Abstract
Background
The assumption is often made that aggressive care in the form of early decompressive hemicraniectomy is appropriate for young patients who suffer a massive stroke. However, neither their attitude toward aggressive treatment, nor their perception of acceptable quality of life after a stroke, has been adequately studied.
Methods
We conducted a cross-sectional questionnaire-based survey that consisted of demographic information and attitude toward neurological disability based on the highest acceptable modified Rankin Scale (mRS) that they would be “willing to live with.” Young adults in the Los Angeles County were surveyed and grouped by whether or not they would want early decompressive hemicraniectomy after a massive stroke. Logistic regression analysis was used to determine the factors associated with willingness to accept decompressive hemicraniectomy.
Results
Sixty-eight community-dwelling young adults (mean age: 24 ± 6 years) were surveyed. The highest acceptable mRS (0–5) participants felt “willing to live with” were: 10.3% (0), 29.4% (1), 27.9% (2), 20.6% (3), 8.8% (4), 2.9% (5). Despite being presented with a hypothetical high likelihood of long-term disability, 46 of 68 (68%) reported they would undergo hemicraniectomy. Neither the demographic factors nor the highest acceptable mRS was associated with the willingness to seek decompressive hemicraniectomy.
Conclusion
Our study supports the commonly held assumption that the majority of young adults would favor early decompressive hemicraniectomy after a massive ischemic stroke. We also show that a substantial minority in this age group is reluctant to accept this aggressive measure, emphasizing the importance of discussing the individual’s previously stated wishes, even in the young population.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
Ischemic stroke in young adults (15–45 years) accounts for up to 12% of all ischemic cerebral infarctions, with a diversity of etiologies spanning cardioembolism, arterial dissection, migraine, drugs, hematological disorders, and early atherosclerosis [1–11]. The annual incidence of ischemic stroke in young adults has been estimated to be 2–11 per 100,000 [2, 7, 12, 13]. Although the survival rate and proportion of good functional outcome are better in the young than in the older patient population [14–16], the impact of ischemic stroke on physical and emotional impairment is substantial [17, 18].
In the large middle cerebral artery (MCA) infarction (also called space-occupying or malignant MCA infarction), which is associated with 80% mortality rate with conservative medical treatment [19, 20], early decompressive hemicraniectomy has been shown to significantly reduce mortality and increase the likelihood of favorable functional outcome [21]. However, despite even aggressive surgical measures, up to 73% of the survivors may be left with moderately severe-to-severe neurological disabilities based on modified Rankin Scale. When making a commitment to proceed with a treatment that is likely life-saving but may not avoid disabling outcomes, the assumption is often made by the surrogates and the healthcare providers that early hemicraniectomy is appropriate and justified in young patients. Perhaps young adults may be viewed as having a greater stake in, and ability to achieve, good functional recovery [22]. This paternalistic approach of substituted decision making, in contrast to acting on the basis of the patient’s known values (principle of autonomy), is not uncommon in clinical practice especially when caring for young patients. This practice may relate to the infrequent opportunity of young adults to express their wishes in the fairly unlikely circumstance of massive ischemic stroke at young age, which leaves the surrogates with a profound challenge of making an informed substituted decision. Improving our understanding of the young community’s perceptions regarding the impact of stroke-related disability, and their willingness to seek aggressive treatment in such scenarios may provide valuable information to providers and surrogates involved in these critical decisions.
We conducted a population-based survey to evaluate the perception of stroke disability among community-dwelling young adults. We specifically assessed the respondent’s willingness to undergo aggressive surgical treatments (early decompressive hemicraniectomy) despite a high likelihood of major long-term disability if they were to have a massive stroke (i.e., complete MCA infarction). In addition, we evaluated the highest level of neurological disability that they would be “willing to live with” using the descriptions from modified Rankin Scale (mRS). Furthermore, we sought to evaluate the possible association between important demographic factors such as age, sex, race, marital and family status, religion, income, education level, and access to healthcare; and the decision to seek aggressive treatment.
Methods
Setting and Subjects
This community-based survey study was conducted in public locations (i.e., school campus, shopping mall, grocery store, and pedestrian streets) in the Los Angeles County over 4 months (from June to September 2008). English-speaking young adults in the community were approached by the study personnel (S.S.N.) to conduct a two-page anonymous paper survey. The study was approved by the Partners Healthcare institutional review board, and followed institutional guidelines.
Data Collection and Measures
The self-administered paper surveys were completed at the time of recruitment and were directly returned to the study personnel (S.S.N.). We collected demographic and personal characteristics including the respondent’s age, sex, race, marital status, family status, insurance status, religious preference, income, education level, history of prior stroke, and whether they knew someone who previously had a stroke. The primary outcome measure was whether or not young adults would favor aggressive care, defined as early decompressive hemicraniectomy, in the setting of a massive MCA stroke (Table 1). Conservative care was defined as “noninvasive treatment”. The secondary outcome measures included their attitude toward the highest acceptable neurological disability that they would be “willing to live with,” based on the mRS description (Table 1). In addition to using the mRS, we also asked about specific motor and language disabilities that they would be “willing to live with.” The respondents did not receive any financial compensation.
Statistical Analysis
Data were analyzed using commercially available statistical software (SPSS 16.0, Chicago, IL). Descriptive summary statistics were calculated for all variables. After dichotomous grouping based upon whether or not early decompressive hemicraniectomy was favored, variables from the two groups were compared using Student’s t-test and chi-square testing as appropriate. Logistic regression analysis was used to determine the factors associated with willingness to accept decompressive hemicraniectomy. Data are presented as means ± SD, and levels of P < 0.05 are considered statistically significant.
Results
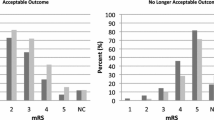
In this community-based survey study, 68 young adults (mean age: 24 ± 6) were recruited to participate in the study. Table 2 summarizes the demographic and personal characteristics of our sample. In this cohort, 46 of 68 (68%) indicated willingness to undergo aggressive treatment with early decompressive hemicraniectomy to increase the chance of survival and favorable functional outcome. Using the mRS as an analog scale of neurological disability, the distribution of the highest acceptable mRS (0–5) the participants felt “willing to live with” was as follows: 10.3% (0), 29.4% (1), 27.9% (2), 20.6% (3), 8.8% (4), 2.9% (5). Interestingly, the distribution of responses was similar in the groups favoring aggressive versus conservative treatment (Fig. 1). Further comparison of specific motor and language disability questionnaire items showed no difference between the two groups (Table 3). In univariate analysis, age of the respondents was inversely associated with favoring aggressive treatment (Table 2; P = 0.04). However, in multivariate analysis neither the demographic factors nor the individual’s highest acceptable mRS were associated with the willingness to seek aggressive treatment.
The distributions of highest acceptable modified Rankin Scale (mRS) that the respondents felt they would be “willing to live with.” The comparison between the group who favored aggressive treatment with decompressive hemicraniectomy (top) and the group who favored conservative non-surgical treatment (bottom) showed no significant difference
Discussion
The majority of community-dwelling young adults in our survey study responded in favor of early decompressive hemicraniectomy after a massive stroke, even when presented with a high likelihood of disabling outcome. Our results also showed that most young adults (73–85%) would not want to live with moderately severe-to-severe disabilities (mRS 4–5). Interestingly, this sentiment was independent of whether or not individuals favored aggressive treatment. This suggests that the assessment of acceptable deficits was not a major determinant of whether aggressive care was favored—rather, it appears that young adults approached the question of aggressive care independent of their aversion to poor neurological outcomes. Although we used the mRS as a summary metric of neurological disability, some individuals may feel more strongly about certain types of disability, such as motor and speech functions. Therefore, many respondents valued the comprehension component of language to be an important factor in their perception of acceptable quality of life. We acknowledge that the survey responses of subjects prospectively considering a hypothetical situation may differ from those of patients who have actually experienced the disabling illness. For example, Gerhart et al. [23]. reported such a difference between quadriplegic spinal cord injury patients reflecting on their own quality of life, and a control group (of physicians) reflecting on the hypothetical circumstance of quadriplegia.
In summary, our results suggest that although most young adults would not want to live with major neurological disabilities, the majority would nevertheless favor aggressive efforts to maximize the likelihood of achieving an acceptable outcome even if marked neurological impairment remains a substantial possibility. This may reflect the positive outlook that many patients exhibit when facing a devastating illness with the hope to “beat the odds.” The results from the pooled analysis of three randomized controlled trials for early decompressive surgery after a large MCA infarction showed that 14% of the surgical cohort were able to achieve very good functional outcome (mRS = 2) in 12 months [21]. From the perspective of an individual, a 14% chance may represent a reasonable hope that aggressive care could result in a favorable outcome.
Our study also indicates that a substantial minority of individuals (~30%) were reluctant to proceed with aggressive care. In this conservative group, none of the demographic factors were associated with the decision to seek conservative non-surgical treatment. We initially expected that the group favoring aggressive care would have less willingness to live with neurological disability, thus accepting the higher risk of surgery for the higher chance of good outcome. However, contrary to our expectation, the distributions of acceptable mRS after a neurological injury were similar in both groups. This important observation suggests that surrogates may not be able to extrapolate a young adult’s willingness to pursue aggressive treatments based on the patient’s perception of acceptable functional outcome. Therefore, we suggest that explicit discussion of the factors influencing the potential aggressiveness of care, especially in this setting of prognostic uncertainty, may provide the best foundation for decision making that is consistent with a person’s unique perspective and values, even in the young patient population.
Our study has several limitations. The non-response rates were difficult to assess in the public survey setting, and thus the extent to which participation bias may have confounded the results remains uncertain. Since the participants were not given the opportunity to ask specific medical questions, the levels of their understanding of this hypothetical situation and the consequences of making this major decision remain uncertain as well. Therefore, our results may not reflect the decision-making process as it occurs within the complex context of acute-onset life-threatening illness. However, we felt that providing such information might itself introduce bias into the survey responses, and, therefore, we chose to minimize medicine-related interactions between the respondents and the study personnel. Clearly, decision making in a similar “real life” scenario would involve extensive interactions with health care providers and support staff, and thus it would be interesting to study the impact of additional information upon goals of care after massive stroke. Finally, this study was conducted in a predominantly Hispanic community in the Los Angeles County area and may not generalize to other populations.
Conclusion
Our study supports the commonly held assumption that the majority of young adults would favor aggressive care in the form of early decompressive hemicraniectomy after a massive stroke. However, a substantial minority also favored conservative noninvasive measures, suggesting a diversity of opinions even in the young population, and emphasizing the importance of discussing a patient’s previously stated wishes. Further study in larger populations is needed to better characterize the factors impacting decisions regarding aggressive care in the young adult population.
References
Varona JF, Guerra JM, Bermejo F. Stroke in young adults. Med Clin (Barc). 2004;122:70–4.
Rasura M, Spalloni A, Ferrari M, et al. A case series of young stroke in Rome. Eur J Neurol. 2006;13:146–52.
Kwon SU, Kim JS, Lee JH, Lee MC. Ischemic stroke in Korean young adults. Acta Neurol Scand. 2000;101:19–24.
Alvarez J, Matias-Guiu J, Sumalla J, et al. Ischemic stroke in young adults. I. Analysis of the etiological subgroups. Acta Neurol Scand. 1989;80:28–34.
Sloan MA, Kittner SJ, Feeser BR, et al. Illicit drug-associated ischemic stroke in the Baltimore–Washington Young Stroke Study. Neurology. 1998;50:1688–93.
Kittner SJ, Stern BJ, Wozniak M, et al. Cerebral infarction in young adults: the Baltimore–Washington Cooperative Young Stroke Study. Neurology. 1998;50:890–4.
Kristensen B, Malm J, Carlberg B, et al. Epidemiology and etiology of ischemic stroke in young adults aged 18 to 44 years in northern Sweden. Stroke. 1997;28:1702–9.
Bogousslavsky J, Pierre P. Ischemic stroke in patients under age 45. Neurol Clin. 1992;10:113–24.
Adams HP Jr, Kappelle LJ, Biller J, et al. Ischemic stroke in young adults. Experience in 329 patients enrolled in the Iowa Registry of stroke in young adults. Arch Neurol. 1995;52:491–5.
Bogousslavsky J, Regli F. Ischemic stroke in adults younger than 30 years of age. Cause and prognosis. Arch Neurol. 1987;44:479–82.
Varona JF, Guerra JM, Bermejo F, Molina JA, Gomez de la Camara A. Causes of ischemic stroke in young adults, and evolution of the etiological diagnosis over the long term. Eur Neurol. 2007;57:212–8.
Nencini P, Inzitari D, Baruffi MC, et al. Incidence of stroke in young adults in Florence, Italy. Stroke. 1988;19:977–81.
Marini C, Totaro R, De Santis F, Ciancarelli I, Baldassarre M, Carolei A. Stroke in young adults in the community-based L’Aquila registry: incidence and prognosis. Stroke. 2001;32:52–6.
Putaala J, Curtze S, Hiltunen S, Tolppanen H, Kaste M, Tatlisumak T. Causes of death and predictors of 5-year mortality in young adults after first-ever ischemic stroke: the Helsinki Young Stroke Registry. Stroke. 2009;40:2698–703.
Varona JF, Bermejo F, Guerra JM, Molina JA. Long-term prognosis of ischemic stroke in young adults. Study of 272 cases. J Neurol. 2004;251:1507–14.
Kappelle LJ, Adams HP Jr, Heffner ML, Torner JC, Gomez F, Biller J. Prognosis of young adults with ischemic stroke. A long-term follow-up study assessing recurrent vascular events and functional outcome in the Iowa Registry of Stroke in Young Adults. Stroke. 1994;25:1360–5.
Naess H, Waje-Andreassen U, Thomassen L, Nyland H, Myhr KM. Health-related quality of life among young adults with ischemic stroke on long-term follow-up. Stroke. 2006;37:1232–6.
Neau JP, Ingrand P, Mouille-Brachet C, et al. Functional recovery and social outcome after cerebral infarction in young adults. Cerebrovasc Dis. 1998;8:296–302.
Hacke W, Schwab S, Horn M, Spranger M, De Georgia M, von Kummer R. ‘Malignant’ middle cerebral artery territory infarction: clinical course and prognostic signs. Arch Neurol. 1996;53:309–15.
Berrouschot J, Sterker M, Bettin S, Koster J, Schneider D. Mortality of space-occupying (‘malignant’) middle cerebral artery infarction under conservative intensive care. Intensive Care Med. 1998;24:620–3.
Vahedi K, Hofmeijer J, Juettler E, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: a pooled analysis of three randomised controlled trials. Lancet Neurol. 2007;6:215–22.
Gupta R, Connolly ES, Mayer S, Elkind MS. Hemicraniectomy for massive middle cerebral artery territory infarction: a systematic review. Stroke. 2004;35:539–43.
Gerhart KA, Koziol-McLain J, Lowenstein SR, Whiteneck GG. Quality of life following spinal cord injury: knowledge and attitudes of emergency care providers. Ann Emerg Med. 1994;23:807–12.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Nakagawa, K., Bianchi, M.T., Nakagawa, S.S. et al. Aggressive Care After a Massive Stroke in Young Patients: Is That What They Want?. Neurocrit Care 13, 118–122 (2010). https://doi.org/10.1007/s12028-010-9340-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12028-010-9340-7