Abstract
Magnesium offers theoretic vascular and neuroprotective benefits for patients with subarachnoid hemorrhage. An electronic literature search was conducted to identify original research studies describing intravenous magnesium treatment in patients with SAH published in English between January 1990 and October 2010. Seventeen articles were identified and reviewed, including one phase III randomized-controlled clinical trial and six phase II randomized-controlled trials. Study quality was low for most of the included studies, with the phase III trial considered to be of moderate quality. Due to inconsistently reported benefits and the occurrence of side effects, phase II data suggested that intravenous magnesium for SAH provided either no overall net benefit or uncertain trade-offs. Benefit was likewise not supported in the single phase III clinical trial.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Magnesium is a noncompetitive calcium antagonist with several important vascular and potentially neuroprotective effects [1, 2]. For instance, magnesium can lead to vasodilatation by blocking the voltage-dependent calcium channel and decreasing glutamate release and the entry of calcium into the cell [3, 4]. In addition, magnesium also attenuates the effect of various potent vasoconstrictors, such as endothelin 1, and blocks the formation of reactive oxygen species [5].
These potentially helpful effects of magnesium on vasodilation and consequent neuroprotection has led some investigators to study the ability of magnesium to prevent of cerebral vasospasm and delayed cerebral ischemia after subarachnoid hemorrhage (SAH). This manuscript was designed to examine the current level of evidence for a role of magnesium in SAH management.
Methods
A Pubmed and EMBASE (Ovid) literature search was conducted for studies investigating the treatment of SAH with intravenous magnesium, using the key word “magnesium” plus at least one of the following additional terms: “subarachnoid hemorrhage,” “neuroprotection,” “clinical trials,” “cerebral vasospasm,” “delayed ischemic deficit,” and “clinical outcome.” Papers could be included if they reported on original studies with human subjects and were published in English between January 1990 and October 2010. Selected articles were those that directly addressed intravenous magnesium treatment in patients with SAH. Quality of data for each included study was determined using the GRADE approach [6].
Summary of Literature
Seventeen papers were included in this review: one phase III randomized-controlled clinical trial [7], six phase II randomized-controlled trials [8–13], one phase I trial [14], four prospective case series [15–18], two case–control studies [19, 20], two retrospective case series [21, 22], and one case report [23]. Study details and quality are described in Table 1.
The quality of most of the studies was low or very low, with the lowest quality given to case–control, case series, and case reports. Although still generally representing fairly low quality, more complete data were provided through phase II and III studies.
Phase I–II Studies
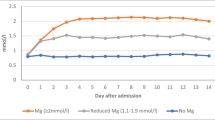
All phase II studies enrolled adult patients who were treated within the first 72 h of symptom onset. There were important differences in methodology among the studies and several limitations. Dosages of magnesium infusions varied among studies and only one paper presented a rational explanation for choosing the rate and quantity of magnesium infused. The latter was based in the only phase I study investigating the safest of 3 different dosage regimens [19]. However, the authors failed to mention how they reached the sample size chosen for their dose-escalation study. Despite this caveat, a review of available phase II data suggests that an infusion of 64 mmol/day of magnesium sulfate is safe in patients with SAH.
Another difficulty with the interpretation of phase II clinical trials is that the primary and secondary outcome measures employed also differed among studies. Reported outcome used a range of potential endpoints, including good or poor outcome defined by the Glasgow outcome scale (GOS), frequency of symptomatic vasospasm or delayed cerebral ischemia (DCI), and the occurrence of adverse events. Differences in the outcome measures make direct comparisons between studies difficult.
Additional limitations included varied aneurysm treatment and relatively small sample sizes. Most patients entered into these trials were treated with surgical clipping for their ruptured cerebral aneurysms; however, other treatments were also used. Sample sizes ranged from 40 to 283 patients. Only one of these studies mentioned power or sample size calculations.
The largest phase II study was powered based on the assumption that intravenous magnesium would reduce the risk of hypodense lesions on computed tomography (CT) by 40% (1−β = 80% with α = 5%) [10]. Patients received active treatment with magnesium sulfate as a continuous infusion at 64 mmol/l per day until 14 days after aneurysm treatment or up to a maximum of 18 days (n = 139), or saline placebo (n = 144). There was no reduction of risk for the outcome of any new hypodensity on CT (the primary endpoint), regardless of cause (RR 1.04; 95% CI 0.79–1.37). DCI (not defined in the article) was reduced by 34% (HR 0.66; 95% CI 0.38–1.14) in the magnesium-treated group, with a number needed-to-treat to benefit one patient of 14. A total of 18 magnesium-treated patients and 6 placebo patients experienced an excellent outcome (RR 3.4; 95% CI 1.3–8.9). Because this was a prospective, randomized, controlled study, the initial grading was high. However, quality was downgraded to low since this was a phase II study and was not powered to detect differences in a meaningfully important clinical outcome.
Most of phase II studies included in this review reported no difference in adverse events between magnesium and placebo. However, the study by Muroi et al. [12] reported hypotension in 3 patients with placebo versus 15 with magnesium infusion (11% vs. 48%, P = 0.04) and hypocalcemia in no placebo patients versus 8 with magnesium (0% vs. 26%, P = 0.005). Furthermore, magnesium infusion had to be stopped in 16 patients (52%) due to side effects. Based on these results, phase II data suggest either no net benefit or uncertain trade-offs with intravenous magnesium for SAH.
Phase III Studies
The only phase III study published at the time of this review studied 327 adult patients with SAH who received study medication within 48 h of symptom onset [7]. Outcomes were clearly defined. The primary outcome was achieving a favorable outcome using the extended GOS (GOSE 5–8) at 6 months. Secondary outcome measures included clinical vasospasm within 2 weeks, modified Rankin scale score 0–2 at 6 months, Barthel Index ≥ 85 at 6 months, and quality of life SF-36 at 6 months. Achieving a favorable GOSE at 6 months was similar with intravenous magnesium and placebo (64% vs. 63%; OR 1.0, 95% CI 0.7–1.6). There were likewise no differences in all secondary outcomes. Predefined subgroups based on age, admission world federation of neurosurgical societies (WFNS) grading, preexisting hypertension, intracerebral hemorrhage, intraventricular hemorrhage, location of aneurysm, or size of aneurysm did not affect outcomes. Hypotension (SBP < 90 mmHg requiring vasopressors) occurred in 15% treated with magnesium versus 13% with placebo (P = 0.590). Mortality rate was similar between treatments (10% with magnesium vs. 12% in placebo). There were no between-treatment differences in incidences of heart failure, renal failure, pneumonia, sepsis, pulmonary emboli, myocardial infarction, or gastrointestinal bleeding.
The initial grading of this trial was high, based on the phase III clinical trial design. However, grading was reduced to moderate quality of evidence due to: lack of on-site trial monitoring, absence of daily blood pressure data, and the use of a hypotension threshold definition considered to be lower than what is typically used in clinical practice.
Conclusion
Limited low to moderate quality data on intravenous magnesium treatment during SAH are available through clinical trials, with very low quality data from case series and a case report. While maintaining magnesium within normal limits in patients with SAH is reasonable, the current evidence does not support routine use of continuous intravenous infusions of magnesium sulfate in patients with SAH. Furthermore, significant side effects associated with intravenous magnesium may offset any potential benefit.
References
Saddeh M. Action of magnesium sulfate in the treatment of preeclampsia-eclampsia. Stroke. 1989;20:1273–5.
Taccone FS. Vasodilation and neuroprotection: the magnesium saga in subarachnoid hemorrhage. Crit Care Med. 2010;38:1382–3.
Marinov MB, Harbaugh KS, Hoopes PJ, Pikus HJ, Harbaugh RE. Neuroprotective effects of preischemia intra-arterial magnesium sulfate in reversible focal cerebral ischemia. J Neurosurg. 1996;85:117–24.
van den Bergh WM, Dijkhuizen RM, Rnkel GJ. Potentials of magnesium treatment in subarachnoid hemorrhage. Magnes Res. 2004;17:301–13.
Ortega-Gutierrez S, Mayer SA. Is the magnesium era for aneurysmal subarachnoid hemorrhage over? Curr Neurol Neurosci Rep. 2010;10:420–2.
Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490.
Wong GKC, Poon WS, Chan MTV, Boet R, Gin T, Ng SCP, Zee BCY, For the IMASH Investigators. Intravenous magnesium sulphate for aneurysmal subarachnoid hemorrhage (IMASH): a randomized, double-blinded, placebo-controlled, multicenter phase III trial. Stroke. 2010;41:921–6.
Westermaier T, Stetter C, Vince GH, et al. Prophylactic intravenous magnesium sulfate for treatment of aneurysmal subarachnoid hemorrhage: a randomized, placebo-controlled, clinical study. Crit Care Med. 2010;38:1284–90.
Wong GKC, Chan MTV, Boet R, Poon WS, Gin T. Intravenous magnesium sulfate after aneurysmal subarachnoid hemorrhage: a prospective randomized pilot study. J Neurosurg Anesthesiol. 2006;18:142–8.
van den Bergh WM, Algra A, van Kooten F, et al. Magnesium sulfate in aneurysmal subarachnoid hemorrhage: a randomized controlled trial. Stroke. 2005;36:1011–5.
Schmid-Elsaesser R, Kunz M, Zausinger S, Prueckner S, Briegel J, Steiger HJ. Intravenous magnesium versus nimodipine in the treatment of patients with aneurysmal subarachnoid hemorrhage: a randomized study. Neurosurgery. 2006;58:1054–65.
Muroi C, Terzic A, Fortunati M, Yonekawa Y, Keller E. Magnesium sulfate in the management of patients with aneurysmal subarachnoid hemorrhage: a randomized, placebo-controlled, dose-adapted trial. Surg Neurol. 2008;69:33–9.
Veyna RS, Seyfried D, Burke DG, et al. Magnesium sulfate therapy after aneurysmal subarachnoid hemorrhage. J Neurosurg. 2002;96:510–4.
van den Bergh WM, Albrecht KW, Berkelbach JW, van der Sprenkel B, Rinkel GJE. Magnesium therapy after aneurysmal subarachnoid haemorrhage dose-finding study for long term treatment. Acta Neurochir. 2003;145:195–9.
Stippler M, Crago E, Levy EI, et al. Magnesium infusion for vasospasm prophylaxis after subarachnoid hemorrhage. J Neurosurg. 2006;105:723–9.
Boet R, Mee E. Magnesium sulfate in the management of patients with Fisher Grade 3 subarachnoid hemorrhage: a pilot study. Neurosurgery. 2000;47:602–7.
Brewer RP, Parra A, Lynch J, Chilukuri V, Borel CO. Cerebral blood flow velocity response to magnesium sulfate in patients after subarachnoid hemorrhage. J Neurosurg Anesthesiol. 2001;13:202–6.
Mori K, Yamamoto T, Nakao Y, et al. Initial clinical experience of vasodilatory effect of intracisternal infusion of magnesium sulfate for the treatment of cerebral vasospasm after aneurysmal subarachnoid hemorrhage. Neurol Med Chir (Tokyo). 2009;49:139–45.
Friedlich D, Agner C, Boulos AS, et al. Retrospective analysis of parenteral magnesium sulfate administration in decreased incidence of clinical and neuroradiological cerebral vasospasm: a single center experience. Neurol Res. 2009;31:621–5.
Kerz T, Victor A, Beyer C, Trapp I, Heid F, Reisch R. A case control study of statin and magnesium administration in patients after aneurysmal subarachnoid hemorrhage: incidence of delayed cerebral ischemia and mortality. Neurol Res. 2008;30:893–7.
Yahia AM, Kirmani JF, Qureshi AI, Guterman LR, Hopkins LN. The safety and feasibility of continuous intravenous magnesium sulfate for prevention of cerebral vasospasm in aneurysmal subarachnoid hemorrhage. Neurocrit Care. 2005;3:16–23.
Shah QA, Memon MZ, Suri MFK, et al. Super-selective intra-arterial magnesium sulfate in combination with nicardipine for the treatment of cerebral vasospasm in patients with subarachnoid hemorrhage. Neurocrit Care. 2009;11:190–8.
Barile M, van de Wyngaert F, Mbia JJE, et al. Intravenous magnesium sulfate administration in a patient with refractory vasospasm following subarachnoid hemorrhage. Intensive Care Med. 2003;29:1182–5.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
The Participants in the International Multidisciplinary Consensus Conference: Michael N. Diringer, Thomas P. Bleck, Nicolas Bruder, E. Sander Connolly, Jr., Giuseppe Citerio, Daryl Gress, Daniel Hanggi, J. Claude Hemphill, III, MAS, Brian Hoh, Giuseppe Lanzino, Peter Le Roux, David Menon, Alejandro Rabinstein, Erich Schmutzhard, Lori Shutter, Nino Stocchetti, Jose Suarez, Miriam Treggiari, MY Tseng, Mervyn Vergouwen, Paul Vespa, Stephan Wolf, Gregory J. Zipfel.
Rights and permissions
About this article
Cite this article
Suarez, J.I., The Participants in the International Multidisciplinary Consensus Conference on the Critical Care Management of Subarachnoid Hemorrhage. Magnesium Sulfate Administration in Subarachnoid Hemorrhage. Neurocrit Care 15, 302–307 (2011). https://doi.org/10.1007/s12028-011-9603-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9603-y