Abstract
Background
Anemia adversely affects cerebral oxygenation and metabolism after subarachnoid hemorrhage (SAH) and is also associated with poor outcome. There is limited evidence to support the use of packed red blood cell (PRBC) transfusion to optimize brain homeostasis after SAH. The aim of this study was to investigate the effect of transfusion on cerebral oxygenation and metabolism in patients with SAH.
Methods
This was a prospective observational study in a neurological intensive care unit of a university hospital. Nineteen transfusions were studied in 15 consecutive patients with SAH that underwent multimodality monitoring (intracranial pressure, brain tissue oxygen, and cerebral microdialysis). Data were collected at baseline and for 12 h after transfusion. The relationship between hemoglobin (Hb) change and lactate/pyruvate ratio (LPR) orbrain tissue oxygen (PbtO2) was tested using univariate and multivariable analyses.
Results
PRBC transfusion was administered on the median post-bleed day 8. The average Hb concentration at baseline was 8.1 g/dL and increased by 2.2 g/dL after transfusion. PbtO2 increased between hours 2 and 4 post-transfusion and this increase was maintained until hour 10. LPR did not change significantly during the 12-h monitoring period. After adjusting for SpO2, cerebral perfusion pressure, and LPR, the change in Hb concentration was independently and positively associated with a change in PbtO2 (adjusted b estimate = 1.39 [95 % confidence interval 0.09–2.69]; P = 0.04). No relationship between the change in Hb concentration and LPR was found.
Conclusions
PRBC transfusion resulted in PbtO2 improvement without a clear effect on cerebral metabolism prior to SAH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In patients with subarachnoid hemorrhage (SAH), anemia is a common complication and an independent predictor of poor outcome [1]. Although observational studies have shown that a Hb concentration >11 g/dL is associated with improved outcome, the optimal Hb concentration after SAH is still unclear [2–4]. Moreover, a low Hb concentration adversely affects cerebral metabolism and oxygenation after SAH [5, 6].
PRBC transfusion has also been associated with unfavorable outcomes after SAH, independent of the degree of anemia, and with higher rates of vasospasm and infections [1, 3, 4, 7–9].
There is limited evidence of the effects of increasing Hb concentration after transfusion on cerebral physiology after SAH [10, 11]. We hypothesized that increased Hb concentration after transfusion is associated with an improvement of brain oxygen and the reduction of LPR. The aim of this study was to investigate the effects of PRBC transfusion on cerebral oxygenation and metabolism in patients with poor-grade SAH.
Methods
This prospective observational study was conducted in the neurological ICU at Columbia University Medical Center between January 2008 and June 2009, under Institutional Review Board approval. We studied 19 PRBC transfusions given to 15 consecutive comatose patients who were admitted with poor-grade (Hunt and Hess grades 3–5) aneurysmal SAH and underwent multimodality neuromonitoring with combined PbtO2 and cerebral microdialysis (CMD). The inclusion criterion was (1) the transfusion of PRBC. The exclusion criteria were (1) active hemorrhage and (2) the malfunction of PbtO2 and CMD.
Patients were managed according to SAH guidelines established by the American Heart Association [12]. PRBC transfusion was left to the discretion of the clinical team, targeting Hb concentrations >8 g/dL unless there was evidence of symptomatic vasospasm or myocardial ischemia.
ICP catheters, CMD catheters (CMA 70; Mdialysis AB; flow rate, 0.3 mL/min; North Chelmsford, Massachusetts, USA), and PbtO2 probes (Licox; Integra Neurosciences; Plainsboro, New Jersey, USA) were inserted via a triple-lumen bolt at the bedside into visually normal white matter of the hemisphere deemed at greatest risk for secondary injury or of the right frontal lobe.
Physiological variables were collected at baseline and every 120 min for 12 h after the after initiation of transfusion. To best reflect the mean physiological variables every 2 h after transfusion, we averaged 5 min of continuous measurement of each parameter. Hb was measured at baseline and post-transfusion. In the exploratory analyses, we plotted the average values of LPR and PbtO2 over time after PRBC transfusion. Changes in PbtO2 and LPR from baseline to post-transfusion were studied using multivariate models.
Statistical Analysis
We performed univariate and multivariate analyses using generalized estimating equations (GEE) to study whether changes in Hb are associated with changes in PbtO2 or LPR. Adjusted b estimates and 95 % confidence intervals (CI) were reported in the final models. Statistical analyses were performed using SPSS 16 software (SPSS Inc., Chicago, IL, USA). A P value <0.05 was considered significant.
Results
All 15 patients included in the study were mechanically ventilated and had a GCS score less than or equal to 8. The median patient age was 52 years old (IQR 41–66). The median APACHE II score was 23 (IQR 22–28), the Hunt and Hess scores were 4 or 5 in 80 % of patients and 53 % of patients had a modified Fisher grade of 4. Transfusion was administered on median post-bleed day 8, and 4 patients received transfusions on 2 different occasions that were at least 1 day apart (Supplemental Table 1).
We plotted PbtO2 and LPR over time for the 12-h monitoring period. PbtO2 showed an increase between hours 2 and 4 after the initiation of transfusion. LPR did not show a clear change during the 12-h monitoring period (Fig. 1).
The average Hb concentration at baseline was 8.1 g/dL and increased by 2.2 g/dL after transfusion. Mean baseline LPR values were below the critical threshold of 40. Mean baseline PbtO2 was normal, and both PbtO2 and CPP increased after transfusion compared to baseline (Table 1).
We studied the relationship between changes in PbtO2 or LPR and other physiologic variables in two separate models. After adjusting for SO2 and LPR, every 1 g/dL increase in Hb concentration was associated with a 0.11 mmHg increase in CPP and a 1.39 mmHg increase in PbtO2 (Table 2). There was no significant relationship observed between changes in Hb concentration and changes in LPR (Supplemental Table 2). We tested for significant interactions between pre-specified variables and none were found.
Discussion
In this small prospective study, we found a significant and positive association between changes in hemoglobin concentration after PRBC transfusion and improvement of PbtO2 in comatose and mechanically ventilated patients with poor-grade SAH.
Recent studies demonstrated improvements in oxygenation after transfusion in patients with SAH [10, 11, 13]. These data suggest that transfusions are associated with an improvement in oxygen delivery to the brain without measurable metabolic impact. The effects on oxygen delivery are most likely explained by improved cerebral blood flow and improved oxygen carrying capacity. This is corroborated in our study because the effect of Hb concentration remains after adjusting for CPP increase. Again, this did not result in improved metabolism. Potential explanations of this result include a lack of ischemia at baseline and metabolic distress caused by mitochondrial dysfunction.
Our study has some limitations. First, we did not assess clinical outcomes and complications. Second, we were not able to evaluate the effects of transfusion with low baseline Hb and PbtO2 or high LPR. Third, our sample size was small. This may explain why we found no changes in metabolism. Fourth, although we ran multivariate models using repeated measurement analyses to study the physiological associations between variables, we acknowledge that the small sample size may warrant caution when interpreting our results.
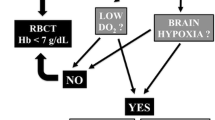
Our findings are hypothesis-generating but may also have important clinical implications. With increasing evidence that anemia affects cerebral physiology and that a liberal blood transfusion strategy may worsen the outcome, using brain oxygen as a target for goal-directed therapy, may allow for an individualized approach to PRBC transfusion. Further studies are needed to determine the effect of transfusions in patients with disrupted tissue metabolism caused by low oxygen delivery. Randomized clinical trials are needed to assess the effect of a goal-directed PRBC transfusion strategy.
References
Wartenberg KE, Schmidt JM, Claassen J, Temes RE, Frontera JA, Ostapkovich N, et al. Impact of medical complications on outcome after subarachnoid hemorrhage. Crit Care Med. 2006;34:617–23 quiz 624.
Naidech AM, Jovanovic B, Wartenberg KE, Parra A, Ostapkovich N, Connolly ES, et al. Higher hemoglobin is associated with improved outcome after subarachnoid hemorrhage. Crit Care Med. 2007;35:2383–9.
Desjardins P, Turgeon AF, Tremblay MH, Lauzier F, Zarychanski R, Boutin A, et al. Hemoglobin levels and transfusions in neurocritically ill patients: a systematic review of comparative studies. Crit Care. 2012;16:R54.
Kramer AH, Diringer MN, Suarez JI, Naidech AM, Macdonald LR, Le Roux PD. Red blood cell transfusion in patients with subarachnoid hemorrhage: a multidisciplinary north american survey. Crit Care. 2011;15:R30.
Kurtz P, Schmidt JM, Claassen J, Carrera E, Fernandez L, Helbok R, et al. Anemia is associated with metabolic distress and brain tissue hypoxia after subarachnoid hemorrhage. Neurocrit Care. 2010;13:10–6.
Oddo M, Milby A, Chen I, Frangos S, MacMurtrie E, Maloney-Wilensky E, et al. Hemoglobin concentration and cerebral metabolism in patients with aneurysmal subarachnoid hemorrhage. Stroke. 2009;40:1275–81.
Festic E, Rabinstein AA, Freeman WD, Mauricio EA, Robinson MT, Mandrekar J, et al. Blood transfusion is an important predictor of hospital mortality among patients with aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2013;18:209–15.
Levine J, Kofke A, Cen L, Chen Z, Faerber J, Elliott JP, et al. Red blood cell transfusion is associated with infection and extracerebral complications after subarachnoid hemorrhage. Neurosurgery. 2010;66:312–8 discussion 318.
Smith MJ, Le Roux PD, Elliott JP, Winn HR. Blood transfusion and increased risk for vasospasm and poor outcome after subarachnoid hemorrhage. J Neurosurg. 2004;101:1–7.
Dhar R, Zazulia AR, Videen TO, Zipfel GJ, Derdeyn CP, Diringer MN. Red blood cell transfusion increases cerebral oxygen delivery in anemic patients with subarachnoid hemorrhage. Stroke. 2009;40:3039–44.
Smith MJ, Stiefel MF, Magge S, Frangos S, Bloom S, Gracias V, et al. Packed red blood cell transfusion increases local cerebral oxygenation. Crit Care Med. 2005;33:1104–8.
Connolly ES Jr, Rabinstein AA, Carhuapoma JR, Derdeyn CP, Dion J, Higashida RT, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a guideline for healthcare professionals from the American heart association/American stroke association. Stroke. 2012;43:1711–37.
Dhar R, Scalfani MT, Zazulia AR, Videen TO, Derdeyn CP, Diringer MN. Comparison of induced hypertension, fluid bolus, and blood transfusion to augment cerebral oxygen delivery after subarachnoid hemorrhage. J Neurosurg. 2012;116:648–56.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Kurtz, P., Helbok, R., Claassen, J. et al. The Effect of Packed Red Blood Cell Transfusion on Cerebral Oxygenation and Metabolism After Subarachnoid Hemorrhage. Neurocrit Care 24, 118–121 (2016). https://doi.org/10.1007/s12028-015-0180-3
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-015-0180-3