Abstract
Background
Transcranial Doppler (TCD) noninvasively measures cerebral blood flow (CBF) velocity and is a well-studied method to monitor cerebral autoregulation (CA). Near-infrared spectroscopy (NIRS) has emerged as a promising noninvasive method to determine CA continuously by using regional cerebral oxygen saturation (rSO2) as a surrogate for CBF. Little is known about its accuracy to determine CA in patients with intracranial lesions. The purpose of this study was to assess the accuracy of rSO2-based CA monitoring with TCD methods in comatose patients with acute neurological injury.
Methods
Thirty-three comatose patients were monitored at the bedside to measure CA using both TCD and NIRS. Patients were monitored daily for up to three days from coma onset. The cerebral oximetry index (COx) was calculated as the moving correlation between the slow waves of rSO2 and mean arterial pressure (MAP). The mean velocity index (Mx) was calculated as a similar coefficient between slow waves of TCD-measured CBF velocity and MAP. Optimal blood pressure was defined as the MAP with the lowest Mx and COx. Averaged Mx and COx as well as optimal MAP, based on both Mx and COx, were compared using Pearson’s correlation. Bias analysis was performed between these same CA metrics.
Results
The median duration of monitoring was 60 min (interquartile range [IQR] 48–78). There was a moderate correlation between the averaged values of COx and Mx (R = 0.40, p = 0.005). Similarly, there was a strong correlation between optimal MAP calculated for COx and Mx (R = 0.87, p < 0.001). Bland–Altman analysis showed moderate agreement with bias (±standard deviation) of −0.107 (±0.191) for COx versus Mx and good agreement with bias of 1.90 (±7.94) for optimal MAP determined by COx versus Mx.
Conclusions
Monitoring CA with NIRS-derived COx is correlated and had good agreement with previously validated TCD-based method. These results suggest that COx may be an acceptable substitute for Mx monitoring in patients with acute intracranial injury.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Cerebral autoregulation (CA) is considered one of the most important physiological mechanisms to maintain a constant cerebral blood flow (CBF) and prevent hypo- or hyper-perfusion, despite changes in arterial blood pressure (ABP) [1]. Transcranial Doppler (TCD) is frequently used in critical care settings to assess cerebral hemodynamics [1]. The mean velocity index (Mx) is the TCD-based measurement used in CA monitoring, by correlating cerebral blood flow velocity (CBFV) of the middle cerebral artery (MCA) either with the mean arterial pressure (MAP) or with cerebral perfusion pressure (CPP) [2, 3]. However, TCD has many limitations including the need for technical training, high susceptibility to motion artifact, and lack of temporal insonating windows in 5–10% of patients [4].
Near-infrared spectroscopy (NIRS) is a noninvasive device that measures regional cerebral oxygen saturation (rSO2), which can be used as a surrogate of CBF to measure CA [5, 6]. The cerebral oximetry index (COx) is calculated by the moving correlation between the slow waves of rSO2 and MAP [6]. rSO2 is a measure of the balance between cerebral oxygen delivery (to which CBF is a major contributor) and utilization (associated with cerebral metabolic rate for oxygen) [7]. Unlike TCD, NIRS requires minimal operator intervention, provides a continuous output, and is not subject to motion artifact [8,9,10,11]. Brady and colleagues reported a significant correlation and agreement between TCD-based Mx and COx in adult patients undergoing cardiopulmonary bypass [5]. CA monitoring in patients with acute neurological injury using NIRS-directed CA monitoring has not been compared with TCD-based Mx. The present study aimed to assess the correlation between the TCD-based Mx and the NIRS-based COx in patients with acute neurological injury causing coma and to compare the optimal MAP calculations derived from both technologies.
Methodology
Type of Study
A prospective observational cohort study was conducted in the neurocritical care unit (NCCU) at the Johns Hopkins Hospital from March 2013 to December 2015. Comatose patients from different etiologies underwent CA monitoring simultaneously using NIRS and TCD within the first 12–48 h from coma onset. All procedures received the approval of the Johns Hopkins Medical Institutions Review Board. Written informed consent was not required because of the low risk and conventional nature of the procedures in this patient population.
Patients
Coma status was defined as a Glasgow Coma Scale (GCS) score ≤8. Exclusion criteria included unresponsiveness not primarily due to coma (i.e., aphasia, sedation, or residual anesthesia). All patients had direct ABP monitoring in place using a catheter in the radial or femoral artery. The pressure transducers were leveled at the heart. Some patients required mechanical lung ventilation. Authors extracted sociodemographic characteristics (i.e., age, race, and gender), clinical characteristics, and coma etiology from the medical record. All data were placed in a database devoid of protected health information. We excluded patients who were younger than 18 years old and who had withdrawal of active treatment in the first 48 h.
Autoregulation Monitoring
Patients were monitored daily for up to 3 days after the enrollment. The neuromonitoring was interrupted or terminated if the patient’s arterial line was removed, and the patient was taken to the operating room or the radiology suite for brain imaging, or death occurred.
NIRS-Based Autoregulation Monitoring
The patients were connected to a NIRS INVOS™ 5100 (cerebral/somatic oximetry monitor, Covidien, Boulder, CO) using self-adhesive sensors attached to each side of the forehead. The sites of NIRS monitoring were not different in patients with frontal lesions. Analog ABP signals were obtained from the hemodynamic monitor and were processed using a DT9800 data acquisition module (Data Translation Inc, Marlboro, MA). These signals and the raw digital NIRS signals were analyzed using ICM+ software (University of Cambridge, Cambridge, UK), as described previously [9, 12, 13]. ABP and NIRS signals were filtered to focus on low-frequency slow vasogenic waves, which have been shown to be a valid objective measure of CA [9, 12, 13]. Specifically, slow, synchronized waves of periods from 20 s to 2 min, as seen in cerebral blood velocity, and traditionally used for the assessment of cerebral dynamic autoregulation can also be observed in NIRS [7]. Slow fluctuations in cerebral oximetry as detected by NIRS coincide with intracranial pressure (ICP) slow waves and increased during periods of exhausted cerebrospinal compensatory reserve. This observation led to the conclusion that NIRS may be used as a noninvasive marker of increased ICP slow waves (and therefore reduced CSF compensatory reserve) [14]. The signals were filtered as non-overlapping 10-s mean values that were time-integrated, which is equivalent to having a moving average filter with a 10-s time window and resampling at 0.1 Hz, eliminating high-frequency noise resulting from respiration and pulse waveforms, while allowing detection of oscillations and transients occurring <0.05 Hz [9]. A continuous, moving Pearson correlation coefficient between changes in MAP and rSO2 was calculated rendering the variable COx. Functional autoregulation is indicated when COx approaches zero (i.e., no correlation between rScO2 and ABP), while COx approaching 1 indicates impaired autoregulation. Averaged COx within each 10-s window was collected as 30 data points to monitor each COx in a 300-s window. Right and left sides were monitored on all patients, and an average COx from both sides was calculated for correlation analysis.
TCD-Based Autoregulation Monitoring
Right and left MCA CBFV was measured with TCD monitoring (Doppler Box; DWL, Compumedics, Charlotte, NC, USA) using two 2.5-MHz transducers fitted on a headband. The depth of insonation was varied until representative spectral artery flow was obtained typically between 35 and 55 mm. The signals were also filtered to remove noise from Doppler signals. A linear (Pearson’s) correlation coefficient performed between 30 paired samples of 10 s averages of MAP and CBFV yields a right and left Mx. We excluded recordings with CBFV less than 25 cm/s as we assumed those measurements did not reflect the MCA CBFV (lowest expected limit 32 cm/s) [15].
Calculation of Optimal MAP
The right and left COx and Mx measurements from the onset of monitoring were binned into 5-mmHg increments of MAP for analysis. Optimal MAP for each side was defined as the MAP with the best autoregulation (i.e., MAP with the lowest COx and Mx) [10, 16, 17]. The right and left optimal MAP were averaged to define the individual patient optimal MAP, when there was only one-side recording that was taken as the individual optimal MAP.
Statistical Analysis
Patient descriptive characteristics and categorical data were presented as absolute frequencies and percentages. Quantitative data were presented as mean ± standard deviation (SD) or as medians plus interquartile ranges (IQR), where appropriate. Non-normality distribution of the data was observed using Shapiro–Wilk test; therefore, the data were analyzed using nonparametric techniques. According to the normal distribution of the data, Pearson (for normal distribution) or Spearman’s (for non-normal distribution) correlation was used for determining the relationship between the NIRS-based index (i.e., COx) and the TCD-based measurements (Mx). Bland–Altman bias analysis was used to compare the differences in COx and Mx versus the average of these values [18]. Right and left recording data were averaged for correlation analysis. ANOVA test and Bonferroni correction were used to determine the statistical significance between nonparametric variables. Mann–Whitney U tests or t tests were used to compare normally distributed quantitative data between subgroups. A p value of <0.05 was considered significant. All analysis was performed using STATA version 13.0 (Stata Corp, College Station, TX).
Results
Thirty-three comatose patients were included. The median number of one-hour recordings per patient was 2 (IQR 1–3). There were a total of 67 recordings. Only 42 recordings out of 67 were adequate for calculating optimal MAP, and the analyses were performed using those recordings. The reasons for exclusion were: lack of temporal window (three recordings), poor patient cooperation causing TCD probe instability (five recordings), not enough recorded time to calculate optimal MAP (seven recordings), inability to calculate optimal MAP due to impaired autoregulation during the full duration of monitoring (seven recordings), and CBFV less than 25 cm/s (two recordings). NIRS was successfully monitored in all patients. The mean age (±SD) was 59.9 ± 15.3 years. The sample included predominantly women (63.6%), and the most frequent coma etiology was intracerebral hemorrhage (ICH) (39.4%). Baseline clinical characteristics of the patients enrolled in this study are listed in Table 1. Both left- and right-sided measurements of TCD monitoring were averaged in 52.4% (22/42), while the remainder of the recordings utilized unilateral data (47.6%, 20/42). Lack of contralateral side data was due to TCD probe instability, patients with hemicraniectomy or invasive ICP monitors with dressings covering one frontal lobe. The median duration of monitoring per recording was 60 min (IQR 41–76 min). The median MAP during monitoring was 88.8 mmHg (IQR 82.7–105.3 mmHg), the median rSO2 was 58.2 (48.3–65.4), and the median MCA CBFV was 44.4 cm/s (35.2–51.6 cm/s).
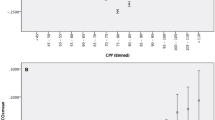
The Pearson correlation between COx and Mx was R = 0.40 (Fig. 1a; p = 0.005). Paired within-subject bias was −0.106 for the correlation (Fig. 1b; 95% CI prediction interval for the difference between both indices = −0.48 to 0.27). The median optimal MAP calculated by COx was 85 mmHg (IQR 80–107.5 mmHg). The median optimal MAP by Mx was 90 mmHg (IQR 80–100 mmHg). There was a strong correlation between these two measures (Pearson R = 0.87, p < 0.001, Fig. 2a). The paired within-subject bias was 1.9 for the latter correlation (Fig. 1b; 95% CI prediction interval for the difference between both indices = −13.7 to 17.5).
The results from this study population do not take into account lesion asymmetry and the potential differential impact of hematomas, subarachnoid blood, or cerebral edema on changes in cerebral oxygenation and CBF. Comparison of left and right sides where available (40 recordings on the left side and 23 on the right side) yielded a correlation coefficient of R = 0.47 (p = 0.002) between left Mx vs left COx, and R = 0.46 (p = 0.027) between the right Mx and right COx.
Impact of Frontal Lesions on Mx Versus COx Correlation
There were six patients who had frontal lesions. Comparison of left and right Mx and COx after removal of these six patients did improve the side-to-side correlation coefficients. After excluding patients with frontal lesions (in total there were 36 recordings on the left side and 19 on the right side), we found a correlation coefficient of R = 0.502 (p = 0.002) between left Mx versus left COx, and R = 0.609 (p = 0.006) between the right Mx and right COx.
Discussion
Our data show that in patients with acute neurological injury the CA indices COx and Mx demonstrated moderate correlation and agreement. Furthermore, we found a strong correlation and agreement between the optimal MAP calculated by COx and Mx. These results demonstrate that NIRS-derived COx is an acceptable substitute for TCD-derived Mx monitoring in patients with intracranial injury for CA monitoring and the calculation of optimal MAP.
Our study provides evidence for the feasibility of stand-alone bedside CA monitoring with cerebral oximetry in general populations of comatose patients with acute brain injury. Coma is a frequent disorder of consciousness and awareness in the intensive care unit [19], and most patients with acute coma are at increased risk of perturbations in cerebral perfusion due to increased vascular permeability and reduced CBF associated with neuronal inflammation and tissue damage [20]. Abnormal CBF may be a significant factor in the pathogenesis and complications of coma. Therefore, bedside CA monitoring with COx and calculation of optimal MAP may have an important utilization in the critical care setting.
Our findings of good correlation and agreement between the two CA monitoring techniques are in agreement with other studies that examined different populations (i.e., subarachnoid hemorrhage [SAH], sepsis, migraine, and cardiac surgery), utilizing two types of NIRS for calculation of rSO2 (i.e., INVOS™ 5100 [Covidien, Boulder, CO] vs. NIRO 300 [Hamamatsu Photonics, Hamamatsu city, Japan]) [5, 7, 11, 13, 21,22,23,24,25]. These two NIRS devices use different measurement techniques for measuring regional tissue oxygen saturation and different algorithms for its calculation. The INVOS uses two wavelengths of near-infrared light (730 and 810 nm) and measures the ratio of oxyhemoglobin (HbO2) to total hemoglobin (HbT), yielding rSO2 (%). The NIRO monitor uses four wavelengths of near-infrared right (775, 825, 850, and 904 nm) and measures the tissue oxygen index (TOI) (%), which is also the ratio of HbO2 to HbT [26]. A study comparing these two NIRS devices found only moderate agreement between TOI and rSO2, r = 0.58, p < 0.01 [26]. Thus, the advantages of this technology include that it has been validated in several different populations and has shown consistent results. The disadvantages are that the calculation of regional tissue oxygen saturation may vary between devices and rSO2 itself is dependent on other physiological variables as detailed below.
Our results extend prior investigations that have validated COx in laboratory and clinical investigations. Table 2 shows a summary of these studies assessing the correlation between cerebral oximetry and TCD-based measurements. Brady and colleagues [5] proposed that monitoring COx in a vascular territory distinct from the MCA, where Mx was calculated, might be an explanation for why the correlation between COx and Mx, while significant, is not as strong as the correlations between other CA indices. The use of NIRS as a surrogate of CBF for CA monitoring is based on assumptions that other determinants of rSO2 (i.e., tissue oxygen diffusivity, cerebral metabolic rate of oxygen, and temperature) are relatively stable over the low frequencies of vasoreactivity that mediate CA. Other physiological variables that alter brain oxygen supply and demand may affect rSO2. These include cardiac output, pulmonary function, systemic hypoxemia, acid–base status, and partial pressure of carbon dioxide, which affect not only the hemoglobin saturation for a given partial pressure of oxygen but also CBF [27]. These variables may confound the relationship between rSO2 and changes in MAP as in during hyperventilation for cerebral herniation, or in during therapeutic manipulation of blood pressure or cardiac output for SAH. Thus, the differences in technologies and local changes in physiology may also explain the moderate correlation between COx and Mx. Although there is heterogeneity among the studied populations in the studies described in Table 2, five out of six studies confirmed a significant relationship between cerebral oximetry-based CA monitoring and other TCD-based measurements (i.e., CBFV, Mx based on ABP, Systolic index, and Mx-CPP). Differences noted between the cardiac surgery studies and other populations may be due to lower rSO2 values often seen after induction of general anesthesia in cardiac bypass patients. Procedure-related factors (e.g., unilateral and bilateral antegrade cerebral perfusion during surgery of the aorta) may also affect oxygenation/perfusion of each hemisphere in a different way [27]. Experimental studies in animals have also shown good agreement between COx and autoregulatory indices using hemodynamic conditions [6, 28].
The results of this study represent new observations demonstrating good agreement between two methods of CA monitoring in a diverse population with acute coma and large intracranial lesions (ICH, SAH, traumatic brain injury with contusions, extradural collections). Discordance between these measurements may also occur because of frontal or MCA lesions, such as frontal or temporal hemorrhages altering the local hemodynamics, or causing vessel stenosis. Our sample size is too small to comment on these differences; however, when we removed the recordings with frontal lesions from the analysis (six patients), the correlation coefficient improved from R = 0.4 to 0.6, suggesting that frontal lesions may have altered NIRS calculations. Discordance may also occur because changes in cerebral oxygenation are much less pronounced than associated blood flow changes, as previously described by Reinhard et al. [29]. Lastly, both COx and Mx based on ABP do not take into account ICP measurements, and it has been demonstrated that there may not be a strong correlation between Mx based on MAP and the most validated index of CA, pressure reactivity index in patients with sustained intracranial hypertension of above 30 mmHg [12].
This study has a number of limitations. The sample size was small, but was comparable to other similar studies (Table 2). Another limitation is the presence of heterogeneous lesions in a population with acute coma. The presence of intracranial hematoma, cerebral edema, and subarachnoid blood are all potential confounders of the NIRS technique and may invalidate some of the assumptions upon which NIRS algorithms are based. However, it was our intention to determine the potential role of NIRS in a general population, for the purpose of understanding whether NIRS could be used reliably in coma of various etiologies. It is not known whether targeting NIRS to the side of pathology compared to bilateral monitoring improves the prediction of optimal MAP or prognostic utility. Further analysis of NIRS by coma etiology, lesion location, and underlying pathophysiology (vasospasm, edema, ischemia, etc.) will require larger populations. Known limitations of CA studies utilizing TCD are the need for frequent transducer repositioning and the inability to obtain a transcranial “window” in some patients. This latter limitation led to the exclusion of ten patients. The calculation of cerebral autoregulation using NIRS requires the ICM plus software. This software must be purchased from the Cambridge group with an expensive license cost [30]. The use of the software may be time-consuming due to technical challenges. The aim of this study was to determine the correlation between optimal MAP measured by NIRS and TCD. Therefore, the included sample of patients is limited to those with intact autoregulation, which is a prerequisite to calculate optimal MAP. We did not study how measurement of impaired autoregulation correlated between these two methods. This study is methodological in terms of assessing CA, although treatment options for the injured brain go beyond the concept of CA. Finally, monitoring CA using these methods relies on spontaneous fluctuations in MAP. The absence of such fluctuations in some patients or a MAP that never crosses the autoregulation threshold may yield low COx values.
Conclusions
Monitoring CA with NIRS-based COx exhibited moderate but significant correlation with previously validated TCD-based methods. These results suggest that NIRS-derived COx may be an acceptable substitute for Mx monitoring of patients with acute neurological injury.
References
Aaslid R, Lindegaard KF, Sorteberg W, Nornes H. Cerebral autoregulation dynamics in humans. Stroke. 1989;20:45–52.
Newell DW, Aaslid R. Transcranial Doppler: clinical and experimental uses. Cerebrovasc Brain Metab Rev. 1992;4:122–43.
Aries MJ, Elting JW, De Keyser J, Kremer BP, Vroomen PC. Cerebral autoregulation in stroke: a review of transcranial Doppler studies. Stroke. 2010;41:2697–704.
Bazan R, Braga GP, Luvizutto GJ, Hueb JC, Hokama NK, Zanati Bazan SG, et al. Evaluation of the temporal acoustic window for transcranial Doppler in a multi-ethnic population in Brazil. Ultrasound Med Biol. 2015;41:2131–4.
Brady K, Joshi B, Zweifel C, Smielewski P, Czosnyka M, Easley RB, et al. Real-time continuous monitoring of cerebral blood flow autoregulation using near-infrared spectroscopy in patients undergoing cardiopulmonary bypass. Stroke. 2010;41:1951–6.
Brady KM, Lee JK, Kibler KK, Smielewski P, Czosnyka M, Easley RB, et al. Continuous time-domain analysis of cerebrovascular autoregulation using near-infrared spectroscopy. Stroke. 2007;38:2818–25.
Steiner LA, Pfister D, Strebel SP, Radolovich D, Smielewski P, Czosnyka M. Near-infrared spectroscopy can monitor dynamic cerebral autoregulation in adults. Neurocrit Care. 2009;10:122–8.
Howlett JA, Northington FJ, Gilmore MM, Tekes A, Huisman TA, Parkinson C, et al. Cerebrovascular autoregulation and neurologic injury in neonatal hypoxic-ischemic encephalopathy. Pediatr Res. 2013;74:525–35.
Ono M, Zheng Y, Joshi B, Sigl JC, Hogue CW. Validation of a stand-alone near-infrared spectroscopy system for monitoring cerebral autoregulation during cardiac surgery. Anesth Analg. 2013;116:198–204.
Hori D, Hogue C, Adachi H, Max L, Price J, Sciortino C, et al. Perioperative optimal blood pressure as determined by ultrasound tagged near infrared spectroscopy and its association with postoperative acute kidney injury in cardiac surgery patients. Interact Cardiovasc Thorac Surg. 2016;22(4):445–51.
Wang X, Ji B, Yang B, Liu G, Miao N, Yang J, et al. Real-time continuous neuromonitoring combines transcranial cerebral Doppler with near-infrared spectroscopy cerebral oxygen saturation during total aortic arch replacement procedure: a pilot study. ASAIO J. 2012;58:122–6.
Budohoski KP, Czosnyka M, de Riva N, Smielewski P, Pickard JD, Menon DK, et al. The relationship between cerebral blood flow autoregulation and cerebrovascular pressure reactivity after traumatic brain injury. Neurosurgery. 2012;71:652–60 (discussion 660-651).
Budohoski KP, Czosnyka M, Smielewski P, Varsos GV, Kasprowicz M, Brady KM, et al. Cerebral autoregulation after subarachnoid hemorrhage: comparison of three methods. J Cereb Blood Flow Metab. 2013;33:449–56.
Weerakkody RA, Czosnyka M, Zweifel C, Castellani G, Smielewski P, Keong N, et al. Slow vasogenic fluctuations of intracranial pressure and cerebral near infrared spectroscopy—an observational study. Acta Neurochir. 2010;152:1763–9.
Lindegaard KF, Lundar T, Wiberg J, Sjoberg D, Aaslid R, Nornes H. Variations in middle cerebral artery blood flow investigated with noninvasive transcranial blood velocity measurements. Stroke. 1987;18:1025–30.
Hori D, Ono M, Rappold TE, Conte JV, Shah AS, Cameron DE, et al. Hypotension after cardiac operations based on autoregulation monitoring leads to brain cellular injury. Ann Thorac Surg. 2015;100:487–93.
Aries MJ, Czosnyka M, Budohoski KP, Steiner LA, Lavinio A, Kolias AG, et al. Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med. 2012;40:2456–63.
Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–10.
Stevens RD, Bhardwaj A. Approach to the comatose patient. Crit Care Med. 2006;34:31–41.
Hughes CG, Patel MB, Pandharipande PP. Pathophysiology of acute brain dysfunction: what’s the cause of all this confusion? Curr Opin Crit Care. 2012;18:518–26.
Tsuji M, Saul JP, du Plessis A, Eichenwald E, Sobh J, Crocker R, et al. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics. 2000;106:625–32.
Olsen KS, Svendsen LB, Larsen FS. Validation of transcranial near-infrared spectroscopy for evaluation of cerebral blood flow autoregulation. J Neurosurg Anesthesiol. 1996;8:280–5.
Vernieri F, Tibuzzi F, Pasqualetti P, Altamura C, Palazzo P, Rossini PM, et al. Increased cerebral vasomotor reactivity in migraine with aura: an autoregulation disorder? A transcranial Doppler and near-infrared spectroscopy study. Cephalalgia. 2008;28:689–95.
Zweifel C, Castellani G, Czosnyka M, Carrera E, Brady KM, Kirkpatrick PJ, et al. Continuous assessment of cerebral autoregulation with near-infrared spectroscopy in adults after subarachnoid hemorrhage. Stroke. 2010;41:1963–8.
Berg RM, Plovsing RR. Near-infrared spectroscopy versus transcranial Doppler ultrasound for assessing dynamic cerebral autoregulation by transfer function analysis in sepsis. Scand J Clin Lab Invest. 2016;76:88–91.
Yoshitani K, Kawaguchi M, Tatsumi K, Kitaguchi K, Furuya H. A comparison of the INVOS 4100 and the NIRO 300 near-infrared spectrophotometers. Anesth Analg. 2002;94:586–90.
Vretzakis G, Georgopoulou S, Stamoulis K, Stamatiou G, Tsakiridis K, Zarogoulidis P, et al. Cerebral oximetry in cardiac anesthesia. J Thorac Dis. 2014;6(Suppl 1):S60–9.
Tsuji M, duPlessis A, Taylor G, Crocker R, Volpe JJ. Near infrared spectroscopy detects cerebral ischemia during hypotension in piglets. Pediatr Res. 1998;44:591–5.
Reinhard M, Wehrle-Wieland E, Grabiak D, Roth M, Guschlbauer B, Timmer J, et al. Oscillatory cerebral hemodynamics—the macro- vs. Microvascular level. J Neurol Sci. 2006;250:103–9.
Smielewski PC, Czosnyka M. https://www.enterprise.cam.ac.uk/opportunities/icm-software-for-brain-monitoring-in-neurological-intensive-care-research/. 2016.
Funding
Dr. Hogue is the PI on an NIH-sponsored clinical study (R01 HL 92259). Dr. Rivera Lara is the PI on an American Academy of Neurology/American Brain Foundation and grant from Medtronic/Covidien, Dublin, IR.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Hogue receives research funding from Medtronic/Covidien, Dublin, IR, and he serves as a consultant to Medtronic/Covidien and Ornim Medical, Inc., Foxborough, MA.
Rights and permissions
About this article
Cite this article
Rivera-Lara, L., Geocadin, R., Zorrilla-Vaca, A. et al. Validation of Near-Infrared Spectroscopy for Monitoring Cerebral Autoregulation in Comatose Patients. Neurocrit Care 27, 362–369 (2017). https://doi.org/10.1007/s12028-017-0421-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-017-0421-8