Abstract
Background
Cerebrovascular time constant (τ) estimates how fast cerebral blood arrives in cerebral arterial bed after each heart stroke. We investigate the pattern of changes in τ following subarachnoid hemorrhage (SAH), with specific emphasis on the temporal profile of changes in relation to the development of cerebral vasospasm.
Methods
Simultaneous recordings of arterial blood pressure (ABP) and transcranial Doppler (TCD) blood flow velocity (CBFV) in MCA were performed daily in patients after SAH. In 22 patients (10 males and 12 females; median age: 48 years, range: 34–84 years) recordings done before spasm were compared to those done during spasm. Vasospasm was confirmed with TCD (mean CBFV in MCA > 120 cm/s and Lindegaard ratio > 3). τ was estimated as a product of compliance of cerebral arteries (C a) and cerebrovascular resistance (CVR). C a and CVR were estimated using mathematical transformations of ABP and CBFV waveforms.
Results
Vasospasm caused shortening of τ on both the spastic (before: 0.20 ± 0.05 s vs. spasm: 0.14 ± 0.04 s, P < 0.0008) and contralateral side (before: 0.22 ± 0.05 s vs. spasm: 0.16 ± 0.04 s, P < 0.0008). Before TCD signs of vasospasm were detected, τ demonstrated asymmetry with lower values on ipsilateral side to aneurysm, in comparison to contralateral side (P < 0.009),
Conclusions
Cerebral vasospasm causes shortening of τ. Shorter τ at the side of aneurysm can be observed before formal TCD signs of vasospasm are observed, therefore, potentially reducing time to escalation of treatment.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Subarachnoid hemorrhage (SAH) is a severe neurological emergency, which currently has a 25% mortality. Delayed cerebral vasospasm is a major complication following SAH and a leading cause of morbidity and mortality in these patients, which typically requires prompt and aggressive treatment in the neurocritical care setting. It is manifested by narrowing of large cerebral arteries with a typical onset 3–5 days after SAH and maximal narrowing at 5–14 days [1]. A critical arterial narrowing leads to a reduction in cerebral blood flow (CBF) and is thought to be one of the major causes of delayed cerebral ischemia (DCI). Noninvasive Transcranial Doppler (TCD) is frequently used to monitor the development and progression of vasospasm [2]. However, the usefulness of TCD is limited by the short interval between detection of arterial narrowing and symptom onset, which leaves a relatively narrow window for further confirmatory testing, such as angiography or perfusion CT. Furthermore, a single TCD measurement of cerebral blood flow velocity (CBFV) is not sufficient when vasospasm progresses from moderate to severe as the relationship between arterial blood pressure (ABP), CBF, CBFV and diameter of the vessel becomes complex [3, 4]. Therefore, a new measure, which is independent of vessel’s radius, and which takes into account the mean velocity as well as pulsatile changes in both CBFV and ABP may be useful to improve the assessment of cerebral hemodynamics in patients after SAH.
The compliance of basal cerebral arteries (C a) decreases during cerebral vasospasm as tension of arterial smooth muscles increases. We recently developed a method to monitor changes in C a in time [5–7]. In patients with preserved autoregulation, a decrease in local perfusion pressure due to arterial narrowing causes a decrease in cerebrovascular resistance (CVR) due to dilatation of resistance vessels in the territory distal to the affected artery, in an attempt to maintain CBF and brain oxygenation [7]. After SAH, autoregulatory mechanisms are frequently impaired and it is uncertain whether downstream arterioles can still dilate during vasospasm [7, 8], and thus, induce a compensatory decrease in distal cerebrovascular resistance (CVR).
Assessment of both CVR and C a requires an assumption for cross-sectional area of insonated vessel to stay constant, which is not valid during vasospasm. We recently proposed a novel methodology to investigate the mutual relationship between compliance of large cerebral arteries (C a) and resistance of small regulatory vessels (CVR). An ultrasound-based index τ (a product of C a and CVR) termed the time constant of arterial bed, is independent of the vessel’s radius and expressed in physically interpreted units (seconds). The time constant describes how fast the arterial bed distal to the point of insonation is filled with blood [9, 10], following cardiac systole. In this study, we investigated serial changes in τ at baseline and during vasospasm in patients after SAH.
Subjects and Methods
We retrospectively analyzed digitally recorded data from the larger databases [11, 12] of SAH patients, examined with TCD day by day, to assess the state of cerebral autoregulation.
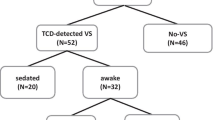
Twenty-two patients (10 males and 12 females; median age: 48 years, range: 34–84 years) suffering aneurysmal SAH, who developed TCD-detected cerebral vasospasm (mean CBFV in MCA > 120 cm/s and Lindegaard ratio (LR) (LR = CBFVMCA/CBFVICA) > 3) during the period of investigations were indentified. 9 patients were studied with approval of the local ethics committee as a part of routine clinical protocol [11, 13]. No separate informed consent was required. 13 patients were studied who were enrolled into a randomized controlled trial of the use of statins to augment cerebral hemodynamics after SAH [12]. In these patients, additional informed consent was obtained. The culprit aneurysm was clipped surgically in 19 patients, 1 patients was treated with endovascular coiling, and 2 patients had no surgical intervention. All patients received aggressive hypertensive, hypervolemic, hemodilutional therapy as part of intensive care management of vasospasm [1]. 6 patients were found to have been in the pravastatin group of the aforementioned randomized controlled trial [12]. LR was calculated and binary coded (1 for LR > 3 and 0 for LR < =3) for all patients during each examination session, in 9 patients exact values of LR were available.
Simultaneous recordings of ABP and CBFV in MCA using TCD (Neurogard, Medasonics, Fremont, CA or DWL Multi-Dop X4) were performed daily. CBFV was recorded bilaterally using 2 MHz probes. Measured signals, CBFV and ABP, were analyzed using ICM + software (Cambridge Enterprise, Cambridge, UK)—see Fig. 1.
Periods of no vasospasm and vasospasm were compared. In addition, differences between the side of vasospasm and contralateral side were analyzed. In 8 patients, vasospasm occurred bilaterally and these cases were excluded from asymmetry analysis.
Data Analysis
Cerebrovascular time constant of arterial bed τ was estimated before and during vasospasm as a product of arterial compliance C a (estimated as a ratio of pulse amplitude of cerebral arterial blood volume derived from CBFV and pulse amplitude of ABP) and cerebrovascular resistance CVR (estimated as a ration of mean ABP and mean CBFV):
Details of the formula derivation are described in [9, 10] and summarized in the appendix. It can be seen that τ is independent of the cross-sectional area of the insonated vessel.
Paired t test was used to analyze the differences in mean values at baseline versus vasospasm, and between the side of vasospasm and the contralateral side. A multivariate regression model was used to investigate the relationship between τ and the day after SAH in all 22 patients. Accounting for inter-subject variability the patient number was explicitly included into the model (using binary dummy variables recoding), and the partial correlation coefficient (R partial) between τ and the day after SAH was calculated. Statistical significance was assumed at P = 0.05.
Results
Vasospasm was detected using TCD criteria: LR > 3 [14] and CBFV > 120 cm/s [2]. Average CBFV during the vasospasm was 146.8 ± 23.4 cm/s and LR 5.1 ± 1.4. Vasospasm caused significant shortening in τ on both sides (ipsi: 0.20 ± 0.05 vs. 0.14 ± 0.04, P < 0.0008; contra: 0.22 ± 0.05 vs. 0.16 ± 0.04, P < 0.0008; see Fig. 2). There was no asymmetry in either CBFV or LR between sides before vasospasm (CBFV contra: 70.8 ± 21.4 cm/s vs. CBFV ipsi: 83.0 ± 22.1 cm/s, p = 0.15 and LR contra: 2.2 ± 0.3 vs. LR ipsi: 2.7 ± 1.3, p = 0.44, respectively). Time constant τ, however, was significantly shorter on the spastic side than on contralateral side before vasospasm (Fig. 2).
There was a negative relationship between τ and the day after SAH on the side of the vasospasm (R partial = −0.49, P = 0.000001) as well as on the contralateral, nonspastic side (R partial = −0.44, P < 0.000001). The gradual shortening of τ was demonstrated in the early days after SAH (Fig. 3). In our cohort, vasospasm was detected in 7 ± 3 days after SAH. τ stabilized in about 10-12 days after hemorrhage corresponding to the time of vasospasm, in most cases.
Discussion
In this project, we applied a novel hemodynamic index, time constant of cerebral arterial bed, to study its behavior during vasospasm in patients after SAH. The results suggest that vasospasm causes significant shortening of τ, which might be a result of a jointly reduced arterial compliance of the affected cerebral artery (C a) and a decrease in CVR due to dilatation of the resistance vessel distal to spastic section in response to diminished local perfusion pressure.
The parameter, τ, calibrated in seconds, reflects an interplay between the cerebral arterial compliance and the cerebrovascular resistance. In case of cerebral spasm, we cannot analyze changes in C a and CVR separately as the condition of unchanged vessel radius is not fulfilled. Therefore, τ, as a parameter independent of the vessel size, seems to be well suited for assessment of hemodynamics in patients after SAH. Our previous experimental study [9] showed that τ is modulated by changes in ICP, ABP and EtCO2. C a is more pressure-dependent than CVR, whereas CVR is more sensitive to changes in EtCO2 than Ca. We also found that τ shortens in patients with ICA stenosis most probably due to autoregulatory reduced CVR in the distal vascular bed [10].
The important finding is that τ demonstrated significantly lower values on the spastic side before the onset of vasospasm as identified using other TCD-indices: mean flow velocity and LR. These findings suggest that the compensatory vasodilatation can be impaired in patients following SAH prior to the development of vasospasm and that this impairment may be one of the mechanisms leading to DCI. In this study, only patients who had symptomatic cerebral vasospasm and subsequent hypertensive, hypervolemic, hemodilutional therapy were studied. Previously, it has been demonstrated that assessment of autoregulatory capacity (transient hyperemic response test) can distinguish patients who are at risk of developing neurological symptoms from those who are not [13]. It remains to be determined in a prospective study, whether assessment of τ can provide similar insight and identify patients who are at risk of DCI without the need for carotid compression. Nevertheless, the sensitivity of τ for detection of early changes in cerebral hemodynamics may improve diagnosis of vasospasm by reducing time to angiography and/or perfusion CT as well as reducing time to escalation of management. Furthermore, the independence from the cross-sectional area of the insonated vessel gives τ an advantage over traditional TCD-indices in longitudinal assessment of vasospasm evolution, therefore, guiding intensive management.
The concept of τ originates from the time constant of the electric resistor–capacitor (RC) circuit. Electric RC time constant can be interpreted as the interval required for a system or circuit to change a specified fraction from one state or condition to another.
There are limitations of the method worth listing. First, for calculation of C a we assumed that the volume of venous blood outflow remains constant during a cardiac cycle. Recent phase contrast MRI study [15] showed that sagittal sinus flow pulsatility is much lower than pulsatility of blood flow in basal arteries. Second, we used a surrogate of cerebral blood pressure by pressure measured in radial artery however we are not able to tell how much the arterial pressure and its waveform is altered by vasospasm.
In conclusion, cerebrovascular time constant becomes shorter during vasospasm and these changes precede the increase of mean blood flow velocity in MCA, thus, potentially extending the ‘therapeutic window.’
References
Bederson JB, Connolly ES Jr, Batjer HH, et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 2009;40:994–1025.
Lysakowski C, Walder B, Costanza MC, Tramer MR. Transcranial Doppler versus angiography in patients with vasospasm due to a ruptured cerebral aneurysm: a systematic review. Stroke. 2001;32:2292–8.
Spencer MP, Reid JM. Quantitation of carotid stenosis with continuous-wave (C-W) Doppler ultrasound. Stroke. 1979;10:326–30.
Aaslid R. Transcranial Doppler assessment of cerebral vasospasm. Eur J Ultrasound. 2002;16:3–10.
Kim DJ, Kasprowicz M, Carrera E, et al. The monitoring of relative changes in compartmental compliances of brain. Physiol Meas. 2009;30:647–59.
Carrera E, Kim DJ, Castellani G, et al. Effect of hyper- and hypocapnia on cerebral arterial compliance in normal subjects. J Neuroimaging. 2011;21:121–5.
Yundt KD, Grubb RL Jr, Diringer MN, Powers WJ. Autoregulatory vasodilation of parenchymal vessels is impaired during cerebral vasospasm. J Cereb Blood Flow Metab. 1998;18:419–24.
Ohkuma H, Manabe H, Tanaka M, Suzuki S. Impact of cerebral microcirculatory changes on cerebral blood flow during cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Stroke. 2000;31:1621–7.
Czosnyka M, Richards KH, Reinhard M, et al. Cerebrovascular time constant : dependence on cerebral perfusion pressure and end-tidal carbon dioxide concentration. Neurol Res. 2011; in press.
Kasprowicz M, Diedler J, Reinhard M, et al. Time constant of the cerebral arterial bed. Acta Neurochir Suppl. 2011; in press.
Soehle M, Czosnyka M, Pickard JD, Kirkpatrick PJ. Continuous assessment of cerebral autoregulation in subarachnoid hemorrhage. Anesth Analg. 2004;98:1133–9. table of contents.
Tseng MY, Czosnyka M, Richards H, Pickard JD, Kirkpatrick PJ. Effects of acute treatment with pravastatin on cerebral vasospasm, autoregulation, and delayed ischemic deficits after aneurysmal subarachnoid hemorrhage: a phase II randomized placebo-controlled trial. Stroke. 2005;36:1627–32.
Lam JM, Smielewski P, Czosnyka M, Pickard JD, Kirkpatrick PJ. Predicting delayed ischemic deficits after aneurysmal subarachnoid hemorrhage using a transient hyperemic response test of cerebral autoregulation. Neurosurgery. 2000;47:819–25. discussions 25-6.
Lindegaard KF, Nornes H, Bakke SJ, Sorteberg W, Nakstad P. Cerebral vasospasm diagnosis by means of angiography and blood velocity measurements. Acta Neurochir. 1989;100:12–24.
Stoquart-Elsankari S, Lehmann P, Villette A, et al. A phase-contrast MRI study of physiologic cerebral venous flow. J Cereb Blood Flow Metab. 2009;29:1208–15.
Avezaat CJ, Van Eijndhoven JH. The role of the pulsatile pressure variations in intracranial pressure monitoring. Neurosurg Rev. 1986;9:113–20.
Seaman DS, Newell KA, Piper JB, et al. Use of polytetrafluoroethylene patch for temporary wound closure after pediatric liver transplantation. Transplantation. 1996;62:1034–6.
Aaslid R, Newell DW, Stooss R, Sorteberg W, Lindegaard KF. Assessment of cerebral autoregulation dynamics from simultaneous arterial and venous transcranial Doppler recordings in humans. Stroke. 1991;22:1148–54.
Czosnyka M, Richards H, Pickard JD, Harris N, Iyer V. Frequency-dependent properties of cerebral blood transport—an experimental study in anaesthetized rabbits. Ultrasound Med Biol. 1994;20:391–9.
Acknowledgments
The authors are indebt to all nursing and research staff of NCCU participating in data collection. The project is supported by the Foundation for Polish Science and Ministry of Science and Higher Education (MK) and National Institute of Health Research, Biomedical Research Centre, Cambridge University Hospital Foundation Trust—Neurosciences Theme and Senior Investigator Award. ICM + software (http://www.neurosurg.cam.ac.uk/icmplus) is licensed by University of Cambridge, UK. PS and MC have interest in a part of licensing fee.
Author information
Authors and Affiliations
Corresponding author
Appendix
Appendix
Cerebral Arterial Blood Volume (C aBV)
The magnitude of the pulsatile changes in C aBV (ΔC aBV) used for calculation C a (Eq. 1, Data analysis) was assessed based on a model proposed by Avezaat and Eijndhoven [16]. According to that concept the changes in cerebral blood volume (ΔCBV) during a cardiac cycle can be calculated as an integral of the difference between pulsatile arterial inflow (CBFa) and venous outflow (CBFv) of cerebral blood [17]:
t 0 denotes beginning of cardiac cycle.
We made an assumption that a low pulsatility venous outflow (CBFv) may be approximated by constant flow equal to averaged arterial inflow (meanCBFa) [18]:
Therefore, the pulsatile cerebral arterial blood volume (ΔC aBV) can be expressed as:
Taking into account finite sampling frequency and assuming that cross-sectional area of the insonated vessel (the middle cerebral artery) is equal S a we can rewrite the previous equation as a discrete time difference equation in terms of flow velocity (CBFV)
where Δt is the sampling interval and CBFVa(i) is sample of cerebral arterial blood flow velocity.
Compliance of Cerebral Arterial Bed (C a)
C a was estimated as the pulsatile changes in cerebral arterial blood volume (AmpC aBV) divided by the amplitude of arterial blood pressure (AmpABP) [5, 6].
where AmpC aBV and AmpABP—the amplitudes of fundamental components (first harmonic) of C aBV and ABP pulse waveforms, respectively.
Resistance of Cerebrovascular Bed (CVR)
CVR was evaluated according to the following model [19]:
where S a denotes a cross-sectional area of the insonated vessel.
Time Constant of Cerebral Arterial Bed (τ)
τ was assessed as a product of C a and CVR:
Substituting the Eqs. 5 and 6 into Eq. 7 allowed to eliminate unknown cross-sectional area of the arterial vessel and calculate in seconds the magnitude of time constant of cerebral arterial blood inflow (τ).
Rights and permissions
About this article
Cite this article
Kasprowicz, M., Czosnyka, M., Soehle, M. et al. Vasospasm Shortens Cerebral Arterial Time Constant. Neurocrit Care 16, 213–218 (2012). https://doi.org/10.1007/s12028-011-9653-1
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9653-1