Abstract
Background
There is some evidence that hyperglycemia increases the rate of poor outcomes in patients with intracerebral hemorrhage (ICH). We explored the relationship between various parameters of serum glucose concentrations measured during acute hospitalization and hematoma expansion, perihematomal edema, and three month outcome among subjects with ICH.
Methods
A post-hoc analysis of a multicenter prospective study recruiting subjects with ICH and elevated systolic blood pressure (SBP) ≥170 mmHg who presented within 6 h of symptom onset was performed. The serum glucose concentration was measured repeatedly up to 5 times over 3 days after admission and change over time was characterized using a summary statistic by fitting the linear regression model for each subject. The admission glucose, glucose change between admission and 24 hour glucose concentration, and estimated parameters (slope and intercept) were entered in the logistic regression model separately to predict the functional outcome as measured by modified Rankin scale (mRS) at 90 days (0–3 vs. 4–6); hematoma expansion at 24 h (≤33 vs. >33%); and relative perihematomal edema expansion at 24 h (≤40 vs. >40%).
Results
A total of 60 subjects were recruited (aged 62.0 ±15.1 years; 56.7% men). The mean of initial glucose concentration (±standard deviation) was 136.7 mg/dl (±58.1). Thirty-five out of 60 (58%) subjects had a declining glucose over time (negative slope). The risk of poor outcome (mRS 4–6) in those with increasing serum glucose levels was over two-fold relative to those who had declining serum glucose levels (RR = 2.64, 95% confidence interval [CI]: 1.03, 6.75). The RRs were 2.59 (95% CI: 1.27, 5.30) for hematoma expansion >33%; and 1.25 (95% CI: 0.73, 2.13) for relative edema expansion >40%.
Conclusions
Decline in serum glucose concentration correlated with reduction in proportion of subjects with hematoma expansion and poor clinical outcome. These results provide a justification for a randomized controlled clinical trial to evaluate the efficacy of aggressive serum glucose reduction in reducing death and disability among patients with ICH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Elevated serum glucose on presentation has been associated with perihematomal edema, cell death, hematoma expansion, and poor clinical outcomes in intracerebral hemorrhage (ICH) [1–4]. The targets for treatment of hyperglycemia provided in guidelines for acute ischemic stroke have varied from 185 to 300 mg/dl [5, 6] and from >150 to >250 mg/dl in studies evaluating treatment of hyperglycemia in other diseases [7]. The European Stroke Initiative (EUSI) guidelines [8] recommend intervention if blood glucose exceeds 180 mg/dl, whereas the American Stroke Association (ASA) advocates a threshold of 200 mg/dl [9]. The existing data specific to patients with ICH is based on admission glucose concentrations and does not provide information regarding the prognostic value of glucose concentrations in the acute period during hospitalization, which may have implications for developing therapeutic protocols. We performed this study to determine the effect of various parameters of serum glucose concentration acquired during acute hospitalization on clinical outcomes among a prospectively studied cohort of ICH patients.
Materials and Methods
The present report is based on a post-hoc analysis of the Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH) trial. The study design and primary results have been presented in previous publications [10]. Briefly, a multicenter prospective study recruited subjects with ICH and elevated systolic blood pressure (SBP) ≥ 170 mmHg who presented within 6 h of symptom onset in one of the three levels of treatment goals of increasing intensity (goal SBP < 200, <170, and 140 mmHg) in a step-wise fashion. A neurological assessment by a qualified neurologist was performed prior to initiation of antihypertensive treatment using the National Institutes of Health Stroke Scale (NIHSS) score, and Glasgow Coma Scale (GCS) score.
Intravenous nicardipine was administered as a continuous intravenous infusion within 6 h of symptom onset and continued until 24 h after onset of ICH. Each subject was admitted in the intensive care unit for a 24-h observation period and examined every 30 min by the nursing staff, and a comprehensive neurological examination was documented in the chart at 2-h intervals. Regular monitoring of SBP, heart rate, transcutaneous oxygen saturation, and respiratory rate were monitored was performed for 18–24 h during the infusion of nicardipine. IV 0.9% sodium chloride (20 mEq/KCl added) at 1 ml/kg/h was initiated unless contraindicated. The clinical management was in general recommended to be consistent with the guidelines provided by the special writing group of the Stroke Council, American Heart Association [11]. Serum glucose concentration was measured recorded at baseline, and at least once daily for the next 3 days according to protocol. If additional measurements were performed, the values (up to a total of 5 values) were recorded in the case report forms. The threshold for and therapy used for treating hyperglycemia was up to the discretion of the treating physician. Post-discharge follow-up was performed at 90 (±15) days from enrollment. Subjects were assessed for their functional outcome using modified Rankin scale (mRS) [12] performed by a designated neurologist who was blinded to treatment tier.
Electronic files of the baseline and 24 h computed tomographic (CT) scans were forwarded to the core laboratory for volumetric analysis. The core laboratory neuroimaging personnel, blinded to the treatment tier and clinical findings, reviewed all CT scans and recorded findings on a case report form including: (1) site of hemorrhage; (2) ventricular extension, by assessing CT scans for presence or absence of blood in the ventricles; (3) parenchymal hematoma volume and edema volume, were measured according to the method described in other studies [13–16]. The perihematoma edema volume was calculated by subtracting hematoma volume from a combined value of hematoma and edema volumes.
Statistical Analyses
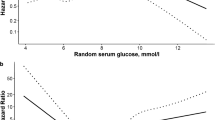
The serum glucose concentration was measured repeatedly up to five times over 3 days after admission. The glucose concentration at admission; change over time; and change at 24 h were used in the analysis. The change of serum glucose concentration over time was characterized using a summary statistic derived from fitting the linear regression model based on all 5 serum glucose measurements within the first 3 days for each subject. The best fit to a series of data points uses regression analysis to determine how much uncertainty is present in a curve that is fit to data observed with random errors. The method has been used to represent change over time for many variables including acute blood pressure changes among patients with ICH in previous studies [17]. The estimated slope was entered in the logistic regression model to predict: (1) the modified Rankin scale (mRS) at 90 days dichotomized into 0–3 vs. 4–6; (2) hematoma expansion at 24 h, dichotomized into ≤33% and >33%; and (3) relative perihematomal edema expansion at 24 h, dichotomized into ≤40% and >40%. The serum glucose variables were dichotomized at the median because no previous cutoff with prognostic validation exists for change in serum glucose between baseline and 24 h. The dichotomization for serum values at baseline for prognostic reasons has varied between studies considerably to identify a uniformly accepted cut off value. Hematoma expansion was defined as an increase in intraparenchymal hemorrhage volume of >33% measured by image analysis on the 24-h CT scan as compared with the baseline CT scan. Relative perihematomal edema volume was defined as absolute edema volume divided by hematoma volume, yielding a unitless ratio variable. The rationale for using these values for defining endpoints of interest was based on ensuring consistency with previous studies and demonstrated relationship with clinical outcomes [18–20]. We chose to dichotomize instead of using continuous variables because the relationship between percentage change in either hematoma volume or edema volume may not have a linear relationship with clinical outcome (at high volumes due to limited intracranial compliance) [21] and variation in error terms may be higher at lower volume values. We have also provided the absolute volume change (in ml) in both hematoma volume and edema volume at 24 h according to strata based on serum glucose parameters.
Primary clinical outcome was moderate to severe disability or death defined by mRS of 4–6 at 3 months following treatment initiation. We chose the mRS because of its high inter-observer reliability, superiority to other indices (e.g., Barthel index) [22, 23] and consistency with previous ICH treatment trials [1, 24, 25]. The cutoff for dichotomization was based on previous multicenter studies evaluating the effect of hematoma expansion on clinical outcome [18, 24] and in ATACH II. A more detailed discussion regarding the rationale and implications of mRS dichotomization is provided in another publication [2]. The dichotomization of 0–3 and 4–6 compares subjects who can live independently at home to subjects who are dead or dependent. A shift in this proportion would be of significant value given the high morbidity and mortality of ICH.
Because the aim of this article is secondary to the main goal of the pilot study, the analyses are descriptive in nature with mostly presentations of relative risks and their 95% confidence intervals. An exploratory multivariate analysis was performed to determine the effect of various serum glucose concentration parameters after adjusting for potential confounders including the initial GCS score, hematoma volume, and presence of intraventricular hemorrhage. We chose to only include variables with the most consistent relationship with outcome as observed in previous studies [26] due to small sample size. Inclusion of additional variables may lead to <10 outcome events per explanatory (independent) variable and may result in inaccurate risk estimates [27] and was therefore avoided. All calculations were conducted using SAS software (Cary, NC).
Results
A total of 60 subjects (62 ± 15.1 years; 56.7% men) were enrolled with 18, 20, and 22 subjects recruited in each of the tiers of increasing SBP reduction intensity. Previously diagnosed diabetes mellitus was observed in 10 subjects. Among these, 6 received subcutaneous insulin, and 3 received intramuscular or intravenous insulin within the first 7 days. Overall, % change in hematoma volume ranged from −98.2% to 1,515.8%, with a median of 3.3%; % change in relative edema volume ranged from −58.9 to 582.4% with a median of 40.5%. Of the 60 subjects, 9 were missing the 90-day mRS. One missing 90-day mRS value was imputed as 1 based on the subject’s 30-day NIHSS score of 1. The distribution among the 52 available mRS scores was: 0 = 2 (4%), 1 = 11 (21%), 2 = 12 (23%), 3 = 5 (10%), 4 = 8 (15%), 5 = 4 (8%), and 6 = 10 (19). An additional subject whose 90-day mRS score was missing had baseline and 7-day NIHSS scores of 2 and 0, respectively, and his GCS scores remained 15 throughout the first 7 days. Therefore, we imputed his dichotomized 90-day missing mRS value as good outcome (i.e., assume his 90-day mRS score to be 0–3). Subsequently, analyses of dichotomized functional outcome involved 53 subjects.
Admission mean glucose concentration (±standard deviation) was 136.7 mg/dl (±58.1) with a median value of 114 mg/dl. A total of 30 subjects had a serum glucose concentration lower than that observed at baseline. The overall median slope of glucose change within 72 h was −0.07 mg/dl/h. Thirty-five (58%) out of 60 subjects had a declining slope.
Table 1 summarizes the demographic and clinical characteristics by: (1) baseline glucose level; (2) the summary statistic (slope) of the glucose levels; and (3) change between admission and 24 h glucose concentrations. Among those with declining slope, the median was −0.32 mg/dl/h and those with increasing slope, the median was 0.20 mg/dl/h. The mean age of the subjects who had serum glucose decline within 72 h was lower than those with increasing serum glucose levels. Subjects with pre-existing diabetes mellitus had a higher proportion of subjects with elevated (>114 mg/dl) serum glucose at baseline but also a higher likelihood of both decline from baseline glucose concentration at 24 h and declining concentrations of serum glucose within 72 h. The initial GCS score and hematoma volume were similar between the subgroups defined by various parameters of serum glucose concentrations during first 72 h of hospitalization. The proportion of subjects who underwent symptomatic hematoma expansion was higher among those with lower magnitude of change from baseline glucose concentration at 24 h. Subjects who had declining concentrations of serum glucose during first 72 h had lower in-hospital and 3 months mortality.
Table 2 presents the relative risk (RR) and its 95% CI for: (1) hematoma expansion at 24 h; (2) relative edema expansion at 24 h; and (3) poor clinical outcome (i.e., mRS 4–6) at 90 days. Admission median glucose concentration or change from baseline glucose concentration at 24 h was not associated with functional outcome, hematoma expansion, or relative edema expansion. Subjects without a serum glucose decline within 72 h had a higher relative risk of symptomatic hematoma expansion (relative risk [RR] = 2.64, 95% confidence intervals [CI] 1.03–6.75) and death or disability at 3 month (RR = 2.59, 95% CI 1.27–5.30). However, there was no statistically significant association observed between the lack of serum glucose decline within 72 h and relative edema volume expansion (RR = 1.25, 95% CI 0.73–2.13). After adjusting for initial GCS score, hematoma volume, and presence of intraventricular hemorrhage, the RR of association between lack of serum glucose decline within 72 h and hematoma expansion decreased from 2.64 to 2.09 and for poor outcome from 2.59 to 1.19 (see Table 2 for adjusted RRs).
Discussion
In this exploratory analysis, we found a univariate association between lowering of glucose concentrations and decreased hematoma expansion as well as improved outcome. We used several methods to analyze the effect of glucose concentration: baseline glucose concentrations; the summary statistic (slope) of the glucose levels over 7 days, and change from baseline glucose concentration at 24 h. The study methodology provides a comprehensive assessment of prognostic significance of serum glucose values within the acute period of ICH. The first 72 h after onset represent a period of increased vulnerability to both primary and secondary (recurrent) hyperglycemia. The summary statistic is a qualitative analogue to area under the curve for serum glucose control over 72 h after initiation of treatment used in prospective studies [28, 29]. The use of summary statistic or equivalent measures is supported by other studies conducted in subjects with non-neurological diseases. A review of 24 reports reported that studies using a multiple glucose recordings provided better detection and control of hyperglycemia [7]. Another review of 49 studies [30] found that the threshold for diagnosing hyperglycemia varied among studies from >150 to >250 mg/dl. The variability prohibited the applicability and hence the reproducibility and comparability of initial glucose levels. Blood glucose concentration summaries were used in 41 out of 49 studies, reported as means and/or medians during the study period, time spent in the predefined blood glucose level range, time needed to reach the defined blood glucose level target, and hyperglycemia-related indicators.
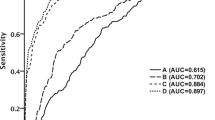
Two studies based on patients with acute ischemic stroke have highlighted the importance of pattern of change in serum glucose concentrations in addition to a single glucose measurement in the prediction of outcome. The GLycemia in Acute Stroke (GLIAS) Study [31] was a multicenter, prospective, and observational cohort study of 476 patients with ischemic stroke within less than 24 h from stroke onset. The receiver operating characteristic curves based on glucose measurements determined on admission and during the first 48 h was associated with poor outcome at 3 months. Hyperglycemia ≥155 mg/dl at any time within the first 48 h from stroke onset, and not only the isolated value of admission glucose, was associated with poor outcome. Another analysis based on 748 patients with acute ischemic stroke in the second European Cooperative Acute Stroke Study (ECASS-II) [32] used two serum glucose measurements, at baseline and at 24 h. Hyperglycemia at baseline only was not associated with any parameter of worse outcome. Persistent hyperglycemia was inversely associated with 30-day favorable functional outcome, and 90-day negligible dependence, and directly with parenchymal ICH and mortality.
The relationship between hyperglycemia at admission and outcome in patients with ICH has been identified in previous studies. A review of 416 patients with ICH reported that the mean admission blood glucose concentration was higher for nondiabetic and diabetic patients who died on the day of onset, and those dying during days 1 to 28, compared with survivors at 28 days. In logistic regression analysis, high admission blood glucose in nondiabetics was a significant predictor of death during the first 28 days of onset (odds ratio 1.2) [33]. Another study evaluated the effects of diabetes and admission hyperglycemia in among 764 patients with ICH in relation to 30-day and 3-month mortality [34] Mean admission blood glucose was higher in non-comatose diabetic subjects who died at 30 days than those who survived. Some studies such as the Acute Brain Bleeding Analysis Study which classified glucose levels in 1,387 patients with ICH found that the highest quartile of glucose level (>167 mg/dl) was an independent risk factor of early mortality [1, 4, 35] In another analysis of 645 patients with ischemic stroke and 105 patients with ICH in the Oxfordshire Community Stroke Project, serum glucose concentration greater than 144 mg/dl was associated with mortality particularly in the first month after stroke [36, 37].
It is not clear whether higher glucose is a consequence of severe neurologic injury, or actually independently contributes to it. Fogelholm et al. [33] reported that admission blood glucose was associated with disturbed consciousness, large hematoma volume and shift of cerebral midline structures in patients with ICH. Stead et al. [38] also found that hyperglycemia in the emergency department was associated with higher rate of death and disability in patients with ICH despite adjustment for stroke severity, hematoma volume, and intraventricular extension. In contrast, however, Van Kooten et al. did not find an association between stroke severity, serum cathecolamine concentrations, and hyperglycemia [37]. Some pilot data does suggest that hyperglycemia directly contributes to secondary neurological injury. One group [39] compared cerebral hemodynamics and neurochemical changes (measured by microdialysis) in ICH patients post-operatively who underwent conventional blood glucose control and intensive control with continuous titrated insulin therapy. The concentrations of lactate and pyruvate within brain parenchyma were higher in the patients with higher glucose concentrations (standard treatment group) despite similar mean cerebral perfusion pressure. Induced hyperglycemia also increased the apoptosis and edema in the perihematoma region in experimental model of ICH [2]. Inflammatory cytokines such as tumor necrosis factor-α (TNF-α) and interleukin-1 (IL-1) activated by hyperglycemia are thought to mediate the observed effect [40]. Another prospective observational study of 295 consecutive patients [41] administered variable-dose IV insulin to maintain serum glucose concentration within 60–150 mg/dl during the first 72 h after ICH. Persistently, high serum glucose concentration was more frequent among patients who died. There was a linear relationship between the mean serum glucose concentration concentrations and the likelihood of mortality. In the multivariate model, entering mean daily insulin dose as a variable attenuated the association between serum glucose concentration and mortality supporting a role for insulin treatment.
The results of the present study suggest that avoidance of hyperglycemia throughout the first 72 h of symptom onset may be the most optimal therapeutic target if the adverse consequences of hyperglycemia are modifiable. The study supports the conclusions of another previous study [41] that a higher frequency of serum glucose concentration measurement is likely to facilitate the identification of hyperglycemic ICH patients and single point measurements underestimate the true glycemic profile. Patients with ICH serum glucose decline within 72 h had a lower relative risk of death or disability at 3 months. Another study similarly suggested that higher initial and 48-h maximum glucose concentrations were significantly associated with poor functional outcome at hospital discharge among 88 patients with ICH associated with high international normalized ratio [42]. Previous studies evaluating the value of intensive glucose control in the medical ICU in non-stroke patients have also chosen the first 72 h as the period to monitor and initiate treatment [29]. Trials with shorter duration of intensive glucose control such as the UK Glucose Insulin in Stroke Trial (GIST-UK) [43] were unable to demonstrate a beneficial effect on outcomes in stroke patients. The trial randomized 933 patients presenting within 24 h of stroke onset (114 patients with ICH) and admission glucose concentration between 108 and 306 mg/dl to receive variable-dose-insulin (target 72–126 mg/dl) or saline for 24 h. There was no significant reduction in mortality at 90 days between the two groups although separate analysis for patients with ICH was not reported. It remains unclear whether inclusion of patients with only severe hyperglycemia, early initiation of treatment (within 6 h of symptom onset), prolonging the duration of control, and/or those with ICH would have modified the results.
The number of timing of serum glucose measurements, and threshold and therapy for treatment of hyperglycemia was not standardized in the ATACH trial. Therefore, the number of measurements may be higher among in patients thought to more critically ill increasing the chance of detecting elevated serum glucose concentrations. The intensity of hyperglycemia treatment may be associated with frequency of serum glucose measurements. However, 5 measurements were available for each patient as specified by protocol and used in the analysis. The case report forms did not record additional values. The study only recruited subjects with initial GCS of 8 or greater [44] therefore excluding subjects with more severe neurological deficits. The relationship between serum glucose concentrations and outcome may be more or less prominent in such patients. However, such criteria may also allow inclusion of patients in whom the effect of secondary injury and deterioration maybe more clearly delineated. The study also only included subjects with admission serum glucose concentration >50 and <400 mg/dl which may have excluded patients with severe glucose abnormalities. The other advantage of the study design was the early evaluation of patients allowing ascertainment in time period of maximum interest.
Overall, this exploratory analysis found that greater serum glucose concentration decline correlated with reduction in proportion of subjects with poor clinical outcome. These results provide a justification for a randomized controlled clinical trial to evaluate the efficacy of aggressive serum glucose reduction in reducing death and disability among patients with ICH [could add here that the GIST-UK trial found no evidence of a benefit for stroke patients], but that ICH patients made up only a small subgroup so no effect was detectable; perhaps ICH patients are those who stand to receive the most benefit from tight insulin control.
References
Qureshi AI, Palesch YY. Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH) II: design, methods, and rationale. Neurocrit Care. 2011.
Song E-C, Chu K, Jeong S-W, et al. Hyperglycemia exacerbates brain edema and perihematomal cell death after intracerebral hemorrhage. Stroke. 2003;34:2215–20.
Broderick JP, Diringer MN, Hill MD, et al. Determinants of intracerebral hemorrhage growth: an exploratory analysis. Stroke. 2007;38:1072–5.
Lee S-H, Kim BJ, Bae H-J, et al. Effects of glucose level on early and long-term mortality after intracerebral haemorrhage: the Acute Brain Bleeding Analysis Study. Diabetologia. 2010;53:429–34.
Adams HPJ, Adams RJ, Brott T, et al. Guidelines for the early management of patients with ischemic stroke: a scientific statement from the Stroke Council of the American Stroke Association. Stroke. 2003;34:1056–83.
Broderick J, Connolly S, Feldmann E, et al. Guidelines for the management of spontaneous intracerebral hemorrhage in adults: 2007 update: a guideline from the American Heart Association/American Stroke Association Stroke Council, High Blood Pressure Research Council, and the Quality of Care and Outcomes in Research Interdisciplinary Working Group. Circulation. 2007;116:e391–413.
Meijering S, Corstjens AM, Tulleken JE, et al. Towards a feasible algorithm for tight glycaemic control in critically ill patients: a systematic review of the literature. Crit Care. 2006;10:R19.
Steiner T, Kaste M, Forsting M, et al. Recommendations for the management of intracranial haemorrhage—part I: spontaneous intracerebral haemorrhage. The European Stroke Initiative Writing Committee and the Writing Committee for the EUSI Executive Committee. Cerebrovasc Dis. 2006;22:294–316.
McCormick MT, Muir KW, Gray CS, Walters MR. Management of hyperglycemia in acute stroke: how, when, and for whom? Stroke. 2008;39:2177–85.
Qureshi AI. Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH): rationale and design. Neurocrit Care. 2007;6:56–66.
Broderick JP, Adams HPJ, Barsan W, et al. Guidelines for the management of spontaneous intracerebral hemorrhage: a statement for healthcare professionals from a special writing group of the Stroke Council, American Heart Association. Stroke. 1999;30:905–15.
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19:604–7.
Brott T, Broderick J, Kothari R, et al. Early hemorrhage growth in patients with intracerebral hemorrhage. Stroke. 1997;28:1–5.
McCarron MO, Hoffmann KL, DeLong DM, et al. Intracerebral hemorrhage outcome: apolipoprotein E genotype, hematoma, and edema volumes. Neurology. 1999;53:2176–9.
McCarron MO, McCarron P, Alberts MJ. Location characteristics of early perihaematomal oedema. J Neurol Neurosurg Psychiatry. 2006;77:378–80.
Zimmerman RD, Maldjian JA, Brun NC, Horvath B, Skolnick BE. Radiologic estimation of hematoma volume in intracerebral hemorrhage trial by CT scan. AJNR Am J Neuroradiol. 2006;27:666–70.
Qureshi AI, Bliwise DL, Bliwise NG, et al. Rate of 24-hour blood pressure decline and mortality after spontaneous intracerebral hemorrhage: a retrospective analysis with a random effects regression model. Crit Care Med. 1999;27:480–5.
Anderson CS, Huang Y, Wang JG, et al. Intensive blood pressure reduction in acute cerebral haemorrhage trial (INTERACT): a randomised pilot trial. Lancet Neurol. 2008;7:391–9.
Davis SM, Broderick J, Hennerici M, et al. Hematoma growth is a determinant of mortality and poor outcome after intracerebral hemorrhage. Neurology. 2006;66:1175–81.
Gebel JMJ, Jauch EC, Brott TG, et al. Natural history of perihematomal edema in patients with hyperacute spontaneous intracerebral hemorrhage. Stroke. 2002;33:2631–5.
Schettini A, Walsh EK. Contribution of brain distortion and displacement to CSF dynamics in experimental brain compression. Am J Physiol. 1991;260:R172–8.
Wilson JTL, Hareendran A, Grant M, et al. Improving the assessment of outcomes in stroke: use of a structured interview to assign grades on the modified Rankin Scale. Stroke. 2002;33:2243–6.
Wolfe CD, Taub NA, Woodrow EJ, Burney PG. Assessment of scales of disability and handicap for stroke patients. Stroke. 1991;22:1242–4.
Mayer SA, Brun NC, Begtrup K, et al. Recombinant activated factor VII for acute intracerebral hemorrhage. N Engl J Med. 2005;352:777–85.
Broderick JP, Brott TG, Tomsick T, Barsan W, Spilker J. Ultra-early evaluation of intracerebral hemorrhage. J Neurosurg. 1990;72:195–9.
Qureshi AI, Mendelow AD, Hanley DF. Intracerebral haemorrhage. Lancet. 2009;373:1632–44.
Concato J, Feinstein AR, Holford TR. The risk of determining risk with multivariable models. Ann Intern Med. 1993;118:201–10.
van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med. 2001;345:1359–67.
Van den Berghe G, Wilmer A, Hermans G, et al. Intensive insulin therapy in the medical ICU. N Engl J Med. 2006;354:449–61.
Eslami S, de Keizer NF, de Jonge E, Schultz MJ, Abu-Hanna A. A systematic review on quality indicators for tight glycaemic control in critically ill patients: need for an unambiguous indicator reference subset. Crit Care. 2008;12:R139.
Fuentes B, Castillo J, San Jose B, et al. The prognostic value of capillary glucose levels in acute stroke: the GLycemia in Acute Stroke (GLIAS) study. Stroke. 2009;40:562–8.
Yong M, Kaste M. Dynamic of hyperglycemia as a predictor of stroke outcome in the ECASS-II trial. Stroke. 2008;39:2749–55.
Fogelholm R, Murros K, Rissanen A, Avikainen S. Admission blood glucose and short term survival in primary intracerebral haemorrhage: a population based study. J Neurol Neurosurg Psychiatry. 2005;76:349–53.
Passero S, Ciacci G, Ulivelli M. The influence of diabetes and hyperglycemia on clinical course after intracerebral hemorrhage. Neurology. 2003;61:1351–6.
Woo J, Lam CW, Kay R, et al. The influence of hyperglycemia and diabetes mellitus on immediate and 3-month morbidity and mortality after acute stroke. Arch Neurol. 1990;47:1174–7.
Weir CJ, Murray GD, Dyker AG, Lees KR. Is hyperglycaemia an independent predictor of poor outcome after acute stroke? Results of a long-term follow up study. BMJ. 1997;314:1303–6.
van Kooten F, Hoogerbrugge N, Naarding P, Koudstaal PJ. Hyperglycemia in the acute phase of stroke is not caused by stress. Stroke. 1993;24:1129–32.
Stead LG, Jain A, Bellolio MF, Odufuye A, Gilmore RM, Rabinstein A, et al. Emergency Department hyperglycemia as a predictor of early mortality and worse functional outcome after intracerebral hemorrhage. Neurocrit Care. 2010;13(1):67–74.
Ho CL, Ang CBT, Lee KK, Ng IHB. Effects of glycaemic control on cerebral neurochemistry in primary intracerebral haemorrhage. J Clin Neurosci. 2008;15:428–33.
Esposito K, Nappo F, Marfella R, et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation. 2002;106:2067–72.
Godoy DA, Pinero GR, Svampa S, Papa F, Di Napoli M. Hyperglycemia and short-term outcome in patients with spontaneous intracerebral hemorrhage. Neurocrit Care. 2008;9:217–29.
Zubkov AY, Mandrekar JN, Claassen DO, et al. Predictors of outcome in warfarin-related intracerebral hemorrhage. Arch Neurol. 2008;65:1320–5.
Gray CS, Hildreth AJ, Sandercock PA, et al. Glucose-potassium-insulin infusions in the management of post-stroke hyperglycaemia: the UK Glucose Insulin in Stroke Trial (GIST-UK). Lancet Neurol. 2007;6:397–406.
Antihypertensive Treatment of Acute Cerebral Hemorrhage (ATACH) investigators. Antihypertensive treatment of acute cerebral hemorrhage. Crit Care Med. 2010;38(2):637–48.
Acknowledgments
The principal investigator, Dr. Qureshi had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Consortia
Corresponding author
Rights and permissions
About this article
Cite this article
Qureshi, A.I., Palesch, Y.Y., Martin, R. et al. Association of Serum Glucose Concentrations During Acute Hospitalization with Hematoma Expansion, Perihematomal Edema, and Three Month Outcome Among Patients with Intracerebral Hemorrhage. Neurocrit Care 15, 428–435 (2011). https://doi.org/10.1007/s12028-011-9541-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-011-9541-8