Abstract
Objective
Posterior fossa stroke is unique in its presentation and outcomes, and mechanical ventilation is commonly used in the management of these patients. We aimed to identify predictors of extubation success in patients with posterior fossa stroke, who require mechanical ventilation.
Design
We included consecutive adult patients admitted to the neurosciences ICU from January 2003 to December 2012. Extubation failure was defined as re-intubation within 7 days of extubation. A modified Rankin Scale score of 0–3 was considered a good outcome.
Measurements and Main Results
We identified 150 patients with mean age of 65 ± 15.7 years with posterior fossa strokes; 77 (51 %) were hemorrhagic, and 73 (49 %) were ischemic. The most common reason for intubation was depressed consciousness (54 %). Fifty-two (35 %) were successfully extubated, 18 (12 %) failed extubation, 17 (11 %) patients had tracheostomy without attempted extubation, and 63 (42 %) were transitioned to palliative care prior to extubation. In the logistic regression analysis, controlling for transition to palliative care, Glasgow Coma Score (GCS) score >6 at the time of intubation (p = 0.020), mechanical ventilation for less than 7 days (p = 0.004), and surgical evacuation of a hematoma (p = 0.058) were independently associated with successful extubation. The presence of cough, gag reflex, and absence of pneumonia/atelectasis were not associated with successful extubation. Success of extubation predicted a good outcome at hospital discharge.
Conclusions
In posterior fossa stroke patients with a GCS ≤ 6 at the time of intubation and who remain intubated for more than 1 week, extubation is less likely to be successful, and tracheostomy should be considered.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Posterior fossa strokes, both ischemic and hemorrhagic, are unique in their presentation as well as outcome. Mechanisms of secondary deterioration include compression of the brainstem and development of obstructive hydrocephalus due to cerebral edema and tissue shift. Outcomes are frequently poor because of direct involvement of the brainstem or compression of the brainstem by cerebral edema [1, 2]. Respiratory complications due to bulbar dysfunction and the need for mechanical ventilation contribute to the morbidity of these patients [3, 4]. Patients with posterior fossa strokes requiring mechanical ventilation are typically managed in a general or neurosciences intensive care unit (ICU). Little is known about the predictors of extubation failure or success in this unique population [5]. Clear differences exist between patients intubated for airway protection because of a decreased level of consciousness, patients intubated for airway protection despite preserved level of consciousness because of loss of protective lower brainstem reflexes (i.e., gag, cough, etc.) and those who require mechanical ventilation because of respiratory failure due to coexistent pulmonary disease (as seen after aspiration) [1].
Unnecessary prolongation of ventilatory support as well as failed extubation is associated with increased sedation and possibly higher mortality rates [6]. Accounting for varying definitions of extubation failure, the incidence varies from 10 to 20 % in mixed ICU populations [7, 8], and the reported mortality rate associated with extubation failure varies from 30 to 40 % [3]. Among the various factors responsible for failed extubations, lower level of consciousness and difficulty in clearing secretions are likely important in patients with posterior fossa stroke [1]. Qureshi et al. found that a Glasgow Coma Score (GCS) >7 at the time of intubation and the absence of brainstem deficits were predictive of extubation success in patients with infratentorial lesions, but that study was not restricted to stroke cases [9]. Also, the influence of goals of care on these predictive variables is not known. We sought to determine the predictors of extubation success specifically in posterior fossa stroke and taking into account the patient’s goals of care.
Materials and Methods
Standard Protocols Approvals and Patient Consents
The study was approved by the Mayo Clinic institutional review board. All included patients or their legally authorized representative had signed a general informed consent form allowing their medical records to be used for research purposes.
Study Design
This is a retrospective study of consecutive patients ≥18 years old admitted to the neurosciences ICU at Mayo Clinic, Rochester, MN from January 2003 through December 2012. We identified all patients with acute posterior fossa stroke (ischemic or hemorrhagic), who required endotracheal intubation and mechanical ventilation during this period.
Study Definitions
Stroke diagnosis was confirmed by neuroimaging including either computed tomography (CT) or magnetic resonance imaging (MRI) of the brain. Ischemic strokes were classified according to the categories of the Trial of Org 10172 in Acute Stroke Treatment (TOAST) trial [10]. Volume of hemorrhage was calculated from the imaging studies using the ABCD/2 method [11]. Tissue shift was defined as (1) distortion of the brainstem, quadrigeminal, ambient, or basal cisterns, (2) tonsillar herniation, or (3) 4th ventricular compression. Atelectasis was defined as radiological evidence of lobar or segmental collapse documented by a radiologist. Pneumonia was defined as new or progressive infiltrate as seen on a chest radiograph or computed tomography (CT) scan along with a high clinical suspicion of pneumonia, defined by at least one of the following: fever (>38 °C); leukopenia (<4000 white blood cells (WBC)/mm3) or leukocytosis (>12,000 WBC/mm3); and at least two of the following: (a) new onset purulent sputum, change in characteristics of sputum, increased respiratory secretions, or suctioning requirements; (b) new onset or worsening cough, dyspnea, or increased ventilation demand [12]. Good or favorable outcome was defined by a modified Rankin Score (mRS) of 0–3. Extubation was considered successful if the patient remained extubated for 7 days. Failed extubation was defined as reintubation within the 7-day period for any reason.
Exclusion Criteria
Patients were excluded if they had (1) simultaneous strokes involving territories other than the posterior fossa, (2) subarachnoid hemorrhage, (3) subdural hemorrhage, (4) chronic infarctions, (5) primary intraventricular hemorrhage, and (6) if they were extubated in the operating room immediately after decompression surgery or (7) had incomplete data.
Clinical Parameters and Investigations
Collected data included age, sex, associated comorbidities including hypertension (HTN), diabetes (DM), congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), chronic kidney disease (CKD), and stroke classification including ischemic or hemorrhagic. Details of the anatomic regions involved (cerebellar, midbrain, pontine, and medullary), tissue shift, surgical intervention, and cerebrospinal fluid (CSF) diversion via ventriculostomy were also gathered. Neuroimaging was interpreted by both a neuroradiologist and a critical care neurologist (SH), who were blinded to the outcome of extubation. The presence of hydrocephalus and tissue shift was recorded at the time of intubation and again on follow-up imaging within 8 h of extubation. We recorded indications for intubation, GCS at the time of intubation, and ventilator settings. The presence of respiratory complications including atelectasis, pneumonia, pulmonary edema, focal infiltrates, and frequencies of suctioning and consistencies of secretions was also documented. Cough and gag reflexes were tested by the ICU nurses every 3–4 h and prior to extubation. Cough to passage of suctioning catheter was graded as strong, moderate, weak, and absent. For analyses, strong, moderate and weak coughs were grouped together as cough present. Gag reflex was noted as present or absent. We gathered data on timing and outcome of extubation, interval to reintubation, and timing of tracheostomy when it was present. Transition to palliative care was also recorded. In order to ascertain the effect of successful extubations, we collected ICU and hospital lengths of stay as well as mRS score at hospital discharge and at 1 year following discharge.
The predominant mode of mechanical ventilation in the patients is either volume control or pressure control. We usually look into the following criteria before considering weaning: (1) resolution or improvement of congestive heart failure, pneumonia, or other conditions requiring intubation, the presence of adequate gas exchange and ventilation as indicated by a ratio of partial pressure of oxygen (PaO2) to the fraction of inspired oxygen (FiO2) above 200 with a positive end-expiratory pressure (PEEP) of less than 6 cm of water, PaCO2 of less than 45 torr, rapid shallow breathing index (RSBI) less than 105, absence of fever (temperature < 38 °C) and no sedative medications. (2) Neurological criteria required GCS of 8 or more, intracranial pressure of less than 15 cm water, and a cerebral perfusion pressure more than 60 mm Hg for patients with intracranial pressure monitoring. In addition to the above criteria, the neurointensivist would have to agree that the patient was in a stable condition and was ready for extubation.
The patients meeting the above criteria for weaning underwent 30 min of T-piece trial with no continuous positive airway pressure or spontaneous breathing trial with a minimal PEEP of 6 cm of water to evaluate readiness for extubation. The trial was discontinued if any of the following were noted: respiratory rate >35 breath/minute for at least 5 min; arterial saturation <90 % for 2 min; heart rate >140 bpm; sustained changes of heart rate of 20 % in either direction; systolic BP > 180 mm Hg or <90 mm Hg and a notable increase in agitation or diaphoresis.
All the patients were assessed for their ability to control their respiratory secretions by the neurointensivist and either the nurse or the respiratory therapist involved in the patient care. In particular, the frequency of suctioning, sputum quantity, and character, and the presence of cough were noted prior to extubation. The bedside nurse and a respiratory therapist assessed all patients after extubation for signs of respiratory distress every hour for 6–12 h. A routine blood gas was obtained within 30–60 min after extubation.
The patients who failed trial of extubation, in whom the underlying condition requiring intubation was not resolved, GCS remained static or became worse and those who had problems protecting the upper airway or had persistent secretions were considered for tracheostomy based on the discretion of the neurointensivist and the critical care physician.
Statistical Analyses
Descriptive summaries were reported as mean and standard deviation, median and interquartile range for continuous variables and frequencies, and as percentages for categorical variables. Associations between categorical variables were assessed using χ2 tests or Fisher’s exact test, and two sample t test or Mann–Whitney test were used to compare continuous variables, as applicable. Further analysis was performed using univariable and multivariable logistic regressions. Variables with p values <0.10 were considered as candidate variables for multivariable modeling (Hypertension, APACHE 3 score, SOFA score, intraventricular blood, surgical evacuation, ventriculostomy, cardio-embolic stroke, brainstem, pontine, medulla involvement, GCS > 6 at intubation, cough present, mechanical ventilation less than 7 days, and transition to palliative care). Associations between outcomes of interest and predictors were summarized as odds ratios (OR) and 95 % confidence intervals (CI). All tests were two sided, and p values ≤0.05 were considered statistically significant. Statistical analysis was performed using JMP 10.0.0 (SAS Institute Inc., Cary, NC).
The primary end point was success of extubation. Patients who were successfully extubated were compared with patients who either (1) failed an extubation attempt, (2) underwent tracheostomy prior to a trial of extubation or (3) were transitioned to palliative care before extubation or tracheostomy. A separate analysis was conducted to compare patients who were successfully extubated to those who failed extubation after excluding patients who underwent tracheostomy or were transitioned to palliative care prior to a trial of extubation.
Results
There were 1321 stroke patients requiring mechanical ventilation in the ICU during the study period, and 150 patients with posterior fossa stroke were included in the final analysis (Fig. 1). Clinical characteristics of the study population are shown in Table 1. The mean age of the patients was 65 ± 15.7 years, and 79 (53 %) were male. Seventy-three (49 %) were ischemic and 77 (51 %) were hemorrhagic in origin. The major reason for intubation was a depressed level of consciousness and inability to protect the airway in 90 (61.6 %) patients, followed by intubation prior to an emergent surgical procedure in 29 (19.9 %), respiratory distress in 10 (6.8 %), apnea/hypoventilation in 8 (5.5 %), hypoxia in 5 (3.4 %), seizures in 2(1.4 %) and pulseless ventricular tachycardia in 2 (1.4 %) patients. GCS ≤ 8 was observed in 89 (59 %) patients. Mean mechanical ventilation duration was 3.8 days (range 0–28 days), and 129 (86 %) patients were intubated for less than or equal to 7 days. Median ICU stay of the entire cohort was 5 days (IQR 2.5–11) and median hospital stay was 10 days (IQR 4–22).
We identified 52 (35 %) patients who were successfully extubated during the ICU admission. Sixty-three (42 %) patients were transitioned to palliative care prior to an extubation attempt. Tracheostomy was performed in 17 (11 %) patients prior to a trial of extubation and took place after a mean of 9.2 ± 7.4 (SD) days of mechanical ventilation. Extubation failure was observed in 18 (12 %) patients after a median of 3 (IQR 2–4) days from the day of first intubation. The main reasons for extubation failure in these patients were altered mental status in 5 (27.8 %), excessive secretions in 4 (22.2 %), airway protection failure in 3 (16.7 %), stridor in 3 (16.7 %) and apnea/hypoventilation in 3 (16.7 %) patients. There were no events of any self-extubation/accidental extubation. All the patients were re-intubated within 24 h of extubation, and none were related to pneumonia or atelectasis. Of these, five were successfully extubated at a median of 3 days from the first extubation failure, nine underwent tracheostomy, and four were transitioned to comfort care.
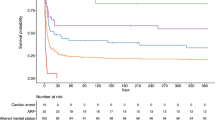
Factors associated with successful extubation are shown in Table 2. Age, gender, vascular comorbidities, stroke type, and prevalence of hydrocephalus were not significantly different between patients who were successfully extubated and those who were not (i.e., extubation failure, direct tracheostomy or transitioned to palliative care). Higher GCS at the time of intubation [median 9 (IQR 7–13) vs median 6 (IQR 4–9), p < 0.001] and surgical evacuation of a hematoma [17 (33.3 %) vs 6 (6.3 %), p < 0.001] were associated with successful extubation. GCS > 6 at the time of intubation was associated with successful extubation in 42 (82.4 %) vs 44 (47.8 %) patients, p < 0.001. Patients with cardio-embolic stroke were more likely to be extubated successfully as compared to other ischemic stroke subtypes [12 (46.2 %) vs 11 (23.4 %), p = 0.047]. Pontine involvement was inversely associated with success of extubation [12 (24 %) vs 37 (39.4 %), p = 0.059]. The frequency of respiratory complications including pneumonia, atelectasis, secretions, and frequency of suctioning were not significantly different between the two groups. A higher percentage of successfully extubated patients had a cough reflex [48 (97.9 %) vs 22 (78.6 %), p = 0.005] but the presence of a gag reflex did not influence the chances of extubation success [15 (79 %) vs 10 (55.6 %), p = 0.126]. Successfully extubated patients required significantly fewer days of intubation and mechanical ventilation (2 vs 3, p = 0.015). The ICU and hospital lengths of stay for patients who underwent successful extubation, extubation failure, early tracheostomy, tracheostomy after extubation failure, and palliative care are shown in Fig. 2.
In the logistic regression analysis (Table 3) controlling for transition to palliative care, GCS score >6 at the time of intubation (OR 3.13; 95 % CI 1.19–8.68), mechanical ventilation for less than 7 days (OR 7.45; 95 % CI 1.79–51.52), and surgical evacuation of a hematoma (OR 3.35, 95 % CI 0.96–13.7), were independently associated with successful extubation. When the logistic regression analysis was performed with a cutoff of GCS > 7, 8 or 9, the association was no longer present.
Successful extubation was associated with a good outcome as measured by mRS at discharge compared with patients who were not successfully extubated [14 (26.9 %) vs 3 (3.1 %), p = 0.001]; however, at 1 year the association was no longer significant [16 (51.6 %) vs 6 (40.0 %), p = 0.459] among the 46 (59.7 %) patients who survived the hospitalization and had a follow-up at 1 year. The mortality at discharge was significantly lower among the patients who were successfully extubated [1 (1.9 %) vs 73 (74.5 %), p < 0.001].
We also compared patients who were successfully extubated to those who failed extubation, after excluding those who underwent direct tracheostomy or were transitioned to palliative care without an extubation attempt (Table 4). All but one of the patients with failed extubation had a GCS score ≤6 at the time of intubation. Prolonged duration of intubation, and mechanical ventilation was inversely related to success of extubation [2 (IQR 1–3.8) vs 3.5 (IQR 2–6.3), p = 0.027]. Patients who failed extubation had longer ICU LOS (14.5 vs 6 days, p < 0.001), longer hospital LOS (23 vs 16 days, p < 0.18), more frequently developed pneumonia [11 (61.1 %) vs 13 (12.5 %), p < 0.007] and more often required tracheostomy [9 (50 %) vs 3 (5.8 %), p < 0.001] compared to successfully extubated patients. The long-term outcome of patients who were successfully extubated compared to those who failed extubation and required reintubation was not significantly different [16 (51.6 %) patients with good outcome vs 4 (57.1 %), p = 0.791]. The patients who underwent tracheostomy before extubation were mostly males [72.7 vs 47.2 %, p = 0.029] and had predominant pontine involvement [12 (54.6 %) vs 24 (28.2 %), p = 0.023]. They also required a longer duration of mechanical ventilation [6 (IQR 3–9.6) vs 2 (IQR 1–4), p < 0.001] and had a longer ICU [18.5 (IQR 14.5–32.3) vs 5 (IQR 3–9), p < 0.001] and hospital length of stay [30 (IQR 23–42.8) vs 11 (IQR 4–20.8), p < 0.001]. However, their hospital mortality [6 (27.3 %) vs 32 (35.9 %), p = 0.435] and the outcome at discharge [1 (4.6 %) vs 16 (18.2 %), p = 0.077] was not different. The comparison between posterior fossa hemorrhage and ischemic stroke groups is shown in Table 5.
Discussion
In this large cohort of posterior fossa stroke patients requiring mechanical ventilation, successful extubation was achieved in 35 % of all patients and 74.3 % of those in whom extubation was attempted. The main factors associated with successful extubation were a GCS > 6 at the time of intubation and mechanical ventilation ≤7 days. The presence of gag reflex, cough, and the absence of pneumonia and atelectasis were not associated with successful extubation.
Predicting extubation success continues to be a challenging clinical question facing clinicians every day. The success or failure of a spontaneous breathing trial is the current standard of care for prediction of extubation success in mechanically ventilated patients [14]. This may not be a reliable indicator in the posterior fossa stroke patients with brainstem involvement affecting airway protective mechanisms. We found that a GCS greater than 6 at the time of intubation was predictive of extubation success, likely reflecting the severity of the primary neurologic injury. There is only one other study evaluating the predictors of extubation success in infratentorial lesions which found a slightly higher GCS (>7) at the time of intubation to be predictive of extubation success [12]. Patients with GCS ≤ 7 at the time of intubation and brainstem deficits had a less than 10 % probability of successful extubation in that study [12]. Extubation success was observed in 33 % of the entire cohort. However that study was smaller (69 patients), included all posterior fossa lesions (not restricted to strokes), had tracheostomy as its main endpoint, and did not control for goals of care. We analyzed a larger and more homogeneous cohort consisting of only stroke patients and controlled for the goals of care in order to realize an accurate analysis of the predictors of extubation success in this population.
The risk factors for failed extubation vary depending upon the population studied. Coplin et al. found no correlation between reintubation and level of consciousness in a group of patients with traumatic brain injury, reporting an extubation success rate of >80 % in patients with GCS less than 8. They also found that 82 % of patients with absent or weak cough and 89 % with absent or weak gag reflex were successfully extubated [13]. However, in our cohort of successfully extubated patients, cough and gag reflex was present in 98 and 79 %, but it was not significant. In general critical care population, a GCS of 8 or more has been shown to be predictive of successful extubation [14]. None of these prior studies specifically evaluated patients with posterior fossa stroke.
Other reported risk factors for failed extubation and eventual reintubation are decreased cough strength, abundant bronchial secretions, and the absence of gag reflex [14–16]. In our cohort of posterior fossa stroke patients, we did not find any significant correlation between these factors and extubation success. The presence of cough reflex was more common in patients with successful extubation but the association was not strong. We relied on the number of tracheal suctioning sessions as a surrogate for the severity of the respiratory secretions. Whether these variables are truly not predictive of extubation outcome in patients with posterior fossa stroke should be confirmed in a prospective study with a standardized assessment of these reflexes and the quantity and quality of respiratory secretions.
The chance of successful extubation was not significantly associated with age or other comorbid conditions as evident by the lack of significance with the APACHE 3 and SOFA scores. Prolonged duration of intubation (>7 days) tended to have a greater risk of reintubation as well as eventual tracheostomy. Failed extubation was also associated with longer ICU length of stay, but hospital length of stay was not different between the two groups. As in the study by Qureshi et al., we found an association between successful extubation, fewer days of mechanical ventilation, and a decreased rate of tracheostomy [2, 17, 18].
We also compared the two cohorts of posterior fossa hemorrhage and infarctions and found that the infarction patients were older, had a less severe GCS on admission, and had a higher prevalence of CHF, compared to the hemorrhage group. They also had a longer duration of mechanical ventilation. However, the ICU and hospital lengths of stay and mortality were not different. This could be possibly explained by the fact that nearly 28 % of the patients with hemorrhagic stroke underwent surgical evacuation, which might have expedited their recovery resulting in a shorter ventilation time.
The main limitations of our study are inherent to its retrospective design. Management decisions, including use of T-piece trial, extubation, tracheostomy, and level of care were decided by the treating team, and we cannot exclude selection bias. Moreover the practice of liberation from mechanical ventilation is likely institutional specific and also depends on the intensivist’s experience. Ours is a referral center, and many patients included in this study were referred from other hospitals. Therefore our findings may be confounded by referral bias and might not be representative of the experience in other hospitals. Since the inclusion criteria of our study spanned 10 years, there have been changes in the patient care including indications for mechanical ventilation, extubation process, tracheostomy as well as overall patient care like indications for surgery, types of surgery, and indication of thrombolysis. This might have affected our final results. We were not able to perform a multivariable analysis comparing successful extubation versus extubation failure (i.e., patients requiring reintubation) because of the small size of the latter group. Despite these limitations our study is the largest and first of its kind to explore the factors responsible for extubation in this unique population of posterior fossa strokes. Prospective comparative trials with larger cohorts or multicenter studies for adequate sample sizes are needed to further evaluate the predictors of extubation failure.
Conclusions
In this study of large cohort of posterior fossa stroke patients, we found that GCS > 6 at the time of intubation and mechanical ventilation duration <1 week are the strongest predictors of successful extubation. Extubation success can be achieved in more than one third of patients with posterior fossa stroke requiring mechanical ventilatory support and in nearly three-quarters of patients in whom extubation is attempted. In posterior fossa stroke patients with a GCS ≤ 6 at the time of intubation and who remain intubated for more than 1 week, extubation is unlikely to be successful.
References
Wijdicks EF, Scott JP. Outcome in patients with acute basilar artery occlusion requiring mechanical ventilation. Stroke. 1996;27:1301–3.
Rabinstein AA, Wijdicks EF. Outcome of survivors of acute stroke who require prolonged ventilatory assistance and tracheostomy. Cerebrovasc Dis. 2004;18:325–31.
Steiner T, Mendoza G, De Georgia M, Schellinger P, Holle R, Hacke W. Prognosis of stroke patients requiring mechanical ventilation in a neurological critical care unit. Stroke. 1997;28:711–5.
Wijdicks EF, Scott JP. Causes and outcome of mechanical ventilation in patients with hemispheric ischemic stroke. Mayo Clin Proc. 1997;72:210–3.
Castro AA, Cortopassi F, Sabbag R, Torre-Bouscoulet L, Kumpel C, Porto EF. WITHDRAWN: respiratory muscle assessment in predicting extubation outcome in patients with stroke. Arch Bronconeumol. 2012;48(8):274–9.
Bosel J, Schiller P, Hook Y, et al. Stroke-related early tracheostomy versus prolonged orotracheal intubation in neurocritical care trial (SETPOINT): a randomized pilot trial. Stroke. 2013;44:21–8.
Epstein SK, Ciubotaru RL. Independent effects of etiology of failure and time to reintubation on outcome for patients failing extubation. Am J Respir Crit Care Med. 1998;158:489–93.
Epstein SK, Ciubotaru RL, Wong JB. Effect of failed extubation on the outcome of mechanical ventilation. Chest. 1997;112:186–92.
Qureshi AI, Suarez JI, Parekh PD, Bhardwaj A. Prediction and timing of tracheostomy in patients with infratentorial lesions requiring mechanical ventilatory support. Crit Care Med. 2000;28:1383–7.
Adams HP Jr, Bendixen BH, Kappelle LJ, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of Org 10172 in Acute Stroke Treatment. Stroke. 1993;24:35–41.
Kothari RU, Brott T, Broderick JP, et al. The ABCs of measuring intracerebral hemorrhage volumes. Stroke. 1996;27:1304–5.
Li M, Liu J, Tan R, Liu Z, Yin J, Qu H. Risk factors for slowly resolving pneumonia in the intensive care unit. J Microbiol Immunol Infect. 2014.
Coplin WM, Pierson DJ, Cooley KD, Newell DW, Rubenfeld GD. Implications of extubation delay in brain-injured patients meeting standard weaning criteria. Am J Respir Crit Care Med. 2000;161:1530–6.
Mokhlesi B, Tulaimat A, Gluckman TJ, Wang Y, Evans AT, Corbridge TC. Predicting extubation failure after successful completion of a spontaneous breathing trial. Respir Care. 2007;52:1710–7.
Namen AM, Ely EW, Tatter SB, et al. Predictors of successful extubation in neurosurgical patients. Am J Respir Crit Care Med. 2001;163:658–64.
Salam A, Tilluckdharry L, Amoateng-Adjepong Y, Manthous CA. Neurologic status, cough, secretions and extubation outcomes. Intensive Care Med. 2004;30:1334–9.
Seneviratne J, Mandrekar J, Wijdicks EF, Rabinstein AA. Predictors of extubation failure in myasthenic crisis. Arch Neurol. 2008;65:929–33.
van der Lely AJ, Veelo DP, Dongelmans DA, Korevaar JC, Vroom MB, Schultz MJ. Time to wean after tracheotomy differs among subgroups of critically ill patients: retrospective analysis in a mixed medical/surgical intensive care unit. Respir Care. 2006;51:1408–15.
Acknowledgments
We thank Professor Jay Mandrekar, Ph.D. for his assistance with statistical analysis.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors have nothing to disclose.
Additional information
Pramod K. Guru and Tarun D. Singh contributed equally to this work.
Rights and permissions
About this article
Cite this article
Guru, P.K., Singh, T.D., Pedavally, S. et al. Predictors of Extubation Success in Patients with Posterior Fossa Strokes. Neurocrit Care 25, 117–127 (2016). https://doi.org/10.1007/s12028-016-0249-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-016-0249-7