Abstract
Introduction
Intracerebral hemorrhage (ICH) is a highly fatal disease with few proven treatments. Data to guide clinician decisions for therapies, including antiepileptic drugs (AED), are limited. Published studies on AED treatment in ICH have provided conflicting results. We investigated the effect of AED treatment on 90-day mortality after ICH in a large prospectively ascertained cohort.
Methods
We conducted a retrospective analysis of a prospectively assembled cohort of patients with ICH in the supratentorial regions, comparing 90-day mortality and modified Rankin Score among 543 patients treated with AED during hospitalization and 639 AED-free ICH. Supratentorial ICH location was categorized as lobar or deep hemispheric.
Results
Multivariate analysis demonstrated an association between AED treatment and reduced 90-day mortality in supratentorial ICH (OR = 0.62, 95 % CI 0.42–0.90, p = 0.01) and the subset of lobar ICH (OR = 0.49, 95 % CI 0.25–0.96, p = 0.04). When analyses were restricted to subjects surviving longer than 5 days from ICH, however, no association between AED treatment and a 90-day outcome, regardless of hemorrhage location (all p > 0.15), was detected, despite more than adequate power to detect the originally observed association.
Conclusion
These results suggest that AED treatment in acute ICH is not associated with 90-day mortality or outcome and that any detected association could arise by confounding by indication, in which the most severely affected patients are those in whom AEDs are prescribed. They provide a cautionary example of the limitations of drawing conclusions about treatment effects from observational data.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Intracerebral hemorrhage (ICH), comprising 15 % of all stroke cases, is a highly fatal disease, resulting in death or severe disability for more than 60 % of those affected [1, 2]. Unfortunately, few treatment options have demonstrated a benefit in randomized trials; consequently, the best available data to guide clinical decision-making often come from observational studies.
Among the many treatments that are commonly considered in the management of acute ICH is the prescription of antiepileptic drugs (AED), most commonly phenytoin and levetiracetam. Previous studies of AED treatment and outcome following ICH have been limited by retrospective design and sample size, and findings from these studies are inconsistent. Although seizures are a known complication of ICH, a recent study suggested that early seizures occur in just 14 % of ICH patients and, more notably, early seizure occurrence was not associated with outcome at 6 months [3]. Conversely, other studies have found that post-ICH seizures are associated with an increased midline shift and a worse NIH Stroke Scale score [4]. A retrospective analysis of 295 subjects (23 receiving AEDs) from the placebo arm of a randomized clinical trial found that prophylactic AED treatment, primarily with phenytoin, was associated with a poor 90-day functional outcome [5]. Naidech et al. [6] conducted a prospective analysis of 98 subjects (40 receiving AEDs), finding that treatment with phenytoin was associated with increased incidence of fever and worse outcome. However, more recent studies have reported no association between AED treatment and disability or death after ICH [7] as well as a trend toward association between levetiracetam treatment and improved cognitive outcome following intracranial hemorrhage [8]. One reason for the heterogeneity in findings may be confounding by indication—that is, the use of AED treatment is non-random, and unmeasured factors associated with outcome are incorporated in the decision to provide this therapy [9]. Therefore, we sought to investigate the effect of AED treatment on clinical outcome in a large cohort of primary ICH cases and to evaluate the role that confounding by indication might play in this setting.
Methods
This study was conducted with the approval of the MGH Institutional Review Board and all subjects either provided written informed consent prior to participation or their consent was waived via protocol-specific allowance.
Patient Recruitment and Characterization
Subjects were obtained from an ongoing longitudinal cohort study of primary ICH as previously described [10]. For the current study, subjects were consecutive patients of ≥18 years of age, presenting to the MGH Emergency Department from January 1, 2000 to July 31, 2011 with a diagnosis of primary ICH. All patients with available clinical data who had no history of seizures and were not prescribed AED prior to admission were eligible.
Clinical data were obtained prospectively by stroke neurologists as part of routine clinical care and trained, full-time study staff as research-specific protocol. Collected data included demographic information, prior medical history, and pre-ICH medication use. Subject AED use prior to acute admission for ICH was determined by querying the Partners Healthcare System Research Patient Data Registry (RPDR), which can identify patients with specific criteria, for AED (i.e., Levetiracetam, Phenytoin, Valproic Acid, Carbamazepine) for the total cohort. Subject AED treatment during admission was extracted from the RPDR dataset and was defined as use of an AED within 14 days of ICH occurrence. All CT scans were reviewed by study investigators blinded to clinical and drug exposure data to determine ICH location and the presence of intraventricular extension. ICH volume was calculated using a previously described method with excellent interrater reliability [11]. Subjects with cerebellar hemorrhages were excluded as the outcome of these hemorrhages is mainly determined by ICH volume and timely hematoma evacuation [12]. Patients and their caregivers were interviewed by telephone at 3 months post-ICH to assess the outcome using the modified Rankin Scale (mRS) score [11]. The primary outcome was defined as 90-day post-ICH mortality. In addition to death during hospital stay, the status for discharged patients was ascertained by trained personnel via telephone interview and further supplemented using the Social Security Death Index (SSDI). Mortality was chosen as the outcome of interest to limit the possibility of misclassification. Following the initial analysis, we performed a secondary analysis with functional outcome, measured by dichotomized mRS similar to Naidech et al. [6] (good outcome = 0–3, poor outcome = 4–6). Furthermore, we stratified AED treatment into phenytoin and levetiracetam to investigate the possibility of a subtype-specific effect.
Statistical Analyses
Discrete variables were expressed as count (percentage [%]) and continuous variables as mean (Standard Deviation [SD]) or median (Interquartile Range [IQR]). The association between AED treatment and clinical outcome after ICH was initially assessed using univariate logistic regression. Subsequently, multivariate logistic regression was performed to estimate the effect of AED treatment on ICH outcome after adjustment for possible confounders. Model building for multivariate analysis was carried out as follows: First, stepwise-forward selection with a lenient p value for inclusion of 0.2 was undertaken; second, variables left out in the previous step were reintroduced one at a time and those that modified the point estimate for the main exposure (AED treatment) by more than 10 % were kept in the model; third, variables excluded in the previous steps, but considered relevant based on biologic knowledge, were reintroduced into the final model. Co-linearity among variables included in the final model was evaluated by assessing changes in standard deviations of each beta after removing one variable at a time. The final model included age, gender, length of hospital stay, admission ICH volume, hypercholesterolemia (HCE), hypertension (HTN), atrial fibrillation, previous hemorrhage, presence of ventricular extension, and warfarin status as covariates; it was initially applied to the entire sample. To account for confounding by indication, the same model was subsequently applied to subjects who survived at least 5 days after an ICH occurred. Using this restricted method, we sought to pose the same analytical question in a subgroup with a more uniform clinical profile—that is, their hemorrhage was not severe enough to cause early death regardless of AED and clinical care conditions.
All statistical analyses were performed using Statistical Analysis Software version 9.3 (SAS Institute Inc. 2011, Cary, NC). A p value of <0.05 was considered statistically significant, all tests being 2-sided.
Results
AED Treatment and ICH Mortality
Within the enrollment period, 1,869 individuals presented to our center with a diagnosis of primary ICH and were enrolled in our study. After restricting the cohort for prior AED use, history of seizures, recurrent hemorrhage, and index ICH date after January 1, 2000, 1,291 subjects remained. Of these, 76 had no available outcome data and 33 had a cerebellar ICH. Therefore, a total of 1,182 subjects were eligible for analysis, comprising 543 AED-treated patients and 639 AED-free patients (Table 1). Of the 543 patients treated with AED, 371 (68 %) received phenytoin, 173 (30 %) received levetiracetam, 5 (1 %) received valproic acid, and 4 (1 %) received carbamazepine (Table 2).
In univariate analysis, AED treatment was associated with reduced mortality only in patients with lobar ICH (OR = 0.54, 95 % CI 0.36–0.80, p = 0.002). This association was not present in deep ICH (p = 0.17) or all ICH cases (p = 0.09) (Table 3). In multivariate analysis, AED treatment was associated with reduced mortality in all ICH (OR = 0.62, 95 % CI 0.42–0.90, p = 0.01) and lobar ICH (OR = 0.49, 95 % CI 0.25–0.96, p = 0.04), but not in deep ICH (p = 0.78), when controlling for established predictors of poor outcome after ICH including age and baseline ICH volume as well as length of hospital stay (Table 4).
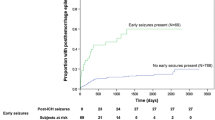
Assessment of Confounding by Indication
A main methodological concern in the analysis was that the observed association between AED and post-ICH mortality could reflect a higher rate of AED use among patients with more severe ICH, perhaps due to unmeasured confounding by indication. Consequently, we restricted our analysis to subjects who survived longer than 5 days from their index ICH to exclude those patients with early mortality during the course of disease. We reasoned that this approach would allow us to distinguish the different contributions to ICH outcome exerted by both AED treatment and other factors (e.g., hemorrhage volume) known to affect the clinical course. This restricted analysis included 779 subjects, and no association was detected between AED treatment and reduced mortality regardless of hemorrhage location (all p > 0.15) (Table 5). Post hoc power calculations performed in the restricted sample showed that this sample size was 80 % powered to detect a 19 % change in either direction. This corresponds to a minimum detectable odds ratio of 0.81 and a maximum of 1.19, which are sufficient to detect the association between AED and mortality in the larger cohort.
AED Treatment and 90-day Functional Outcome
As was the case for analysis of mortality at 90 days, the relationship between AED treatment and 90-day mRS also disappeared when the cohort was restricted to those surviving beyond 5 days. In multivariate analysis, AED treatment was associated with an improved 90-day functional outcome in all ICH (OR = 0.69, 95 % CI 0.50–0.94, p = 0.02). When the sample was restricted to subjects who survived longer than 5 days from their index ICH, no effect was detected (OR = 0.86, 95 % CI 0.61–1.20, p > 0.15) (Supplemental Table 1).
Stratification by AED Type
We stratified AED treatment into phenytoin and levetiracetam in order to ascertain any subtype-specific effect in our study. Following up on the association uncovered in lobar ICH in our initial analysis, we utilized a restricted sample in a secondary analysis to account for confounding by indication. Phenytoin treatment was not associated with 90-day mortality in the complete sample for lobar ICH (OR = 0.63, 95 % CI 0.31–1.29, p > 0.15) and in the restricted sample (OR = 1.94, 95 % CI 0.61–6.17, p > 0.15). Levetiracetam treatment was associated with reduced mortality in the complete sample for lobar ICH (OR = 0.19, 95 % CI 0.05–0.85, p = 0.03). However, this association dissipated when the sample was restricted to subjects who survived longer than 5 days from their index ICH to account for confounding by indication (OR = 0.19, 95 % CI 0.02–2.31, p > 0.15).
Discussion
Our results suggest that there is no association between AED treatment and a 90-day outcome in primary ICH patients after proper consideration of confounding by indication. Although an initial, unrestricted analysis revealed an association between exposure to AED treatment and 90-day mortality for supratentorial ICH, that association dissipated when accounting for confounding by indication through restriction of the analysis to subjects who survived for at least 5 days. Secondary analyses indicate that there is no association between AED treatment and a 90-day functional outcome as measured by mRS, and that there is no persistent subtype-specific effect when AED treatment is stratified into phenytoin and levetiracetam treatment. A post hoc power calculation revealed that the absence of any detectable association between AED treatment and outcome among those surviving beyond 5 days could not be attributed to limitations in power.
Prior retrospective studies have suggested contradictory roles for AED treatment in ICH patients, with some showing increased complications and worse outcome [5, 6], while others have failed to confirm any association between AED treatment and epilepsy, disability, or death [7]. Notably, a majority of these studies focus on treatment with phenytoin. Treatment with levetiracetam has only been suggested to either improve cognitive outcome [8] or have no effect on complications or outcomes [5]. These studies have all been observational, highlighting the paucity of randomized data available to clinicians. Given the difficulties inherent in accounting for confounding by indication in the setting of this particular outcome and exposure, only a randomized clinical trial can define the role of AED treatment in ICH patients.
Our study has a number of limitations, most of which are inherent in its observational nature. First, selection bias may be present from differential loss to follow-up. We addressed this by supplementing outcome data using the SSDI and subsequently restricting analyses to exclude subjects with no available 90-day outcome data. Second, our sample could be restricted by survival bias—that is, we are only able to ascertain the effect of AED in ICH subjects who reached the hospital alive. Even if this were the case, this would change the research question, rather than introducing bias, leading us to assess the role of AED treatment in a milder form of ICH, comprised of patients with a less severe clinical condition that allows them to reach the hospital alive.
Conclusion
Our data suggest that individuals judged to have more severe ICH are more likely to be prescribed AED by their physicians. Our initial finding that AED treatment in primary ICH patients improves the 90-day outcome did not prove robust when we eliminated from the analysis those subjects with early fatality. These results provide a cautionary reminder of the challenges of interpreting associations arising from observational studies.
References
Qureshi AI, Tuhrim S, Broderick JP, Batjer H, Hondo H, Hanley DF. Spontaneous intracerebral hemorrhage. N Engl J Med. 2001;344(19):1450–60.
Van Asch CJ, Luitse MJ, Rinkel GJ, van der Tweel I, Algra A, Klijn CJ. Incidence, case fatality, and functional outcome of intracerebral haemorrhage over time, according to age, sex, and ethnic origin: a systematic review and meta-analysis. Lancet Neurol. 2010;9:167–76.
De Herdt V, Dumont F, Henon H, Derambure P, Vonck K, Leys D, Cordonnier C. Early seizures in intracerebral hemorrhage: incidence, associated factors, and outcome. Neurology. 2011;77(20):1794–800.
Vespa PM, O’Phelan K, Shah M, et al. Acute seizures after intracerebral hemorrhage: a factor in progressive midline shift and outcome. Neurology. 2003;60(9):1441–6.
Messe SR, Sansing LH, Cucchiara BL, Herman ST, Lyden PD, Kasner SE. Prophylactic antiepileptic drug use is associated with poor outcome following ICH. Neurocrit Care. 2009;11(1):38–44.
Naidech AM, Garg RK, Liebling S, Levasseur K, Macken MP, Schuele SU, Batjer HH. Antiepileptic use and outcomes after intracerebral hemorrhage. Stroke. 2009;40(12):3810–5.
Reddig RT, Nixdorf KE, Jensen MB. The prophylactic use of an antiepileptic drug in intracerebral hemorrhage. Clin Neurol Neurosurg. 2011;113(10):895–7.
Taylor S, Heinrichs RJ, Janzen JM, Ehtisham A. Levetiracetam is associated with improved cognitive outcome for patients with intracranial hemorrhage. Neurocrit Care. 2011;15(1):80–4.
Brookhart MA, Sturmer T, Glynn RJ, Rassen J, Schneeweiss S. Confounding control in healthcare database research: challenges and potential approaches. Med Care. 2010;48(6 Suppl):S114–20.
FitzMaurice E, Wendell L, Snider R, et al. Effect of statins on intracerebral hemorrhage outcome and recurrence. Stroke. 2008;39(7):2151–4.
Flibotte JJ, Hagan N, O’Donnell J, Greenberg SM, Rosand J. Warfarin, hematoma expansion, and outcome of intracerebral hemorrhage. Neurology. 2004;63(6):1059–64.
Morioka J, Fujii M, Kato S, et al. Surgery for spontaneous intracerebral hemorrhage has greater remedial value than conservative therapy. Surg Neurol. 2006;65(1):67–72.
Acknowledgments
This work was funded by the National Institute for Neurological Disease and Stroke RO1NS059727, NIH R01NS073344, NIH K23NS059774. The authors thank Shawn Murphy and Henry Chueh and the Partners Health Care Research Patient Data Registry group for facilitating use of their database.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Battey, T.W.K., Falcone, G.J., Ayres, A.M. et al. Confounding by Indication in Retrospective Studies of Intracerebral Hemorrhage: Antiepileptic Treatment and Mortality. Neurocrit Care 17, 361–366 (2012). https://doi.org/10.1007/s12028-012-9776-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-012-9776-z