessment tool in critically ill patients on mechanical ventilation: an observational cohort study. Clin Nutr ESPEN. 2021;43:408–14.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP; STROBE Initiative. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. Int J Surg. 2014;12(12):1495–9.
Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol. 1994;47(11):1245–51.
Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13(10):818–29.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonça A, Bruining H, et al. on behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22(7):707–10.
Teasdale G, Jennett B. Assessment of coma and impaired consciousness A practical scale. Lancet. 1974;2(7872):81–4.
Rahman A, Hasan RM, Agarwala R, Martin C, Day AG, Heyland DK. Identifying critically-ill patients who will benefit most from nutritional therapy: further validation of the “modified NUTRIC” nutritional risk assessment tool. Clin Nutr. 2016;35(1):158–62.
Pandharipande PP, Girard TD, Jackson JC, Morandi A, Thompson JL, Pun BT, et al. BRAIN-ICU Study Investigators. Long-term cognitive impairment after critical illness. N Engl J Med. 2013;369(14):1306–16.
BEBIS. Ebispro for Windows, Stuttgart, Germany; Turkish version BEBIS; Data Bases: Bundeslebenmittelschlüssell, 11.3 and other sources; 2004.
Harris JA, Benedict FG. A biometric study of human basal metabolism. Proc Natl Acad Sci USA. 1918;4(12):370–3.
Singer P, Blaser AR, Berger MM, Alhazzani W, Calder PC, Casaer MP, et al. ESPEN guideline on clinical nutrition in the intensive care unit. Clin Nutr. 2019;38(1):48–79.
Heyland DK, Day A, Clarke GJ, Hough CT, Files DC, Mourtzakis M, et al. Nutrition and Exercise in Critical Illness Trial (NEXIS Trial): a protocol of a multicentred, randomised controlled trial of combined cycle ergometry and amino acid supplementation commenced early during critical illness. BMJ Open. 2019;9(7):e027893.
Puthucheary ZA, Rawal J, McPhail M, Connolly B, Ratnayake G, Chan P, et al. Acute skeletal muscle wasting in critical illness. JAMA. 2013;310(15):1591–600. Erratum in: JAMA. 2014;311(6):62.
Puthucheary ZA, McNelly AS, Rawal J, Connolly B, Sidhu PS, Rowlerson A, et al. Rectus femoris cross-sectional area and muscle layer thickness: comparative markers of muscle wasting and weakness. Am J Respir Crit Care Med. 2017;195(1):136–8.
Lee ZY, Ong SP, Ng CC, Yap CS, Engkasan JP, Barakatun-Nisak MY, et al. Association between ultrasound quadriceps muscle status with premorbid functional status and 60-day mortality in mechanically ventilated critically ill patient: A single-center prospective observational study. Clin Nutr. 2021;40(3):1338–47.
Kangalgil M, Ulusoy H, Turan S, Oncu K. Association between skeletal muscle changes, anthropometric measurements, and clinical outcomes in critically ill trauma and surgical patients: A prospective observational study. Nutr Clin Pract. 2022;37(6):1326–35.
Mayer KP, Thompson Bastin ML, Montgomery-Yates AA, Pastva AM, Dupont-Versteegden EE, Parry SM, et al. Acute skeletal muscle wasting and dysfunction predict physical disability at hospital discharge in patients with critical illness. Crit Care. 2020;24(1):637.
Faul F, Erdfelder E, Lang AG, Buchner A. G*Power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–91.
Joskova V, Patkova A, Havel E, Najpaverova S, Uramova D, Kovarik M, et al. Critical evaluation of muscle mass loss as a prognostic marker of morbidity in critically ill patients and methods for its determination. J Rehabil Med. 2018;50(8):696–704.
Palakshappa JA, Reilly JP, Schweickert WD, Anderson BJ, Khoury V, Shashaty MG, et al. Quantitative peripheral muscle ultrasound in sepsis: muscle area superior to thickness. J Crit Care. 2018;47:324–30.
Hrdy O, Vrbica K, Kovar M, Korbicka T, Stepanova R, Gal R. Incidence of muscle wasting in the critically ill: a prospective observational cohort study. Sci Rep. 2023;13(1):742.
Yang T, Li Z, Jiang L, Wang Y, Xi X. Risk factors for intensive care unit-acquired weakness: a systematic review and meta-analysis. Acta Neurol Scand. 2018;138(2):104–14.
Tortuyaux R, Davion JB, Jourdain M. Intensive care unit-acquired weakness: questions the clinician should ask. Rev Neurol (Paris). 2022;178(1–2):84–92.
Bellaver P, Schaeffer AF, Leitao CB, Rech TH, Nedel WL. Association between neuromuscular blocking agents and the development of intensive care unit-acquired weakness (ICU-AW): a systematic review with meta-analysis and trial sequential analysis. Anaesth Crit Care Pain Med. 2023;42(3):101202.
Wang L, Long DY. Significant risk factors for intensive care unit-acquired weakness: a processing strategy based on repeated machine learning. World J Clin Cases. 2024;12(7):1235–42.
Fetterplace K, Deane AM, Tierney A, Beach LJ, Knight LD, Presneill J, et al. Targeted full energy and protein delivery in critically ill patients: a pilot randomized controlled trial (FEED trial). JPEN J Parenter Enteral Nutr. 2018;42(8):1252–62.
Ferrie S, Allman-Farinelli M, Daley M, Smith K. Protein requirements in the critically ill: a randomized controlled trial using parenteral nutrition. JPEN J Parenter Enteral Nutr. 2016;40(6):795–805.
Dresen E, Weißbrich C, Fimmers R, Putensen C, Stehle P. Medical high-protein nutrition therapy and loss of muscle mass in adult ICU patients: a randomized controlled trial. Clin Nutr. 2021;40(4):1562–70.
Kangalgil M, Küçük AO, Ulusoy H, Özçelik AÖ. Nutrition determinants of acute skeletal muscle loss in critically ill patients: a prospective observational cohort study. Nutr Clin Pract. 2024;39(3):579–88.
Nakanishi N, Matsushima S, Tatsuno J, Liu K, Tamura T, Yonekura H, et al. Impact of energy and protein delivery to critically ill patients: A systematic review and meta-analysis of randomized controlled trials. Nutrients. 2022;14(22):4849.
Lee ZY, Yap CS, Hasan MS, Engkasan JP, Barakatun-Nisak MY, Day AG, et al. The effect of higher versus lower protein delivery in critically ill patients: a systematic review and meta-analysis of randomized controlled trials. Crit Care. 2021;25(1):260.
Gungor L, Arsava EM, Guler A, Togay Isikay C, Aykac O, Batur Caglayan HZ, et al. MASS investigators. Determinants of in-hospital muscle loss in acute ischemic stroke—results of the Muscle Assessment in Stroke Study (MASS). Clin Nutr. 2023;42(3):431–9.
Zhang XM, Chen D, Xie XH, Zhang JE, Zeng Y, Cheng AS. Sarcopenia as a predictor of mortality among the critically ill in an intensive care unit: a systematic review and meta-analysis. BMC Geriatr. 2021;21(1):339.
Jiang T, Lin T, Shu X, Song Q, Dai M, Zhao Y, et al. Prevalence and prognostic value of preexisting sarcopenia in patients with mechanical ventilation: a systematic review and meta-analysis. Crit Care. 2022;26(1):140.
Sabatino A, Maggiore U, Regolisti G, Rossi GM, Di Mario F, Gentile M, et al. Ultrasound for non-invasive assessment and monitoring of quadriceps muscle thickness in critically ill patients with acute kidney injury. Front Nutr. 2021;8:622823.
Witteveen E, Sommers J, Wieske L, Doorduin J, van Alfen N, Schultz MJ, et al. Diagnostic accuracy of quantitative neuromuscular ultrasound for the diagnosis of intensive care unit-acquired weakness: a cross-sectional observational study. Ann Intensive Care. 2017;7(1):40.
Klawitter F, Walter U, Axer H, Patejdl R, Ehler J. Neuromuscular ultrasound in intensive care unit-acquired weakness: current state and future directions. Medicina (Kaunas). 2023;59(5):844.
Funding
Open access funding provided by the Scientific and Technological Research Council of Türkiye (TÜBİTAK). This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MK and HU conceived and designed the study. MK and SA acquired clinical data. MK and HU performed the statistical analyses. MK drafted the manuscript. HU provided critical revisions to the manuscript. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no conflicts of interest.
Ethical approval/informed consent
This study was approved by the Ethics Committee of Karadeniz Technical University. Written informed consent was obtained from all participants or their relatives.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kangalgil, M., Ulusoy, H. & Ayaz, S. Acute Skeletal Muscle Wasting is Associated with Prolonged Hospital Stay in Critical Illness with Brain Injury. Neurocrit Care (2024). https://doi.org/10.1007/s12028-024-02017-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s12028-024-02017-y